Published online Oct 28, 2018. doi: 10.4329/wjr.v10.i10.135
Peer-review started: April 30, 2018
First decision: June 6, 2018
Revised: August 14, 2018
Accepted: October 8, 2018
Article in press: October 8, 2018
Published online: October 28, 2018
To determine the radiation dose and image quality in coronary computed tomography angiography (CCTA) using state-of-the-art dose reduction methods in unselected “real world” patients.
In this single-centre study, consecutive patients in sinus rhythm underwent CCTA for suspected coronary artery disease (CAD) using a 320-row detector CT scanner. All patients underwent the standard CT acquisition protocol at our institute (Morriston Hospital) a combination of dose saving advances including prospective electrocardiogram-gating, automated tube current modulation, tube voltage reduction, heart rate reduction, and the most recent novel adaptive iterative dose reconstruction 3D (AIDR3D) algorithm. The cohort comprised real-world patients for routine CCTA who were not selected on age, body mass index, or heart rate. Subjective image quality was graded on a 4-point scale (4 = excellent, 1 = non-diagnostic).
A total of 543 patients were included in the study with a mean body weight of 81 ± 18 kg and a pre-scan mean heart rate of 70 ± 11 beats per minute (bpm). When indicated, patients received rate-limiting medication with an oral beta-blocker followed by additional intravenous beta-blocker to achieve a heart rate below 65 bpm. The median effective radiation dose was 0.88 mSv (IQR, 0.6-1.4 mSv) derived from a Dose Length Product of 61.45 mGy.cm (IQR, 42.86-100.00 mGy.cm). This also includes what we believe to be the lowest ever-reported radiation dose for a routine clinical CCTA (0.18 mSv). The mean image quality (± SD) was 3.65 ± 0.61, with a subjective image quality score of 3 (“good”) or above for 93% of patient CCTAs.
Combining a low-dose scan protocol and AIDR3D with a 320-detector row CT scanner can provide high quality images at exceptionally low radiation dose in unselected patients being investigated for CAD.
Core tip: Coronary computed tomography angiography (CCTA) is now widely used in the diagnosis of coronary artery disease since it is a rapid, minimally invasive test with high diagnostic accuracy. To meet the demands for increasing spatial and temporal resolution of CT images, a number of dose saving algorithms have been implemented to CCTA to minimise radiation exposure to “as low as reasonably achievable” without compromising diagnostic image quality. This study demonstrates that advances in CT scanner hardware and reconstruction software allow ultra-low dose of radiation with high image quality in routine clinical examination of real-world patients.
- Citation: Richards CE, Dorman S, John P, Davies A, Evans S, Ninan T, Martin D, Kannoly S, Roberts-Davies G, Ramsey M, Obaid DR. Low-radiation and high image quality coronary computed tomography angiography in “real-world” unselected patients. World J Radiol 2018; 10(10): 135-142
- URL: https://www.wjgnet.com/1949-8470/full/v10/i10/135.htm
- DOI: https://dx.doi.org/10.4329/wjr.v10.i10.135
Coronary computed tomography angiography (CCTA) is increasingly being used in the diagnosis of coronary artery disease (CAD) since it is rapid and minimally invasive[1,2]. However, the high radiation doses[3] previously required for optimising the image signal-to-noise ratio in CCTA were a major healthcare concern due to an associated increase in lifetime risk of radiation-induced malignancy[4]. CCTA has thus been a driving force behind a number of dose reduction strategies to pursue radiation exposure to “as low as reasonably achievable” (ALARA) without compromising image quality[5].
Sub-millisievert CCTA was initially proven feasible in 2009 using dual-source CT with prospectively electrocardiogram (ECG)-triggered high-pitch spiral acquisition[6], and doses as low as 0.06 mSv have been reported using this technique with a combination of iterative reconstruction (IR) and reduced tube voltage[7]. However, these were conducted on highly selected populations with low body weight and heart rate. We prospectively analyzed the radiation exposure and image quality in consecutive unselected patients undergoing CCTA for suspected coronary disease with a 320-detector row CT scanner and IR, and active reduction of tube voltage, exposure window, and volume coverage.
This is a prospective single-centre study of 549 consecutive patients (age >18 years) who were referred to our institute between June 2012 and August 2016 to undergo CCTA for suspected CAD. Patients were excluded if they were undergoing cardiac CT for other indications (e.g., assessment for trans-catheter aortic valve replacement or atrial fibrillation ablation). Patients were not pre-selected according to age, heart rate or body mass index (BMI).
All examinations were performed on a 320-slice CT scanner with 320 mm × 0.5 mm detector rows giving z-axis coverage of 160 mm (Aquilion One, Toshiba Medical Systems, Japan). After acquisition of scout images, prospective ECG-gated CCTA was performed using half-segment reconstruction and a 350 ms rotation time. Scanning field of view was selected based on scout images using volume sizes of 100-160 mm and radiographer led to be the smallest possible that included the area of clinical interest (20 mm below carina to base of heart). Iodinated contrast media-75 mL of Iohexol (Omnipaque 300 if BMI < 30 kg/m2), (Omnipaque 350 if BMI > 30 kg/m2)-was injected in a biphasic protocol at 5 mL/s triggered by bolus tracking.
The Sure Cardio Prospective Package was used to reduce the exposure window depending on heart rate. For patients with a heart rate below 65 bpm, images were acquired with an acquisition window of 70%-80% of the interval between two consecutive QRS complexes. If patients had a heart rate below 60 bpm the acquisition window could be reduced further at the radiographer’s discretion. Tube current and voltage were also minimised according to each patient’s BMI and density, using the Sure Exposure 3D (SUREexposure, Toshiba Medical Systems, Japan) with an automatic exposure control system.
Unless contraindicated, patients received rate-limiting medication as required with an oral beta-blocker (atenolol 25 mg) followed by additional intravenous beta-blocker (metoprolol 5-25 mg) aiming for a heart rate below 65 bpm. All patients also received sublingual glyceryl trinitrate (300 μg).
The effective radiation dose for each patient was derived by multiplying the dose-length product (DLP), recorded from the CT scanner, by the conversion factor 0.014 mSv mGy-1 cm-1, according to guidelines from the International Commission on Radiological Protection[8]. The effective radiation dose can then be compared to the lowest mean effective doses recorded in literature. In patients with repeated coronary CT angiography scans, the cumulative DLP and the cumulative effective dose were included in the analysis.
Images were reconstructed with a section thickness of 0.5 mm and an increment of 0.25 mm using the Adaptive Iterative Dose Reconstruction 3D (AIDR3D) algorithm. CCTA images were analyzed on a dedicated post-processing workstation by two trained observers. Subjective image quality was assessed by the two trained observers and scored on a four-point scale (4 = excellent, 1 = non-diagnostic). If any patients went on to undergo invasive coronary angiography then the accuracy of CCTA in determining the presence of significant coronary disease (stenosis > 50%) compared with the gold standard of invasive angiography was recorded.
CT data from a total of 543 consecutive patients who underwent CCTA for suspected CAD were assessed. A total of six patients were excluded from the evaluation due to failure to perform CCTA; four patients due to an inability to obtain intravenous access and two patients from incomplete dose data.
Table 1 summarises the characteristics of the 543 patients included in the final analysis. The mean age was 56 ± 11 years; and 33% were male. The mean body weight was 81 ± 18 kg and mean heart rate was 70 ± 11 bpm. Additional IV metoprolol was required in 47% of the scans. The presence of CAD was confirmed by CCTA in 57 (10%) of patients.
