Published online May 24, 2022. doi: 10.5306/wjco.v13.i5.339
Peer-review started: October 3, 2021
First decision: November 19, 2021
Revised: November 30, 2021
Accepted: April 25, 2022
Article in press: April 25, 2022
Published online: May 24, 2022
Coronavirus disease 2019 (COVID-19) patients with malignancy are published worldwide but are lacking in data from India.
To characterize COVID-19 related mortality outcomes within 30 d of diagnosis with HRCT score and RT-PCR Ct value-based viral load in various solid malignancies.
Patients included in this study were with an active or previous malignancy and with confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection from the institute database. We collected data on demographic details, baseline clinical conditions, medications, cancer diagnosis, treatment and the COVID-19 disease course. The primary endpoint was the association between the mortality outcome and the potential prognostic variables, specially, HRCT score, RT-PCR Ct value-based viral load, etc. using logistic regression analyses treatment received in 30 d.
Out of 131 patients, 123 met inclusion criteria for our analysis. The median age was 57 years (interquartile range = 19-82) while 7 (5.7%) were aged 75 years or older. The most prevalent malignancies were of GUT origin 49 (39.8%), hepatopancreatobiliary (HPB) 40 (32.5%). 109 (88.6%) patients were on active anticancer treatment, 115 (93.5%) had active (measurable) cancer. At analysis on May 20, 2021, 26 (21.1%) patients had died. In logistic regression analysis, independent factors associated with an increased 30-d mortality were in patients with the symptomatic presentation. Chemotherapy in the last 4 wk, number of comorbidities (≥ 2 vs none: 3.43, 1.08-8.56). The univariate analysis showed that the risk of death was significantly associated with the HRCT score: for moderate (8-15) [odds ratio (OR): 3.44; 95% confidence interval (CI): 1.3-9.12; P = 0.0132], severe (> 15) (OR: 7.44; 95%CI: 1.58-35.1; P = 0.0112).
To the best of our knowledge, this is the first study from India reporting the association of HRCT score and RT-PCR Ct value-based 30-d mortality outcomes in SARS-CoV-2 infected cancer patients.
Core Tip: There is a higher fatality rate in cancer patients as compared to non-cancer patients. Also, a higher incidence of serious clinical events and intensive care unit (ICU) admissions in cancer patients. Analysis suggests patients have increased morbidity and mortality from recent cytotoxic chemotherapy. Patients with active untreated cancer, metastatic disease, progressive disease with multiple co-morbidity as well as getting palliative treatment are at a higher risk of mortality. Mortality rates are higher in patients with high baseline HRCT values at presentation and need longer ICU stays. Mortality rates are not a statistically significant co-relation with higher baseline RT-PCR based viral load values at presentation. Mortality rates are not higher in older cancer patients as compared to younger counterparts with cancer.
- Citation: Narayan S, Talwar V, Goel V, Chaudhary K, Sharma A, Redhu P, Soni S, Jain A. Co-relation of SARS-CoV-2 related 30-d mortality with HRCT score and RT-PCR Ct value-based viral load in patients with solid malignancy. World J Clin Oncol 2022; 13(5): 339-351
- URL: https://www.wjgnet.com/2218-4333/full/v13/i5/339.htm
- DOI: https://dx.doi.org/10.5306/wjco.v13.i5.339
After initially being identified in December 2019 in the Chinese city of Wuhan, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the associated sickness of coronavirus disease 2019 (COVID-19) has become a global pandemic[1]. The novel enveloped beta-coronavirus was immediately recognized as the infecting agent[2,3]. Coronaviruses are non-segmented enveloped positive-sense RNA viruses that belong to the Coronaviridae family[4]. This is the 3rd large-scale health crisis caused by beta-coronaviruses. The novel coronavirus pandemic (2019-nCoV) was designated a public health emergency of international concern by the World Health Organization (WHO) on January 30 and COVID19 was classified as a pandemic by the WHO on March 11, 2020[5]. As of May 31, 2021, there have been 171 million cases reported worldwide in 222 countries with 3.55 million deaths. In India alone, there are 28 million cases and 0.32 million fatalities. India represents an approximately 16.3% share of worldwide coronavirus cases and a 9.1% share of worldwide mortality[6]. Patients with a history of active malignancy may be at a higher risk of getting COVID-19 and having COVID-19-related problems according to various reports[7-9]. Initial reports, however, are limited by sample size, geographic region and the inability to generalize findings to the entire community of cancer patients. The impact of antineoplastic therapy and supportive care for cancer patients may impair their immune system. We conducted a retrospective study on cancer patients with COVID-19 infection comparing different demographic and clinical parameters with treatment-related mortality.
This is a single-center, retrospective study conducted at a tertiary cancer care hospital. Patients with active cancer presented to the hospital between April 2020 to April 2021 with a confirmed SARS-CoV-2 infection. The inclusion criteria were the patients with confirmed COVID-19 in a diagnosed case of solid malignancy.
The study has been approved by our Institutional Review Board (RGCIRC/Res/SCM/46 2021/95) and was conducted according to the Declaration of Helsinki.
The primary endpoint was to measure mortality within 30 d of diagnosis of COVID-19 with HRCT score and RT-PCR Ct value-based viral load. Secondary endpoints were measuring mortality compared with demographic variables (i.e. age, sex, obesity, smoking status) and clinic variables such as HRCT scoring including baseline laboratory values for D dimer, C-reactive protein (CRP), number of comorbidities, Eastern Cooperative Oncology Group (ECOG) performance status, requiring active treatment, recent surgery (including, but not limited to cancer surgeries, within 4 wk of COVID-19 diagnosis), type of malignancy, cancer status (remission vs active disease), with active further need as stable vs responding to treatment vs progressing disease), anticancer therapy and COVID-19 treatment with azithromycin, hydroxychloroquine, ivermectin or in combination vs various other treatment options used, i.e. Steroid alone or in combination with Remdesivir, Tocilizumab, Plasma therapy during infection. As it is a retrospective cohort study, selection bias occurred due to the unavailability of data for a few patients.
Descriptive statistics such as age and sex was used to show the baseline demographic information of the participants included in our analyses. All quantitative data are expressed as a mean ± SD. Categorical variables are expressed as numbers and their respective percentage. Univariate analysis was conducted to determine the risk factor of death in all the admitted patients by using Logistic regression. All data entries and statistical analyses will be performed by using SPSS® Version 23.0 software. All these statistics will be accompanied by 95% confidence intervals (CI). All the reported p-values will be two-sided and P-values < 0.05 shall be considered to indicate statistical significance.
Out of 131 patients, 123 met the inclusion criteria for our analysis. The clinical features are shown in Table 1. The median age was 57 years (interquartile range [IQR] 19-82), 7 (5.7%) were aged ≥ 75 and 64 (52%) of the patients were female. The most common malignancies were of GUT origin 49 (39.8%) and hepato-pancreaticobiliary 40 (32.5%). 109 (88.6%) patients were receiving active anticancer therapy with 115 (93.5%) patients having active (measurable) cancer. At analysis on May 20, 2021, 26 (21.1%) of the patients had died.
| Characteristics | Analysable population (n = 123) |
| Age, yr | |
| Median | 59 |
| Range | 19-82 |
| < 65 | 91 (74) |
| 65-74 | 25 (20.3) |
| ≥ 75 | 7 (5.7) |
| Sex | |
| Male | 59 (48) |
| Female | 64 (52) |
| Smoking status | |
| Never smoked | 69 (58.9) |
| Smoker (former/current) | 31 (26.3) |
| Unknown | 18 (15.2) |
| Obesity status | |
| Not specified | 106 (86.2) |
| Obese | 13 (10.4) |
| Data missing | 4 (3.4) |
| Number of comorbidities | |
| 0 | 54 (43.9) |
| 1 | 32 (26) |
| ≥ 2 | 37 (30.1) |
| Type of malignancy | |
| Thorax | 10 (8.1) |
| GIT | 9 (7.3) |
| HPB | 40 (32.5) |
| GUT | 49 (39.8) |
| Others | 15 (12.2) |
| Cancer status | |
| Remission or no evidence of disease | 8 (6.5) |
| Present, stable, or responding to treatment | 66 (53.7) |
| Present, progressive disease unknown | 49 (39.8) |
| ECOG performance status | |
| 0 or 1 | 90 (73.2) |
| 2 | 18 (14.6) |
| ≥ 3 | 15 (12.2) |
| Type of anticancer therapy | |
| None in the 4 wk before COVID-19 diagnosis | 14 (11.4) |
| Non-cytotoxic therapy targeted therapy/endocrine therapy | 9 (7.3) |
| Immunotherapy | 3 (2.4) |
| Cytotoxic systemic therapy | 90 (73.2) |
| External beam radiotherapy | 7 (5.7) |
| Recent surgery | |
| None in the 4 wk before COVID-19 diagnosis | 113 (91.9) |
| Yes | 10 (8.9) |
| Baseline laboratory parameters | |
| C Reactive protein | 44 (35.8) |
| D-Dimer | 11 (8.9) |
| IL-6 | 5 (4.1) |
| RT-PCR test (viral load) | |
| Mild (17-24) | 49 (39.8) |
| Moderate (25-31) | 30 (24.4) |
| High (> 31) | 44 (35.8) |
| HRCT score | |
| Mild | 77 (62.6) |
| Moderate | 38 (30.8) |
| Severe | 8 (6.5) |
| Treatment of COVID-19 | |
| Hydroxychloroquine (HCQ) alone, azithromycin alone or with combination HCQ/azithromycin/ivermectin | 22 (17.9) |
| + Steroids | 36 (293) |
| + Remdesivir | 29 (23.6) |
| + Tocilizumab | 3 (2.4) |
| + Plasma therapy | 11 (8.9) |
| Neither | 22 (17.9) |
Patients with mild or moderate disease were given symptomatic treatment, and most mild disease patients were treated with home-based care. Hydroxychloroquine, ivermectin and/or dexamethasone were administered in moderate disease cases. Corticosteroids, hydroxychloroquine, ivermectin, remdesivir, tocilizumab and convalescent plasma therapy were used to treat severe COVID-19-infected cancer patients. Assisted ventilation was given to 18 patients (6.45%) but all of these patients later experienced COVID-19-related complications such as pneumonitis and subsequent respiratory failure, septic shock, or sudden cardiac arrest and succumbed to their illness.
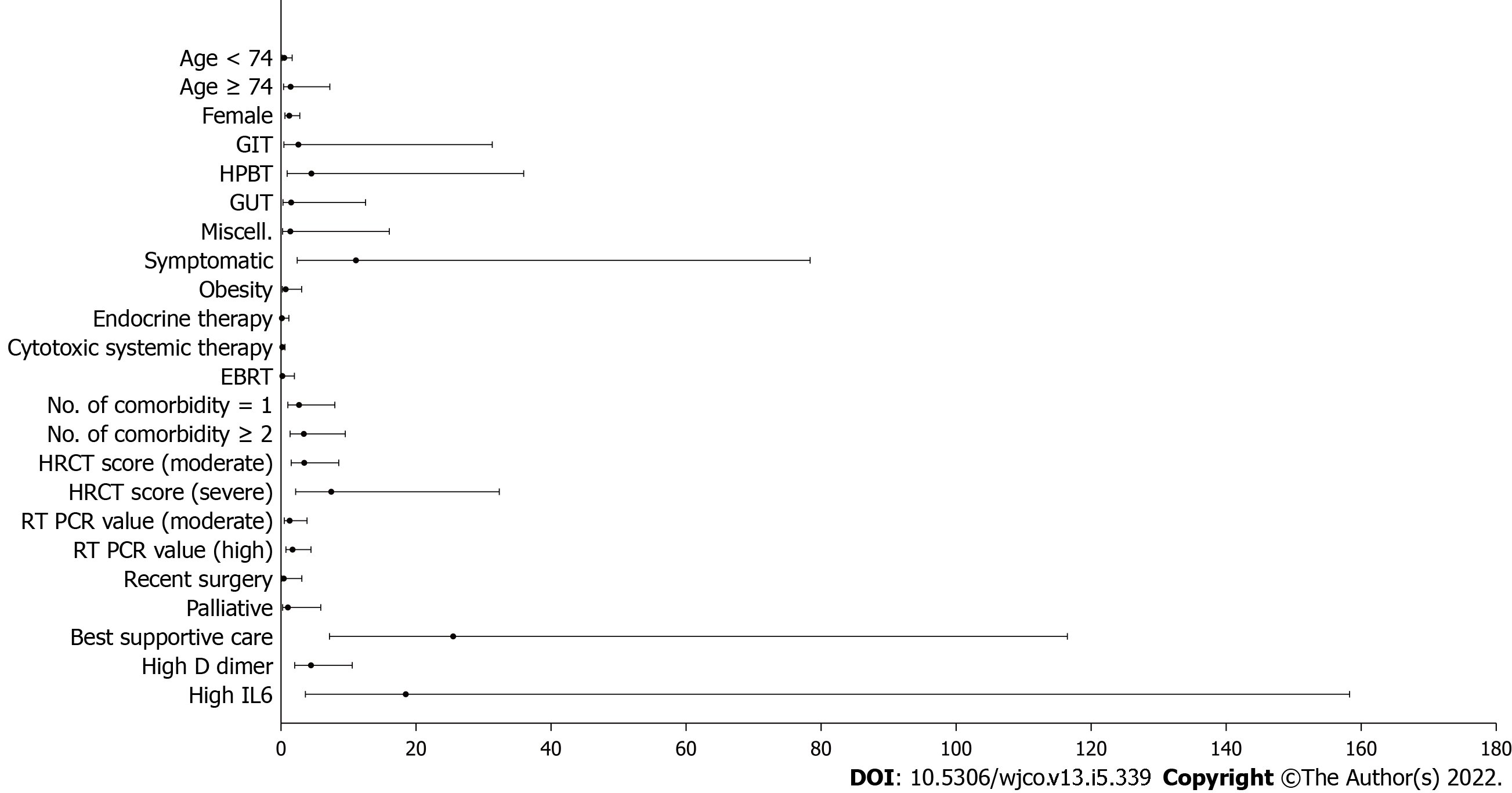
The univariate logistic regression analysis for mortality has been shown in Table 2. The risk of death was statistically significant with the presence of symptomatic presentation (odds ratio [OR] = 11.1, P = 0.0211), number of comorbidities ≥ 2 vs none (OR = 3.43, P = 0.0303), Eastern Cooperative Oncology Group performance status of 0/1 v/s ≥ 2 (OR = 3.88, P = 0.047). The odds of mortality were significantly higher in patients presenting with moderate OR = 3.44, P = 0.0132) and severe HRCT score (OR = 7.44, P = 0.0112) as compared to patients with mild HRCT score (Table 3). Similarly, patients with smoking habits were at a high risk of 30-d mortality (OR = 5.54, P < 0.001). Progressive disease was also found to be a significant risk factor for mortality with OR = 25.5) (Figure 1).
| Admitted to ICU | Met composite endpoint | Required mechanical ventilation | Died | |
| Total (n = 123) | 20 (16.2) | 30 (24.3) | 10 (8.1) | 18 (14.6) |
| Age, yr | ||||
| < 65 (n = 91) | 18 (19.7) | 22 (22.2) | 9 (9.9) | 16 (17.6) |
| 65-74 (n = 25) | 1 (4) | 5 (20) | 1 (4) | 1 (4) |
| ≥ 75 (n = 7) | 1 (14.3) | 3 (42.8) | 0 | 1 (14.3) |
| Sex | ||||
| Male (n = 59) | 6 (10.2) | 11 (18.6) | 3 (5) | 5 (8.5) |
| Female (n = 64) | 14 (21.8) | 19 (29.7) | 7 (10.9) | 13 (20.3) |
| Number of comorbidities | ||||
| 0 (n = 54) | 6 (11.1) | 9 (16.7) | 0 | 4 (7.4) |
| 1 (n = 32) | 5 (15.6) | 11 (34.4) | 4 (12.5) | 5 (15.6) |
| ≥ 2 (n = 37) | 9 (24.3) | 10 (27) | 6 (16.2) | 9 (24.3) |
| Type of malignancy | ||||
| Thorax (n = 10) | 1 (10) | 2 (20) | 1 (10) | 1 (10) |
| GIT (n = 9) | 5 (55.5) | 6 (66.6) | 3 (33.3) | 4 (44.5) |
| HPB (n = 40) | 8 (20) | 14 (35) | 4 (10) | 7 (17.3) |
| GUT (n = 49) | 5 (10) | 7 (14.2) | 2 (4) | 5 (10) |
| Others (n = 15) | 1 (6.7) | 1 (6.7) | 0 | 1 (6.7) |
| Cancer status | ||||
| Remission or no evidence of disease (n = 8) | 0 | 2 (25) | 0 | 0 |
| Present, stable, or responding to treatment (n = 66) | 6 (9.9) | 9 (13.6) | 5 (7.6) | 5 (7.6) |
| Present, progressive disease unknown (n = 49) | 14 (28.6) | 19 (38.7) | 5 (10) | 13 (26.5) |
| ECOG performance status | ||||
| 0 or 1 (n = 90) | 0 | 10 (11.1) | 0 | 0 |
| 2 (n = 18) | 2 (11.1) | 5 (27.7) | 2 (11.1) | 4 (22.2) |
| ≥ 3 (n = 15) | 15 (100) | 15 (100) | 8 (53.3) | 14 (93.3) |
| Type of anticancer therapy | ||||
| None in the 4 wk before COVID-19 diagnosis (n = 14) | 6 (42.5) | 8 (57.1) | 3 (21.4) | 5 (35.7) |
| Non-cytotoxic therapy targeted therapy/endocrine therapy (n = 9) | 2 (22.2) | 5 (55.5) | 1 (11.1) | 2 (22.2) |
| Immunotherapy (n = 3) | 0 | 0 | 0 | 0 |
| Cytotoxic systemic therapy (n = 90) | 11 (12.2) | 16 (17.7) | 6 (6.7) | 10 (11.1) |
| External beam radiotherapy (n = 7) | 1 (14.3) | 1 (14.3) | 0 | 1 (14.3) |
| Recent surgery | ||||
| None in the 4 wk before COVID-19 diagnosis (n = 113) | 19 (16.8) | 28 (24.8) | 9 (8) | 17 (15) |
| Yes (n = 10) | 1 (10) | 2 (20) | 1 (10) | 1 (10) |
| RT-PCR Test (viral load) | ||||
| Mild (n = 49) | 5 (10.2) | 8 (16.3) | 3 (6.1) | 5 (10.2) |
| Moderate (n = 30) | 5 (16.7) | 9 (30) | 4 (13.3) | 5 (16.7) |
| High (n = 44) | 10 (22.7) | 13 (29.5) | 3 (6.8) | 8 (18.1) |
| HRCT Score | ||||
| Mild (n = 77) | 7 (9) | 13 (16.9) | 0 | 5 (6.5) |
| Moderate (n = 38) | 7 (18.4) | 11 (28.9) | 4 (10.5) | 7 (18.4) |
| Severe (n = 8) | 6 (75) | 6 (75) | 6 (75) | 6 (75) |
| Treatment of COVID-19 | ||||
| Hydroxychloroquine (HCQ) alone, azithromycin alone or with combination HCQ/azithromycin/ivermectin (n = 22) | 1 (4.5) | 3 (13.6) | 0 | 1 (4.5) |
| + Steroids (n = 36) | 4 (11.1) | 8 (22.2) | 2 (5.6) | 4 (11.1) |
| + Remdesivir (n = 29) | 8 (27.6) | 11 (37.9) | 4 (13.8) | 7 (24.1) |
| + Tocilizumab (n = 3) | 1 (33.3) | 1 (33.3) | 0 | 1 (33.3) |
| + Plasma therapy (n = 11) | 6 (54.4) | 7 (63.6) | 4 (36.6) | 4 (36.6) |
| Neither (n = 22) | 0 | 0 | 0 | 0 |
| Odds ratio | P value | |
| Age, yr | ||
| < 65 | 1 | |
| 65-74 | 0.48 (0.13-1.78) | 0.2756 |
| ≥ 75 | 1.42 (0.26-7.88) | 0.6883 |
| Sex | ||
| Male | 1 | |
| Female | 1.22 (0.51-2.96) | 0.6567 |
| Smoking status | ||
| Never smoked | 1 | |
| Smoker (former/current) | 5.54 (2.05-14.99) | 0.0008 |
| Unknown | 2.19 (0.39-12.21) | 0.3711 |
| Obesity status | ||
| Not specified | 1 | |
| Obese | 0.69 (0.14-3.32) | 0.6414 |
| Number of comorbidities | ||
| 0 | 1 | |
| 1 | 2.67 (0.83-8.56) | 0.0993 |
| ≥ 2 | 3.38 (1.12-10.20) | 0.0303 |
| Type of malignancy | ||
| Thorax | 1 | |
| GIT | 2.57 (0.19-34.48) | 0.4758 |
| HPB | 4.5 (0.51-39.44) | 0.1744 |
| GUT | 1.5 (0.16-13.75) | 0.7198 |
| Others | 1.38 (0.11-17.67) | 0.8022 |
| Cancer status | ||
| Remission or no evidence of disease | 1 | |
| Present, stable, or responding to treatment | 1.02 (0.16-6.43) | 0.9832 |
| Present, progressive disease unknown | 25.5 (5.14-126.59) | 0.0001 |
| Type of anticancer therapy | ||
| None in the 4 wk before COVID-19 diagnosis | 1 | |
| Non-cytotoxic therapy targeted therapy/endocrine therapy | 0.13 (0.01-1.28) | 0.08 |
| Immunotherapy | 0 | 0.9981 |
| Cytotoxic systemic therapy | 0.19 (0.06-0.63) | 0.0067 |
| External beam radiotherapy | 0.2 (0.02-2.18) | 0.1867 |
| Recent surgery | ||
| None in the 4 wk before COVID-19 diagnosis | 1 | |
| Yes | 0.41 (0.05-3.38) | 0.4053 |
| Baseline laboratory parameters | ||
| C reactive protein | 1 | |
| D-dimer | 4.44 (1.76-11.23) | 0.0016 |
| IL-6 | 18.48 (1.96-173.82) | 0.0108 |
| HRCT score | ||
| Mild | 1 | |
| Moderate | 3.44 (1.3-9.12) | 0.0132 |
| Severe | 7.44 (1.58-35.1) | 0.0112 |
| RT-PCR Test (viral load) | ||
| Mild (49) | 1 | |
| Moderate (30) | 1.28 (0.40-4.14) | 0.6786 |
| High (44) | 1.71 (0.62-4.76) | 0.3933 |
| Treatment of COVID-19 | ||
| Hydroxychloroquine (HCQ) alone, azithromycin alone or with combination HCQ/azithromycin/ivermectin | 1 | |
| + Steroids | 3.91 (0.39-39.31) | |
| + Remdesivir | 31.06 (3.79-255.41) | 0.2470 |
| + Tocilizumab | 0.0014 | |
| + Plasma therapy | 75.25 (7.30-775.28) | 0.0003 |
| Presentation | ||
| Asymptomatic | 1 | |
| Symptomatic | 11.1 (1.43-85.85) | 0.0211 |
| Managed at | ||
| Home-based care | 1 | |
| Ward admission | 121.6 (21.8-677.7) | < 0.0001 |
| ICU admission | 0.4 (0.04-3.57) | 0.4119 |
No statistically significant association of 30-d mortality was found concerning age, sex, type of malignancy, type of anticancer therapy obesity status, recent surgery and active cancer (progressing vs remission). Also, no significant effect on mortality was noted for the patients with RT PCR based on different viral load levels.
Cancer patients are a particularly vulnerable group in the current COVID-19 pandemic. They are at a higher probability of severe illness and increased mortality once diagnosed with COVID-19. This article analyzes previously known cancer patients and COVID-19 prognostic factors provide information on clinical management and outcomes of cancer and COVID-19 patients.
In a few studies, men were found to have a higher mortality risk than women. In addition to sex disparities and smoking rates, this is due to the difference in immunological and endocrine systems between men and women which may result in differential responses to the SARS-CoV-2 infection. The present study has no similar difference related to the sex of the patient. In reports from Europe, the United States and China, non-malignant populations are consistent with COVID-19 outcome data reported for overall mortality and was associated with comorbidities such as obesity and advanced population age[10,11].
Moreover, case-fatality rates for patients with COVID-19 who had breast, thyroid, or cervical cancer were low in the previously published study. As reported, 62 (57%) of 109 women had one of these three types of cancers[12-14]. The United Kingdom Coronavirus Cancer Monitoring project (UKCCMP) with a database of 800 patients with the most common cancers were the gastrointestinal, respiratory, breast, male genital and hematological cancers. In our study, 43% of our patients had metastatic disease and 89 (72.3%) of these patients having the metastatic disease were in the GIT and HPB malignancy cohorts. Sixty-five patients had cancer treatment in the previous 4 wk for the UKCCMP while in our study 88.6% of patients had received some form of treatment in the last 4 wk. In the UKCCMP study and in our study ≥ 50% of the patients receiving treatment had received cytotoxic chemotherapy. 45 patients had a severe form of infection. The mortality rates were high at 28% (226 out of 800 in the UKCCMP) while in our present study 21.1% (26 out of 123). Disease fatality is the function of pathogen virulence, host tolerance and pathogen load[15]. Pathogenicity is often the consequence of an overactive immune or inflammatory response[15,16]. Cancer patients normally have a compromised immunity due to their existing cancer and associated treatment[17]. So, cancer patients may have persistent SARS-CoV-2 viral infection which cannot be cleared by their compromised immune system in a short time, but their COVID-19 disease is not severe and some of them may still recover from the COVID-19 disease. The majority of patients exhibited COVID-19-like symptoms and the overall rate of complications were higher. The patients who died had higher co-morbidities and were older than those who recovered. Patients who got chemotherapy within the last 4 wk of COVID-19 did not have a higher mortality rate than those who did not get chemotherapy. Patients who received non-chemotherapy treatments (radiation, hormone therapy, immunotherapy, and targeted therapy) did not have an increased risk of death[18]. COVID-19 has been associated to a greater fatality rate in cancer patients but cancer treatments have not been associated with an increased risk of mortality as found in this study.
The COVID-19 and Cancer Consortium (CCC19) published the results of 928 cancer patients from the United States, Canada and Spain who had COVID-19 infection. 654 patients with solid tumors, hematological malignancies diagnosed in 167 patients and 107 patients with multiple malignancies. In this study, 73.2% of the patients got cytotoxic chemotherapy in the previous 4 wk, whereas 160 patients received chemotherapy treatment and 206 patients received alternative forms of cancer therapy. The mortality rate was 13% within 30 d of COVID-19 diagnosis. Interestingly, 59% (n = 71) of the patients who died were never admitted to the intensive care unit (ICU); while in this study 30.8% (n = 8) died who were never admitted to the ICU. Outside the ICU, patients with active cancer have a higher death rate than those in remission. There was no association between 30-d all-cause mortality and non-cytotoxic treatments, recent surgery and cytotoxic treatment[19].
Mehta et al[20] have reported outcomes on 218 cancer patients with COVID-19. Seventy-five patients had solid tumors and 25% had hematological malignancies. The most common tumor types were genitourinary, breast and colorectal cancer, respectively. A total of 61 (28%) patients died. The mortality rate was 55% in patients with lung cancer and 67% with pancreatic cancer. Breast (14%) and genitourinary cancer (15%) were associated with a relatively lower mortality rate. Active chemotherapy and radiation therapy were not associated with increased mortality. Active disease (< 1 year) and metastatic disease were associated with higher numerical mortality values but without statistical significance[20].
Studies that report Ct values of RT-PCR to quantify SARS-CoV-2 RNA in clinical material is limited. Patients with severe disease had significantly higher viral loads and the viral load was higher during the early stages of the disease according to Zheng et al[21]. Karahasan Yagci et al[22] reported that higher viral load was linked with increased age, comorbidities, smoking status and recent chemotherapy. SARS-CoV-2 RNA had a median Ct value of 28.16 (IQR: 24.5–31.6) in hospitalized patients and 26.77 (IQR: 23.1-29.7) in outpatients in the study. The number of comorbidities were higher in hospitalized patients (P < 0.01). In COVID-19, Huang et al[23], in 2020, reported that elevated CRP was associated with higher composite poor outcome and disease severity.
The CRP levels available at the time of the PCR request were largely for hospitalized patients, hence a statistical comparison could not be established in this study. In a study of 76 patients, it was found that the Ct values of severe cases remained considerably lower for the first 12 d following commencement as compared to moderate instances[24].
Early in the disease course, Pan et al[25] observed a lot of ground-glass opacity abnormalities followed by the development of crazy paving patterns on chest CT and finally increasing consolidation later on. According to study outcomes, chest CT has a high specificity but a low sensitivity, particularly in patients who appear within the first 4 d of the sickness. The clinical value of chest CT was observed to be limited in a review article, particularly for individuals who have no symptoms and are screened early in the disease progression[26]. The inverse relationship between viral load and chest CT TSS was the most striking finding. In hospitalized patients and outpatients with extensive lesions on CT, the viral load of nasopharyngeal samples was considerably lower. The severity of a CT scan was related to the patient's age and older patients having higher severity scores (P < 0.01). Hospitalization was related to the presence of any kind and number of comorbidities, but not to CT severity. Patients with obesity or other metabolic syndromes like diabetes mellitus still have a competent immunity which may be malfunctioning due to overnutrition. When these patients are infected by the SARS-CoV-2 virus, the infection may trigger hyper inflammation which makes a lot of collateral damage to all organs (those who were not infected by the virus) in the body. So, the COVID-19 disease can be very severe or even the quick demise of the patient, even if their competent immune system is able to clear the SARS-CoV-2 viruses effectively.
Even if the viral load of SARS CoV-2 in nasopharyngeal swab specimens is high in the early stages of COVID-19, it is not always related to changes in chest CT. The viral load of nasopharyngeal swab specimens decreases as SARS CoV-2 progresses but the viral load of lower respiratory tract samples increases and chest CT changes become more visible. It's thought that viral load is vital for recognizing early stages of Covid-19 infection and limiting transmission but CT can only help identify cases that require substantial medical care.
Patients who died had lower average Ct values across multiple time points during the disease course than those who recovered or were still hospitalized at the end of the study [recovered: median 37.43 (IQR 34.94-38.67); still hospitalized: median 36.97 (IQR 34.33-38.70); deceased: median 34.79 (IQR 24.46-37.65); P = 0.001] in a study of 308 patients from China. A study reported on the link between mortality and SARS-Cov-2 Ct values and found that lower Ct values were associated with a higher risk of death which is consistent with previous results regarding epidemic-causing coronaviruses[27,28]. C-reactive protein levels were shown to be adversely linked with Ct value in a study of 12 patients (r = -0.584; P = 0.03), but not in a study of 25 patients (P = 0.07)[29].
Several studies have reported the relationship between viral load as determined by Ct values and disease severity, and one of them (including 96 patients) found that higher viral loads were significantly related with more severe disease (Table 2)[30]. Mean viral loads were not significantly different between patients with pneumonia, severe pneumonia and those without pneumonia in a study by Shi et al[31]. Patients with severe pneumonia had a significantly higher viral load than those without pneumonia but severity outcomes were not statistically significant in this study. Shah et al[32] reported similar results in that there is no correlation between Ct values and severity of the disease.
With a CFR of 21.1%, this study reveals the significant rates of mortality in COVID-19 cancer patients. When comparing older cancer patients to younger cancer patients, mortality rates are not higher. Patients who had high baseline HRCT values at presentation and required ICU care had a higher mortality.
The lack of correlation data between coronavirus disease 2019 (COVID-19) and Solid malignancy limits the understanding of the true mortality impact of the COVID-19 in the Indian settings.
Higher incidence of serious clinical events and intensive care unit (ICU) admissions in cancer patients. Analysis suggests patients have increased morbidity and mortality from recent cytotoxic chemotherapy. Patients with active untreated cancer, metastatic disease, progressive disease with multiple co-morbidity and getting palliative treatment are at a higher risk of mortality.
The primary objectives of the study include COVID-19 related mortality outcomes within 30 d of diagnosis with HRCT score and RT-PCR Ct value-based viral load in various solid malignancies.
This is a single-center, retrospective study conducted at a tertiary cancer care hospital including confirmed COVID-19 in a diagnosed case of solid malignancy. The primary endpoint was to measure mortality within 30 d of diagnosis of COVID-19 with HRCT score and RT-PCR Ct value-based viral load.
The risk of death was statistically significant with the presence of symptomatic presentation, number of comorbidities ≥ 2 vs none, Eastern Cooperative Oncology Group performance status of 0/1 v/s ≥ 2. The odds ratio of mortality were significantly higher in patients presented with moderate and severe HRCT scores as compared to patients with mild HRCT scores. No statistically significant association of 30-d mortality was found concerning age, sex, type of malignancy, type of anticancer therapy, obesity status, recent surgery and active cancer (progressing vs remission). Also, no significant effect on mortality was noted for the patients with RT PCR based on different viral load levels.
Mortality rates are higher in patients with high baseline HRCT values at presentation and who need longer ICU stays. Mortality rates are not higher in older cancer patients as compared to younger counterparts with cancer. Mortality rates are not statistically significant in co-relation with high baseline RT-PCR based viral load values at presentation.
If there are further COVID-19 outbreaks, the findings of these studies will be helpful for clinical practice to categorize the patients on the basis of various demographic and clinical parameters for prognostication of patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: European Society for Medical Oncology.
Specialty type: Oncology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Phiri P, United Kingdom; Yu L, Singapore S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol. 2020;92:401-402. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1670] [Cited by in F6Publishing: 1693] [Article Influence: 423.3] [Reference Citation Analysis (0)] |
| 2. | Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565-574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7915] [Cited by in F6Publishing: 7190] [Article Influence: 1797.5] [Reference Citation Analysis (0)] |
| 3. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18987] [Cited by in F6Publishing: 16549] [Article Influence: 4137.3] [Reference Citation Analysis (0)] |
| 4. | Richman DD, Whitley RJ, Hayden FG, eds. Clinical virology, 4th edn Washington: ASM Press; 2016. [DOI] [Cited in This Article: ] |
| 5. | World Health Organization. WHO time-line COVID19 [Internet]. 2021 [cited 2021 Sept 12] Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. [Cited in This Article: ] |
| 6. | Johns Hopkins University. COVID-19 Dashboard [Internet]. 2021 [cited 2021 Oct 17] Available from: https://coronavirus.jhu.edu/map.html. [Cited in This Article: ] |
| 7. | Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2695] [Cited by in F6Publishing: 2980] [Article Influence: 745.0] [Reference Citation Analysis (0)] |
| 8. | Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, Zhang Z, You H, Wu M, Zheng Q, Xiong Y, Xiong H, Wang C, Chen C, Xiong F, Zhang Y, Peng Y, Ge S, Zhen B, Yu T, Wang L, Wang H, Liu Y, Chen Y, Mei J, Gao X, Li Z, Gan L, He C, Shi Y, Qi Y, Yang J, Tenen DG, Chai L, Mucci LA, Santillana M, Cai H. Patients with Cancer Appear More Vulnerable to SARS-CoV-2: A Multicenter Study during the COVID-19 Outbreak. Cancer Discov. 2020;10:783-791. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1142] [Cited by in F6Publishing: 890] [Article Influence: 222.5] [Reference Citation Analysis (0)] |
| 9. | Miyashita H, Mikami T, Chopra N, Yamada T, Chernyavsky S, Rizk D, Cruz C. Do patients with cancer have a poorer prognosis of COVID-19? Ann Oncol. 2020;31:1088-1089. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 257] [Cited by in F6Publishing: 286] [Article Influence: 71.5] [Reference Citation Analysis (0)] |
| 10. | Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020;323:1775-1776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1653] [Cited by in F6Publishing: 2082] [Article Influence: 520.5] [Reference Citation Analysis (0)] |
| 11. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11409] [Cited by in F6Publishing: 10969] [Article Influence: 2742.3] [Reference Citation Analysis (0)] |
| 12. | Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, Guo Y, Chen Y, Bian Z, Lancaster G, Sherliker P, Pang S, Wang H, Su H, Wu M, Wu X, Chen J, Collins R, Li L; China Kadoorie Biobank (CKB) collaborative group. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. 2015;386:1447-1456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 277] [Cited by in F6Publishing: 283] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 13. | Giefing-Kröll C, Berger P, Lepperdinger G, Grubeck-Loebenstein B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell. 2015;14:309-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 402] [Cited by in F6Publishing: 460] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 14. | Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16:626-638. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2321] [Cited by in F6Publishing: 3044] [Article Influence: 380.5] [Reference Citation Analysis (0)] |
| 15. | Humphries DL, Scott ME, Vermund SH. Pathways linking nutritional status and infectious disease. In: Humphries D, Scott ME, Vermund SH, editors. Nutrition and infectious disease: shifting the clinical paradigm: Humana Press; 2020: 4-5. [DOI] [Cited in This Article: ] |
| 16. | Levin BR, Antia R. Why we don't get sick: the within-host population dynamics of bacterial infections. Science. 2001;292:1112-1115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 80] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Couzin-Frankel J. A cancer survivor had the longest documented COVID-19 infection. Here's what scientists learned. SCIENCEINSIDER 2021. [DOI] [Cited in This Article: ] |
| 18. | Lee LY, Cazier JB, Angelis V, Arnold R, Bisht V, Campton NA, Chackathayil J, Cheng VW, Curley HM, Fittall MW, Freeman-Mills L, Gennatas S, Goel A, Hartley S, Hughes DJ, Kerr D, Lee AJ, Lee RJ, McGrath SE, Middleton CP, Murugaesu N, Newsom-Davis T, Okines AF, Olsson-Brown AC, Palles C, Pan Y, Pettengell R, Powles T, Protheroe EA, Purshouse K, Sharma-Oates A, Sivakumar S, Smith AJ, Starkey T, Turnbull CD, Várnai C, Yousaf N; UK Coronavirus Monitoring Project Team, Kerr R, Middleton G. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395:1919-1926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 805] [Cited by in F6Publishing: 781] [Article Influence: 195.3] [Reference Citation Analysis (0)] |
| 19. | Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, Shete S, Hsu CY, Desai A, de Lima Lopes G Jr, Grivas P, Painter CA, Peters S, Thompson MA, Bakouny Z, Batist G, Bekaii-Saab T, Bilen MA, Bouganim N, Larroya MB, Castellano D, Del Prete SA, Doroshow DB, Egan PC, Elkrief A, Farmakiotis D, Flora D, Galsky MD, Glover MJ, Griffiths EA, Gulati AP, Gupta S, Hafez N, Halfdanarson TR, Hawley JE, Hsu E, Kasi A, Khaki AR, Lemmon CA, Lewis C, Logan B, Masters T, McKay RR, Mesa RA, Morgans AK, Mulcahy MF, Panagiotou OA, Peddi P, Pennell NA, Reynolds K, Rosen LR, Rosovsky R, Salazar M, Schmidt A, Shah SA, Shaya JA, Steinharter J, Stockerl-Goldstein KE, Subbiah S, Vinh DC, Wehbe FH, Weissmann LB, Wu JT, Wulff-Burchfield E, Xie Z, Yeh A, Yu PP, Zhou AY, Zubiri L, Mishra S, Lyman GH, Rini BI, Warner JL; COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395:1907-1918. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1195] [Cited by in F6Publishing: 1193] [Article Influence: 298.3] [Reference Citation Analysis (0)] |
| 20. | Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A, Pradhan K, Thota R, Reissman S, Sparano JA, Gartrell BA, Smith RV, Ohri N, Garg M, Racine AD, Kalnicki S, Perez-Soler R, Halmos B, Verma A. Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020;10:935-941. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 493] [Cited by in F6Publishing: 550] [Article Influence: 137.5] [Reference Citation Analysis (0)] |
| 21. | Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259-260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1825] [Cited by in F6Publishing: 1965] [Article Influence: 491.3] [Reference Citation Analysis (0)] |
| 22. | Karahasan Yagci A, Sarinoglu RC, Bilgin H, Yanılmaz Ö, Sayın E, Deniz G, Guncu MM, Doyuk Z, Barıs C, Kuzan BN, Aslan B, Korten V, Cimsit C. Relationship of the cycle threshold values of SARS-CoV-2 polymerase chain reaction and total severity score of computerized tomography in patients with COVID 19. Int J Infect Dis. 2020;101:160-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 23. | Huang JT, Ran RX, Lv ZH, Feng LN, Ran CY, Tong YQ, Li D, Su HW, Zhu CL, Qiu SL, Yang J, Xiao MY, Liu MJ, Yang YT, Liu SM, Li Y. Chronological Changes of Viral Shedding in Adult Inpatients With COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71:2158-2166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 77] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 24. | Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, Wang Z, Li J, Feng C, Zhang Z, Wang L, Peng L, Chen L, Qin Y, Zhao D, Tan S, Yin L, Xu J, Zhou C, Jiang C, Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364-374. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1435] [Cited by in F6Publishing: 1302] [Article Influence: 325.5] [Reference Citation Analysis (0)] |
| 25. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295:715-721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1617] [Cited by in F6Publishing: 1665] [Article Influence: 416.3] [Reference Citation Analysis (0)] |
| 26. | Waller JV, Allen IE, Lin KK, Diaz MJ, Henry TS, Hope MD. The Limited Sensitivity of Chest Computed Tomography Relative to Reverse Transcription Polymerase Chain Reaction for Severe Acute Respiratory Syndrome Coronavirus-2 Infection: A Systematic Review on COVID-19 Diagnostics. Invest Radiol. 2020;55:754-761. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 27. | Rao SN, Manissero D, Steele VR, Pareja J. A Systematic Review of the Clinical Utility of Cycle Threshold Values in the Context of COVID-19. Infect Dis Ther. 2020;9:573-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 275] [Cited by in F6Publishing: 246] [Article Influence: 61.5] [Reference Citation Analysis (0)] |
| 28. | Feikin DR, Alraddadi B, Qutub M, Shabouni O, Curns A, Oboho IK, Tomczyk SM, Wolff B, Watson JT, Madani TA. Association of Higher MERS-CoV Virus Load with Severe Disease and Death, Saudi Arabia, 2014. Emerg Infect Dis. 2015;21:2029-2035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 29. | Azzi L, Carcano G, Gianfagna F, Grossi P, Gasperina DD, Genoni A, Fasano M, Sessa F, Tettamanti L, Carinci F, Maurino V, Rossi A, Tagliabue A, Baj A. Saliva is a reliable tool to detect SARS-CoV-2. J Infect. 2020;81:e45-e50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 512] [Cited by in F6Publishing: 422] [Article Influence: 105.5] [Reference Citation Analysis (0)] |
| 30. | Zheng S, Fan J, Yu F, Feng B, Lou B, Zou Q, Xie G, Lin S, Wang R, Yang X, Chen W, Wang Q, Zhang D, Liu Y, Gong R, Ma Z, Lu S, Xiao Y, Gu Y, Zhang J, Yao H, Xu K, Lu X, Wei G, Zhou J, Fang Q, Cai H, Qiu Y, Sheng J, Chen Y, Liang T. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. 2020;369:m1443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 935] [Cited by in F6Publishing: 963] [Article Influence: 240.8] [Reference Citation Analysis (0)] |
| 31. | Shi F, Wu T, Zhu X, Ge Y, Zeng X, Chi Y, Du X, Zhu L, Zhu F, Zhu B, Cui L, Wu B. Association of viral load with serum biomakers among COVID-19 cases. Virology. 2020;546:122-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 32. | Shah S, Singhal T, Davar N, Thakkar P. No correlation between Ct values and severity of disease or mortality in patients with COVID 19 disease. Indian J Med Microbiol. 2021;39:116-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |