Published online Jan 27, 2012. doi: 10.4240/wjgs.v4.i1.1
Revised: October 26, 2011
Accepted: December 8, 2011
Published online: January 27, 2012
Laparoscopic surgery for colorectal disease has become widespread as a minimally invasive treatment. This is important because the increasing availability of new devices allows us to perform procedures with a reduced length of surgery and decreased blood loss. We herein report the results of a literature review of energy sources for laparoscopic colorectal surgery, focused especially on 6 studies comparing ultrasonic coagulating shears (UCS) and other instruments. We also describe our laparoscopic dissection techniques using UCS for colorectal cancer. The short-term outcomes of surgeries using UCS and Ligasure for laparoscopic colorectal surgery were superior to conventional electrosurgery. Some authors have reported that the length of surgery or blood loss when Ligasure was used for laparoscopic colorectal surgery is less than when UCS was used. On the other hand, a recent study demonstrated that there were no significant differences between the short-term outcomes of UCS and Ligasure for laparoscopic colorectal surgery. It is therefore suggested that the choice of technique used should be made according to the surgeon’s preference. We also describe our laparoscopic dissection techniques using UCS (Harmonic ACE) for colorectal cancer with regard to the retroperitoneum dissection, dissection technique, dissection technique around the feeding artery, and various other dissection techniques. We therefore review the outcomes of using various energy sources for laparoscopic colorectal surgery and describe our laparoscopic dissection techniques with UCS (Harmonic ACE) for colorectal cancer.
- Citation: Hotta T, Takifuji K, Yokoyama S, Matsuda K, Higashiguchi T, Tominaga T, Oku Y, Watanabe T, Nasu T, Hashimoto T, Tamura K, Ieda J, Yamamoto N, Iwamoto H, Yamaue H. Literature review of the energy sources for performing laparoscopic colorectal surgery. World J Gastrointest Surg 2012; 4(1): 1-8
- URL: https://www.wjgnet.com/1948-9366/full/v4/i1/1.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i1.1
Laparoscopic surgery for colorectal disease has become widespread as a minimally invasive treatment because of the benefits of this procedure, such as decreased pain, faster recovery and a shorter hospital stay. Furthermore, several randomized controlled trials have demonstrated that laparoscopic colectomy could provide favorable short-term outcomes and postoperative survival in comparison with open surgery[1-9]. It is also important that the increasing availability of new devices allows us to perform procedures that reduce the length of surgery and minimize blood loss[7].
Conventional monopolar electrosurgery scissors have several shortcomings in laparoscopic surgery, including the risk of thermal injury, difficult hemostasis and smoke production, necessitating the use of additional tools such as bipolar graspers, sutures and clips. Several multifunctional tools have been developed in order to overcome these problems and to reduce the number of instrument changes, trocars and the length of surgery. An electrothermal bipolar vessel sealer and ultrasonic coagulating shears (UCS) are the most popular devices[8]. These instruments are well established in laparoscopic surgery[8]. The UCS principle is based on inducing protein denaturation inside vessels which leads to their subsequent occlusion. On the other hand, electrothermal bipolar vessel sealer Ligasure applies electrical power to the tissue with high frequency and low voltage, which results in elastin and collagen degeneration that can seal blood vessels up to 7 mm in diameter[9].
In this report, we provide a literature review of the energy sources used to perform laparoscopic colorectal surgery and describe our laparoscopic dissection techniques using UCS for colorectal cancer.
We reviewed the published literature describing the various energy sources for laparoscopic colorectal surgery, focusing on 6 studies comparing UCS and other instruments (Table 1).One study of 38 patients with colon disease requiring an elective laparoscopic segmental left-sided colon resection reported a reduced length of surgery and decreased blood loss with computer-controlled bipolar electrosurgery (Ligasure, Tyco) and 5 mm ultrasonic shears (Harmonic Scalpel, Ethicon) versus conventional electrosurgery (Valley Lab)[4]. In this study, the patients were preoperatively randomized into three groups. Group I received conventional electrosurgery; the vascular dissection was performed entirely with an electrosurgery generator and vessels were controlled with clips. Group II underwent computer-controlled bipolar electrosurgery; vascular and mesocolon resection were completed by using the 10-mm Ligasure device alone. In group III, 5 mm ultrasonic shears (Harmonic Scalpel) were used for bowel dissection, vascular pedicle dissection and mesocolon transection. The mesenteric vessel pedicle was controlled with an endostapler. The length of surgery was longer in patients operated on using conventional electrosurgery vs the Harmonic Scalpel or Ligasure (median operation time: conventional electrosurgery, 180 min; Harmonic Scalpel, 120 min; Ligasure, 110 min). These findings correlated with a significant reduction in intraoperative blood loss (median blood loss: conventional electrosurgery, 200 mL; Harmonic Scalpel, 100 mL; Ligasure, 100 mL). Conversion to other endoscopic techniques was more frequent in the conventional electrosurgery group (conventional electrosurgery, 3/11 cases; Harmonic Scalpel, 0/12 cases; Ligasure, 1/15 cases). However, the conversion to open surgery was similar in all three groups (conventional electrosurgery, 1/11 cases; Harmonic Scalpel, 0/12 cases; Ligasure, 1/15 cases). No surgical accidents related to the use of the specific devices were observed in any group. Immediate outcomes were similar in the three groups, without any significant differences in morbidity, mortality or hospital stay. An analysis of the operative costs showed no significant differences between the three groups (median final cost: conventional electrosurgery, 2995 euros; Harmonic Scalpel, 2928 euros; Ligasure, 2664 euros).
| Study | Length of surgery (min) | Blood loss (mL) | Conversion rate (%) | Morbidity (%) | Mortality (%) | Hospital stay |
| Targarona et al[4]; data expressed as the mean (range); aP < 0.01 vsI, cP < 0.01 vsI | ||||||
| I Electrosurgery (n = 11) | 180 (90-210) | 200 (0-350) | 9.1 | 36.3 | ND | 7 (6-32) d |
| II Ultracision (n = 12) | 120 (65-220)a | 100 (0-150)c | 0 | 18.2 | ND | 8 (4-18) d |
| III Ligasure (n = 15) | 110 (70-210)a | 100 (0-450) | 6.7 | 13.3 | ND | 6 (6-16) d |
| Morino et al[5]; data expressed as the mean (range); eP < 0.032 vsI | ||||||
| I Monopolar electrosurgery (n = 72) | 102.6 (75-190) | 182.6 (50-330) | 11.1 | 6.9 | 0 | 8.9 (6-12) POD |
| II Ultracision (n = 74) | 93.0 (45-170) | 140.8 (35-290)e | 12.2 | 6.7 | 0 | 8.5 (6-11) POD |
| Takada et al[6]; data expressed as the mean ± SE; gP < 0.001 vs TC ofI, iP < 0.001 vs Sig ofI, hP < 0.05 vs TC ofI, jP < 0.01 vs Sig ofI | ||||||
| I Harmonic scalpel (n = 15) | ||||||
| TC (n = 8) | 18.4 ± 0.7 | ND | ND | 1.2 ± 0.4 | ND | 15.3 ± 1.5 d |
| Sig (n = 7) | 27.6 ± 1.7 | ND | ND | 2.0 ± 0.4 | ND | 14.2 ± 1.5 d |
| II Ligasure (n = 15) | ||||||
| TC (n = 8) | 7.9 ± 0.9g | ND | ND | 0.3 ± 0.2h | ND | 14.2 ± 1.3 d |
| Sig (n = 7) | 15.0 ± 0.9i | ND | ND | 0.3 ± 0.2j | ND | 12.8 ± 1.5 d |
| Campagnacci et al[7]; data expressed as the mean (range); kP < 0.001 vs RC ofI, mP < 0.001 vs LC ofI, oP = 0.002 vs LAR ofI | ||||||
| I Harmonic scalpel (n = 100) | ||||||
| RC (n = 37) | 133 (95-190) | 370 (150-680) | 0 | 2.0 | 0 | 6.1 (5-7) POD |
| LC (n = 47) | 176 (95-240) | 455 (270-845) | 1.0 | 0 | 0 | 7.1 (5-8) POD |
| LAR (n = 16) | 201 (145-320) | 495 (280-900) | 0 | 0 | 0 | 7.3 (6-8) POD |
| II Ligasure (n = 100) | ||||||
| RC (n = 32) | 111 (70-195) | 115 (30-160)k | 0 | 0 | 0 | 5.2 (4-6) POD |
| LC (n = 50) | 140 (120-170) | 150 (70-220)m | 0 | 0 | 0 | 6.5 (5-7) POD |
| LAR (n = 18) | 153 (130-220) | 185 (100-285)o | 0 | 0 | 0 | 6.8 (5-8) POD |
| Hubner et al[8]; data expressed as the mean (range); qP < 0.001 vsI | ||||||
| I MES (n = 20) | 137 (65-230) | 125 (0-450) | ND | 50.0 | ND | 8.5 (5-29) d |
| II UCS (n = 20) | 90 (45-177)q | 50 (0-500) | ND | 30.0 | ND | 7 (3-28) d |
| III BVS (n = 21) | 105 (58-195)q | 50 (0-600) | ND | 47.6 | ND | 7 (3-31) d |
| Rimonda et al[9]; data expressed as the mean ± SD | ||||||
| I Ultracision (n = 70) | 114.8 ± 47.6 | 107.9 ± 42.0 | 8.6 | 11.4 | 0 | 7.4 ± 2.2 POD |
| II Ligasure (n = 70) | 116.3 ± 44.0 | 111.2 ± 51.5 | 7.1 | 10.0 | 1.4 | 6.9 ± 3.3 POD |
A larger trial of 146 patients demonstrated that ultrasonic dissection (UC) (Ultracision, Ethicon) is useful for laparoscopic colorectal surgery because it facilitates the completion of difficult cases and reduces intraoperative blood loss compared with standard electrosurgery (ES) (Erbotom ICC 350, ERBE)[5]. The diagnoses of the 146 patients were diverticulitis (44), colonic adenoma (31), adenocarcinoma (70) or epidermoid carcinoma (1), and these patients underwent laparoscopic right hemicolectomy (28), left hemicolectomy (31), sigmoidectomy (47) or low anterior resection (40). The overall conversion rate to open surgery was 11.6%, with no differences between the two groups; 20.8% of those undergoing ES were converted to UC and this occurred more frequently during right hemicolectomy or low anterior resection than during other procedures. The length of the surgery did not differ between the two groups: UC 93 min vs ES 102.6 min. Intraoperative blood loss was significantly lower in the UC (140.8 mL) vs the ES (182.6 mL) patients. No differences were observed in postoperative morbidity or other preoperative or postoperative parameters.
Two cohort studies comparing a bipolar vessel sealer (BVS) with the UCS for laparoscopic colectomy reported a slightly reduced length of surgery and decreased blood loss in the BVS groups[6,7]. One of these studies included 30 patients with colon cancer who underwent laparoscopic transverse colectomy and sigmoidectomy using either the electrothermal bipolar vessel sealer (EBVS) (Ligasure) or UCS (Harmonic Scalpel)[6]. The EBVS and the UCS were used for the mesocolon dissection in the transverse and sigmoid colon. The incidence of re-bleeding was significantly lower in the EBVS group than in the UCS group for both surgical procedures (0.3 vs 1.2 in transverse colectomy, 0.3 vs 2.0 in sigmoidectomy, respectively). The required time for mesocolon dissection was also significantly shorter when the EBVS was used in both laparoscopic transverse colectomy and sigmoidectomy (7.9 vs 18.4, 15.0 vs 27.6, respectively). Another report demonstrated the outcome of 200 consecutive unselected patients who underwent laparoscopic colorectal resections, of which 100 were performed with EBVS (Ligasure) and 100 with UCS (harmonic scalpel)[7]. Only right colectomy (RC), left colectomy (LC) and low anterior resections (LAR) were performed during this study. There were no deaths in either group. One conversion to open surgery and two major complications occurred in the UCS harmonic scalpel group. There were no differences in the mean length of surgery (111 vs 133, 140 vs 176 and 153 vs 201 min) or in the mean postoperative hospital stay (5.2 vs 6.1, 6.5 vs 7.1 and 6.8 vs 7.3 d) for RC, LC and LAR between EBVS Ligasure group and UCS harmonic scalpel group, respectively. There were, however, differences in the mean blood loss: 115 vs 370, 150 vs 455 and 185 vs 495 mL for RC, LC and LAR between the EBVS Ligasure group and the UCS harmonic scalpel group, respectively.
On the other hand, there was a study in which BVS, UCS and monopolar electrosurgery scissors (MES) were compared in a standardized single type of laparoscopic left-sided colectomy[8]. This study reported that electrothermal BVS (Ligasure) and UCS (Harmonic ACE, Ethicon) shorten the dissection time in laparoscopic left-sided colectomy (105 min for BVS, 90 min for UCS and 137 min for MES) and are more cost-effective compared with MES (Endo Shears 5 mm, Covidien). In this report, 61 consecutive patients undergoing laparoscopic left-sided colectomy were randomized to MES, BVS or UCS. With BVS and UCS, fewer additional clips were required and there was a trend towards lower median blood loss (125 vs 50 vs 50 mL, respectively) and a reduced median volume of suction fluid (425 vs 80 vs 110 mL).
Recently, a prospective randomized study demonstrated that an electrothermal bipolar vessel sealing system (Ligasure) and ultrasonic dissection (Ultracision) were both useful instruments for laparoscopic colorectal surgery, with no significant differences in terms of intraoperative/postoperative morbidity or the length of surgery in 140 consecutive patients who received 31 right hemicolectomies, 69 left hemicolectomies and 40 anterior resections of the rectum (70 Ligasure and 70 Ultracision)[9]. The intraoperative complication rate was 2.8% (Ultracision 1.4% vs Ligasure 4.2%). The overall complication rate was 10.7 percent (Ultracision 11.4% vs Ligasure 10.0%). Postoperative mortality was 0.7% due to one death that occurred in the Ligasure group as a consequence of an anastomotic leakage and subsequent sepsis. The overall conversion rate was 7.8%, being necessary in 6 patients in the Ligasure group and in 5 patients in the Ultracision group. The mean length of surgery, considered from the time of pneumoperitoneum to minilaparotomy, was 115.7 min (Ultracision 114.8 min vs Ligasure 116.3 min). There were no differences in the mean blood loss (Ultracision 107.9 mL vs Ligasure 111.2 mL).
This literature review demonstrates that the short-term outcomes of UCS and Ligasure for laparoscopic colorectal surgery were superior to those of conventional electrosurgery. Several authors reported that the length of surgery and blood loss when the Ligasure was used for laparoscopic colorectal surgery were reduced compared to UCS[6,7]. On the other hand, other recent studies have demonstrated no significant differences between the short-term outcomes of UCS and Ligasure for laparoscopic colorectal surgery[9]. Rimonda et al[9] concluded that choice of technique should be made according to the individual surgeon’s preference.
The development of the UCS in the early 1990s provided an alternative to conventional methods of hemostasis because it allows the simultaneous ligation and cutting of blood vessels[10]. A titanium knife blade is driven by a high-power ultrasound transducer that oscillates longitudinally with a displacement amplitude of 10 to 50 μm. At the interface between the blade and tissue, high temperatures and cavitation occur and coagulation of the tissue provides closure of the vascular structures, in addition to cutting capabilities[11]. Ultrasonic dissection works at a temperature below 80 °C, compared with the 100 °C generated during electrosurgery, and consequently, the risk of thermal damage to adjacent structures is reduced[5]. Furthermore, another advantage resulting from the lower temperature is that charring is minimized[5]. The absence of smoke is another characteristic related to the use of ultrasonic dissection, ensuring better visibility. On the other hand, the cavitation of the UCS produces some mist. The mist is considered to be more acceptable than smoke because it disperses more rapidly than the smoke produced by high-frequency cautery[5].
UCS devices effect secure sealing of vessels up to 3-5 mm in diameter[8], while maintaining a minimal thermal spread (2-3 mm)[8]. This device is widely used for various kinds of surgery[12-14]. When used with a scissor-type tip, UCS is one of the few available multifunctional laparoscopic instruments. It can be used as a grasper, dissector, coagulating device and cutter[5]. We frequently use the UCS for laparoscopic colorectal surgery because of these advantages.
We herein describe our laparoscopic dissection techniques using the UCS (Harmonic ACE, Ethicon) for colorectal cancer.
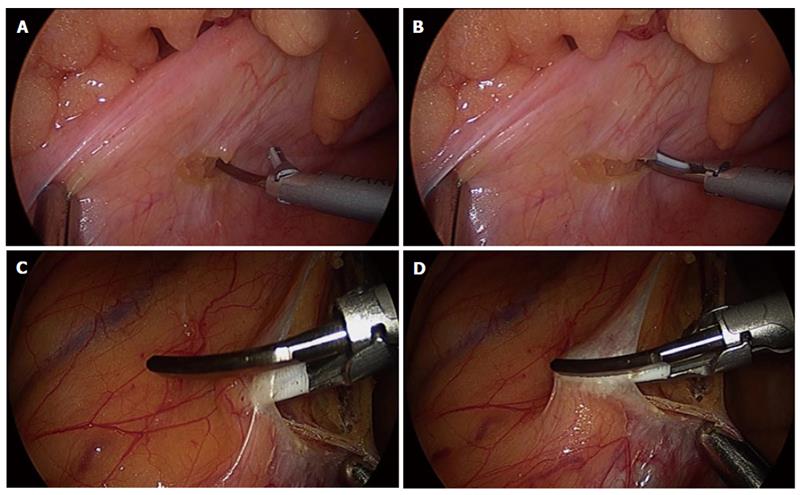
It is important for the ultrasonic surgical blade of the Harmonic ACE to be able to be seen by all surgical members in order to avoid thermal damage to adjacent structures. After a small incision for the retroperitoneum is performed, the incision is enlarged, sealing forwards to the right direction while hooking with the ultrasonic surgical blade of the Harmonic ACE or clamping with the ultrasonic surgical blade and the tissue pad (Figure 1A and B). When the incision is enlarged forwards to the left, cutting is performed by clamping the ultrasonic surgical blade and tissue pad of the Harmonic ACE, applying the tissue pad on the vessel side in order to decrease thermal damage to adjacent structures (Figures 1C and D).
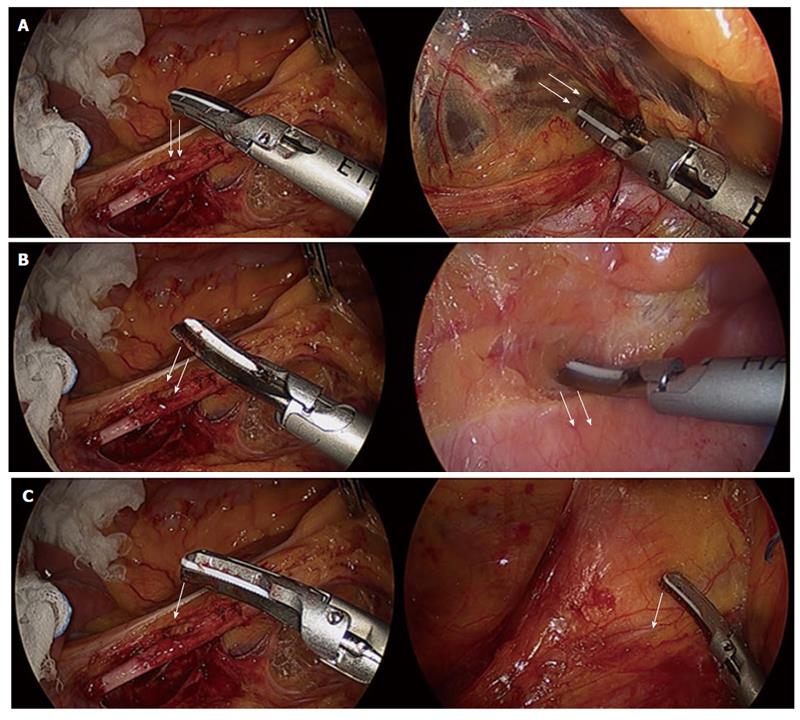
Various shapes of scissor-type tips of the Harmonic ACE can be used for the dissection. Figure 2A shows a dissection by the sharp curve of the Harmonic ACE. This method is used to dissect the tissue widely and quickly. Figure 2B shows the dissection by the round curve of the Harmonic ACE. This is used to dissect the tissue carefully and gently. The blade tip of the Harmonic ACE is used for pinpoint dissection (Figure 2C). The left figures show the dissection face of the Harmonic ACE, whereas the right figures show that the Harmonic ACE is dissecting the tissue. These methods are used by rounding the tip of the Harmonic ACE in various directions and can be changed according to the circumstances.
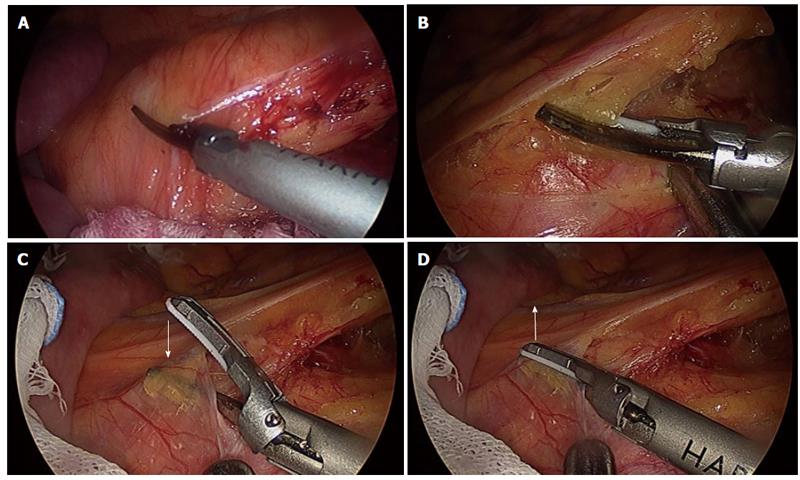
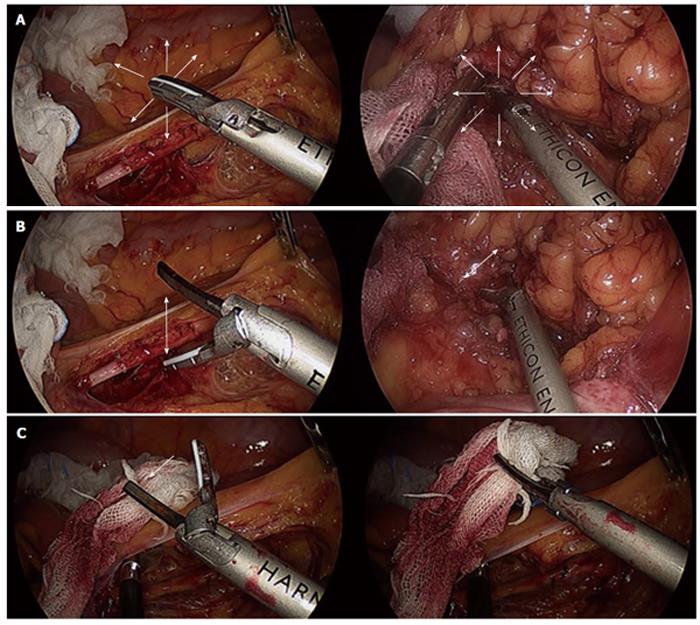
The dissection around the feeding artery is enlarged, sealing while clamping with the ultrasonic surgical blade and tissue pad of the Harmonic ACE, applying the tissue pad to the vessel side in order to decrease thermal damage to adjacent structures (Figures 3A and B). On the other hand, it is necessary to force the dissection in the direction against the feeding artery when the ultrasonic surgical blade of the Harmonic ACE has to be applied to the feeding artery side (Figures 3C and D). Figure 3C shows the clamping with the ultrasonic surgical blade and the tissue pad of the Harmonic ACE. Figure 3D shows the direction that must be forced in the other direction, with sealing. Figure 4 shows the skeletonization technique used on the feeding artery. First, the ultrasonic surgical blade of the Harmonic ACE penetrates the sheath of the feeding artery (Figure 4A) and then the dissection margin is enlarged by moving the surgical blade along the feeding artery (Figure 4B). After sufficient enlargement of the dissection margin for the sheath of the feeding artery, the ultrasonic surgical blade of the Harmonic ACE is taken out from the sheath of the feeding artery (Figure 4C). Next, the tip of the Harmonic ACE is rotated (Figure 4D) and the tissue pad side of the Harmonic ACE is applied in the penetrated space of the sheath of the feeding artery (Figure 4E). One side of the sheath of the feeding artery is sealed and skeletonized safely (Figure 4F). The other side of it is then treated similarly and consequently the complete skeletonization of the feeding artery is completed.
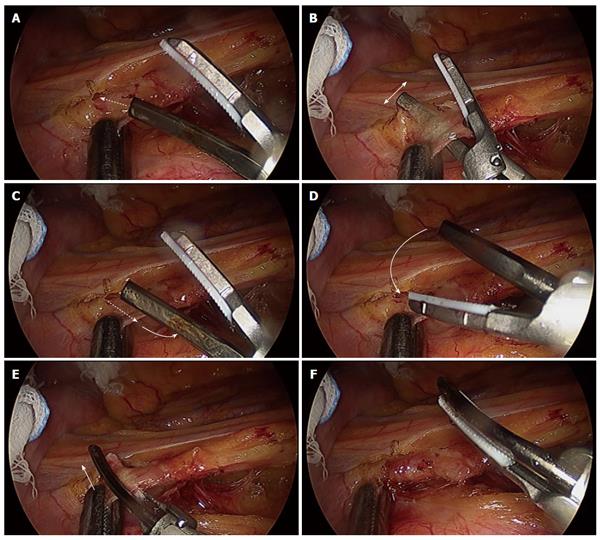
Figure 5A shows the dissection technique wherein the closed tip of the Harmonic ACE is pushed, moving in the various directions. Figure 5B shows that the Harmonic ACE can be used as a dissector, such as a Kelly forceps, while Figure 5C shows that it can be used as a grasper. The left figures show the movement of the tip of the Harmonic ACE, whereas the right figures show that the Harmonic ACE is treating tissue.
We herein have reviewed the outcomes of using different energy sources for laparoscopic colorectal surgery and have described our laparoscopic dissection techniques using UCS (Harmonic ACE) for colorectal cancer.
Peer reviewer: Giuseppe R Nigri, MD, PhD, FACS, Assistant Professor, Department of Surgery, University of Rome La Sapienza, II School of Medicine, St. Andrea Hospital, Rome, Italy
S- Editor Wang JL L- Editor Roemmele A E- Editor Li JY
| 1. | Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [PubMed] |
| 2. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2298] [Article Influence: 114.9] [Reference Citation Analysis (0)] |
| 3. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1681] [Article Influence: 84.1] [Reference Citation Analysis (0)] |
| 4. | Targarona EM, Balague C, Marin J, Neto RB, Martinez C, Garriga J, Trias M. Energy sources for laparoscopic colectomy: a prospective randomized comparison of conventional electrosurgery, bipolar computer-controlled electrosurgery and ultrasonic dissection. Operative outcome and costs analysis. Surg Innov. 2005;12:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Morino M, Rimonda R, Allaix ME, Giraudo G, Garrone C. Ultrasonic versus standard electric dissection in laparoscopic colorectal surgery: a prospective randomized clinical trial. Ann Surg. 2005;242:897-901, discussion 901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Takada M, Ichihara T, Kuroda Y. Comparative study of electrothermal bipolar vessel sealer and ultrasonic coagulating shears in laparoscopic colectomy. Surg Endosc. 2005;19:226-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Campagnacci R, de Sanctis A, Baldarelli M, Rimini M, Lezoche G, Guerrieri M. Electrothermal bipolar vessel sealing device vs. ultrasonic coagulating shears in laparoscopic colectomies: a comparative study. Surg Endosc. 2007;21:1526-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Hubner M, Demartines N, Muller S, Dindo D, Clavien PA, Hahnloser D. Prospective randomized study of monopolar scissors, bipolar vessel sealer and ultrasonic shears in laparoscopic colorectal surgery. Br J Surg. 2008;95:1098-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Rimonda R, Arezzo A, Garrone C, Allaix ME, Giraudo G, Morino M. Electrothermal bipolar vessel sealing system vs. harmonic scalpel in colorectal laparoscopic surgery: a prospective, randomized study. Dis Colon Rectum. 2009;52:657-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Koh YW, Park JH, Lee SW, Choi EC. The harmonic scalpel technique without supplementary ligation in total thyroidectomy with central neck dissection: a prospective randomized study. Ann Surg. 2008;247:945-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Koch C, Friedrich T, Metternich F, Tannapfel A, Reimann HP, Eichfeld U. Determination of temperature elevation in tissue during the application of the harmonic scalpel. Ultrasound Med Biol. 2003;29:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Nezhat F, Yadav J, Rahaman J, Gretz H, Gardner GJ, Cohen CJ. Laparoscopic lymphadenectomy for gynecologic malignancies using ultrasonically activated shears: analysis of first 100 cases. Gynecol Oncol. 2005;97:813-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Carroll T, Ladner K, Meyers AD. Alternative surgical dissection techniques. Otolaryngol Clin North Am. 2005;38:397-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Holub Z, Jabor A, Kliment L, Lukac J, Voracek J. Laparoscopic lymph node dissection using ultrasonically activated shears: comparison with electrosurgery. J Laparoendosc Adv Surg Tech A. 2002;12:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |