Published online May 26, 2013. doi: 10.4330/wjc.v5.i5.124
Revised: April 20, 2013
Accepted: April 28, 2013
Published online: May 26, 2013
AIM: To determine whether there are gender differences in the epidemiological profile of atrial fibrillation (AF) and to characterise the clinical, biochemical, and therapeutic factors associated with AF.
METHODS: Each investigator (primary care physicians or physicians based in hospital units for hypertension treatment) recruited the first 3 patients with an age of ≥ 65 years and a clinical diagnosis of hypertension (ambulatory blood pressure monitoring and an electrocardiogram, were performed) on the first working day of the week for 5 wk and identified those individuals with atrial fibrillation. A binary logistic regression was performed, including all of the variables that were significant in the univariate analysis, to establish the variables that were associated with the presence of arrhythmia.
RESULTS: A total of 1028 patients were included in the study, with a mean age of 72.8 ± 5.8 years. Of these patients, 47.3% were male, 9% were smokers, 27.6% were diabetics, 48.3% had dyslipidaemia, 10.9% had angina, and 6.5% had experienced a myocardial infarction. Regarding gender differences, the men exhibited a larger waist circumference, a lower body mass index, less obesity, and a more extensive history of diabetes, smoking, ischaemic heart disease, kidney failure, peripheral arterial disease and carotid disease than the women. There were no differences, however, in the prevalence of AF between the men and the women (11.5% vs 9.2%, respectively; P = no significant). Regarding treatment, the women received antiplatelet agents and diuretics less frequently, but there were no other differences in the use of antihypertensive and antithrombotic therapies. In the multivariate analysis, AF in the total study population was associated with age, alcohol consumption, the presence of heart disease, and decreased glomerular filtration. In the women, AF was associated with all of the factors included in the overall analysis, as well as the presence of left ventricle hypertrophy. In contrast, in the men, the only risk factors associated with AF were age, the presence of heart disease and alcohol consumption.
CONCLUSION: In patients with hypertension over 65 years of age, there are relevant gender differences in the factors associated with AF.
Core tip: The presence of atrial fibrillation (AF) in hypertensive patients with an age of ≥ 65 years was associated with age, alcohol consumption, the presence of heart disease, and decreased glomerular filtration. In women, AF was associated with all of the factors included in the overall analysis, as well as the presence of left ventricle hypertrophy, whereas in men, the only risk factors associated with AF were age, the presence of heart disease and alcohol consumption. Thus, in patients with hypertension who are over 65 years of age, there are relevant gender differences in the factors associated with AF.
- Citation: Fácila L, Pallarés V, Morillas P, Cordero A, Llisterri JL, Sánchis C, Gorriz JL, Castillo J, Gil V, Redon J. Gender differences related to the presence of atrial fibrillation in older hypertensive patients. World J Cardiol 2013; 5(5): 124-131
- URL: https://www.wjgnet.com/1949-8462/full/v5/i5/124.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i5.124
Although cardiovascular disease (CVD) has historically been considered to affect mainly men, we now know that CVD is the main cause of death in both men and women worldwide[1]. However, a number of occasionally significant gender differences can be observed in the morbidity, mortality, risk-factor profiles, and clinical presentation of CVD. These differences are consistent between all of the populations and regions analysed and are thus relevant to the development of programmes for the prevention and treatment of CVD.
The INTERHEART study found that, on average, women experience their first myocardial infarction 9 years later than men[2]. Similarly, a recent review reported that men experience their first stroke 4.3 years before women, on average[3]. However, as the prevalence of atrial fibrillation (AF) has increased in recent years due to the ageing of the population, the longer survival of patients with heart disease and, of course, more frequent diagnosis, among other factors, AF has become a major public health problem, particularly due to the associated risk of stroke and mortality[4]. Women are not exempt from this disease, as in addition to presenting several cardiovascular risk factors, their life expectancy is longer. The incidence in women is thus not negligible, and the probability of complications, and particularly cerebrovascular problems, is relatively high. This phenomenon is likely due to the prevalence of hypertension in women, which is the most important risk factor for both AF and stroke.
The purpose of this sub-study is to establish whether there are any gender-related epidemiological, clinical, biochemical, or therapeutic differences or differences in the factors associated with AF in hypertensive patients over 65 years of age.
The FAPRES registry is a healthcare, teaching and research project sponsored by the Valencian Society of Hypertension and Vascular Risk and supported by the Spanish Society of Hypertension-Spanish League for the Fight Against Hypertension (SEH-LELHA). The current study was designed to establish the prevalence of AF in patients of ≥ 65 years of age with a clinical diagnosis of hypertension (HT) in the region of Valencia, Spain. This study involved the participation of 69 primary care physicians and physicians based in HT hospital units, a proportion similar to the population census of each of the three provinces. Written informed consent was obtained from all of the patients, and the study was performed following the principles of the Declaration of Helsinki (Edinburgh Amendment, 2000) and after approval by a hospital ethics committee (Clinical Research Ethics Committee of the Hospital General Universitario of Castellon). The general study methods and the determination of the sample size were described in previous publications[5,6]. This study is a subanalysis of these data, focusing on differential issues based on gender.
Each investigator recruited the first three patients who attended the outpatient clinic on the first working day of the week for 5 wk during the recruitment period and who met all of the inclusion criteria and none of the exclusion criteria. The inclusion criteria were as follows: (1) over 65 years of age; (2) a previous diagnosis of HT, at least 3 mo before the start of the study, according to the Good Clinical Practice (GCP) guidelines[7]; and (3) consent to participate in the study. The exclusion criteria were an arm circumference greater than 42 cm, the presence of conditions ineligible for the study or for performing ambulatory blood pressure monitoring (ABPM), and the inability to understand and sign the consent form.
Clinical blood pressure (BP) measurement was performed following the GCP recommendations[8,9], using a validated automatic electronic device. The patient was considered to have good HT control when the mean systolic BP (SBP) and diastolic BP (DBP), based on the two measurements obtained at the visit, were below 140 and 90 mmHg, respectively.
The 24-h ABPM was performed using SpaceLabs 90207 devices (SpaceLabs, Inc. Richmond, WA, United States) specifically supplied for the project. The monitors were scheduled to perform a BP measurement every 20 min during the activity period and every 30 min during the night rest period. Each period was defined individually in each registry according to the bedtime and wake-up time reported by the patient. Registries not meeting the pre-established quality standards were excluded[10]. According to the guidelines of the European Societies of Cardiology and Hypertension (ESH/ESC)[8], a good ambulatory control was defined as having BP values of < 130/80 mmHg (SBP/DBP) in a 24-h period.
The variables collected via clinical interview were age; gender; weight; height; body mass index (BMI) (obesity was defined when this parameter was ≥ 30 kg/m2); waist circumference (abdominal obesity was defined when this parameter was ≥ 102 cm in men or ≥ 88 cm in women)[11]; time from the onset of HT; excessive alcohol intake (over 30 g/d)[12]; and known cardiovascular risk factors (CVRFs), such as smoking, diabetes, dyslipidaemia (total cholesterol > 250 mg/dL, low-density lipoprotein (LDL)-cholesterol > 155 mg/dL, high-density lipoprotein (HDL)-cholesterol < 40 mg/dL in men or < 48 mg/dL in women, or receiving lipid-lowering treatment), and a family history of early cardiovascular disease (< 55 years of age in men or < 65 years of age in women).
All of the patients underwent an electrocardiogram that was sent by regular mail to a reference centre, where two expert cardiologists who were not familiar with the patients’ clinical data analysed the heart rhythm independently. In the case of a disagreement between the experts, another specialist was asked to participate. Data on lesions in the target organs and associated clinical conditions were also collected, as follows: the presence or absence of left ventricular hypertrophy (Sokolow or Cornell electrocardiographic criteria), renal damage (increased serum creatinine from 1.3-1.5 mg/dL in men or 1.2-1.4 mg/dL in women), microalbuminuria, an albumin/creatinine ratio of 22-300 mg/g in men or 31-300 mg/g in women or albuminuria of 30-300 mg/24 h, and a glomerular filtration rate (GFR) estimated from the serum creatinine values according to the abbreviated formula from the Modification of Diet in Renal Disease study[13] (renal disease was defined for a GFR of < 60 mL/h peer m2). Further data were collected on carotid disease (when the patient was diagnosed with an intima-media thickness > 0.9 mm or plaque) and previous heart disease (defined as the presence of ischaemic heart disease, heart failure or both). Additionally, we recorded the presence of previous cerebrovascular disease and peripheral arterial disease. The class and number of therapeutic subgroups of antihypertensives used for the treatment of HT were also recorded. AF was defined as having a history of arrhythmia beginning at least 3 mo before the study, as determined by medical records), even if the patients were now experiencing sinus rhythm or were diagnosed by the ECG performed on all of the patients.
An external audit of 10% of the questionnaires was performed randomly to verify the reliability of the data included in the study.
The results were expressed as frequencies and percentages for the qualitative variables and as averages with standard deviations for the quantitative variables. The 95%CI was calculated for the variables of interest assuming normality using a Kolmogorov-Smirnov test. For the comparison of means, a Student’s t test for independent data was used; when comparing quantitative data not following a normal distribution, the nonparametric Mann-Whitney test was used; and for the possible association between qualitative variables, the χ2 test was implemented, establishing statistical significance at P < 0.05. Finally, to establish the variables that were associated with the presence of AF, a binary logistic regression was performed that included all of the variables that were significant in the univariate analysis. The presence of confounding factors was evaluated by the analysis of interactions. The calibration of the multivariate model was tested using the Hosmer-Lemeshow statistic and the discriminative power using the area under the receiver operating characteristic (ROC) curve obtained by analysing the probability of the prognosticated value of the multivariate model. A general analysis and an analysis for each gender were conducted. All of the analyses were performed using the SPSS statistical package, version 15.0 (SPSS Inc., Chicago, Illinois, United States).
During the period from June to December 2008, 1028 patient records were included in this study, 954 of which (92.8%) met the pre-established quality standards for evaluation (lacking incomplete data and protocol deviations, for example)[10]. The mean age of the patients was 72.8 ± 5.8 years, and 486 (47.3%) were men, 48.3% had dyslipidaemia, 27.6% were diagnosed with diabetes mellitus, 36.2% performed physical exercise at least twice a week, 3.7% reported regular alcohol intake, 10.9% had a history of angina, 6.5% presented with myocardial infarction, and 5% experienced coronary revascularisation. Other associated diseases were heart failure in 7.3% of patients, stroke in 7.5%, and renal failure in 6.1%. Of the patients included in the study, 37.4% were obese based on BMI, and 75.8% were obese based on waist circumference. The prevalence of AF was 10.3% (9.2% in women and 11.5% in men), with 6.7% evidencing AF when an electrocardiogram (ECG), was performed and the other 3.6% having a history of AF, but at the time of analysis, experiencing sinus rhythm. Additionally, 1.7% of patients had no history of AF but were currently experiencing this arrhythmia. The laboratory, electrocardiographic and treatment data are included in Table 1.
| Characteristics | Data |
| WBC, mm3 | 6727 ± 1774 |
| Haemoglobin, g/dL | 13.6 ± 1.8 |
| Glucose, mg/dL | 108 ± 31 |
| LDL-cholesterol, mg/dL | 118 ± 34 |
| Triglycerides, mg/dL | 129 ± 73 |
| Uric acid, mg/dL | 5.2 ± 1.1 |
| Creatinine, mg/dL | 0.97 ± 0.28 |
| Glomerular filtration rate, mL/min | 75 ± 22.5 |
| Albumin/creatinine ratio | 39.4 ± 109.8 |
| Heart rate, bpm | 71.7 ± 14 |
| Normal QRS | 794 (77.2) |
| Q waves | 25 (2.4) |
| Sokolow LVH | 15 (1.5) |
| Cornell LVH | 103 (10) |
| Strain | 84 (8.2) |
| Global LVH | 177 (17.2) |
| Measurement of anti-HT | 1.7 ± 0.87 |
| Diuretics | 535 (52.1) |
| Beta-blockers | 240 (23.4) |
| Calcium antagonists | 199 (19.4) |
| ACEI | 265 (25.8) |
| ARB | 611 (59.5) |
| Antiplatelet agents | 196 (19.1) |
| VKA | 72 (7.0) |
| No anti-HT drugs | 62 (6) |
| Monotherapy | 366 (35.6) |
| 2 drugs | 366 (35.6) |
| 3 or more anti-HT drugs | 234 (22.7) |
The mean duration of HT in the overall sample was 10.9 ± 8.2 years, and 35.3% of the patients were treated according to the BP measured at the clinic, whereas 50.9% were treated according to the BP determined by ABPM. The mean BP measured at the clinic was 146.7/81.1 mmHg and determined by ABPM was 128.5/70.8 mmHg. Only 6% of the patients were not being treated with antihypertensive drugs, 35.6% were taking a single drug, 35.6% were taking two, and 22.7% were taking three or more.
Table 2 shows the differences between the men and the women in epidemiological, biochemical, BP and therapeutic characteristics. The women exhibited more obesity, greater sedentariness, a higher systolic and diastolic BP in the first clinic measurement, a higher heart rate, a higher percentage of BP control during ABPM (55.7% in women vs 45.7% in men, P < 0.001), and higher HDL-cholesterol values (56.1 ± 13.5 in women vs 49.4 ± 15.1 in men, P < 0.001). In addition, the women had a higher percentage of LVH, as determined by ECG (Cornell voltage criterion), and more frequently used diuretics than the men. In contrast, the men exhibited a greater abdominal circumference and a higher prevalence of a history of diabetes, active smoking, alcohol consumption, ischaemic heart disease, peripheral arterial disease, renal disease, and carotid disease. Regarding the control of BP at the clinic, this parameter was higher in the men (39.9% in men vs 31.2% in women, P = 0.004), who also had higher uric acid values and more frequently used anti-aggregation drugs. There were no differences in the presence of AF; the use of other antihypertensive treatments, such as beta-blockers, ARA-2, and ACEIs; or other biochemical data, including blood sugar, total cholesterol, LDL-cholesterol, triglycerides and creatinine levels and GFR.
| Females | Males | P value | |
| (n = 542) | (n = 486) | ||
| Mean age, yr | 72.7 ± 5.8 | 72.8 ± 5.8 | NS |
| Abdominal circumference, cm | 96.6 ± 11.8 | 100.4 ± 11.0 | < 0.001 |
| Weight, kg | 71.4 ± 11.5 | 79.5 ± 11.5 | < 0.001 |
| Mean height, cm | 155.2 ± 6.7 | 166.7 ± 6.7 | < 0.001 |
| BMI | 29.6 ± 4.5 | 28.6 ± 3.6 | < 0.001 |
| Obesity | 224 (41.4) | 160 (32.9) | 0.005 |
| Years from the onset of HT | 11.0 ± 8.2 | 10.8 ± 8.1 | NS |
| Diabetes mellitus | 134 (24.7) | 150 (30.9) | 0.03 |
| Dyslipidaemia | 267 (49.3) | 230 (47.3) | NS |
| Smokers | 17 (3.1) | 76 (15.6) | < 0.001 |
| Sedentariness | 352 (70.5) | 274 (56.4) | < 0.001 |
| Regular alcohol intake | 5 (0.9) | 33 (6.8) | < 0.001 |
| History of stroke | 32 (6.0) | 32 (6.7) | NS |
| History of IHD | 55 (10.1) | 124 (25.5) | < 0.001 |
| History of HF | 35 (6.5) | 39 (8.1) | NS |
| History of renal insufficiency | 24 (4.5) | 38 (7.9) | 0.025 |
| Peripheral arterial disease | 15 (2.7) | 37 (7.7) | 0.001 |
| Carotid disease | 2 (0.4) | 13 (2.8) | 0.003 |
| Atrial fibrillation | 50 (9.2) | 56 (11.5) | NS |
| CHADS ≥ 2 | 275 (50.7) | 272 (56.0) | NS |
| LVH by ECG | 111 (20.5) | 66 (13.6) | 0.004 |
| LVH_Sokolow | 6 (1.1) | 9 (1.9) | NS |
| LVH_Cornell | 91 (16.8) | 12 (2.5) | < 0.001 |
| Mean HR, bpm | 75.4 (10.7) | 72.1(10.7) | < 0.001 |
| Mean number of anti-HT | 1.7 ± 0.87 | 1.8 ± 1.0 | NS |
| Diuretics | 304 (56.1) | 226 (46.5) | 0.002 |
| Beta-blockers | 105 (19.4) | 98 (20.2) | NS |
| Calcium antagonists | 93 (17.2) | 80 (16.5) | NS |
| ACEI | 118 (21.8) | 128 (26.3) | NS |
| ARB | 318 (58.7) | 294 (60.5) | NS |
| Antiplatelet agents | 90 (16.6) | 112 (23.0) | 0.012 |
| VKA | 33 (6.1) | 32 (6.6) | NS |
No significant interactions were determined between gender and other clinical features in AF patients (Table 3). However, the presence of AF in the total study population was associated with age, with a 10% increase in AF prevalence per year; alcohol intake; previous heart disease; and GFR reduction.
| Variable | Total | Females | Males |
| OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Age, yr | 1.1 (1.1-1.1) | 1.1 (1.1-1.1) | 1.1 (1.03-1.13) |
| P < 0.001 | P = 0.010 | P = 0.003 | |
| Alcohol abuse | 5.2 (2.1-12.2) | 7.0 (0.6-82.9) | 4.2 (1.5-11.4) |
| P = 0.001 | NS | P = 0.005 | |
| Heart disease | 4.7 (3.0-7.5) | 6.1 (3.1-12.4), | 3.4 (1.9-6.2) |
| P < 0.001 | P < 0.001 | P < 0.01 | |
| GFR, mL/min per m2 | 0.98 (0.97-0.99) | 0.98 (0.96-0.99) | 0.99 (0.9-1.0) |
| P = 0.027 | P = 0.039 | NS | |
| Strain on ECG | 1.8 (0.9-3.4) | 2.97 (1.1-8.1) | 1.2 (0.53-2.81) |
| P = NS | P = 0.032 | NS |
In the gender-specific multivariate analysis, the presence of AF in the women was related to all of the overall analysis factors, in addition to the presence of strain in the ECGs (associated with LVH). In contrast, there was no association between AF and regular alcohol intake. In the men, unlike in the women, AF was only associated with age, the presence of heart disease (ischaemic or heart failure or both), and regular alcohol intake. The multivariate analysis was accurately calibrated [P = no significant (NS) and χ2 = 16.5] and had discriminative power (for the total study population, an area under the curve of 0.78, 95%CI: 0.74-0.83, and P < 0.01; for the analysis of the men only, an area of under the curve of 0.75, 95%CI: 0.68-0.81, and P < 0.01; and for the analysis of the women only, an area under the curve of 0.82, 95%CI: 0.76-0.88, and P < 0.01).
Regarding the treatment of patients diagnosed with AF (Table 4), statistically significant differences were observed between the men and the women in their use of calcium antagonists (8.9% vs 30%, respectively; P = 0.007) and antiplatelet agents (26.8% vs 8%, respectively; P = 0.01). The rates of use of antiplatelet agents and anticoagulants was higher in the men than in the women, although this disparity was also not significant (71.4% vs 66%, respectively; P = NS).
| Females | Males | P value | |
| (n = 50) | (n = 56) | ||
| Diuretics | 34 (68.0) | 30 (53.6) | NS |
| Beta-blockers | 16 (32) | 17 (30.4) | NS |
| Calcium antagonists | 15 (30) | 5 (8.9) | 0.007 |
| ACEI | 12 (24) | 14 (25) | NS |
| ARB | 32 (64) | 31 (55.4) | NS |
| Antiplatelet agents | 4 (8) | 16 (26.8) | 0.010 |
| VKA | 29 (58) | 25 (44.6) | NS |
| ATG or VKA | 33 (66) | 41 (71.4) | NS |
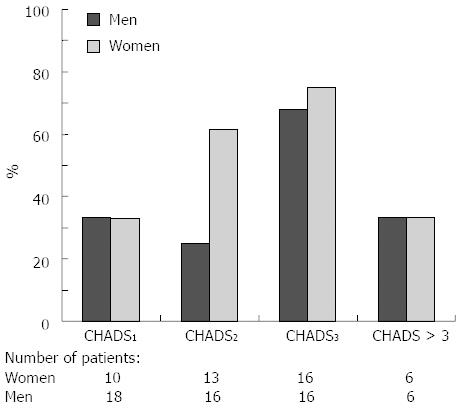
After stratification according to the CHADS2 calculated score in patients with AF, we observed that the women and men had a similar rate of using oral anticoagulation therapy in all degrees of CHADS2, except in CHADS2 = 2, in which the use of anticoagulation therapy in the women was nearly double the use in the men (Figure 1).
This study is one of the few in our country that analysed the prevalence of AF[5] and epidemiological differences by gender in a hypertensive population of over 65 years of age visiting outpatient clinics. The AF prevalence determined here (10.3%) is the same as the prevalence in another national registry, the CARDIOTENS 2009, which reported AF in 10.22% of patients with cardiovascular disease or other risk factors and in 6.22% of patients in the overall sample of the registry[14]. These data are equal to twofold the prevalence reported in 1999[15], which did not include patients diagnosed “de novo” by ECG, and are slightly higher than the AF prevalence of 8.5% reported for the PREV-ICTUS registry, which analysed 7108 subjects of over 60 years of age[16]. The higher AF prevalence reported in the current study is likely due to the different mean age of the two study populations (72.8 years in the current study vs 71.9 years in the PREV-ICTUS study), the origin of the recruited patients (here, primary care and hypertension units), and the method of AF detection (here, presence in ECGs and history of AF).
Furthermore, in our study, we noted gender differences between the classic epidemiological factors. Women exhibited a higher prevalence of non-abdominal obesity, whereas men more frequently presented a history of diabetes; smoking; alcohol use; target-organ lesions; and established cardiovascular disease, such as ischaemic heart disease, peripheral arterial disease, and stroke. However, unlike in other studies[16], no significant differences were detected in the presence of AF between men and women, although a slight disparity was noted (11.5% in men vs 9.2% in women).
Regarding the risk factors related to the presence of AF in women, the involvement of the target organ, as in the cases of LVH and renal dysfunction, and heart disease are significant conditions associated with this arrhythmia. In contrast, in men, excessive alcohol intake has a strong association with this condition, possibly due to the toxic effect of alcohol on the myocardium[17]. This knowledge can help clinicians to develop strategies to prevent AF in the hypertensive population. In women, our effort should be aimed at a greater control of BP to prevent the occurrence of lesions in target organs and of cardiovascular disease, whereas in men, the reduction of alcohol intake should be an additional objective, as described in other recent studies[18,19].
Moreover, an important finding of our study is the treatment differences between genders in patients with AF, and particularly differences in the use of antiplatelet agents and anticoagulants. Although the data were is not significant, we observed greater use in men, in contrast to the results obtained by Riesgo et al[20], who reported more frequent use in women. However, the patient profile of this prior study was different, as the subjects were recruited only from primary care, and the results were also not significant. Our results are similar to the findings of another recent report indicating higher rates of anticoagulation therapy use in men but no significant gender-related differences for other treatments[21]. Yet, when the population was stratified into groups based on CHADS2 score, women with a score of 2 had a nearly twofold higher rate of using oral anticoagulants than men. One potential reason for this discrepancy is the perception that women have a higher incidence of stroke as a complication of the evolution of AF[22,23]. This perception could lead to the expectation that women receive anti-aggregation and anticoagulation more frequently than men, as recommended in the most recent practice guidelines published[24], in which the female gender is assigned one point on the new CHADS2-VAS2C scale. Thus, hypothetically, if the practice guidelines were applied to this study, the rate of anticoagulant use in women should approach 100% if there is no contraindication (the CHADS2-VAS2C score in the women included in this study was 3). One of the main limitations of this sub-study is that it was not specifically designed to analyse differences between genders. Additionally, the sub-study did not analyse the initial reason for a consultation to diagnose arrhythmia, which would have contributed to a better interpretation of the results. There also may be other unknown confounding factors related to practitioner preferences and guideline adherence, which could explain the presence or absence of gender-related differences. Finally, the nonrandomised selection of physicians and patients may reduce the external validity of the study.
The authors wish to thank the Lácer laboratory for its contributions and constant dedication to this project. The authors also thank all of the participating researchers, without whose daily work and effort this study would not have been possible (see appendix).
Juan Alberola, Vicente Javier; Maestre Amat, Luis; Mateo Limiñana, José Manuel; Monleón Gómez, José; Montagud Moncho, Miguel; Guinot Martínez, Enrique; Gamón Pastor, José Blas; Salanova Penalba, Alejandro; Sanchis Domenech, Carlos; Pallares Carratala, Vicente; Palacios Del Cerro, Antonio; Pérez Martínez, Rafael; Baudet Dejean, Chantal; Pérez Alonso, Manuel; Fácila Rubio, Lorenzo; Sipan Sarrión Yolanda; Saro Pérez, Eugenia; Villaro Gumpert, Juan; Cabrera Ferriols, M. Ángeles; Fraile Fraile, Belén; Carbonell Franco, Francisco; Cornejo Mari, Francisco Javier; Barberá Comes, Javier; Quiles Añon, Fernando; Llisterri Caro, José Luis; Almenar Cubells, Enrique; Casado González, Joaquín; Godoy Rocati, Diego; Martínez Guerola, Carmen; Bonet García, Jorge Alejo; Blázquez Encinar, Julio César; Botella Estrada, Carlos; Saen Alcoy, Montepio; Almarcha Pérez, Natividad; Salanova Chilet, Lorena; Torres Ferrando, Miquel; Debon Belda, Manuel; Fluixa Carrascosa, Carlos; Aznar Baset, Lucía; Vivancos Aparicio, Diego; Pineda Cuenca, Manuel; Obarrio Moreno, Alicia; Núñez Jorge, Carlos; Matoses Nacher, Daniel; Baño Aracil, Manuel; Balanza Garzón, Alicia; García Palomar, Carlos; Peña Forcada, Enrique; Raga Casasus, José; Martínez Lahuerta, Juan; Mendizábal Núñez, Andrea; Santos Alonso, Eufrosina; Corbí Pascual, Miguel; Lillo Sánchez, Antonio; Martorell Adsuara, Vicente; Sánchez Ruiz, Tomás; Ortiz Díaz, Francisco; Llinares Orts, José Francisco; Lahoz Ferrer, Julio; Morillas Blasco, Pedro; Pertusa Martínez, Salvador; Manclus Montoya, Carlos; Adriá Mico, José Manuel; Llaudes Soler, Ricardo; Castillo Castillo, Jesús; Llopis Martínez, Francisco; Ruiz De La Prada Abarzuza, Ignacio; Nebot Rico, Lidia.
The incidence of atrial fibrillation (AF) is important in the general population but is even more so in hypertensive patients. As atrial fibrillation increases cardiovascular risk, knowledge of the factors that are associated with this condition is highly clinically relevant. Furthermore, the incidence of atrial fibrillation in women is different than in men, and therefore, the factors associated with atrial fibrillation in women may also be different.
Risk factors related to the presence of atrial fibrillation are under investigation, as knowledge of these factors can aid the development of preventive strategies. The difference in risk between men and women is also being studied in the field of cardiovascular medicine.
It is possible that the more aggressive treatment of these patients, particularly by administering cardiovascular drugs, could improve the patients’ prognosis.
The main application of this registry is to determine the risk factors associated with atrial fibrillation. By targeting these factors, we can avoid the development of this disease in both men and women, which has been little studied in large clinical trials.
AF is the most common cardiac arrhythmia (irregular heart beat). It may cause no symptoms, but it is often associated with palpitations, fainting, chest pain, or congestive heart failure. However, in some people atrial fibrillation is caused by otherwise idiopathic or benign conditions. Hypertension or high blood pressure, arterial hypertension, is a chronic medical condition in which the blood pressure in the arteries is elevated. ROC curve, is a graphical plot which illustrates the performance of a binary classifier system as its discrimination threshold is varied. It is created by plotting the fraction of true positives out of the positives true positive rate (TPR) vs the fraction of false positives out of the negatives false positive rate (FPR), at various threshold settings. TPR is also known as sensitivity (also called recall in some fields), and FPR is one minus the specificity or true negative rate. Univariate analysis is the simplest form of quantitative (statistical) analysis. The analysis is carried out with the description of a single variable and its attributes of the applicable unit of analysis. For example, if the variable age was the subject of the analysis, the researcher would look at how many subjects fall into a given age attribute categories.
This study is one of the few in our country that analyses the prevalence of AF and the epidemiological differences by gender in a hypertensive population of over 65 years of age attended in outpatient clinics.
P- Reviewers Facila L, Farand P, Said S S- Editor Wen LL L- Editor A E- Editor Zhang DN
| 1. | Blauwet LA, Redberg RF. The role of sex-specific results reporting in cardiovascular disease. Cardiol Rev. 2007;15:275-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Anand SS, Islam S, Rosengren A, Franzosi MG, Steyn K, Yusufali AH, Keltai M, Diaz R, Rangarajan S, Yusuf S. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur Heart J. 2008;29:932-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 492] [Cited by in F6Publishing: 497] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 3. | Appelros P, Stegmayr B, Terént A. A review on sex differences in stroke treatment and outcome. Acta Neurol Scand. 2010;121:359-369. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Moro Serrano C, Hernández-Madrid A. [Atrial fibrillation: are we faced with an epidemic? ]. Rev Esp Cardiol. 2009;62:10-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Morillas P, Pallarés V, Llisterri JL, Sanchis C, Sánchez T, Fácila L, Pérez-Alonso M, Castillo J, Redón J, Bertomeu V. Prevalence of atrial fibrillation and use of antithrombotics in hypertensive patients aged & gt; or=65 years. The FAPRES trial. Rev Esp Cardiol. 2010;63:943-950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Llisterri JL, Morillas P, Pallarés V, Fácila L, Sanchís C, Sánchez T. [Differences in the degree of control of arterial hypertension according to the measurement procedure of blood pressure in patients ≥ 65 years. FAPRES study]. Rev Clin Esp. 2011;211:76-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Europace. 2006;8:746-837. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 372] [Cited by in F6Publishing: 357] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 8. | Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105-1187. [PubMed] [Cited in This Article: ] |
| 9. | Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, Cifkova R, Clément D, Coca A, Dominiczak A. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009;27:2121-2158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1060] [Cited by in F6Publishing: 999] [Article Influence: 71.4] [Reference Citation Analysis (0)] |
| 10. | O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821-848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1193] [Cited by in F6Publishing: 1184] [Article Influence: 56.4] [Reference Citation Analysis (0)] |
| 11. | National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143-3421. [PubMed] [Cited in This Article: ] |
| 12. | Anderson P, Cremona A, Paton A, Turner C, Wallace P. The risk of alcohol. Addiction. 1993;88:1493-1508. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 180] [Cited by in F6Publishing: 178] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 568] [Cited by in F6Publishing: 565] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 14. | Rodríguez-Mañero M, Cordero A, Bertomeu-González V, Moreno-Arribas J, Bertomeu-Martínez V, Mazón P, Fácila L, Cosín J, Lekuona I, Galve E. Impact of new criteria for anticoagulant treatment in atrial fibrillation. Rev Esp Cardiol. 2011;64:649-653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | García-Acuña JM, González-Juanatey JR, Alegría Ezquerra E, González Maqueda I, Listerri JL. [Permanent atrial fibrillation in heart disease in Spain. The CARDIOTENS study 1999]. Rev Esp Cardiol. 2002;55:943-952. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 59] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Cea-Calvo L, Redón J, Lozano JV, Fernández-Pérez C, Martí-Canales JC, Llisterri JL, González-Esteban J, Aznar J. [Prevalence of atrial fibrillation in the Spanish population aged 60 years or more. The PREV-ICTUS study]. Rev Esp Cardiol. 2007;60:616-624. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 17. | Vary TC, Kimball SR, Sumner A. Sex-dependent differences in the regulation of myocardial protein synthesis following long-term ethanol consumption. Am J Physiol Regul Integr Comp Physiol. 2007;292:R778-R787. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Mukamal KJ, Tolstrup JS, Friberg J, Jensen G, Grønbaek M. Alcohol consumption and risk of atrial fibrillation in men and women: the Copenhagen City Heart Study. Circulation. 2005;112:1736-1742. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 192] [Cited by in F6Publishing: 209] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 19. | Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2011;57:427-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 192] [Cited by in F6Publishing: 205] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 20. | Riesgo A, Sant E, Benito L, Hoyo J, Miró O, Mont L, Bragulat E, Coll-Vinent B. Sex differences in the treatment of patients with atrial fibrillation: population-based study in a local health district. Rev Esp Cardiol. 2011;64:233-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Potpara TS, Marinkovic JM, Polovina MM, Stankovic GR, Seferovic PM, Ostojic MC, Lip GY. Gender-related differences in presentation, treatment and long-term outcome in patients with first-diagnosed atrial fibrillation and structurally normal heart: the Belgrade atrial fibrillation study. Int J Cardiol. 2012;161:39-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Dagres N, Nieuwlaat R, Vardas PE, Andresen D, Lévy S, Cobbe S, Kremastinos DT, Breithardt G, Cokkinos DV, Crijns HJ. Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Heart Survey on Atrial Fibrillation. J Am Coll Cardiol. 2007;49:572-577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 278] [Cited by in F6Publishing: 284] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 23. | Stroke Risk in Atrial Fibrillation Working Group. Independent predictors of stroke in patients with atrial fibrillation: a systematic review. Neurology. 2007;69:546-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 441] [Cited by in F6Publishing: 456] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 24. | Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31:2369-2429. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3227] [Cited by in F6Publishing: 3267] [Article Influence: 233.4] [Reference Citation Analysis (0)] |