| Parameter | n (%) | |
| Number of patients | 543 | |
| Age (yr) | 56 ± 11 | |
| Gender | Male/Female (33%/67%) | |
| Mean weight (kg) | 81 ± 181 | |
| Mean heart rate (bpm) | 70.3 ± 11.4 | |
| Oral Beta-blocker | 204 (38) | |
| IV Beta-blocker | 255 (47) | |
| Heart rate during scan (bpm) | < 60 bpm | 349 (64) |
| 60-65 bpm | 112 (21) | |
| 65-75 bpm | 55 (10) | |
| > 75 bpm | 18 (3) | |
| Not recorded | 11 (2) | |
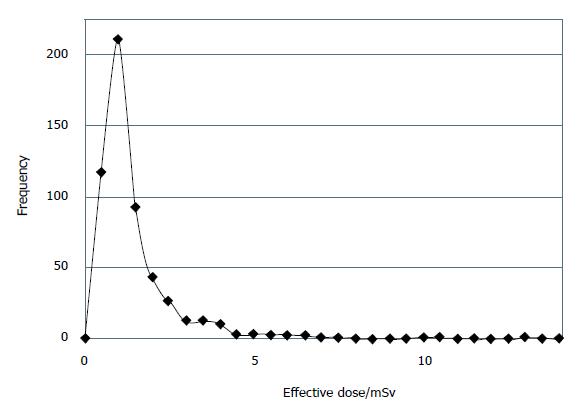
The median DLP for all 543 patients was 61.45 mGy.cm (IQR, 42.86-100.00 mGy.cm) corresponding to a median effective dose of 0.88 mSv (IQR, 0.6-1.4 mSv). A total of 23 scans were repeated and whose cumulative radiation doses were thus included in the final median dose value. The frequency of the per-patient radiation dose, plotted in Figure 1, indicates a high positive skew with a Pearson coefficient of 3.26 from the normal distribution. This further demonstrates that the majority of patients received a very low dose of radiation and those that received a high dose were few in number.
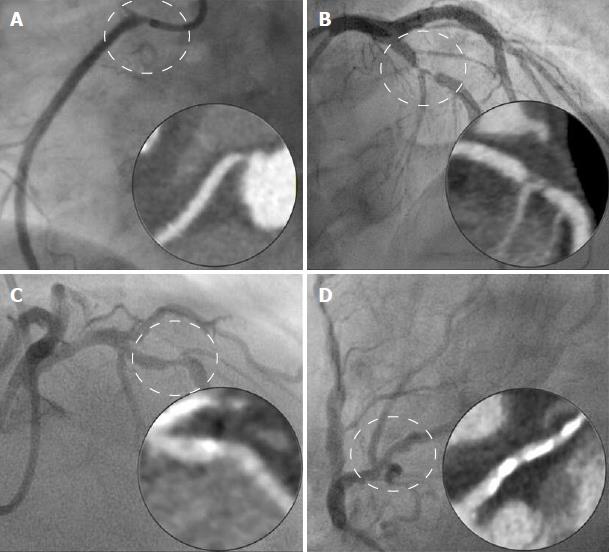
A total of 328 (56%) patients received an effective dose < 1 mSv, 409 patients (75%) received an effective dose < 1.5 mSv. Moreover, we believe we have demonstrated the lowest ever-recorded effective dose for a CCTA performed in routine clinical practice of 0.18 mSv with a subjective image quality score of 4 (Figure 2).
The mean image quality (± SD) for all 543 scans was 3.65 ± 0.61 with a corresponding score breakdown; excellent 392 (72%), good 118 (22%), poor but usable 30 (5%), and poor 3 (1%). We compared the patient characteristics of the excellent and good scans (image quality score 3 + 4) with those that were poor and unusable (image quality score 1 + 2). There was no difference in mean age or sex between the groups. However, compared with excellent and good scans, poor and unusable scans were more likely to occur in patients with heart rates > 65 bpm (31% vs 9%, P < 0.0001) and require a higher effective dose (1.98 ± 1.69 vs 1.24 ± 1.41, P = 0.0041) (Table 2).
| Image quality score 1 + 2 | Image quality Score 3 + 4 | P value | |
| Female patient | 12/30 (63%) | 216/391 (67%) | P = 0.1068 |
| Mean age ± SD (years) | 57.5 ± 10.5 | 55.5 ± 10.6 | P = 0.2979 |
| No. of patients with | 22 (69%) | 457 (91%) | P < 0.0001 |
| heart rate ≤ 65 bpm | |||
| No. of patients with | 10 (31%) | 43 (9%) | P < 0.0001 |
| heart rate > 65 bpm | |||
| Effective dose ± SD (mSv) | 1.98 ± 1.69 | 1.24 ± 1.41 | P = 0.0041 |
Twenty-one of the patients underwent invasive coronary angiography in addition to CCTA yielding 84 coronary arteries for comparison (21 left main stem, 21 left anterior descending, 21 left circumflex and 21 right coronary artery). CCTA correctly identified a significant (> 50%) stenosis in 16/17 coronary arteries and correctly excluded significant stenosis in 62/67 coronary arteries. This gave CCTA a sensitivity of 94%, specificity 93%, negative predictive value 98% and positive predictive value 76% to identify a significantly (> 50%) stenosis coronary artery in comparison with the gold standard of invasive angiography. Examples of correct and incorrect CCTA classifications are provided in Figure 3.
We analyzed the CCTA data of 543 unselected consecutive patients with suspected CAD. The median effective radiation dose was 0.88 mSv (IQR, 0.6-1.4 mSv) with diagnostic image quality in 99% of patients, verifying that sub-millisievert radiation doses are possible in unselected, real-world patients undergoing CCTA.
A number of integrated strategies were used to achieve this consistently low dose, including; prospective ECG-gated acquisition, lowest possible tube current and voltage, IR (AIDR3D image reconstruction algorithm) and meticulous attention to patient preparation, both pre scan (heart rate control) and during the scan (reduction in volume of coverage to minimal size possible whilst allowing complete acquisition in a single volume.
Prospective ECG-gated tube current modulation is reported to be one of the most effective methods at reducing the radiation dose. Unlike traditional retrospective-gating, where data are acquired over the whole heart phase, in prospective gating the X-ray tube is switched on only at predefined time-points of the cardiac cycle. In their systematic review, Menke et al[9] confirmed a pooled effective dose of 3.5 mSv with prospective gating, a factor of 3.5 lower than the pooled effective dose of 12.3 mSv with retrospective gating.
Radiation dose increases with the square of the tube voltage at a constant tube current, reducing the tube voltage further lowers radiation exposure[10]. Tube current and voltage were minimised to each patient’s BMI and density, using the Sure Exposure 3D (SUREExposure, Toshiba Medical Systems, Japan) with an automatic exposure control system which reduces tube current and voltage on the basis of scout images and the reconstruction kernel[11].
However, dose reduction by lowering tube voltage and current causes a substantial increase in noise, especially in obese patients[12]. To overcome these limitations and allow further dose reduction, new IR algorithms represent another milestone in CCTA[13]. IR algorithms adaptively apply noise correction at a reduced X-ray exposure without compromising spatial resolution[14]. AIDR and more recently 3D AIDR (AIDR3D) decreases image noise thus allowing for reductions in tube current while preserving overall image quality[15]. BMI-adapted tube voltage and current work synergistically with AIDR3D to reduce image noise while achieving a 75% radiation dose reduction relative to a scan reconstructed with filtered back-projection[16].
Patient irradiation is further limited by decreasing the craniocaudal field of view to the minimum required following analysis of the scout view[17]. The wide area detector row CT scanner can be used with less than the maximum 16 cm (320-detector) craniocaudal coverage. For example, imaging over a 14 cm (280 detectors) craniocaudal field of view will decrease patient dose by 12.5% and is proven sufficient for most patients[18].
The radiation dose with the 320-detector CT scanner is significantly lower if data acquisition occurs as a single volume[19]. To facilitate this we were judicious in our use of beta-blockers to slow the resting heart rate. Lowering the heart rate with beta-blockers has previously shown to be a safe practice[20], reducing radiation exposure and improving image quality[21]. We achieved comparable X-ray doses in our real world population to Chen et al[19] using a 320-detector CT scanner despite a slower gantry rotation speed ( 350 ms vs 275 ms due to the aggressive measures to control heart rate, with 65% of patients receiving betablockers [either oral only (15%), iv only (27%) or both (23%)] and 85% of patients achieving a heart rate < 65 bpm. Moreover, we have demonstrated what we believe is the lowest ever-recorded effective dose of 0.18 mSv with a subjective image quality score of 4 (“excellent”) from a study of real-world unselected patients. This ultra-low radiation dose for CCTA is comparable to the radiation range reported for a chest X-ray in two views[22]. Advances in radiation dose reduction without compromising image quality justify the use of CCTA as a non-invasive alternative to coronary catheterization in investigating appropriate populations for CAD[23].
The prospective ECG-gated single volume acquisition with AIDR-3D protocol we use at our institution is not the only potential strategy for very low dose CCTA. Another contemporary strategy is Prospective ECG-triggered high-pitch spiral acquisition which also allows the entire heart to be scanned within one single cardiac cycle thus significantly lowering the radiation dose[24-26]. This coupled with IR techniques have shown ultra-low mean effective radiation doses ranging from 0.06 mSv to 0.3 mSv with clinically acceptable diagnostic images[7,27]. While demonstrating the feasibility of ultra-low dose CCTA, these studies were limited to carefully selected patents with a low and regular heart rate (< 60 bpm) and a body weight of less than 100 kg. Other IR algorithms are also in use including Model-based IR (MBIR, GE Healthcare, Waukesha, Wisconsin) which has also shown promising results for noise reduction in very-low-dose CCTA[22]. iDose4 and iterative model reconstruction are alternative IR algorithms released by Philips Healthcare (Philips Healthcare, Best, the Netherlands) that have also maintained image quality at 80% lower radiation exposure[13].
Our study has some limitations. Whilst we included all consecutive patients undergoing CCTA for the evaluation of suspected CAD we did not include cardiac CT performed for other indications such as evaluation of coronary bypass grafts, evaluation of left atrium anatomy prior to atrial fibrillation ablation, pre-operative assessment for trans-catheter aortic valve replacement or assessment of cardiac function so the same low doses may not be achieved in these patient groups. In addition, patients in atrial fibrillation were not included and whilst the patients were not selected on the basis of body weight, body mass index was not recorded and actual weight measurements were only available for 32% of the patients meaning the effect of patient weight on dose could not be investigated in this study. In view of this, the results may not be generalizable to patients who are overweight or in atrial fibrillation.
The image quality score used is a subjective assessment and was performed by the authors. Whilst the results of patients who underwent invasive coronary angiography are included, the proportion is relatively small and a more robust assessment of image adequacy would have been obtained if all patients had undergone the gold standard of invasive angiography.
Finally, the conversion factor to determine effective radiation dose equivalents has been a point of controversy[28]. Previous ICRP conversion factors for the chest have varied from 0.012-0.026 mSv mGy-1 cm-1 potentially yielding even lower radiation estimates[29].
We report a series of over 500 CCTAs performed at our health board with excellent image quality and median effective dose of 0.88 mSv. This includes the lowest ever-reported radiation dose for a routine clinical CCTA (0.18 mSv). We have demonstrated that provided patients are in sinus rhythm and with the judicious use of beta blockers to achieve heart rates < 65 bpm a combination of low-dose CCTA scan protocol and AIDR3D with a 320-detector row CT scanner can provide high quality images at exceptionally low radiation dose in patients being investigated for CAD.
Traditionally, coronary angiography has been the gold standard in diagnosing coronary artery disease (CAD). Coronary computed tomography angiography (CCTA), however, is increasingly being used as a rapid and less invasive alternative in diagnosing patients at risk of CAD. A 3D image of the heart and coronary circulation can be rendered with a CT scanner using only an intravenous injection of iodine-rich contrast, thus circumventing the need for insertion of a catheter via an artery of vein. However, imaging coronary arteries presents increased challenges, since it requires both a high temporal resolution to reduce motion artifacts caused by cardiac motion and a high spatial resolution to differentiate small coronary structures. While images obtained with CCTA scanners are now comparable to coronary angiography these CT requirements have previously resulted in higher radiation doses thus increasing the lifetime risk of radiation-induced malignancy. Advances in CCTA scanner hardware and image reconstruction techniques have led to reports of exceptionally low radiation doses, down to 0.06 mSv, while maintaining diagnostic image quality of the coronary arteries. For example, in prospective electrocardiogram-gated acquisition the X-ray tube is switched on only for a reduced percentage of the cardiac cycle rather than the whole cycle. Automatic exposure control uses the lowest possible CT tube current and voltage adjusted to the patient’s body habitus. This works in synergy with novel image IR algorithms that adaptively apply noise correction to offset an increase in image noise caused by a reduced tube voltage. Using pharmacological methods to reduce heart rate, with oral or intravenous beta-blockers, has proven to reduce cardiac motion during the acquisition leading to improved images. An initial scout view of the thorax can also be used to minimize the volume covered per-patient in a single complete acquisition to further reduce the radiation. However, these previous studies were conducted on small cohorts that were pre-selected for low body weight and heart rate, and were limited by a low prevalence of CAD. The feasibility and effect of these low-dose scan modes on both image quality and radiation exposure in a large patient population with various heart rates is currently unknown. In this study, we determined the radiation dose and subjective image quality using a combination of state-of-the-art CCTA acquisition protocols at our institution in consecutive unselected patients undergoing CCTA for suspected coronary disease.
Ultra-low radiation doses of less than one mSv have been reported in other feasibility studies. While these advances in cardiac CT may effectively lower radiation dose, these studies are limited to small cohorts of pre-selected patients with very low and regular heart rates and low body habitus and are thus not representative of the typical population undergoing screening for CAD. This study aims to determine the feasibility of these low-dose CCTA acquisition protocols adopted at our institution in an unselected cohort from a series of consecutive patients who underwent CCTA for suspected CAD. We hope that the outcome may demonstrate that CCTA is a viable, non-invasive alternative to coronary catheterization for screening low-risk populations with suspected CAD.
The primary end points of the study were effective radiation dose and image quality in patients not selected in term of heart rate and body habitus undergoing routine CCTA. Our objective was to demonstrate that low radiation doses were feasible for the majority of real-world patients undergoing routine screening for CAD with CCTA without losing diagnostic image quality.
The radiation dose and subjective image quality were analysed over a total of 543 consecutive patients in sinus rhythm who underwent CCTA at our institute for suspected CAD between June 2012 and August 2016. Subjective image quality was assessed by the two trained observers and scored on a four-point scale (4 = excellent, 1 = non-diagnostic). Images were acquired with a 320-row detector CT scanner (Aquilion One, Toshiba Medical Systems, Japan) and a number of integrated packages that have been developed to reduce the radiation dose to as low as reasonably achievable. Prospective electrocardiogram (ECG)-gated acquisition was implemented using the SURE Cardio Prospective Package over an acquisition window of 70%–80% of the interval between two consecutive QRS complexes in ppatients with a heart rate below 65 bpm. The Sure Exposure 3D package (SUREexposure, Toshiba Medical Systems, Japan) automatically adjusted to the lowest possible tube current and voltage in accordance with each patient’s attenuation profile while noise reduction during each acquisition was implemented with the three-dimensional adaptive iterative dose reduction (AIDR-3D) image reconstruction algorithm. If necessary, patients were prepared prior to the scan with rate-limiting oral beta-blockers followed by additional intravenous beta-blocker to achieve a heart rate below 65 bpm unless contraindicated. During the scan, the volume of coverage was reduced to minimal size whilst allowing complete acquisition in a single volume. Contrary to previous studies in which the patients were prospectively selected, the patients were not selected based on age, heart rate, and body mass index. We believe that this is a better representation of real world patients who would be undergoing routine CCTA for diagnosis of CAD.
The median effective radiation dose was 0.88 mSv, which includes what we believe to be the lowest ever-reported radiation dose for a routine clinical CCTA (0.18 mSv). The mean image quality (± SD) was 3.65 ± 0.61, with a subjective image quality score of 3 (“good”) or above for 93% of patient CCTAs. CAD was confirmed by CCTA in 57 (10%) of patients.
The median effective radiation dose was 0.88 mSv (IQR, 0.6-1.4 mSv) with a mean subjective image quality score (± SD) of 3.65 ± 0.61 averaged over 500 real-world unselected patients undergoing routine clinical CCTA. This ultra-low radiation dose for CCTA is comparable to the radiation range reported for a chest X-ray in two views. The data also includes what we believe to be the lowest ever-reported radiation dose for a routine clinical CCTA 0.18 mSv with a subjective image quality score of 4 (“excellent”). This demonstrates that low radiation dose CCTA can be used as a routine clinical screening tool for CAD without loss of diagnostic image quality. To date, radiation dose reduction advances in CCTA technology have only been reported in feasibility studies on small cohorts of highly selected patients with low body habitus and heart rate. This study demonstrates that low radiation CCTA with good image quality is possible for most patients undergoing routine screening for CAD with CCTA using a combination of commercially available, state-of-the-art cardiac CT technology advances. CCTA is rapid and non-invasive compared with coronary angiography and has reduced patient recovery time. The reduced risk in radiation-induced malignancy implies that CCTA is a feasible alternative to coronary angiography as a primary screening tool for patients with low risk CAD.
This study did not include patients with atrial fibrillation or other cardiac CT indications such as evaluation of coronary bypass grafts, evaluation of left atrium anatomy prior to atrial fibrillation ablation, pre-operative assessment for trans-catheter aortic valve replacement or assessment of cardiac function. Feasibility studies with alternative dose-saving strategies have also recorded ultra-low mean effective radiation doses ranging from 0.06 mSv to 0.3 mSv with clinically acceptable diagnostic images. These include techniques such as prospective ECG-triggered high-pitch spiral acquisition but again were limited to carefully selected patients. Extending these techniques to unselected patients could highlight the need for alternative protocols for undertaking routine CCTA for assessment of different patient groups or to incorporate existing technology at other institutions.
STROBE Statement: The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Bazeed MF, Pastromas S, Stavroulopoulos A S- Editor: Wang JL L- Editor: A E- Editor: Tan WW
| 1. | Salavati A, Radmanesh F, Heidari K, Dwamena BA, Kelly AM, Cronin P. Dual-source computed tomography angiography for diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. J Cardiovasc Comput Tomogr. 2012;6:78-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Haberl R, Tittus J, Böhme E, Czernik A, Richartz BM, Buck J, Steinbigler P. Multislice spiral computed tomographic angiography of coronary arteries in patients with suspected coronary artery disease: an effective filter before catheter angiography? Am Heart J. 2005;149:1112-1119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, McCollough C, Martinoff S, Kastrati A, Schömig A. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500-507. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 776] [Cited by in F6Publishing: 730] [Article Influence: 48.7] [Reference Citation Analysis (0)] |
| 4. | Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298:317-323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1081] [Cited by in F6Publishing: 976] [Article Influence: 57.4] [Reference Citation Analysis (0)] |
| 5. | Halliburton SS, Abbara S, Chen MY, Gentry R, Mahesh M, Raff GL, Shaw LJ, Hausleiter J; Society of Cardiovascular Computed Tomography. SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr. 2011;5:198-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 370] [Cited by in F6Publishing: 312] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 6. | Lell M, Marwan M, Schepis T, Pflederer T, Anders K, Flohr T, Allmendinger T, Kalender W, Ertel D, Thierfelder C. Prospectively ECG-triggered high-pitch spiral acquisition for coronary CT angiography using dual source CT: technique and initial experience. Eur Radiol. 2009;19:2576-2583. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 7. | Schuhbaeck A, Achenbach S, Layritz C, Eisentopf J, Hecker F, Pflederer T, Gauss S, Rixe J, Kalender W, Daniel WG. Image quality of ultra-low radiation exposure coronary CT angiography with an effective dose < 0.1 mSv using high-pitch spiral acquisition and raw data-based iterative reconstruction. Eur Radiol. 2013;23:597-606. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 111] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Kalender WA, Schmidt B, Zankl M, Schmidt M. A PC program for estimating organ dose and effective dose values in computed tomography. Eur Radiol. 1999;9:555-562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 177] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Menke J, Unterberg-Buchwald C, Staab W, Sohns JM, Seif Amir Hosseini A, Schwarz A. Head-to-head comparison of prospectively triggered vs retrospectively gated coronary computed tomography angiography: Meta-analysis of diagnostic accuracy, image quality, and radiation dose. Am Heart J. 2013;165:154-163.e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Sabarudin A, Sun Z. Coronary CT angiography: Dose reduction strategies. World J Cardiol. 2013;5:465-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Sasdelli Neto R, Nomura CH, Macedo AC, Bianco DP, Kay FU, Szarf G, Teles GB, Shoji H, Santana Netto PV, Passos RB. Coronary computed tomography angiography with 320-row detector and using the AIDR-3D: initial experience. Einstein (Sao Paulo). 2013;11:400-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Xu L, Zhang Z. Coronary CT angiography with low radiation dose. Int J Cardiovasc Imaging. 2010;26 Suppl 1:17-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Naoum C, Blanke P, Leipsic J. Iterative reconstruction in cardiac CT. J Cardiovasc Comput Tomogr. 2015;9:255-263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Padole A, Ali Khawaja RD, Kalra MK, Singh S. CT radiation dose and iterative reconstruction techniques. AJR Am J Roentgenol. 2015;204:W384-W392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 15. | Shen H, Dai G, Luo M, Duan C, Cai W, Liang D, Wang X, Zhu D, Li W, Qiu J. Image Quality and Radiation Dose of CT Coronary Angiography with Automatic Tube Current Modulation and Strong Adaptive Iterative Dose Reduction Three-Dimensional (AIDR3D). PLoS One. 2015;10:e0142185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Williams MC, Weir NW, Mirsadraee S, Millar F, Baird A, Minns F, Uren NG, McKillop G, Bull RK, van Beek EJ. Iterative reconstruction and individualized automatic tube current selection reduce radiation dose while maintaining image quality in 320-multidetector computed tomography coronary angiography. Clin Radiol. 2013;68:e570-e577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Maurer MH, Hamm B, Huppertz A, Lembcke A. Ultra-low-dose dual-source CT coronary angiography with high pitch: diagnostic yield of a volumetric planning scan and effects on dose reduction and imaging strategy. Br J Radiol. 2015;88:20140602. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Rybicki FJ, Otero HJ, Steigner ML, Vorobiof G, Nallamshetty L, Mitsouras D, Ersoy H, Mather RT, Judy PF, Cai T. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging. 2008;24:535-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 459] [Cited by in F6Publishing: 385] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 19. | Chen MY, Shanbhag SM, Arai AE. Submillisievert median radiation dose for coronary angiography with a second-generation 320-detector row CT scanner in 107 consecutive patients. Radiology. 2013;267:76-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 20. | Roberts WT, Wright AR, Timmis JB, Timmis AD. Safety and efficacy of a rate control protocol for cardiac CT. Br J Radiol. 2009;82:267-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Dewey M, Vavere AL, Arbab-Zadeh A, Miller JM, Sara L, Cox C, Gottlieb I, Yoshioka K, Paul N, Hoe J. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 Multicenter International Trial. AJR Am J Roentgenol. 2010;194:93-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 22. | Stehli J, Fuchs TA, Bull S, Clerc OF, Possner M, Buechel RR, Gaemperli O, Kaufmann PA. Accuracy of coronary CT angiography using a submillisievert fraction of radiation exposure: comparison with invasive coronary angiography. J Am Coll Cardiol. 2014;64:772-780. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 23. | Moscariello A, Takx RA, Schoepf UJ, Renker M, Zwerner PL, O'Brien TX, Allmendinger T, Vogt S, Schmidt B, Savino G. Coronary CT angiography: image quality, diagnostic accuracy, and potential for radiation dose reduction using a novel iterative image reconstruction technique-comparison with traditional filtered back projection. Eur Radiol. 2011;21:2130-2138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 231] [Cited by in F6Publishing: 232] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 24. | Alkadhi H, Stolzmann P, Desbiolles L, Baumueller S, Goetti R, Plass A, Scheffel H, Feuchtner G, Falk V, Marincek B. Low-dose, 128-slice, dual-source CT coronary angiography: accuracy and radiation dose of the high-pitch and the step-and-shoot mode. Heart. 2010;96:933-938. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 151] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 25. | Litmanovich DE, Tack DM, Shahrzad M, Bankier AA. Dose reduction in cardiothoracic CT: review of currently available methods. Radiographics. 2014;34:1469-1489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Achenbach S, Marwan M, Ropers D, Schepis T, Pflederer T, Anders K, Kuettner A, Daniel WG, Uder M, Lell MM. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010;31:340-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 457] [Cited by in F6Publishing: 475] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 27. | Hell MM, Bittner D, Schuhbaeck A, Muschiol G, Brand M, Lell M, Uder M, Achenbach S, Marwan M. Prospectively ECG-triggered high-pitch coronary angiography with third-generation dual-source CT at 70 kVp tube voltage: feasibility, image quality, radiation dose, and effect of iterative reconstruction. J Cardiovasc Comput Tomogr. 2014;8:418-425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 28. | Christner JA, Kofler JM, McCollough CH. Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting International Commission on Radiological Protection publication 103 or dual-energy scanning. AJR Am J Roentgenol. 2010;194:881-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 360] [Cited by in F6Publishing: 352] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 29. | Gosling O, Loader R, Venables P, Roobottom C, Rowles N, Bellenger N, Morgan-Hughes G. A comparison of radiation doses between state-of-the-art multislice CT coronary angiography with iterative reconstruction, multislice CT coronary angiography with standard filtered back-projection and invasive diagnostic coronary angiography. Heart. 2010;96:922-926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |