Published online Jun 15, 2014. doi: 10.4239/wjd.v5.i3.342
Revised: March 8, 2014
Accepted: April 17, 2014
Published online: June 15, 2014
Diabetic kidney disease (DKD) is the most common cause of chronic kidney disease, leading to end-stage renal disease and cardiovascular disease. The overall number of patients with DKD will continue to increase in parallel with the increasing global pandemic of type 2 diabetes. Based on landmark clinical trials, DKD has become preventable by controlling conventional factors, including hyperglycemia and hypertension, with multifactorial therapy; however, the remaining risk of DKD progression is still high. In this review, we show the importance of targeting remission/regression of microalbuminuria in type 2 diabetic patients, which may protect against the progression of DKD and cardiovascular events. To achieve remission/regression of microalbuminuria, several steps are important, including the early detection of microalbuminuria with continuous screening, targeting HbA1c < 7.0% for glucose control, the use of renin angiotensin system inhibitors to control blood pressure, the use of statins or fibrates to control dyslipidemia, and multifactorial treatment. Reducing microalbuminuria is therefore an important therapeutic goal, and the absence of microalbuminuria could be a pivotal biomarker of therapeutic success in diabetic patients. Other therapies, including vitamin D receptor activation, uric acid-lowering drugs, and incretin-related drugs, may also be promising for the prevention of DKD progression.
Core tip: We show the significance of targeting the remission/regression of microalbuminuria in type 2 diabetic patients, leading to protection against the progression of diabetic kidney disease (DKD) and cardiovascular events. To achieve the remission/regression of microalbuminuria, the multifactorial intervention and the early detection of microalbuminuria with continuous screening is important, as management of DKD. Multifactorial intervention includes glucose, blood pressure and lipid control. Additionally, other therapies, including vitamin D receptor activation, uric acid-lowering medicine and incretin-related medicines may be promising for preventing the progression of DKD. We review the current standard treatment for DKD and other prospective therapies for DKD.
- Citation: Kitada M, Kanasaki K, Koya D. Clinical therapeutic strategies for early stage of diabetic kidney disease. World J Diabetes 2014; 5(3): 342-356
- URL: https://www.wjgnet.com/1948-9358/full/v5/i3/342.htm
- DOI: https://dx.doi.org/10.4239/wjd.v5.i3.342
The prevalence of diabetes mellitus is increasing. According to the International Diabetes Federation Atlas of 2012, the estimated diabetes prevalence in 2012 was 371 million, representing 8.3% of the world’s adult population; it was predicted that by 2030, the number of people with diabetes in the world will have risen to 552 million[1]. Long-term diabetes results in vascular changes and dysfunction, and diabetic complications are the major causes of morbidity and mortality in diabetic patients. Among diabetic vascular complications, diabetic kidney disease (DKD) is a common cause of chronic kidney disease (CKD) and is a leading cause of end-stage renal disease (ESRD)[2]. In addition, microalbuminuria/proteinuria and a decline in the glomerular filtration rate (GFR) are observed in CKD and are recognized as independent risk factors for the development of ESRD and the onset of cardiovascular diseases, respectively. Therefore, it is important to establish therapeutic strategies for DKD.
The pathogenesis of DKD is complex and has not yet been completely elucidated. Hyperglycemia is one major factor that is responsible for the pathogenesis of DKD[3]. Moreover, elevated systemic blood pressure and intra-glomerular pressure, which are associated with the renin-angiotensin system (RAS), several cytokines and growth factors induced by metabolic and hemodynamic factors, and abnormal lipid metabolism are involved in the pathogenesis of DKD[4,5]. Current therapeutic strategies targeting these mechanisms, particularly the control of blood glucose and blood pressure, have been established in many hallmark clinical trials. In addition, a reduction in microalbuminuria is more frequent than progression to overt proteinuria, and a multifactorial control approach is important for this reduction in microalbuminuria, leading to reductions in renal and cardiovascular risk. In this review, we discuss the current standard treatment and other prospective therapies in DKD (especially early stage) that target a reduction of albuminuria.
Albuminuria is a signature feature of DKD. Albuminuria in DKD is predominantly due to impairment in the glomerular filtration barrier, consisting of the glomerular endothelial cells, the glomerular basement membrane (GBM), and the podocytes[6]. Podocytes are the predominant component of this barrier, and the reduced number of podocytes due to increased apoptosis and detachment from the GBM is observed in the diabetic kidney, resulting in leakage of albumin through areas of denuded podocytes[7-12]. In addition to a decrease in podocyte number and density, the widening of the foot processes, shortening of the slit diaphragm/loss of slit diaphragm proteins, changes in the actin cytoskeleton, and decreases in negative charge may cause albuminuria in DKD[13-15]. Furthermore, endothelial cell injuries in diabetic conditions leading to reduced nitric oxide production[16,17], altered vascular endothelial growth factor (VEGF) signaling[18,19] and diminished glycocalyx[20] also play pivotal roles in albuminuria. Glomerular endothelial cells and podocytes crosstalk through several mediators, including VEGF-A[19], angiopoietin-1[21,22] and -2[23] and activated protein C[24]; therefore, the missing link between endothelial cells and podocytes in diabetic conditions contributes to dysfunction of both cell types, resulting in increased albuminuria[25]. Glomerular hemodynamic changes, including hyperfiltration and hyperperfusion, are observed in diabetic conditions and hypertension. Elevated intraglomerular pressure creates a shear stress on the glomeruli and leads to an increase in albuminuria due to endothelial and podocyte dysfunction[26]. Vascular endothelial dysfunction is closely related to the pathogenesis of the initiation of cardiovascular disease (CVD); albuminuria also reflects glomerular endothelial dysfunction. Therefore, albuminuria is a marker of both glomerular and early systemic endothelial dysfunction[27,28].
Tubular cell injury may also contribute to albuminuria by impairing proximal tubular albumin and protein reabsorption. In diabetes, proximal tubular reuptake of albumin and protein may be impaired by high glucose[29], transforming growth factor (TGF)-β[30], or angiotensin II[31]. Tubulointerstitial injury is enhanced and the ability to reabsorb albumin and protein is further reduced, along with the development of glomerular disease, and there is a direct correlation between the degree of tubulointerstitial scarring and the extent of albuminuria[32].
The early clinical sign of DKD is elevated urinary albumin excretion, referred to as microalbuminuria, which progresses to overt proteinuria and leads to nephritic-range proteinuria in some cases. Increasing albuminuria (proteinuria) leads to a decline in renal function, which is defined in terms of the GFR[33] and generally progresses inexorably to ESRD 6-8 years after the detection of overt proteinuria[34]. Microalbuminuria is defined as a urinary albumin-creatinine ratio (ACR) of 30-299 mg/g creatinine (Cr), and macroalbuminuria is defined as an ACR > 300 mg/g Cr[35]. Elevated ACR should be confirmed in the absence of urinary tract infection in two additional first-void specimens collected during the following 3 to 6 mo[35].
Microalbuminuria in diabetic patients has been recognized as a useful biomarker for diagnosing DKD and as a predictive factor for progression to ESRD. In most patients with diabetes, CKD should be attributed to diabetes if any of the following is true: macroalbuminuria is present, microalbuminuria is present in the presence of diabetic retinopathy, or type 1 diabetes has occurred with a duration of at least 10 years[35]. However, other causes of CKD should be considered in the presence of any of the following circumstances: diabetic retinopathy is absent, GFR is low or rapidly decreasing, proteinuria is increasing or there is evidence of nephritic syndrome, refractory hypertension is noted, active urinary sediments are present, signs or symptoms of other systemic diseases are present, or a > 30% reduction in GFR has occurred within 2-3 mo after initiation of treatment with an angiotensin converting enzyme (ACE) inhibitor or angiotensin II receptor blocker (ARB)[35].
Additionally, microalbuminuria has been shown to be closely associated with an increased risk of cardiovascular morbidity and mortality[36-38]. In a sub-analysis of the United Kingdom Prospective Diabetes Study (UKPDS), the cardiovascular mortality of type 2 diabetic patients with microalbuminuria was reported to be two times higher than that of patients with normoalbuminuria[39]. Therefore, microalbuminuria is not only a biomarker for the diagnosis of DKD but is also an important therapeutic target for improving the prognosis of renal and cardiovascular risk in diabetic patients.
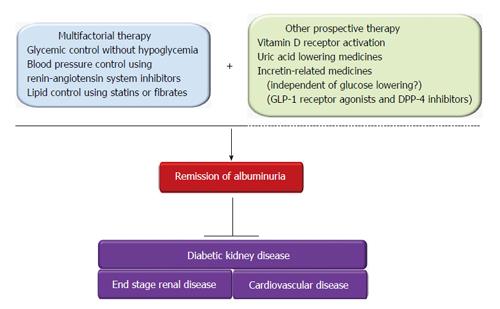
The current therapeutic strategy for DKD is shown in Figure 1. A multifactorial therapeutic approach, including glycemic control, blood pressure management, and lipid control, is recommended to prevent the progression of DKD. The remission and regression of albuminuria as a result of multifactorial therapy may be closely associated with reduced risk of both the progression of DKD and cardiovascular disease. In addition to these therapies, vitamin D receptor activation, uric acid-lowering drugs, and incretin-related drugs are potential treatments for DKD.
Chronic hyperglycemia is the main causal factor underlying diabetic vascular complications, including DKD. Multiple potential molecular mechanisms have been proposed to explain hyperglycemia-induced diabetic complications. Some of the most-studied mechanisms include disruption of the polyol pathway, activation of the diacylglycerol-protein kinase C pathway, increased oxidative stress, increased formation and activity of advanced glycation end products, and activation of the hexosamine pathway[3]. Additionally, alterations in signal transduction pathways induced by hyperglycemia or toxic metabolites have been reported to cause multiple vascular dysfunctions, such as abnormal blood flow, and increased apoptosis, inflammation, and accumulation of extracellular matrix in the kidney by alteration of gene expression or protein function[3]. Therefore, glycemic control is fundamentally necessary to prevent the onset and progression of DKD by influencing both hyperglycemia itself and hyperglycemia-induced metabolic abnormalities; this premise has been supported by several randomized controlled clinical trials in both type 1 and type 2 diabetes, as described below.
Type 1 diabetes: In the Diabetes Control and Complications Trial (DCCT), the average HbA1c levels were 7% and 9% for the intensive and conventional therapy groups, respectively. Intensive glycemic control was associated with a risk reduction of 34% for the onset of microalbuminuria and a risk reduction of 56% for progression to overt albuminuria[40]. Additionally, in the Epidemiology of Diabetes Interventions and Complications study (the follow-up study to the DCCT), intensive glycemic control prevented the onset of microalbuminuria (yielding a decrease in the odds ratio of 84% for the intensive therapy group) and the progression to overt albuminuria (yielding a decrease in the odds ratio of 59% for the intensive therapy group) at 7-8 years after the end of the DCCT, although the differences in HbA1c between the intensive and conventional therapy groups had decreased over that time. Moreover, 24 cases exhibited elevated serum Cr levels (≥ 2.0 mg/dL); of these 24 cases, 19 were in the conventional therapy group, and five were in the intensive therapy group[41]. In the follow-up study conducted 22 years after initiation of the DCCT[42], a decrease in the GFR (< 60 mL/min per 1.73 m2) was observed in the intensive therapy group, with a risk reduction of 50% compared with the conventional therapy group. The decrease in GFR per year was significantly suppressed in the intensive therapy group compared with the conventional therapy group (intensive therapy: conventional therapy, 1.27 mL/min per 1.73 m2/year: 1.56 mL/min per 1.73 m2/year).
Type 2 diabetes: In the UKPDS33, the median HbA1c levels were 7.0% and 7.9% for the intensive and conventional therapy groups, respectively. The development of diabetic microvascular complications, including nephropathy, in the intensive therapy group was reduced by 25% relative to the conventional therapy group[43]. In the follow-up study conducted 10 years after the end of the UKPDS, the development of microvascular complications, including nephropathy, in the intensive therapy group was still reduced by 24% compared with the conventional therapy group, although the differences in the HbA1c levels between the intensive and conventional therapy groups had diminished.
In the Kumamoto Study, the average HbA1c levels were 7.5% and 9.8% for the intensive and conventional therapy groups, respectively. The cumulative rates for the development and progression of nephropathy after 6 years were 7.7% for the intensive therapy group and 28.0% for the conventional therapy group in the primary prevention cohort; these rates were 11.5% and 32.0%, respectively, in the secondary intervention cohort. In this study, an HbA1c < 6.9% was identified as the target for preventing the onset and progression of diabetic nephropathy[44]. In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study, the HbA1c levels at the end of the study were 6.4% and 7.5% for the intensive and conventional therapy groups, respectively. Intensive glycemic control reduced the onset of microalbuminuria by 21% and the progression to macroalbuminuria by 32%[45] (Table 1). In the Action in Diabetes and Vascular disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) study, the HbA1c levels at the end of the study were 6.5% and 7.3% for the intensive and conventional therapy groups, respectively. Intensive glycemic control resulted in a 21% reduction in new onset or worsening nephropathy defined by new onset macroalbuminuria, doubling of serum Cr, need for kidney replacement therapy, or death due to kidney disease. Additionally, intensive glycemic control decreased the development of new onset microalbuminuria by 9%, and development of macroalbuminuria by 30%[46] (Table 1). In the Veterans Affairs Diabetes Trial (VADT) study, the HbA1c levels at the end of the study were 6.9% and 8.4% for the intensive and conventional therapy groups, respectively. Intensive glycemic control resulted in a 32% reduction in the progression from normal albuminuria to microalbuminuria or macroalbuminuria, and a 37% reduction in the progression from normal albuminuria to microalbuminuria to macroalbuminuria, and a 34% reduction in any increase in albuminuria[47] (Table 1). The ACCORD, ADVANCE, and VADT studies showed the beneficial effects of intensive glycemic control on the prevention of microalbuminuria and reduced progression to macroalbuminuria; however, these studies showed no significant benefit of more intensive glycemic control on Cr-based estimates of GFR (eGFR).
| Study | HbA1c | Outcome of albuminuria or renal events | |
| Intensive treatment | Conventional treatment | ||
| ACCORD[45] | 6.4% vs 7.6% | 21% ↓ in onset of microalbuminuria | |
| 32% ↓ in progression to macroalbuminuria | |||
| ADVANCE[46] | 6.5% vs 7.3% | 9% ↓ in onset of microalbuminuria | |
| 30% ↓ in progression to macroalbuminuria | |||
| 21% ↓ in renal events | |||
| New onset macroalbuminuria | |||
| Doubling of serum Cr | |||
| Kidney replacement therapy | |||
| Death due to kidney disease | |||
| VADT[47] | 6.9% vs 8.4% | 32% ↓ in progression from normal to microalbuminuria or macroalbuminuria | |
| 37% ↓ in progression from normal to microalbuminuria to macroalbuminuria | |||
| 34% ↓ in any increase in albuminuria | |||
Based on the results from these clinical trials, the Standards of Medical Care in Diabetes 2014 of the American Diabetes Association (ADA)[33], the Kidney Disease Improving Global Outcomes (KDIGO) 2012 Clinical Practice Guidelines for the Evaluation and Management of Chronic Kidney Disease and the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines for the management of diabetes with CKD[35] recommend a target HbA1c < 7.0% to prevent or delay the progression of DKD. However, clinical evidence that intensive glycemic control reduces DKD is limited to the prevention of microalbuminuria and reduced progression to macroalbuminuria. Evidence of intensive glucose control effecting renal outcomes, including reduced eGFR or the doubling of plasma Cr levels, or on cardiovascular disease, is still ambiguous. Additionally, no reports have prospectively examined the effect of intensive blood glucose control on overt nephropathy with macroalbuminuria, and ESRD or CKD stage 4.
Recent clinical trials, including ADVANCE[46], ACCORD[48], and VADT[47], which reported HbA1c levels of 6.5%, 6.4%, and 6.9%, respectively, showed 1.5-3-fold increases in hypoglycemia in patients with type 2 diabetes who received intensive therapy to reach target glucose levels (with targeted HbA1c levels of < 6.5%, < 6.0%, and < 6.0%, respectively). However, intensive therapy did not decrease the risk of cardiovascular events. Moreover, in the ACCORD study[48], the mortality rates for patients treated with intensive therapy were significantly higher compared to conventional therapy patients. Although the source of the relationship between hypoglycemia and increased mortality in this study was unclear[49], hypoglycemia should be avoided. Therefore, glycemic control without hypoglycemia is important, and the use of glycemic control to target HbA1c levels should be considered in light of the risk factors pertinent to the individual patient, such as the presence of diabetic vascular complications, history of diabetes, and age. At the advanced stage of overt nephropathy with a reduction in renal functioning, the risk of hypoglycemia may be increased because of decreased gluconeogenesis in the kidney, changes in pharmacokinetics resulting from reduced renal function, and reduced insulin metabolism in the kidney. Therefore, it is necessary to select anti-diabetic medicines while considering the individual patient’s renal functioning.
Systolic blood pressure control is universally recommended in patients with diabetes to reduce the incidence of stroke, heart failure, diabetes-related death, and retinal photocoagulation, as well as to reduce the risk of the onset of microalbuminuria or progression to overt proteinuria. The early findings from the UKPDS suggest that a 10 mmHg decrease in systolic blood pressure is associated with a reduction of diabetic microvascular complications, including nephropathy, by 13%[50]. Additionally, in the ADVANCE study, a reduction of blood pressure from 140/73 mmHg (control group) to 136/73 mmHg (indapamide-perindopril group) was shown to reduce the risk of a major macro- or microvascular (mostly new microalbuminuria) event and mortality from any cause, including cardiovascular disease[51]. Therefore, the goal of blood pressure < 130/80 mmHg appears to be appropriate in type 2 diabetes to fight against the development and progression of DKD[52]. However, there are recent clinical guidelines for the management of high blood pressure in patients with diabetes and CKD. The KDIGO 2012 Clinical Practice Guidelines for the Evaluation and Management of Chronic Kidney Disease recommends targets for blood pressure in diabetes and CKD as follows. Blood pressure in diabetic adults with CKD and urine albumin excretion < 30 mg/24 h (or ACR < 30 mg/g Cr) should be treated to ≤ 140/90 mmHg, and blood pressure in diabetic adults with CKD and urine albumin excretion ≥ 30 mg/24 h (or ACR ≥ 30 mg/g Cr) should be treated to ≤ 130/80 mmHg. Moreover, the Standards of Medical Care in Diabetes 2014 of the ADA[33] recommends that people with diabetes and hypertension should be treated to < 140/80 mmHg, and lower systolic targets, such as < 130 mmHg, may be appropriate for certain individuals, such as younger patients. However, the 2014 Evidence-Based Guidelines for the Management of High Blood Pressure in Adults from the Panel Members Appointed to the Eighth Joint National Committee (JNC8)[53] recommend a blood pressure goal of < 140/90 mmHg in the population aged ≥ 18 years with CKD or/and diabetes. Thus, recommendations for blood pressure targets differ between the guidelines (Table 2); however, blood control targets should be considered with the risk of the individual patient, such as the presence or absence of other diabetic vascular complications, history of CVD and age, as well as glucose control targets.
| Clinical guideline | Target population | Target of blood pressure |
| Standard of Medical Care in Diabetes-2014 (ADA) | Diabetic patients | < 140/80 mmHg (< 130 mmHg, younger patients if it can be achieved without undue treatment burden) |
| KDIGO 2012 CKD guideline | Diabetes + CKD | |
| UAE < 30 mg/24 h or ACR < 30 mg/gCr | ≤ 140/90 mmHg | |
| UAE ≥ 30 mg/24 h or ACR ≥ 30 mg/gCr | ≤ 130/80 mmHg | |
| JNC8 | Diabetic patients | < 140/90 mmHg |
| CKD patients |
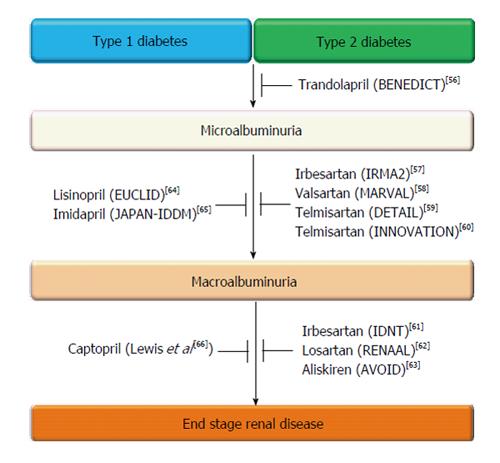
RAS activation is implicated in the pathogenesis of DKD. In diabetic patients with microalbuminuria or overt proteinuria, RAS inhibitors play a pivotal role in the prevention and treatment of DKD[54,55]. Landmark studies including type 1 and type 2 diabetic patients at various stages of DKD have provided abundant clinical evidence that treatment with RAS inhibitors, including ACE inhibitors and ARBs, slow the progressive decline of GFR, reduce micro- and macroalbuminuria, and reduce cardiovascular mortality and morbidity[54], as shown in Figure 2. Therefore, the use of RAS inhibitors for hypertension and albuminuria in diabetic patients is recommended as a first-line treatment[56-66].
Dual RAS blockade with an ACE inhibitor and ARB may be more effective in reducing proteinuria than monotherapy in patients with DKD. Based on the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial, combination therapy with ramipril and telmisartan reduces proteinuria better than monotherapy; however, it worsens major renal outcomes, including dialysis, the doubling of serum Cr levels, and death[67,68]. Additionally, the Veterans Affairs Nephropathy in Diabetes Clinical Trials showed that combination therapy with an ARB (losartan) and an ACE inhibitor (lisinopril) in type 2 diabetic patients with macroalbuminuria significantly increased the risk of hyperkalemia and acute kidney injury[69]. Thus, combined RAS blockade should not be used in diabetic patients, especially elderly type 2 diabetic patients with normo- or microalbuminuria. First, an ACE inhibitor or ARB should be used, and its dosage should be increased to obtain an optimal anti-albuminuric or proteinuric response. Combination treatment with both an ACE inhibitor and an ARB should be prescribed by a nephrologist and given to patients with overt proteinuria or severe proteinuria, notwithstanding the use of the maximum dosage of the ACE inhibitor or ARBs. In such diabetic patients, monitoring of renal function is necessary, and treatment should be halted in the event of acute kidney injury, low blood pressure, or high potassium levels.
Some clinical trials have demonstrated that treatment with spironolactone and eplerenone in addition to an ACE inhibitor or an ARB reduces proteinuria in patients with diabetes[70-75]. However, the long-term effect of mineralocorticoid receptor antagonists on GFR is not clear, and serum potassium levels should be monitored carefully.
Aliskiren, a direct renin inhibitor, has been promoted for the suppression of DKD and cardiovascular disease. In the Evaluation of Proteinuria in Diabetes study[62], patients with DKD with overt proteinuria were treated with 100 mg of losartan, followed by the addition of a placebo or aliskiren (300 mg). Treatment with 300 mg of aliskiren reduced the mean urinary ACR compared with placebo treatment. However, the Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints study[76], which was performed to confirm the effectiveness of combination treatment with either an ACE inhibitor or an ARB plus aliskiren on both renal and cardiovascular events, was terminated because of adverse outcomes, including hyperkalemia and hypotension, and predicted futility in meeting the cardiovascular and renal endpoints.
Because many hypertensive patients with DKD will require a combination therapy to adequately control blood pressure, commonly used combination therapies include an ACE inhibitor or an ARB plus a diuretic or a calcium channel blocker (CCB).
The Gauging Albuminuria Reduction With Lotrel in Diabetic Patients With Hypertension study tested the effect on albuminuria of initial combination therapy of either a dihydropyridine calcium channel blocker or a thiazide diuretic combined with the same ACE inhibitor in patients with type 2 diabetes and hypertension. In the study, both amlodipine and hydrochlorothiazide (HCTZ) combined with an initial treatment using benazepril decreased the median percent change in ACR from baseline to the end of the study; however, the benazepril plus HCTZ group had a greater reduction in albuminuria compared to the benazepril plus amlodipine group (median percent change in ACR: -72.1 vs 40.5, P < 0.0001)[77]. In contrast, the mean decrease in the eGFR during the observational period was less in the benazepril plus amlodipine group than in the benazepril plus HCTZ group (-2.03 ± 14.2 mL/min vs -13.64 ± 16.1 mL/min, P < 0.0001)[77].
The Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial was a randomized and double-blind trial in which 11506 patients with hypertension (60% of whom were diabetics) who were at high risk for cardiovascular events were assigned to receive treatment with either benazepril plus amlodipine or benazepril plus HCTZ. The benazepril-amlodipine combination had a relative risk reduction of 19.6% in cardiovascular events[78]. According to the sub-analysis of the ACCOMPLISH trial on renal outcomes, the events of CKD progression defined as a doubling of serum Cr concentration or ESRD (eGFR < 15 mL/min per 1.73 m2 or need for dialysis) occurred at a frequency of 2.0% in the benazepril plus amlodipine group compared to 3.7% in the benazepril plus HCTZ group (HR = 0.52, 0.41-0.65, P < 0.0001). However, in the patients with CKD (more than half of patients have DKD), both the progression of CKD and cardiovascular mortality did not differ between groups[79].
It is still unclear which additional anti-hypertensive drug (CCB or diuretic) is better for providing both reno- and cardioprotection in DKD. Therefore, the risk of the individual patient, such as the history of CVD and age, should be taken into consideration.
Dyslipidemia is a major risk factor for atherosclerotic cardiovascular disease, which is a cause of mortality and morbidity in patients with diabetes and CKD[80,81]. In particular, low-density lipoprotein cholesterol (LDL-C) plays an important role in the development of coronary artery disease. Several clinical trials using statin-based lipid-lowering therapies in patients with CKD and diabetes have shown reductions in the risk of major atherosclerotic events. In addition to reducing the risk of cardiovascular diseases in CKD patients, evidence suggests that statin therapy in patients with predialysis CKD may slow the progressive loss of kidney function, measured as changes in urinary albumin/protein excretion or eGFR[82-89]. In the Collaborative Atorvastatin in Diabetes Study, atorvastatin (10 mg/d) treatment was associated with increased GFR in comparison with a placebo, and a modest beneficial effect was observed, particularly in patients with albuminuria. Moreover, atorvastatin was effective at decreasing cardiovascular disease (by 42%) in patients with a moderately decreased eGFR (30-60 mL/min per 1.73 m2), and this treatment effect was similar to the 37% reduction in cardiovascular disease observed in patients without decreased eGFR[90]. Furthermore, a meta-analysis showed that statin therapy was associated with decreased albuminuria compared to a placebo[87].
The Fenofibrate Intervention and Event Lowering in Diabetes study demonstrated that fenofibrate (200 mg/d) reduced cardiovascular events, reduced albuminuria, and slowed eGFR loss over 5 years, although it initially and reversibly increased plasma Cr levels. In a meta-analysis, fibrates reduced the risk of albuminuria progression in patients with diabetes and reduced the risk of major cardiovascular events and cardiovascular death in patients with an eGFR of 30-59.9 mL/min per 1.73 m2[91,92].
Statins and fibrates can exert renoprotective effects pleiotropically, such as anti-oxidant, anti-inflammation, and anti-fibrotic effects, independent of their lipid-lowering effects, in experimental animal models[93,94].
KDOQI guidelines and the ADA recommend that the LDL-C target in patients with diabetes or/and CKD should be < 100 mg/dL, and a lower LDL-C goal of < 70 mg/dL is a therapeutic option in individuals with overt CVD, by treatment with statins. Triglyceride levels < 150 mg/dL and high-density lipoprotein cholesterol (HDL-C) > 40 mg/dL in males and > 50 mg/dL in females are desirable[33,35].
The Steno-2 study showed the effect of multifactorial intensive therapy on the progression of nephropathy in patients with type 2 diabetes[95]. In this study, 160 patients with type 2 diabetes and microalbuminuria (average age, 55 years) were randomly divided, with 80 patients assigned to a standard therapy group and 80 patients assigned to an intensive therapy group. The progression of nephropathy was evaluated as a secondary end point. During the 1993-1999 period, the targets for glycemic control, systolic blood pressure, diastolic blood pressure, total cholesterol levels, and triglyceride levels were < 6.5%, < 140 mmHg, < 85 mmHg, < 190 mg/dL, and < 150 mg/dL, respectively, in the intensive therapy group. Patients were administered ARB or ACE inhibitors (regardless of their blood pressure); patients with ischemic heart disease or peripheral vascular disease were given aspirin, and supplementation with vitamin C and E was also provided. Additionally, diet therapy (lipid restriction, < 30% of energy intake per day and < 10% from saturated fatty acid intake) and exercise therapy (3-5 times/wk, moderately intense activity) were prescribed. In the 2000-2001 period, the targets for fasting total cholesterol levels, systolic blood pressure, and diastolic blood pressure were changed to < 175 mg/dL, < 130 mmHg, and < 80 mmHg, respectively, because the treatment guidelines in Denmark changed. In the average observation period of 7.8 years, HbA1c; systolic and diastolic blood pressure; total cholesterol, LDL-C, and triglyceride levels; and fat intake were significantly reduced in the intensive therapy group compared with the standard therapy group. Moreover, the use of aspirin was significantly higher in the intensive therapy group, and urinary albumin excretion was significantly decreased in the intensive therapy group (46 mg/d) compared with the standard therapy group (126 mg/d). Moreover, the risk of onset and progression of nephropathy was reduced to a hazard ratio of 0.39 (CI: 0.17-0.87).
Furthermore, after the Steno-2 study, 63 patients in the standard therapy group underwent intensive therapy with 67 patients of the intensive therapy group in the average follow-up period of 5.5 years[96]. In the follow-up study, the onset and progression of nephropathy were assessed as secondary endpoints. At the end of the follow-up period, glucose, blood pressure, and lipid control in the standard therapy group were improved to almost the same levels as in the intensive therapy group. However, for the total observation period of 13.3 years combined with an average follow-up period of 7.8 years, the onset and progression of nephropathy were decreased in the intensive therapy group [HR = 0.44 (CI: 0.25-0.77)]. Six cases and one case progressed to ESRD in the standard and intensive therapy groups, respectively (P = 0.04).
Additionally, a cohort study with a 4-year follow-up of 1290 type 2 diabetic patients with normal albuminuria was performed using multifactorial intensive therapy[97]. In this cohort study, the targets of blood glucose, blood pressure, LDL and triglyceride levels were as follows: HbA1c < 7.0%, < 130/80 mmHg, < 100 mg/dL, < 150 mg/dL, and HDL ≥ 40 mg/dL (male) per 50 mg/mg per deciliter (female). New microalbuminuria appeared in 211 patients (16.4%) and HbA1c levels < 7% (HR = 0.729, 95%CI: 0.553-0.906, P = 0.03), blood pressure < 130 mmHg [HR = 0.645 (CI: 0.491-0.848), HDL ≥ 40 mg/dL (male) per 50 mg/dL (female), HR = 0.715 (CI: 0.537-0.951)] were associated with the onset of albuminuria.
Accordingly, multifactorial intensive therapy is recommended for suppressing the onset and progression of early diabetic nephropathy; however, it should be noted that this recommendation is based on a small RCT. Moreover, the suppressive effect of multifactorial intensive therapy on nephropathy is not clear in the advanced stage of overt nephropathy.
In the Steno-2 study described above, the incidence of cardiovascular diseases, including cardiovascular death, non-fatal myocardial infarction, non-fatal stroke, revascularization, and amputation, were evaluated as the primary endpoints over 7.8 years[95]. Thirty-three cardiovascular events (24%) in 19 cases were observed for the intensive therapy group; conversely, 35 cardiovascular events (40%) were observed in the standard therapy group. These results indicate that the risk of cardiovascular disease in type 2 diabetic patients with microalbuminuria was significantly reduced after multifactorial intensive therapy compared with standard therapy [HR = 0.47 (CI: 0.24-0.73)].
In the Steno-2 follow-up study, performed for an average of 5.5 years in addition to the original 7.8 years, the incidence of lower limb amputation, nonfatal stroke, nonfatal myocardial infarction, coronary artery bypass grafting, and percutaneous transluminal coronary angioplasty were assessed as the primary endpoints[96]. At the end of the follow-up period, glycemia, blood pressure, and lipid control for the standard therapy group had improved to levels similar to those found in the intensive therapy group. However, for the total observation period of 13.3 years, the onset of cardiovascular disease was decreased in the intensive therapy group. In addition, there were 48 cases and 158 cardiovascular events in the standard therapy group, in contrast to 28 cases and 51 cardiovascular events in the intensive therapy group.
Reduction of microalbuminuria in diabetic patients occurred more frequently than we expected. Araki et al[98] reported that microalbuminuria in type 2 diabetic patients could improve to normoalbuminuria (remission) or could decrease by more than 50% from the baseline (regression) based on the results of a prospective observational follow-up study over a 6-year period. The 6-year cumulative incidence of progression from microalbuminuria to overt proteinuria was 28% (95%CI: 19%-37%), whereas the remission and regression rates were 51% (95%CI: 42%-60%) and 54% (95%CI: 45%-63%), respectively (Figure 2). In a pooled logistic regression analysis, each modifiable factor was trisected according to the number of patients and was applied as three categories in the analysis. The results showed that microalbuminuria of short duration, the use of RAS blockade, HbA1c < 7.35%, and lower systolic blood pressure (< 130 mmHg) were identified as independent factors associated with remission/regression of microalbuminuria.
ARBs have also been shown to induce remission and regression of microalbuminuria in type 2 diabetic patients. In the Incipient to Overt: Angiotensin II Blocker, Telmisartan, Investigation on Type 2 Diabetic Nephropathy study, remission of microalbuminuria at the final observation point occurred in 21.2% of patients treated with 80 mg of telmisartan, 12.8% of patients treated with 40 mg of telmisartan, and 1.2% of patients given a placebo (both telmisartan doses vs placebo, P < 0.001)[58]. Additionally, patients receiving 80 or 40 mg of telmisartan achieved superior renoprotection, as indicated by lower transition rates to overt nephropathy compared to the placebo patients. Taken together, these results strongly indicate that RAS blockade using an ARB not only prevents the progression of microalbuminuria to overt proteinuria but also induces remission and regression of microalbuminuria in type 2 diabetic patients.
The Steno-2 study also demonstrated that a high proportion of patients with microalbuminuria returned to normoalbuminuria through the multifactorial intervention. After a mean of 7.8 years of follow-up, 46 (31%) patients returned to normoalbuminuria, 58 (38%) patients still had microalbuminuria, and 47 (31%) patients progressed to overt proteinuria[99]. Lower HbA1c levels, initiation of antihypertensive therapy, and initiation of RAS inhibitors during the follow-up period were independently associated with remission of microalbuminuria. A recent analysis focusing particularly on the effect of lowering blood pressure clearly showed that more than half of all type 2 diabetic patients with microalbuminuria and macroalbuminuria returned to normoalbuminuria with receiving any blood pressure-lowering drugs in the ADVANCE study[100]. However, more patients achieved remission to normoalbuminuria in the perindopril-indapamide treatment group than in the placebo treatment group.
The clinical impact of the remission and regression of microalbuminuria was demonstrated by the observed reduction in the risk of renal and cardiovascular events during an expanded 2-year follow-up (beyond the initial 6 years of the study reported by Araki et al[101], described above). The primary outcome measure consisted of “combined incidence,” defined as cardiovascular death by and first hospitalization for renal and cardiovascular events. A secondary outcome was kidney function, as determined by the annual decline of eGFR. During the total 8-year follow-up period, 47 patients experienced primary renal and cardiovascular events. Eleven first occurrences of outcomes occurred in subgroups that achieved remission of microalbuminuria; in contrast, 36 such events were observed for the non-remission group. The pooled logistic analysis, adjusted for sex, age, initial ACR levels, history of cardiovascular disease, current smoking, HbA1c level, total cholesterol level, blood pressure, use of RAS inhibitors, use of lipid-lowering drugs, and body mass index, showed that the relative risk for outcomes in patients who achieved remission was 0.25 (95%CI: 0.07-0.87) compared with those whose microalbuminuric status did not change during the follow-up period, whereas the relative risk for patients who progressed to overt proteinuria was 2.55 (95%CI: 1.04-6.30) (Figure 2). First occurrences of these outcomes were classified into subgroups defined by achieving a reduction greater than 50% in urinary albumin excretion in the course of 12 events for the regression group and in 35 events in the non-regression group; these patients were labeled as having failed to achieve remission.
Kaplan-Meier estimations showed that the cumulative incidence of evaluated events was significantly lower in the regression group than in the non-regression group. The 8-year cumulative incidence of these outcomes in the regression group showed a 59% decrease compared to the non-regression group. The adjusted risk for outcomes in patients who achieved regression was 0.41 (95%CI: 0.15-0.96) compared with those whose microalbuminuric status did not show regression during the follow-up. As anticipated, the annual decline of eGFR for the progression group (median: 4.2 mL/min per year) was significantly faster than that for the non-change group (2.4 mL/min per year), whereas the annual decline of eGFR for the remission group was significantly slower (1.1 mL/min per year) and was almost identical to the decline experienced through normal aging reported in healthy people[102].
The effect of reducing microalbuminuria on kidney functioning was also shown in a secondary analysis of the Steno-2 study[101]. The patients who reverted to normoalbuminuria had an average eGFR decrease of 2.3 mL/min per year; however, those who still had microalbuminuria experienced an average eGFR decrease of 3.7 mL/min per year, and those who progressed to overt proteinuria showed the highest eGFR decline of 5.4 mL/min per year. These results show that remission of microalbuminuria is closely related to the improved renal functioning over the long term.
Stimulation of vitamin D receptors exerts protective activity through multiple mechanisms, including inhibition of the RAS, regulation of proliferation and differentiation, reduction of proteinuria, anti-inflammation, and anti-fibrosis[103]. Growing evidence indicates that vitamin D exerts anti-proteinuric and renoprotective effects in DKD patients. The VITAL study demonstrated that treatment with paricalcitol, a selective vitamin D receptor activator, reduced urinary albumin excretion in type 2 diabetic patients treated with RAS inhibitors[104]. Additionally, Kim et al[105] showed beneficial effects of vitamin D (cholecalciferol) repletion on urinary albumin and transforming growth factor-β1 excretion in type 2 diabetic patients with CKD undergoing established RAS inhibition therapy; similar effects were also observed in the VITAL study. Treatment with cholecalciferol led to significantly higher levels of circulating 25(OH)D and 1,25(OH)2D3 relative to baseline, and increased levels of active forms of vitamin D were correlated with a decrease in urinary ACR and TGF-β1 at the end of a 4-mo intervention period. These data indicate that vitamin D compounds may be useful tools for delaying the progression of DKD beyond the effects expected from established RAS inhibition protocols.
Multiple longitudinal cohort studies have shown that elevated serum uric acid levels are associated with a higher risk of the onset and progression of microalbuminuria in addition to sustained decline of GFR among type 1 diabetic patients[106-108]. In a cohort study of 263 newly diagnosed type 1 diabetic patients performed by the Steno Diabetes Center group[106], serum uric acid levels measured shortly after the onset of type 1 diabetes were a significant independent predictor of macroalbuminuria 18 years later (HR = 2.37, 95%CI: 1.04-5.37, P = 0.04). Additionally, the Coronary Artery Calcification in Type 1 Diabetes study showed that serum uric acid levels predicted the transition from microalbuminuria to macroalbuminuria[107]. In 324 type 1 diabetic patients, every 1 mg/dL increase in uric acid levels at baseline was associated with an 80% increase in the predicted odds ratio of developing microalbuminuria or macroalbuminuria after 6 years of follow-up (OR = 1.8, 95%CI: 1.2-2.8, P = 0.005). A 6-year follow-up of a prospective cohort study of type 1 diabetic patients without proteinuria conducted by the Joslin Diabetes Center demonstrated a significant association (P < 0.0002) between serum uric acid and an early decrease in GFR, defined as a GFR cystatin decrease exceeding 3.3% per year[108]. When baseline uric acid concentrations were treated categorically (in mg/dL: < 3.0, 3.0-3.9, 4.0-4.9, 5.0-5.9, and ≥ 6), the risk of early decrease in GFR increased linearly (9%, 13%, 20%, 29%, and 36%, respectively). This linear increase corresponds to an OR of 1.4 (95%CI: 1.1-1.8) per 1 mg/dL increase in uric acid levels.
Furthermore, a post-hoc analysis of the Reduction of Endpoints in non-Insulin Dependent Diabetes Mellitus with the Angiotensin II Antagonist Losartan trial showed that the decrease in serum uric acid levels induced by losartan accounted for 20% of the renoprotective benefit provided by this medication[109]. However, it is not clear whether reducing uric acid levels could prevent or delay GFR decline in diabetic patients who are at high risk for the progression of DKD; therefore, clinical trials are necessary to elucidate the beneficial effects of uric acid-lowering medicine on preventing DKD.
Incretin-related therapies, including dipeptidyl peptidase (DPP)-4 inhibitors and glucagon-like peptide (GLP)-1 receptor agonists, have been developed as one of the most promising treatments for type 2 diabetes because of their effectiveness at reducing glucose levels with a low risk of hypoglycemia and no weight gain[110-112]. DPP-4 inhibitors increase the concentration of endogenous incretins, such as GLP-1 and glucose-dependent insulinotropic polypeptides, and GLP-1 analogues that are not degraded by DPP-4 may stimulate GLP-1 receptors in turn. Stimulation of GLP-1 receptors increases glucose-dependent insulin secretion from pancreatic β-cells and suppresses glucagon release from α-cells, leading to improved glucose control[110]. In addition to its action on the pancreas, GLP-1 may have direct effects on other cells and tissues, including the kidney, heart, and blood vessels, via stimulation of the GLP-1 receptor[113,114], independent of its glucose-lowering effects.
The GLP-1 receptors in the kidney are expressed in the glomerular endothelial cells, mesangial cells, and proximal tubular cells[115-120], and previous reports have shown that the expression of GLP-1 receptors decreases in the diabetic kidneys of animal models[115]. The renoprotective effect of GLP-1 may be accomplished through anti-inflammation[116], anti-oxidants mediated through cyclic AMP-mediated protein kinase A activation[117,120], or blood pressure regulation via sodium handling in proximal tubular cells[121]. DPP-4 is expressed in renal tubular cells, especially in the brush-border and microvillus fractions, podocytes, and endothelial cells[122,123]; however, the physiological role of DPP-4 in the kidney has not been elucidated. Previous reports have shown that DPP-4 expression is increased in the diabetic kidneys of animal models[124]. DPP-4 is a serine exopeptidase that cleaves X-proline dipeptides from the N-terminus of polypeptides. Therefore, DPP-4 cleaves not only incretins but also many substrates, such as cytokines, chemokines, hormones, and neuropeptides[125]. Among these substrates, high-mobility group protein-B1, meprin β, and neuropeptide Y have been identified as candidate targets for GLP-1-independent effects of DPP-4 inhibitors in the kidneys[114].
Several clinical studies have shown beneficial effects of DPP-4 inhibitors[126,127] and GLP-1 analogues[128] on albuminuria in type 2 diabetic patients. Recent reports have demonstrated that linagliptin administration in addition to stable RAS inhibition leads to a significant reduction in type 2 diabetes with albuminuria and renal dysfunction, independent of changes in glucose levels or systolic blood pressure[129]. Further studies, including randomized controlled clinical trials in large populations, are necessary to confirm the long-term effects of incretin-related medicines in DKD.
Reduced microalbuminuria may be frequent in diabetic patients. Physicians have to care for these diabetic patients with an aggressive multifactorial management plan as early as possible after the development of microalbuminuria. This multifactorial management regimen includes glycemic control without triggering hypoglycemia, blood pressure control using RAS inhibitors, and lipid control using statins or fibrates. In addition to these therapies, vitamin D receptor activators, uric acid-lowering drugs, and incretin-related drugs for glycemic control are promising therapies for stopping the progression of DKD. However, in the future, the development of novel therapies that not only function to prevent renal decline but also simultaneously attenuate CVD are necessary because the current multifactorial treatment is not still enough.
The remission or regression of microalbuminuria results in reduced risk of both renal and cardiovascular events; therefore, albuminuria is a useful biomarker for the diagnosis of DKD and the assessment of therapeutic effects for DKD. However, some patients with diabetes have advanced renal pathological changes and progressive kidney function decline even though urinary albumin levels are in the normal range, indicating that albuminuria is not the perfect biomarker for early detection of DKD[130]. Recent studies have provided some possible new markers for DKD in type 1[131,132] and type 2 diabetic patients[133]. Serum concentrations of the soluble receptors 1 and 2 for Tissue Necrosis Factor (sTNFR1 and sTNFR2) had a stronger correlation with decline in GFR than urinary ACR[131,132]. sTNFR1 was associated with the development of ESRD in type 2 patients during a 12 year follow-up[133]. However, additional clinical data about such new biomarkers for the early diagnosis and prediction of DKD should be accumulated, and at the same time, it is necessary to determine whether the new biomarker is a predictive marker for CVD.
P- Reviewers: Cui WP, Lehtonen SH, Schaalan M S- Editor: Wen LL L- Editor: A E- Editor: Liu SQ
| 1. | International Diabetes Federation. IDF Diabetes Atlas. 2012; Available from: http: //www.idf.org/diabetesatlas/5e/Update2012. [Cited in This Article: ] |
| 2. | Packham DK, Alves TP, Dwyer JP, Atkins R, de Zeeuw D, Cooper M, Shahinfar S, Lewis JB, Lambers Heerspink HJ. Relative incidence of ESRD versus cardiovascular mortality in proteinuric type 2 diabetes and nephropathy: results from the DIAMETRIC (Diabetes Mellitus Treatment for Renal Insufficiency Consortium) database. Am J Kidney Dis. 2012;59:75-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Kitada M, Zhang Z, Mima A, and King GL. Molecular mechanisms of diabetic vascular complications. J Diabetes Invest. 2010;1:77-89. [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 116] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 4. | Forbes JM, Cooper ME. Mechanisms of diabetic complications. Physiol Rev. 2013;93:137-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1360] [Cited by in F6Publishing: 1556] [Article Influence: 141.5] [Reference Citation Analysis (1)] |
| 5. | Giunti S, Barit D, Cooper ME. Mechanisms of diabetic nephropathy: role of hypertension. Hypertension. 2006;48:519-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Jefferson JA, Shankland SJ, Pichler RH. Proteinuria in diabetic kidney disease: a mechanistic viewpoint. Kidney Int. 2008;74:22-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 276] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 7. | Meyer TW, Bennett PH, Nelson RG. Podocyte number predicts long-term urinary albumin excretion in Pima Indians with Type II diabetes and microalbuminuria. Diabetologia. 1999;42:1341-1344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 345] [Cited by in F6Publishing: 351] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 8. | Pagtalunan ME, Miller PL, Jumping-Eagle S, Nelson RG, Myers BD, Rennke HG, Coplon NS, Sun L, Meyer TW. Podocyte loss and progressive glomerular injury in type II diabetes. J Clin Invest. 1997;99:342-348. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 800] [Cited by in F6Publishing: 826] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 9. | White KE, Bilous RW, Marshall SM, El Nahas M, Remuzzi G, Piras G, De Cosmo S, Viberti G. Podocyte number in normotensive type 1 diabetic patients with albuminuria. Diabetes. 2002;51:3083-3089. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 230] [Cited by in F6Publishing: 239] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 10. | Dalla Vestra M, Masiero A, Roiter AM, Saller A, Crepaldi G, Fioretto P. Is podocyte injury relevant in diabetic nephropathy? Studies in patients with type 2 diabetes. Diabetes. 2003;52:1031-1035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 224] [Cited by in F6Publishing: 241] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 11. | Petermann AT, Pippin J, Krofft R, Blonski M, Griffin S, Durvasula R, Shankland SJ. Viable podocytes detach in experimental diabetic nephropathy: potential mechanism underlying glomerulosclerosis. Nephron Exp Nephrol. 2004;98:e114-e123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 97] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Susztak K, Raff AC, Schiffer M, Böttinger EP. Glucose-induced reactive oxygen species cause apoptosis of podocytes and podocyte depletion at the onset of diabetic nephropathy. Diabetes. 2006;55:225-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 754] [Cited by in F6Publishing: 775] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 13. | Doublier S, Salvidio G, Lupia E, Ruotsalainen V, Verzola D, Deferrari G, Camussi G. Nephrin expression is reduced in human diabetic nephropathy: evidence for a distinct role for glycated albumin and angiotensin II. Diabetes. 2003;52:1023-1030. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 257] [Cited by in F6Publishing: 272] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 14. | Langham RG, Kelly DJ, Cox AJ, Thomson NM, Holthöfer H, Zaoui P, Pinel N, Cordonnier DJ, Gilbert RE. Proteinuria and the expression of the podocyte slit diaphragm protein, nephrin, in diabetic nephropathy: effects of angiotensin converting enzyme inhibition. Diabetologia. 2002;45:1572-1576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 172] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Mifsud SA, Allen TJ, Bertram JF, Hulthen UL, Kelly DJ, Cooper ME, Wilkinson-Berka JL, Gilbert RE. Podocyte foot process broadening in experimental diabetic nephropathy: amelioration with renin-angiotensin blockade. Diabetologia. 2001;44:878-882. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 115] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Nakagawa T, Sato W, Glushakova O, Heinig M, Clarke T, Campbell-Thompson M, Yuzawa Y, Atkinson MA, Johnson RJ, Croker B. Diabetic endothelial nitric oxide synthase knockout mice develop advanced diabetic nephropathy. J Am Soc Nephrol. 2007;18:539-550. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 277] [Cited by in F6Publishing: 289] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 17. | Rask-Madsen C, King GL. Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab. 2013;17:20-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 471] [Cited by in F6Publishing: 501] [Article Influence: 45.5] [Reference Citation Analysis (0)] |
| 18. | Hohenstein B, Hausknecht B, Boehmer K, Riess R, Brekken RA, Hugo CP. Local VEGF activity but not VEGF expression is tightly regulated during diabetic nephropathy in man. Kidney Int. 2006;69:1654-1661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 136] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Singh A, Satchell SC, Neal CR, McKenzie EA, Tooke JE, Mathieson PW. Glomerular endothelial glycocalyx constitutes a barrier to protein permeability. J Am Soc Nephrol. 2007;18:2885-2893. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 186] [Cited by in F6Publishing: 190] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 20. | Advani A. Vascular endothelial growth factor and the kidney: something of the marvellous. Curr Opin Nephrol Hypertens. 2014;23:87-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Jeansson M, Gawlik A, Anderson G, Li C, Kerjaschki D, Henkelman M, Quaggin SE. Angiopoietin-1 is essential in mouse vasculature during development and in response to injury. J Clin Invest. 2011;121:2278-2289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 316] [Cited by in F6Publishing: 314] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 22. | Dessapt-Baradez C, Woolf AS, White KE, Pan J, Huang JL, Hayward AA, Price KL, Kolatsi-Joannou M, Locatelli M, Diennet M. Targeted glomerular angiopoietin-1 therapy for early diabetic kidney disease. J Am Soc Nephrol. 2014;25:33-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 23. | Davis B, Dei Cas A, Long DA, White KE, Hayward A, Ku CH, Woolf AS, Bilous R, Viberti G, Gnudi L. Podocyte-specific expression of angiopoietin-2 causes proteinuria and apoptosis of glomerular endothelia. J Am Soc Nephrol. 2007;18:2320-2329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 118] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 24. | Isermann B, Vinnikov IA, Madhusudhan T, Herzog S, Kashif M, Blautzik J, Corat MA, Zeier M, Blessing E, Oh J. Activated protein C protects against diabetic nephropathy by inhibiting endothelial and podocyte apoptosis. Nat Med. 2007;13:1349-1358. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 296] [Cited by in F6Publishing: 304] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 25. | Siddiqi FS, Advani A. Endothelial-podocyte crosstalk: the missing link between endothelial dysfunction and albuminuria in diabetes. Diabetes. 2013;62:3647-3655. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 26. | Wolf G. New insights into the pathophysiology of diabetic nephropathy: from haemodynamics to molecular pathology. Eur J Clin Invest. 2004;34:785-796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 233] [Cited by in F6Publishing: 219] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 27. | Deckert T, Kofoed-Enevoldsen A, Nørgaard K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen T. Microalbuminuria. Implications for micro- and macrovascular disease. Diabetes Care. 1992;15:1181-1191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 115] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Satoh M. Endothelial dysfunction as an underlying pathophysiological condition of chronic kidney disease. Clin Exp Nephrol. 2012;16:518-521. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 29. | Ishibashi F. High glucose reduces albumin uptake in cultured proximal tubular cells (LLC-PK1). Diabetes Res Clin Pract. 2004;65:217-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Russo LM, del Re E, Brown D, Lin HY. Evidence for a role of transforming growth factor (TGF)-beta1 in the induction of postglomerular albuminuria in diabetic nephropathy: amelioration by soluble TGF-beta type II receptor. Diabetes. 2007;56:380-388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 90] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Clavant SP, Forbes JM, Thallas V, Osicka TM, Jerums G, Comper WD. Reversible angiotensin II-mediated albuminuria in rat kidneys is dynamically associated with cytoskeletal organization. Nephron Physiol. 2003;93:p51-p60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Gilbert RE, Cooper ME. The tubulointerstitium in progressive diabetic kidney disease: more than an aftermath of glomerular injury? Kidney Int. 1999;56:1627-1637. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 470] [Cited by in F6Publishing: 480] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 33. | American Diabetes Association. Standards of medical care in diabetes--2014. Diabetes Care. 2014;37 Suppl 1:S14-S80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2830] [Cited by in F6Publishing: 2933] [Article Influence: 293.3] [Reference Citation Analysis (0)] |
| 34. | Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28:164-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1037] [Cited by in F6Publishing: 1038] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 35. | National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis. 2012;60:850-886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 829] [Cited by in F6Publishing: 873] [Article Influence: 72.8] [Reference Citation Analysis (0)] |
| 36. | Garg JP, Bakris GL. Microalbuminuria: marker of vascular dysfunction, risk factor for cardiovascular disease. Vasc Med. 2002;7:35-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 210] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 37. | Lane JT. Microalbuminuria as a marker of cardiovascular and renal risk in type 2 diabetes mellitus: a temporal perspective. Am J Physiol Renal Physiol. 2004;286:F442-F450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Basi S, Lewis JB. Microalbuminuria as a target to improve cardiovascular and renal outcomes. Am J Kidney Dis. 2006;47:927-946. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 39. | Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63:225-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1163] [Cited by in F6Publishing: 1081] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 40. | The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329:977-986. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17510] [Cited by in F6Publishing: 15819] [Article Influence: 510.3] [Reference Citation Analysis (3)] |
| 41. | Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. JAMA. 2003;290:2159-2167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 883] [Cited by in F6Publishing: 786] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 42. | de Boer IH, Sun W, Cleary PA, Lachin JM, Molitch ME, Steffes MW, Zinman B. Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. N Engl J Med. 2011;365:2366-2376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 402] [Cited by in F6Publishing: 388] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 43. | Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837-853. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14327] [Cited by in F6Publishing: 12338] [Article Influence: 474.5] [Reference Citation Analysis (0)] |
| 44. | Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, Kojima Y, Furuyoshi N, Shichiri M. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995;28:103-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2132] [Cited by in F6Publishing: 1891] [Article Influence: 65.2] [Reference Citation Analysis (0)] |
| 45. | Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, Cuddihy R, Cushman WC, Genuth S, Grimm RH. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 954] [Cited by in F6Publishing: 935] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 46. | Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560-2572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4759] [Cited by in F6Publishing: 4697] [Article Influence: 293.6] [Reference Citation Analysis (0)] |
| 47. | Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3445] [Cited by in F6Publishing: 3204] [Article Influence: 213.6] [Reference Citation Analysis (0)] |
| 48. | Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545-2559. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5985] [Cited by in F6Publishing: 5384] [Article Influence: 336.5] [Reference Citation Analysis (0)] |
| 49. | Bonds DE, Miller ME, Bergenstal RM, Buse JB, Byington RP, Cutler JA, Dudl RJ, Ismail-Beigi F, Kimel AR, Hoogwerf B. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ. 2010;340:b4909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 686] [Cited by in F6Publishing: 684] [Article Influence: 48.9] [Reference Citation Analysis (0)] |
| 50. | Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4930] [Cited by in F6Publishing: 4180] [Article Influence: 160.8] [Reference Citation Analysis (0)] |
| 51. | Patel A, MacMahon S, Chalmers J, Neal B, Woodward M, Billot L, Harrap S, Poulter N, Marre M, Cooper M. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370:829-840. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1475] [Cited by in F6Publishing: 1379] [Article Influence: 81.1] [Reference Citation Analysis (0)] |
| 52. | Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Patel A, Cass A, Neal B, Poulter N. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009;20:1813-1821. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 637] [Cited by in F6Publishing: 669] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 53. | James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-520. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5429] [Cited by in F6Publishing: 5256] [Article Influence: 525.6] [Reference Citation Analysis (0)] |
| 54. | Koya D, Araki S, and Haneda M. Management of diabetes kidney disease. J Diabetes Invest. 2011;2:248-254. [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 55. | Fineberg D, Jandeleit-Dahm KA, Cooper ME. Diabetic nephropathy: diagnosis and treatment. Nat Rev Endocrinol. 2013;9:713-723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 178] [Cited by in F6Publishing: 181] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 56. | Ruggenenti P, Fassi A, Ilieva AP, Bruno S, Iliev IP, Brusegan V, Rubis N, Gherardi G, Arnoldi F, Ganeva M. Preventing microalbuminuria in type 2 diabetes. N Engl J Med. 2004;351:1941-1951. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 717] [Cited by in F6Publishing: 633] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 57. | Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345:870-878. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2280] [Cited by in F6Publishing: 2068] [Article Influence: 89.9] [Reference Citation Analysis (0)] |
| 58. | Viberti G, Wheeldon NM. Microalbuminuria reduction with valsartan in patients with type 2 diabetes mellitus: a blood pressure-independent effect. Circulation. 2002;106:672-678. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 599] [Cited by in F6Publishing: 593] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 59. | Barnett AH, Bain SC, Bouter P, Karlberg B, Madsbad S, Jervell J, Mustonen J. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. N Engl J Med. 2004;351:1952-1961. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 625] [Cited by in F6Publishing: 535] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 60. | Makino H, Haneda M, Babazono T, Moriya T, Ito S, Iwamoto Y, Kawamori R, Takeuchi M, Katayama S. Prevention of transition from incipient to overt nephropathy with telmisartan in patients with type 2 diabetes. Diabetes Care. 2007;30:1577-1578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 155] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 61. | Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345:851-860. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4068] [Cited by in F6Publishing: 3829] [Article Influence: 166.5] [Reference Citation Analysis (0)] |
| 62. | Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345:861-869. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5059] [Cited by in F6Publishing: 4851] [Article Influence: 210.9] [Reference Citation Analysis (0)] |
| 63. | Parving HH, Persson F, Lewis JB, Lewis EJ, Hollenberg NK. Aliskiren combined with losartan in type 2 diabetes and nephropathy. N Engl J Med. 2008;358:2433-2446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 847] [Cited by in F6Publishing: 716] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 64. | Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. The EUCLID Study Group. Lancet. 1997;349:1787-1792. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 361] [Cited by in F6Publishing: 208] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 65. | Katayama S, Kikkawa R, Isogai S, Sasaki N, Matsuura N, Tajima N, Urakami T, Uchigata Y, Ohashi Y. Effect of captopril or imidapril on the progression of diabetic nephropathy in Japanese with type 1 diabetes mellitus: a randomized controlled study (JAPAN-IDDM). Diabetes Res Clin Pract. 2002;55:113-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 66. | Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329:1456-1462. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3760] [Cited by in F6Publishing: 3464] [Article Influence: 111.7] [Reference Citation Analysis (1)] |
| 67. | Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, Dagenais G, Sleight P, Anderson C. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2526] [Cited by in F6Publishing: 2304] [Article Influence: 144.0] [Reference Citation Analysis (0)] |
| 68. | Mann JF, Schmieder RE, McQueen M, Dyal L, Schumacher H, Pogue J, Wang X, Maggioni A, Budaj A, Chaithiraphan S. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372:547-553. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1168] [Cited by in F6Publishing: 997] [Article Influence: 62.3] [Reference Citation Analysis (0)] |
| 69. | Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, Leehey DJ, McCullough PA, O’Connor T, Palevsky PM. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369:1892-1903. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 770] [Cited by in F6Publishing: 738] [Article Influence: 67.1] [Reference Citation Analysis (0)] |
| 70. | Kang YS, Ko GJ, Lee MH, Song HK, Han SY, Han KH, Kim HK, Han JY, Cha DR. Effect of eplerenone, enalapril and their combination treatment on diabetic nephropathy in type II diabetic rats. Nephrol Dial Transplant. 2009;24:73-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 71. | Rachmani R, Slavachevsky I, Amit M, Levi Z, Kedar Y, Berla M, Ravid M. The effect of spironolactone, cilazapril and their combination on albuminuria in patients with hypertension and diabetic nephropathy is independent of blood pressure reduction: a randomized controlled study. Diabet Med. 2004;21:471-475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 72. | Rossing K, Schjoedt KJ, Smidt UM, Boomsma F, Parving HH. Beneficial effects of adding spironolactone to recommended antihypertensive treatment in diabetic nephropathy: a randomized, double-masked, cross-over study. Diabetes Care. 2005;28:2106-2112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 225] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 73. | Schjoedt KJ, Rossing K, Juhl TR, Boomsma F, Tarnow L, Rossing P, Parving HH. Beneficial impact of spironolactone on nephrotic range albuminuria in diabetic nephropathy. Kidney Int. 2006;70:536-542. [PubMed] [Cited in This Article: ] |
| 74. | Bianchi S, Bigazzi R, Campese VM. Antagonists of aldosterone and proteinuria in patients with CKD: an uncontrolled pilot study. Am J Kidney Dis. 2005;46:45-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 103] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 75. | Mehdi UF, Adams-Huet B, Raskin P, Vega GL, Toto RD. Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximal angiotensin-converting enzyme inhibition in diabetic nephropathy. J Am Soc Nephrol. 2009;20:2641-2650. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 263] [Cited by in F6Publishing: 269] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 76. | Parving HH, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, Chaturvedi N, Persson F, Desai AS, Nicolaides M. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N Engl J Med. 2012;367:2204-2213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 936] [Cited by in F6Publishing: 850] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 77. | Bakris GL, Toto RD, McCullough PA, Rocha R, Purkayastha D, Davis P. Effects of different ACE inhibitor combinations on albuminuria: results of the GUARD study. Kidney Int. 2008;73:1303-1309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 78. | Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359:2417-2428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1515] [Cited by in F6Publishing: 1381] [Article Influence: 86.3] [Reference Citation Analysis (0)] |
| 79. | Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, Velazquez EJ, Staikos-Byrne L, Kelly RY, Shi V. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375:1173-1181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 376] [Cited by in F6Publishing: 325] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 80. | Koya D, Campese VM. Statin use in patients with diabetes and kidney disease: the Japanese experience. J Atheroscler Thromb. 2013;20:407-424. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 81. | Tonelli M, Muntner P, Lloyd A, Manns BJ, Klarenbach S, Pannu N, James MT, Hemmelgarn BR. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet. 2012;380:807-814. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 498] [Cited by in F6Publishing: 500] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 82. | Shepherd J, Kastelein JJ, Bittner V, Deedwania P, Breazna A, Dobson S, Wilson DJ, Zuckerman A, Wenger NK. Intensive lipid lowering with atorvastatin in patients with coronary heart disease and chronic kidney disease: the TNT (Treating to New Targets) study. J Am Coll Cardiol. 2008;51:1448-1454. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 208] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 83. | Koren MJ, Davidson MH, Wilson DJ, Fayyad RS, Zuckerman A, Reed DP. Focused atorvastatin therapy in managed-care patients with coronary heart disease and CKD. Am J Kidney Dis. 2009;53:741-750. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 84. | Tonelli M, Moyé L, Sacks FM, Cole T, Curhan GC. Effect of pravastatin on loss of renal function in people with moderate chronic renal insufficiency and cardiovascular disease. J Am Soc Nephrol. 2003;14:1605-1613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 238] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 85. | Tonelli M, Isles C, Craven T, Tonkin A, Pfeffer MA, Shepherd J, Sacks FM, Furberg C, Cobbe SM, Simes J. Effect of pravastatin on rate of kidney function loss in people with or at risk for coronary disease. Circulation. 2005;112:171-178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 143] [Cited by in F6Publishing: 153] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 86. | Vidt DG, Ridker PM, Monyak JT, Schreiber MJ, Cressman MD. Longitudinal assessment of estimated glomerular filtration rate in apparently healthy adults: a post hoc analysis from the JUPITER study (justification for the use of statins in prevention: an intervention trial evaluating rosuvastatin). Clin Ther. 2011;33:717-725. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 87. | Sandhu S, Wiebe N, Fried LF, Tonelli M. Statins for improving renal outcomes: a meta-analysis. J Am Soc Nephrol. 2006;17:2006-2016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 341] [Cited by in F6Publishing: 376] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 88. | Takagi H, Umemoto T. A meta-analysis of randomized trials for effects of atorvastatin on renal function in chronic kidney disease. Int J Cardiol. 2011;152:242-244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 89. | Kimura S, Inoguchi T, Yokomizo H, Maeda Y, Sonoda N, Takayanagi R. Randomized comparison of pitavastatin and pravastatin treatment on the reduction of urinary albumin in patients with type 2 diabetic nephropathy. Diabetes Obes Metab. 2012;14:666-669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 90. | Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Charlton-Menys V, DeMicco DA, Fuller JH. Effects of atorvastatin on kidney outcomes and cardiovascular disease in patients with diabetes: an analysis from the Collaborative Atorvastatin Diabetes Study (CARDS). Am J Kidney Dis. 2009;54:810-819. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 183] [Cited by in F6Publishing: 192] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 91. | Jun M, Zhu B, Tonelli M, Jardine MJ, Patel A, Neal B, Liyanage T, Keech A, Cass A, Perkovic V. Effects of fibrates in kidney disease: a systematic review and meta-analysis. J Am Coll Cardiol. 2012;60:2061-2071. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 92. | Palmer SC, Craig JC, Navaneethan SD, Tonelli M, Pellegrini F, Strippoli GF. Benefits and harms of statin therapy for persons with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med. 2012;157:263-275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 252] [Cited by in F6Publishing: 241] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 93. | Haslinger-Löffler B. Multiple effects of HMG-CoA reductase inhibitors (statins) besides their lipid-lowering function. Kidney Int. 2008;74:553-555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 94. | Balakumar P, Kadian S, Mahadevan N. Are PPAR alpha agonists a rational therapeutic strategy for preventing abnormalities of the diabetic kidney? Pharmacol Res. 2012;65:430-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 95. | Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3042] [Cited by in F6Publishing: 2784] [Article Influence: 132.6] [Reference Citation Analysis (0)] |
| 96. | Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580-591. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2459] [Cited by in F6Publishing: 2259] [Article Influence: 141.2] [Reference Citation Analysis (0)] |
| 97. | Tu ST, Chang SJ, Chen JF, Tien KJ, Hsiao JY, Chen HC, Hsieh MC. Prevention of diabetic nephropathy by tight target control in an asian population with type 2 diabetes mellitus: a 4-year prospective analysis. Arch Intern Med. 2010;170:155-161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 98. | Araki S, Haneda M, Sugimoto T, Isono M, Isshiki K, Kashiwagi A, Koya D. Factors associated with frequent remission of microalbuminuria in patients with type 2 diabetes. Diabetes. 2005;54:2983-2987. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 99. | Gaede P, Tarnow L, Vedel P, Parving HH, Pedersen O. Remission to normoalbuminuria during multifactorial treatment preserves kidney function in patients with type 2 diabetes and microalbuminuria. Nephrol Dial Transplant. 2004;19:2784-2788. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 146] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 100. | de Galan BE, Perkovic V, Ninomiya T, Pillai A, Patel A, Cass A, Neal B, Poulter N, Harrap S, Mogensen CE. Lowering blood pressure reduces renal events in type 2 diabetes. J Am Soc Nephrol. 2009;20:883-892. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 207] [Cited by in F6Publishing: 191] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 101. | Araki S, Haneda M, Koya D, Hidaka H, Sugimoto T, Isono M, Isshiki K, Chin-Kanasaki M, Uzu T, Kashiwagi A. Reduction in microalbuminuria as an integrated indicator for renal and cardiovascular risk reduction in patients with type 2 diabetes. Diabetes. 2007;56:1727-1730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 116] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 102. | Lindeman RD, Tobin J, Shock NW. Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc. 1985;33:278-285. [PubMed] [Cited in This Article: ] |
| 103. | Li YC. Vitamin D: roles in renal and cardiovascular protection. Curr Opin Nephrol Hypertens. 2012;21:72-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 104. | de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T, Parving HH, Pritchett Y, Remuzzi G, Ritz E. Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet. 2010;376:1543-1551. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 512] [Cited by in F6Publishing: 537] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 105. | Kim MJ, Frankel AH, Donaldson M, Darch SJ, Pusey CD, Hill PD, Mayr M, Tam FW. Oral cholecalciferol decreases albuminuria and urinary TGF-β1 in patients with type 2 diabetic nephropathy on established renin-angiotensin-aldosterone system inhibition. Kidney Int. 2011;80:851-860. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 106. | Hovind P, Rossing P, Tarnow L, Johnson RJ, Parving HH. Serum uric acid as a predictor for development of diabetic nephropathy in type 1 diabetes: an inception cohort study. Diabetes. 2009;58:1668-1671. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 157] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 107. | Jalal DI, Rivard CJ, Johnson RJ, Maahs DM, McFann K, Rewers M, Snell-Bergeon JK. Serum uric acid levels predict the development of albuminuria over 6 years in patients with type 1 diabetes: findings from the Coronary Artery Calcification in Type 1 Diabetes study. Nephrol Dial Transplant. 2010;25:1865-1869. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 122] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 108. | Ficociello LH, Rosolowsky ET, Niewczas MA, Maselli NJ, Weinberg JM, Aschengrau A, Eckfeldt JH, Stanton RC, Galecki AT, Doria A. High-normal serum uric acid increases risk of early progressive renal function loss in type 1 diabetes: results of a 6-year follow-up. Diabetes Care. 2010;33:1337-1343. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 168] [Cited by in F6Publishing: 166] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 109. | Miao Y, Ottenbros SA, Laverman GD, Brenner BM, Cooper ME, Parving HH, Grobbee DE, Shahinfar S, de Zeeuw D, Lambers Heerspink HJ. Effect of a reduction in uric acid on renal outcomes during losartan treatment: a post hoc analysis of the reduction of endpoints in non-insulin-dependent diabetes mellitus with the Angiotensin II Antagonist Losartan Trial. Hypertension. 2011;58:2-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 136] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 110. | Kim W, Egan JM. The role of incretins in glucose homeostasis and diabetes treatment. Pharmacol Rev. 2008;60:470-512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 511] [Cited by in F6Publishing: 554] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 111. | Gallwitz B. The evolving place of incretin-based therapies in type 2 diabetes. Pediatr Nephrol. 2010;25:1207-1217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 112. | Neumiller JJ. Clinical pharmacology of incretin therapies for type 2 diabetes mellitus: implications for treatment. Clin Ther. 2011;33:528-576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 113. | Bullock BP, Heller RS, Habener JF. Tissue distribution of messenger ribonucleic acid encoding the rat glucagon-like peptide-1 receptor. Endocrinology. 1996;137:2968-2978. [PubMed] [Cited in This Article: ] |
| 114. | Panchapakesan U, Mather A, Pollock C. Role of GLP-1 and DPP-4 in diabetic nephropathy and cardiovascular disease. Clin Sci (Lond). 2013;124:17-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 115. | Mima A, Hiraoka-Yamomoto J, Li Q, Kitada M, Li C, Geraldes P, Matsumoto M, Mizutani K, Park K, Cahill C. Protective effects of GLP-1 on glomerular endothelium and its inhibition by PKCβ activation in diabetes. Diabetes. 2012;61:2967-2979. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 116. | Kodera R, Shikata K, Kataoka HU, Takatsuka T, Miyamoto S, Sasaki M, Kajitani N, Nishishita S, Sarai K, Hirota D. Glucagon-like peptide-1 receptor agonist ameliorates renal injury through its anti-inflammatory action without lowering blood glucose level in a rat model of type 1 diabetes. Diabetologia. 2011;54:965-978. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 263] [Cited by in F6Publishing: 284] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 117. | Fujita H, Morii T, Fujishima H, Sato T, Shimizu T, Hosoba M, Tsukiyama K, Narita T, Takahashi T, Drucker DJ. The protective roles of GLP-1R signaling in diabetic nephropathy: possible mechanism and therapeutic potential. Kidney Int. 2014;85:579-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 189] [Cited by in F6Publishing: 210] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 118. | Li W, Cui M, Wei Y, Kong X, Tang L, Xu D. Inhibition of the expression of TGF-β1 and CTGF in human mesangial cells by exendin-4, a glucagon-like peptide-1 receptor agonist. Cell Physiol Biochem. 2012;30:749-757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 119. | Schlatter P, Beglinger C, Drewe J, Gutmann H. Glucagon-like peptide 1 receptor expression in primary porcine proximal tubular cells. Regul Pept. 2007;141:120-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 120. | Hendarto H, Inoguchi T, Maeda Y, Ikeda N, Zheng J, Takei R, Yokomizo H, Hirata E, Sonoda N, Takayanagi R. GLP-1 analog liraglutide protects against oxidative stress and albuminuria in streptozotocin-induced diabetic rats via protein kinase A-mediated inhibition of renal NAD(P)H oxidases. Metabolism. 2012;61:1422-1434. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 152] [Cited by in F6Publishing: 167] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 121. | Hirata K, Kume S, Araki S, Sakaguchi M, Chin-Kanasaki M, Isshiki K, Sugimoto T, Nishiyama A, Koya D, Haneda M. Exendin-4 has an anti-hypertensive effect in salt-sensitive mice model. Biochem Biophys Res Commun. 2009;380:44-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 114] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 122. | Mentlein R. Dipeptidyl-peptidase IV (CD26)--role in the inactivation of regulatory peptides. Regul Pept. 1999;85:9-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 994] [Cited by in F6Publishing: 952] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 123. | Sun AL, Deng JT, Guan GJ, Chen SH, Liu YT, Cheng J, Li ZW, Zhuang XH, Sun FD, Deng HP. Dipeptidyl peptidase-IV is a potential molecular biomarker in diabetic kidney disease. Diab Vasc Dis Res. 2012;9:301-308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 90] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 124. | Yang J, Campitelli J, Hu G, Lin Y, Luo J, Xue C. Increase in DPP-IV in the intestine, liver and kidney of the rat treated with high fat diet and streptozotocin. Life Sci. 2007;81:272-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 125. | Ansorge S, Nordhoff K, Bank U, Heimburg A, Julius H, Breyer D, Thielitz A, Reinhold D, Täger M. Novel aspects of cellular action of dipeptidyl peptidase IV/CD26. Biol Chem. 2011;392:153-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 126. | Hattori S. Sitagliptin reduces albuminuria in patients with type 2 diabetes. Endocr J. 2011;58:69-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 124] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 127. | Harashima SI, Ogura M, Tanaka D, Fukushima T, Wang Y, Koizumi T, Aono M, Murata Y, Seike M, Inagaki N. Sitagliptin add-on to low dosage sulphonylureas: efficacy and safety of combination therapy on glycaemic control and insulin secretion capacity in type 2 diabetes. Int J Clin Pract. 2012;66:465-476. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 128. | Zhang H, Zhang X, Hu C, Lu W. Exenatide reduces urinary transforming growth factor-β1 and type IV collagen excretion in patients with type 2 diabetes and microalbuminuria. Kidney Blood Press Res. 2012;35:483-488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 129. | Groop PH, Cooper ME, Perkovic V, Emser A, Woerle HJ, von Eynatten M. Linagliptin lowers albuminuria on top of recommended standard treatment in patients with type 2 diabetes and renal dysfunction. Diabetes Care. 2013;36:3460-3468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 219] [Cited by in F6Publishing: 217] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 130. | Jerums G, Panagiotopoulos S, Premaratne E, MacIsaac RJ. Integrating albuminuria and GFR in the assessment of diabetic nephropathy. Nat Rev Nephrol. 2009;5:397-406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 131. | Niewczas MA, Ficociello LH, Johnson AC, Walker W, Rosolowsky ET, Roshan B, Warram JH, Krolewski AS. Serum concentrations of markers of TNFalpha and Fas-mediated pathways and renal function in nonproteinuric patients with type 1 diabetes. Clin J Am Soc Nephrol. 2009;4:62-70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 132. | Gohda T, Niewczas MA, Ficociello LH, Walker WH, Skupien J, Rosetti F, Cullere X, Johnson AC, Crabtree G, Smiles AM. Circulating TNF receptors 1 and 2 predict stage 3 CKD in type 1 diabetes. J Am Soc Nephrol. 2012;23:516-524. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 253] [Cited by in F6Publishing: 256] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 133. | Niewczas MA, Gohda T, Skupien J, Smiles AM, Walker WH, Rosetti F, Cullere X, Eckfeldt JH, Doria A, Mayadas TN. Circulating TNF receptors 1 and 2 predict ESRD in type 2 diabetes. J Am Soc Nephrol. 2012;23:507-515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 327] [Cited by in F6Publishing: 336] [Article Influence: 28.0] [Reference Citation Analysis (0)] |