Published online Oct 16, 2013. doi: 10.4253/wjge.v5.i10.508
Revised: August 7, 2013
Accepted: August 20, 2013
Published online: October 16, 2013
AIM: To develop a new continuous suction mouthpiece (CSM) and evaluate its usefulness for screening esophagogastroduodenoscopy (EGD).
METHODS: A total of 196 patients who were scheduled to undergo screening EGD were assigned to one of two groups: a group using the CSM and a group using a conventional mouthpiece. Extent of salivary flow, frequency of saliva suction, number of choking episodes during the examination, and incidence of aspiration pneumonia after the examination were evaluated and compared between the two groups. Adverse events during and after EGD were also examined. In addition, the oral cavity was meticulously examined after the EGD.
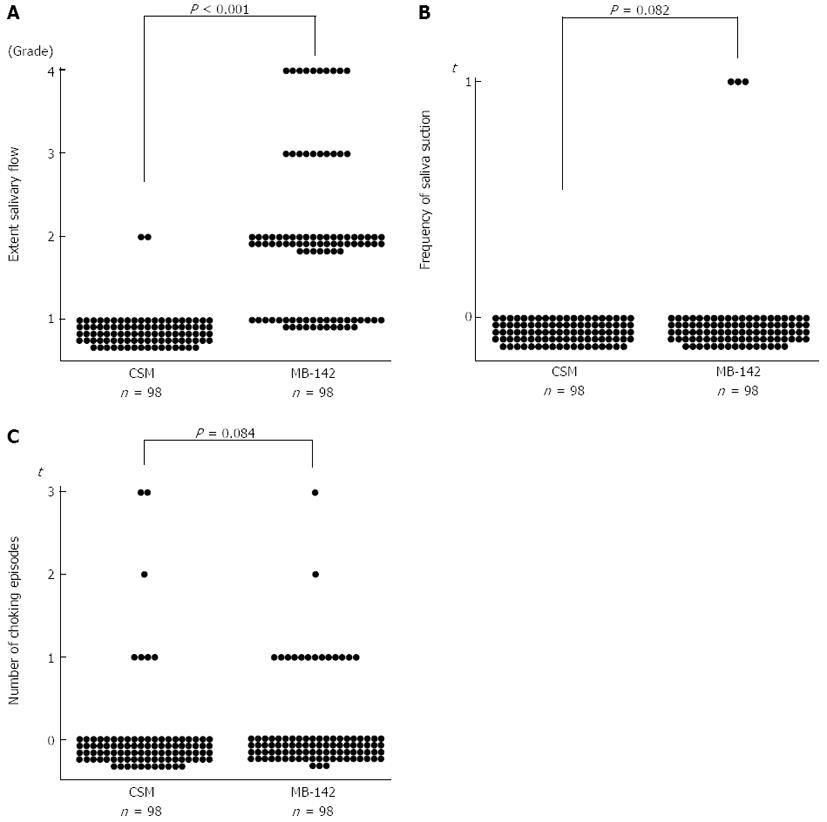
RESULTS: The same number of patients was randomly allocated to each group. There were no significant differences between the two groups in sex, age, biopsy procedure, duration of procedure and depth of sedation. Aspiration pneumonia and other significant adverse events were not observed in either group. The grade of extent of salivary flow was significantly lower in patients with the CSM than in patients with the conventional mouthpiece (P < 0.001). Although there was no significant difference, less frequent suctioning and fewer choking episodes were observed in patients with the CSM than in patients with the conventional mouthpiece (P = 0.082 and P = 0.084, respectively). In addition, there were no patients in the CSM group who required saliva suctioning during the procedure.
CONCLUSION: Use of the CSM during screening EGD can reduce the extent of salivary flow. The device is expected to reduce complications and contamination with saliva.
Core tip: Control of salivary flow during endoscopic examination is important. We focused on a mouthpiece designed for control of saliva in this study. First, we produced a new continuous suction mouthpiece (CSM). Then, we evaluated its usefulness for esophagogastroduodenoscopy (EGD). This study indicates that the CSM can reduce the extent of salivary flow during EGD. Moreover, it tended to reduce the frequencies of suction and choking episodes during EGD.
- Citation: Maekita T, Kato J, Nakatani Y, Enomoto S, Takano E, Tsuji M, Nakaya T, Moribata K, Muraki Y, Shingaki N, Niwa T, Deguchi H, Ueda K, Inoue I, Iguchi M, Tamai H, Ichinose M. Usefulness of continuous suction mouthpiece during esophagogastroduodenoscopy: A single-center, prospective, randomized study. World J Gastrointest Endosc 2013; 5(10): 508-513
- URL: https://www.wjgnet.com/1948-5190/full/v5/i10/508.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i10.508
Screening esophagogastroduodenoscopy (EGD) is a common examination that is useful in detecting upper gastrointestinal disease. Hence, it is increasingly performed for patients. However, performance of EGD is associated with the risk of certain adverse events, including aspiration, because EGD is often performed with sedation. A study reported that the rate of aspiration during EGD with sedation was as high as 3.94%[1] when subclinical cases were included. More attention should be paid to this risk.
One of the most important factors correlating with aspiration is the salivary flow induced by introduction/extraction of the endoscope into the oral cavity. Therefore, control of salivary flow during EGD is important for prevention of aspiration. However, few attempts have been made to control salivary flow, perhaps due to its difficulty. Currently, the endoscopist or an assistant must watch for the accumulation of saliva and suction it using a catheter, in case the patient undergoing EGD cannot discharge saliva from the mouth. In this context, control of salivary flow during EGD, if possible, might reduce the endoscopist’s or nurse’s suctioning efforts, resulting in prevention of complications associated with aspiration. Moreover, contamination of the patient’s face or clothes with saliva could also be minimized.
During EGD, a hard plastic mouthpiece is used to protect the endoscope from being bitten and to enable its smooth insertion. A mouthpiece that can also suction saliva might be useful for preventing aspiration and contamination with saliva during EGD. Accordingly, we recently developed a new continuous suction mouthpiece (CSM), and reported its usefulness for prevention of complications associated with salivary flow during percutaneous endoscopic gastrostomy (PEG) procedures[2]. The background of the study patients in this study differed from that of the patients in the PEG study. PEG is performed with the patient in the supine position, is a lengthy process, and is indicated for elderly patients with dysphagia. In contrast, EGD is performed with the patient in the left lateral position, is a shorter process, and is indicated for patients without dysphagia and severe complications.
The aim of this study was to evaluate the usefulness and ability of the CSM for prevention of complications and contamination associated with saliva, including aspiration, during screening EGD.
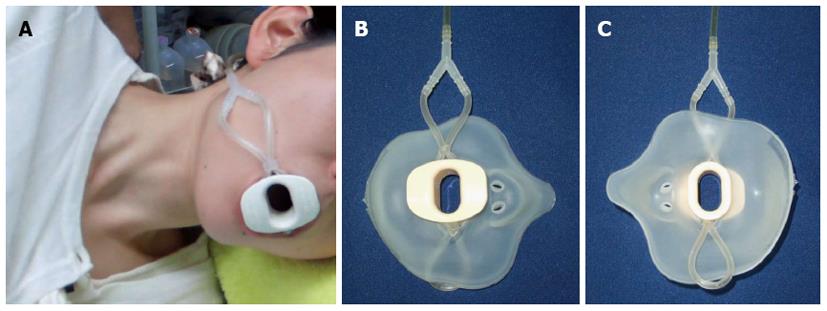
The details of production of the CSM were reported previously[2]. In summary, after cutting the junction part of a non-toxic polyvinyl chloride (PVC) suction tube (Nipro Suction Catheter® 14-Fr, Nipro, Osaka, Japan), the tube was bent double and the two sides were connected with two movable short bands made of non-toxic PVC suction tubing (Nipro Suction Catheter® 16-Fr, Nipro). The three parts divided by the short bands were made into: a 2- to 5-cm-diameter, adjustable intraoral loop part with 6 smooth 2.7-mm-diameter holes for suction; a binding loop part to fit mouthpieces of various sizes; and an extraoral part having two ends, both of which were linked to the Y-shaped connector (ARAM, Osaka, Japan). Finally, the MB-142 mouthpiece (Olympus, Tokyo, Japan) was inserted into the binding loop part (Figure 1).
For screening EGD in the CSM group, patients were placed on their left side and asked to bite down on the mouthpiece, with the intraoral loop with holes placed inside the left cheek. During EGD, continuous low pressure (10 kPa) suctioning with a suction unit (Shin-Ei Industries, Tokyo, Japan) was performed through the unification tube attached to the Y-shaped connector (Figure 2). In control subjects, the MB-142 mouthpiece was used in the usual way.
This was a single-center, prospective, randomized, controlled study. Patients who underwent screening EGD in Nakaya Hospital (Wakayama, Japan) from February 2011 to December 2011 were recruited. Patients were excluded if they had a history of respiratory problems that could increase the risk of complications associated with aspiration pneumonia and salivary flow. Eligible patients were randomly assigned to one of the following groups: the group using the CSM, or the group using the conventional mouthpiece for EGD. During the EGD, salivary flow and complications associated with aspiration were evaluated and compared between the two groups. However, due to its nature, this study could not be blinded.
This study was approved by the ethics committee of Nakaya Hospital. Written, informed consent was obtained from each patient. This study was registered with the University Hospital Medical Information Network (UMIN) (registration number UMIN000009294). The CSM was developed solely by our institute without any financial or equipment support from companies.
A conventional gastrointestinal videoscope (GIF-XP260N; Olympus) was orally inserted into the stomach to observe the upper gastrointestinal tract. During the examination, patients were placed on their left side. EGD for all patients was performed by one endoscopist and one assistant nurse.
Premedication with anticholinergic agents or glucagon was not used. Lidocaine (8%) was sprayed into the posterior pharynx of all patients before insertion of the endoscope to reduce the gag reflex. Then, midazolam (1-5 mg) was administered intravenously for sedation. Adequate monitoring of vital signs and oxygen saturation was performed throughout the examination.
The primary outcome was occurrence of aspiration pneumonia. Secondary outcomes were extent of salivary flow, frequency of saliva suction, and the number of choking episodes during the procedure. Adverse events during and after EGD were also examined. In addition, the oral cavity was meticulously examined after the EGD to determine whether blood blisters or any suction tube fragments were present.
The duration of EGD using the CSM included the time required to bite down on the mouthpiece with the intraoral loop placed inside the left cheek. The level of sedation was defined as follows: mild, conscious sedation; moderate, between conscious and deep sedation; and deep, deep sedation. None means no use of sedatives. The extent of salivary flow was defined as follows: grade 1, no flow of saliva from mouth; grade 2, flow to the cheek; grade 3, flow to the ear; and grade 4, flow to hair or clothing. When a gurgling sound was heard in the oropharyngeal region, the assistant nurse promptly suctioned the saliva using the suction catheter (Nipro Suction Catheter® 14-Fr, Nipro). Choking episodes were counted each time they occurred during the examination, while consecutive coughs or chokes were counted as one choking episode.
The data are expressed as medians with ranges. Data were analyzed using the unpaired Mann-Whitney U test and Fisher’s exact test. The level of statistical significance was P < 0.05. All analyses were performed using the SPSS 21.0 software package (SPSS Inc., Chicago, IL, United States).
A total of 196 subjects (115 men and 81 women, median age 62 years (range, 33-99 years) were recruited during the study period; all were considered eligible. Patients were divided equally into the CSM group and conventional mouthpiece groups (both n = 98). The patients’ characteristics are summarized in Table 1. There were no significant differences between the two groups in sex, age, biopsy procedure, duration of the examination and depth of sedation.
| CSM | MB-142 | P value | |
| Sex, male/female | 56/42 | 59/39 | 0.125 |
| Age, yr, median (range) | 66 (33-99) | 56 (35-96) | 0.269 |
| Biopsy (yes/no) | 30:68 | 24:74 | 0.344 |
| Duration of procedure, min, median (range) | 8 (4-21) | 7 (3-21) | 0.194 |
| Sedation, none/mild/moderate/deep | 11/7/17/63 | 17/3/8/70 | 0.090 |
Obvious aspiration pneumonia was not observed in any of the participating patients. The extent of salivary flow was significantly less in patients with the CSM than in patients with the conventional mouthpiece (P < 0.001) (Figure 3A). Although there was no statistical significance, less frequent suctioning and choking episodes were observed in patients with the CSM than in patients with the conventional mouthpiece (P = 0.082, and P = 0.084, respectively) (Figure 3B, C). In addition, no patients in the CSM group required saliva suctioning during the procedure. Complete failure of suctioning function did not occur in any patients with the CSM. In addition, neither blood blisters nor fragments of the PVC suction tubes were observed in the mouths of patients who used the CSM. No other significant adverse events were observed in any of the patients.
This is the first attempt to control salivary flow by continuous suctioning during screening EGD examination. Previously, little attention has been paid to the troubles and complications associated with endoscopy-related salivary flow. This study showed that, during EGD, salivary flow did not extend as far out of the mouth in patients with the CSM as in patients with the conventional mouthpiece. Moreover, fewer suctioning and choking episodes were observed in patients with the CSM, although the difference was not statistically significant.
The most relevant finding of this study is that the CSM could reduce the extent of salivary flow during screening EGD. As shown in the results, the grade of extent of salivary flow was higher in patients with the conventional mouthpiece, despite relatively short examination times. In contrast, patients with the CSM discharged less saliva during the procedure. This advantage implies that use of the CSM during EGD could prevent exposure of the patient’s body or clothing and operating bed to saliva, resulting in relief for the patient from the discomfort associated with drooling of saliva. Moreover, reduced contamination of the operating bed with saliva could decrease the effort, time and cost required for cleanup.
In the present study, use of the CSM tended to reduce the frequencies of saliva suction and choking episodes during screening EGD, although statistical differences were not observed. The fact that there were no episodes of suctioning in the CSM group could imply that the assistant nurse’s time and effort can be directed towards other, more important tasks during EGD. Reduced choking episodes from use of the CSM may decrease the complication of aspiration during EGD, although no aspiration pneumonia was observed in patients in both groups, perhaps due to the small number of patients in this study. Thus, use of this equipment, which can be easily prepared with no special materials and at a low cost, is recommended during screening EGD.
Moreover, the CSM’s continuous suction creates airflow in the oral cavity, which may reduce the discomfort in the oral cavity caused by endoscopy. In the questionnaire administered after EGD, 3 of 11 patients in the CSM group who did not use sedation answered that continuous suction during the procedure was comfortable. In this study, most of the patients were sedated with midazolam and could not comment about the CSM after the procedure. Future studies should confirm the level of comfort associated with use of the CSM during EGD performed without sedation.
Administration of anticholinergic agents is an alternative strategy to reduce salivary secretion and peristaltic activity of the gut during EGD. However, these agents cannot be used in patients with heart disease, glaucoma or prostate enlargement. In contrast, the CSM can be used in all patients because its use is not associated with any serious adverse effects. Thus, the improved mouthpiece would be superior to anticholinergics in terms of controlling salivary secretion during EGD.
The CSM may also be effective in endoscopic procedures other than EGD. Recently, we reported that the CSM is effective during PEG[2]. Besides EGD and PEG, many other kinds of time-consuming upper endoscopic procedures have become commonplace, such as endoscopic submucosal dissection and peroral double-balloon enteroscopy. Since these procedures are also associated with an increased risk of aspiration[3,4], use of the CSM may be recommended in all patients who undergo these procedures. Hence, the usefulness of this item in various procedures should be evaluated in the future.
This study had several limitations. First, neither the endoscopist nor the assistant nurse was blind as to which mouthpiece was used. Since the shape of the mouthpiece was different from conventional mouthpieces, blinding was not possible. Second, the number of patients was too small to evaluate some endoscopy-related complications, such as the frequency of aspiration pneumonia, the primary outcome of this study. This could be partly attributed to the study design, since the diagnosis of aspiration pneumonia was based on patients’ symptoms alone. The reported rate of aspiration pneumonia with conventional EGD methods is 3.94%, as assessed by 18F-FDG PET scan[1]. Therefore, the advantage of the CSM in terms of aspiration needs to be confirmed in studies that are designed for evaluating subclinical aspiration pneumonia and in older patients who have difficulty swallowing. Third, several factors may have influenced the outcome of this study. In particular, the amount of midazolam administered (1-5 mg) for sedation varied widely. The sedative agent might have influenced the extent of salivary flow. To overcome this limitation, it would have been preferable if we had defined the amount of sedative agent to be administered in mg/kg. Finally, use of the CSM involves a certain amount of time and cost. However, construction of a single CSM costs no more than $1 (1 US dollar), in addition to the cost of the MB-142 mouthpiece.
The CSM reduced the extent of salivary flow during EGD. Moreover, it tended to reduce the frequencies of suction and choking episodes during EGD. This type of simple and inexpensive device is expected to reduce not only patient discomfort, but also the burden on medical staff during EGD. Therefore, use of the device in routine clinical practice is highly recommended.
Screening esophagogastroduodenoscopy (EGD) is a common examination that is useful in detecting upper gastrointestinal disease. Hence, it is increasingly performed for patients. However, more attention should be paid to the risk of aspiration during the procedure. One of the most important factors correlating with aspiration is salivary flow. No mouthpiece has previously been designed to control salivary flow during endoscopic examination.
A new continuous suction mouthpiece (CSM) was developed and its usefulness during percutaneous endoscopic gastrostomy (PEG) was recently reported.
This is the first attempt to control salivary flow by continuous suctioning during screening EGD examination. Previously, little attention had been paid to the troubles and complications associated with endoscopy-related salivary flow. This study showed that, during EGD, salivary flow did not extend as far out of the mouth in patients with the CSM as in patients with the conventional mouthpiece. Moreover, fewer suctioning and choking episodes were observed in patients with the CSM, although the difference was not statistically significant.
The CSM may also be effective in endoscopic procedures other than EGD and PEG.
A mouthpiece is used to protect the endoscope from being bitten and for smooth insertion of the endoscope, without hindrance from the tongue, during EGD.
This is an interesting original article introducing a new continuous suction mouthpiece during EGD. The idea is very good. There was no statistical difference between choking episodes and the incidence of aspiration pneumonia in this article. However, it could reduce the extent of salivary flow during EGD. This is advantageous from a hygienic point of view. Use of this device is a good option during screening EGD and other endoscopic procedures. This device has the potential to make a significant contribution to the practice procedures of readers in the field.
P- Reviewers Amornyotin S, Lee SY, Sakurazawa N S- Editor Gou SX L- Editor A E- Editor Liu XM
| 1. | Hsieh TC, Wu YC, Ding HJ, Wang CH, Yen KY, Sun SS, Yeh JJ, Kao CH. Clinically unrecognized pulmonary aspiration during gastrointestinal endoscopy with sedation: a potential pitfall interfering the performance of 18F-FDG PET for cancer screening. Eur J Radiol. 2011;80:e510-e515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Maekita T, Kato J, Nakatani Y, Enomoto S, Kayama T, Tsuji M, Nakaya T, Muraki Y, Deguchi H, Ueda K. Usefulness of a continuous suction mouthpiece during percutaneous endoscopic gastrostomy: A single-center, prospective, randomized study. Dig Endosc. 2012;Epud ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Akasaka T, Nishida T, Tsutsui S, Michida T, Yamada T, Ogiyama H, Kitamura S, Ichiba M, Komori M, Nishiyama O. Short-term outcomes of endoscopic submucosal dissection (ESD) for early gastric neoplasm: multicenter survey by osaka university ESD study group. Dig Endosc. 2011;23:73-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Tanaka S, Mitsui K, Tatsuguchi A, Kobayashi T, Ehara A, Gudis K, Sakamoto C. Current status of double balloon endoscopy--indications, insertion route, sedation, complications, technical matters. Gastrointest Endosc. 2007;66:S30-S33. [PubMed] [Cited in This Article: ] |