Published online Jan 10, 2012. doi: 10.5306/wjco.v3.i1.12
Revised: October 25, 2011
Accepted: January 7, 2012
Published online: January 10, 2012
Problems have been reported in the treatment of pancreatic cancer with radiofrequency ablation (RFA), such as the friability of the organ itself. This report presents possible solutions to such problems. Although our patient suffered from locally advanced unresectable pancreatic cancer, she remained well at 18 mo after RFA with no evidence of recurrence. To ameliorate the side effects of RFA, after a palliative bypass procedure, the subject was treated with combined radiotherapy and chemotherapy. After this regimen had been administered, a contrast-enhanced computed tomography scan confirmed that RFA is a viable approach to the treatment of pancreatic cancer as the chemoradiotherapy had resulted in marked tumor shrinkage and pancreatic fibrosis; i.e., sufficient tumor ablation was achieved without serious RFA-related complications, such as pancreatitis or pancreatic fistulae. The present case suggests that RFA combined with preceding chemoradiotherapy is safe and effective for the palliative treatment of locally advanced pancreatic cancer.
- Citation: Ikuta S, Kurimoto A, Iida H, Aihara T, Takechi M, Kamikonya N, Yamanaka N. Optimal combination of radiofrequency ablation with chemoradiotherapy for locally advanced pancreatic cancer. World J Clin Oncol 2012; 3(1): 12-14
- URL: https://www.wjgnet.com/2218-4333/full/v3/i1/12.htm
- DOI: https://dx.doi.org/10.5306/wjco.v3.i1.12
Radical surgery is the only potentially curative treatment for pancreatic cancer, but only 5%-25% of cases are indicated for resection due to its late presentation[1,2]. Most cases of pancreatic cancer are diagnosed at an advanced stage; i.e., when they display locally advanced (presence of perineural and vascular invasion) or metastatic disease (commonly in the liver, lungs and/or peritoneum). The prognosis of patients with unresectable pancreatic cancer is dismal. The median overall survival rate is 10-12 mo and 3-6 mo in patients with unresectable locally advanced cancer and metastatic disease, respectively[2]. In patients with locally advanced pancreatic cancer, chemotherapy with or without radiotherapy, has been applied to induce tumor regression, obtain local control, slow tumor growth and relieve pain and/or symptoms. However, the treatment options for locally advanced pancreatic cancer are limited, and new therapeutic measures are required.
Radiofrequency ablation (RFA) is a local thermal therapy that is widely used for the treatment of solid parenchymal tumors[1-3]. In particular, it is effective for treating liver tumors and has been successfully employed in palliative therapy for tumors in the lung, kidney, brain, prostate and breast[1,2]. Although RFA appears to be an attractive treatment option for patients with unresectable, locally advanced and non-metastatic pancreatic cancer, the risk of thermal injury to the soft and friable pancreatic tissue has limited its clinical application. Indeed, a high frequency of life-threatening complications, such as necrotizing pancreatitis, has been reported after RFA for pancreatic tumors[4]. The aim of this report is to describe the case of a patient with locally advanced pancreatic cancer who was successfully treated with combination therapy involving open RFA and chemoradiotherapy, and thus, improve the safety and efficacy of RFA for pancreatic cancer.
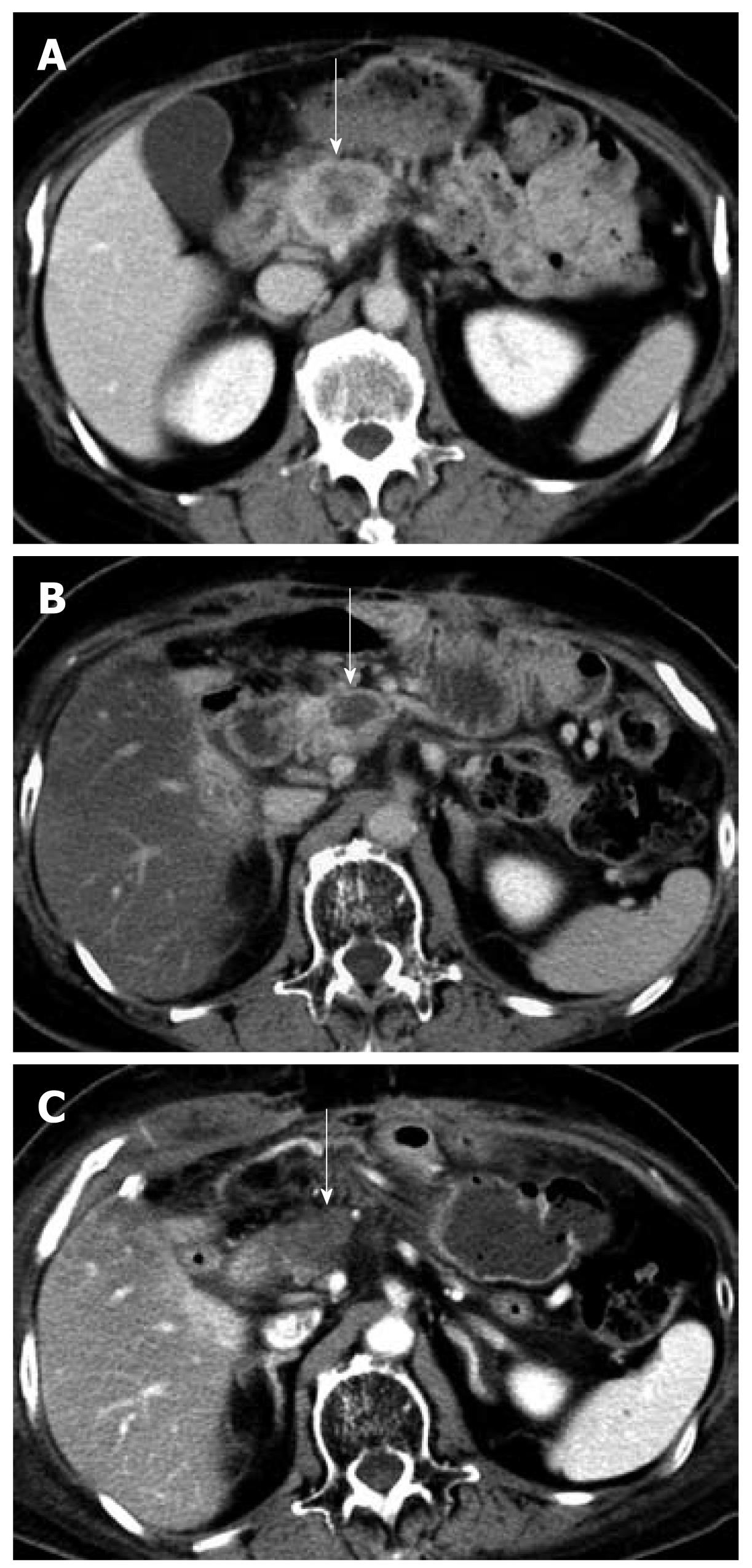
A 60-year-old woman with diabetes mellitus presented with recent weight loss and a lack of appetite. A contrast-enhanced computed tomography (CE-CT) scan revealed a pancreatic head tumor measuring 35 mm in diameter (Figure 1A), which had infiltrated into the superior mesenteric vein (SMV). Endoscopic retrograde cholangiopancreatography demonstrated main pancreatic duct disruption in the head of the pancreas and distal common bile duct stricture. A diagnosis of pancreatic adenocarcinoma was confirmed by endoscopic ultrasound guided fine-needle aspiration cytology. She was then referred to our hospital for surgical treatment. Her laboratory findings showed mild liver dysfunction and elevated serum levels of carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19-9 (7.5 ng/mL, normal < 5; 759 U/mL, normal < 37, respectively).
During laparotomy, there was no evidence of liver metastasis or peritoneal involvement, but the tumor was found to be bigger than suggested by preoperative imaging. It had grown to a diameter of 40 mm and infiltrated into the distal SMV at the level of the jejunal branch, indicating locally advanced and unresectable disease. The patient consequently underwent common bile duct-jejunostomy and gastrojejunostomy. After the initial operation, we planned to treat the patient with chemoradiotherapy to reduce the size of the tumor and induce pancreatic fibrosis, followed by RFA if possible. Extra beam radiotherapy was started one month after the bypass surgery using a 10 MV X-ray at a total dose of 4500 cGy in 180 cGy fractions. The patient was then offered gemcitabine, which was administered intravenously at 1000 mg/m2 on days 1, 8 and 15 followed by a 1-wk rest period. S-1 40 mg/m2 was co-administered orally twice daily on days 1 to 14 of each cycle. The cycles were repeated every four weeks for four cycles. A second CE-CT scan taken after the completion of chemoradiotherapy confirmed that the pancreatic head mass had shrunk (to 20 mm in diameter) (Figure 1B). Her serum levels of CEA and CA19-9 decreased to 4.0 ng/mL and 120 U/mL, respectively. Since imaging studies revealed no evidence of distant metastases and the patient was in a good general condition, the patient elected to undergo operative RFA after providing informed consent.
During the second laparotomy, fibrotic changes, which had probably been induced by the chemoradiotherapy, were observed in the duodenal wall and pancreatic head, including the tumor and surrounding normal pancreatic tissue. Frozen section examination of a needle biopsy specimen detected a small number of viable malignant cells in the necrotic fibrous tissue. We decided to perform RFA as planned because radical resection with vascular reconstruction was considered impossible. We used the latest Cool-tip™ RFA system (Radionics Inc.) and a cooled electrode (17-gauge, 15 cm in length with 2 cm insertion for rapid tumor destruction). The radiofrequency needle was placed accurately into the tumor under ultrasonographic guidance. The coagulative effect of the treatment was monitored by intraoperative ultrasonography. Two overlapping ablations were performed, the first lasted for 4 min 30 s, and the second lasted for 3 min 30 s, resulting in an intratumoral temperature of 99 °C. An abdominal drainage tube was left in place close to the ablated area.
After the procedure, the patient was intravenously infused with octreotide acetate for 5 d to prevent pancreatitis. Consequently, the patient’s postoperative course was uneventful; i.e., without complications such as pancreatitis, gastroduodenal bleeding, pancreatic fistulae and sepsis. A CE-CT scan obtained 8 d after the RFA showed a necrotic area in the head of the pancreas that corresponded to the ablation site (Figure 1C). One month after the RFA, her serum CEA and CA19-9 levels had returned to the normal range. The patient received postoperative chemotherapy with tegafur-uracil and is alive at 18 postoperative months with no signs of tumor recurrence.
The safety of RFA for pancreatic cancer is still under debate. In 2000, Matsui et al[3] first reported 20 patients with unresectable and metastatic pancreatic cancer who were treated with RFA. Of the 20 cases, two (10%) suffered critical complications; one patient died from septic shock, and the other from gastrointestinal bleeding. In 2004, Elias et al[4] reported their experience of two patients with multiple pancreatic renal cancer metastases who were treated with RFA. Unfortunately, both patients died from acute necrotizing pancreatitis and massive destruction of the normal pancreatic parenchyma. They concluded that because of the severe complications that it causes, RFA in the pancreas is not recommended. Recently, other authors have reported good postoperative results; i.e., no major procedure-related morbidity or mortality, after treating pancreatic cancer with RFA. To avoid damage to normal pancreatic tissue, Varshney et al[5] restricted the area of the tumor that was ablated in a study of three patients with unresectable pancreatic cancer. Moreover, Girelli et al[6] reported that reducing the RFA temperature from 105 °C to 90 °C resulted in a significant reduction in RFA-related complications. However, it is inevitable that such measures will attenuate the cytoreductive effect of RFA.
This case is the first to demonstrate the safety and efficacy of combining RFA with other palliative treatments such as chemoradiotherapy as a treatment for pancreatic cancer. We speculate that in the present case the chemoradiotherapy-induced peritumoral fibrosis reduced thermal conduction in the surrounding normal parenchyma, even at a higher ablation temperature than is recommended in the literature. Sufficient tumor ablation was thus achieved without increasing the risk of RFA-related pancreatitis or pancreatic fistulae. Moreover, RFA-related biliary injury and duodenal occlusion were avoided by biliary and gastric bypass surgery. Post-operative octreotide administration further reduced the risk of complications after RFA.
Although gemcitabine monotherapy is accepted as a standard first-line treatment for unresectable pancreatic cancer, gemcitabine and S-1 combination chemotherapy also has a favorable profile and results in a median overall survival of 9.3 mo[7]. Furthermore, several trials have demonstrated that the addition of radiation to chemotherapy is beneficial in terms of overall survival[8]. On the other hand, only a few studies have demonstrated a survival benefit of RFA for unresectable pancreatic cancer[9].
The application of RFA to the treatment of pancreatic tumors is still at an early stage and is undergoing research to improve its safety. The findings obtained in this case led us to the conclusion that RFA combined with preceding chemoradiotherapy is safe and might be more effective than using either modality alone, which could lead to better palliation of locally advanced pancreatic cancer. However, a case series study is required to confirm our encouraging results.
This paper is dedicated to the memory of Dr. Chiaki Yasui who gave his life to the advancement of medical science.
Peer reviewer: Thomas Yau, MBBS, MRCP, FHKCP, FHKAM, Department of Medicine, Queen Mary Hospital, University of Hong Kong, Room 405, 4/F Professorial Block, 102 Pokfulam Road, Hong Kong, China
S- Editor Yang XC L- Editor Webster JR E- Editor Li JY
| 1. | Casadei R, Ricci C, Pezzilli R, Serra C, Calculli L, Morselli-Labate AM, Santini D, Minni F. A prospective study on radiofrequency ablation locally advanced pancreatic cancer. Hepatobiliary Pancreat Dis Int. 2010;9:306-311. [PubMed] [Cited in This Article: ] |
| 2. | Pezzilli R, Serra C, Ricci C, Casadei R, Monari F, D’Ambra M, Minni F. Radiofrequency ablation for advanced ductal pancreatic carcinoma: is this approach beneficial for our patients? A systematic review. Pancreas. 2011;40:163-165. [PubMed] [Cited in This Article: ] |
| 3. | Matsui Y, Nakagawa A, Kamiyama Y, Yamamoto K, Kubo N, Nakase Y. Selective thermocoagulation of unresectable pancreatic cancers by using radiofrequency capacitive heating. Pancreas. 2000;20:14-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Elias D, Baton O, Sideris L, Lasser P, Pocard M. Necrotizing pancreatitis after radiofrequency destruction of pancreatic tumours. Eur J Surg Oncol. 2004;30:85-87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Varshney S, Sewkani A, Sharma S, Kapoor S, Naik S, Sharma A, Patel K. Radiofrequency ablation of unresectable pancreatic carcinoma: feasibility, efficacy and safety. JOP. 2006;7:74-78. [PubMed] [Cited in This Article: ] |
| 6. | Girelli R, Frigerio I, Salvia R, Barbi E, Tinazzi Martini P, Bassi C. Feasibility and safety of radiofrequency ablation for locally advanced pancreatic cancer. Br J Surg. 2010;97:220-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 7. | Oh DY, Cha Y, Choi IS, Yoon SY, Choi IK, Kim JH, Oh SC, Kim CD, Kim JS, Bang YJ. A multicenter phase II study of gemcitabine and S-1 combination chemotherapy in patients with unresectable pancreatic cancer. Cancer Chemother Pharmacol. 2010;65:527-536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Loehrer PJ, Powell ME, Cardenes HR, Wagner L, Brell JM, Ramanathan RK, Crane CH, Alberts SR, Benson AB III. A randomized phase III study of gemcitabine in combination with radiation therapy versus gemcitabine alone in patients with localized, unresectable pancreatic cancer: E4201. J Clin Oncol. 2008;26:abstr 4506. [Cited in This Article: ] |
| 9. | Zou YP, Li WM, Zheng F, Li FC, Huang H, Du JD, Liu HR. Intraoperative radiofrequency ablation combined with 125 iodine seed implantation for unresectable pancreatic cancer. World J Gastroenterol. 2010;16:5104-5110. [PubMed] [Cited in This Article: ] |