Published online Mar 16, 2019. doi: 10.4253/wjge.v11.i3.249
Peer-review started: January 23, 2019
First decision: February 20, 2019
Revised: February 23, 2019
Accepted: March 11, 2019
Article in press: March 11, 2019
Published online: March 16, 2019
Hiatal hernia (HH) contents commonly include stomach, transverse colon, small intestine, and spleen but herniation of the pancreas is an extremely rare phenomenon.
79-year-old female with multiple comorbidities presented to emergency department with complaints of weight loss for 6 mo and abdominal pain for one day. Physical examination revealed cachectic and dehydrated female and bowel sounds could be auscultated on the right side of chest. Computed tomography of the chest and abdomen revealed interval enlargement of a massive HH, containing stomach and much of the bowel as well as pancreas and distal extra-hepatic biliary duct, probably responsible for obstructive effect upon same. There was increased prominence of the pancreas consistent with pancreatitis. There was a large HH causing obstructive effect with dilated biliary system along gall bladder wall edema and pancreatitis. Patient clinical status improved with conservative treatment.
HH presenting with acute pancreatitis is a serious diagnostic and therapeutic challenge. The initial management is conservative, even if the abdominal content has herniated to mediastinum. The incentive spirometry can be utilized in the conservative of the large HH. After stabilization of the patient, elective surgical intervention remains the mainstay of the management. Definitive treatment will vary from case to case depending on the acuity of situation and comorbidities.
Core tip: Large hiatal hernia (HH) with inclusion of the pancreas in the hernial sac is extremely rare. We present a case of 79-year-old female with multiple comorbidities presented to emergency department with abdominal pain. Computed tomography of the chest and abdomen showed a large HH causing obstructive effect with dilated biliary system along gall bladder wall edema and pancreatitis. The acute pancreatitis can be from pancreatic trauma or ischemia. Transaminitis can be present from biliary traction or volvulus. As in our case, the conservative management includes incentive spirometry leading to the reduction of the hernia sac is essence of the treatment. The surgical intervention is the definitive treatment, although it varies on case to case based on the comorbidities and patient wishes.
- Citation: Kamal MU, Baiomi A, Erfani M, Patel H. Rare sequalae of hiatal hernia causing pancreatitis and hepatitis: A case report. World J Gastrointest Endosc 2019; 11(3): 249-255
- URL: https://www.wjgnet.com/1948-5190/full/v11/i3/249.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i3.249
Hiatal hernia (HH) is defined as protrusion of the contents of the abdomen into the thoracic cavity through the openings in the diaphragm. Ambore Pare mentioned this disease for the first time in the fifteenth century[1,2]. Most commonly stomach herniates through the diaphragm followed by other organs like transverse colon, small intestine, and spleen etc. Herniation of the pancreas through the hiatus is an extremely rare phenomena and very few cases are reported in literature which include both symptomatic and asymptomatic presentations[3,4]. Pancreatitis is the usual complication of the herniation of pancreas. Rarely, transaminitis is noted due to the traction and the extrinsic biliary obstruction in the hernia sac.
A systematic review of the literature revealed approximately 16 cases pancreatic herniation through diaphragm resulting in pancreatitis[2,5-19]. We came across three cases of transaminitis and pancreatitis due to HH and ours is the fourth case of such presentation ever reported in literature[12,17,19]. Literature search was performed using following electronic bibliographic databases: MEDLINE (Ovid SP and PubMed), Scopus and Web of Science till October of 2018. The bibliographies of retrieved articles were searched to obtain additional articles. The search terms included “hiatal hernia”, “pancreatitis”, “hepatitis”, “transaminitis”, “paraesophageal hernia”, “pancreatic herniation”, “diaphragmatic hernia”, “Percutaneous endoscopic gastrostomy”, “Gastropexy”.
Here we mention a rare case of a patient diagnosed with transaminitis like due to the biliary etiology and pancreatitis due to herniation of the stomach, pancreas, gut and parts of biliary tree into the chest. Our case is novel due to rarity of the pathology and in addition, it depicts the rare association of hepatitis. We have discussed the possible pathogenesis of the acute pancreatitis and transaminitis along with its management. We have also opined on the conservative management strategies for the HH.
79-year-old female with presented to emergency department with one day of abdominal pain.
She described the pain in the right upper quadrant of abdomen as sudden onset, moderate to severe in intensity, non-radiating aching associated with chest discomfort. Patient also reported more about 8 pounds weight loss over the past 5 months and poor appetite.
Her medical comorbidities include Hypertension, hyperlipidemia, Gastroesophageal reflux disease, Osteoarthritis, Rheumatoid arthritis, paraesophageal hernia. Patient denied any toxic habits.
Over the last two years’ patient had the hospitalization for the abdominal pain and dizziness. She is noted to have large HH and managed for the same. She did not report the dysphagia.
Her surgical history included right breast lumpectomy for breast cancer and status post chemotherapy and radiotherapy, left eye surgery for macular degeneration and lumbar laminectomy. She denied any thoracic surgery. Family history was negative for any gastrointestinal cancers.
On presentation her vitals were temperature: 97.1 degrees °F, pulse of 66 bpm, respiratory rate of 19/min and blood pressure of 154/77 mmHg.
On general physical examination she looked cachectic and dehydrated. Abdominal examination revealed non-distended, soft, non-tender abdomen with no rebound tenderness and normal bowel sounds. The bowel sounds could be perceived on the right chest. Exam of the cardiovascular, pulmonary and Neurological was unremarkable. Retrospectively we were not able to corroborate the radiological finding on the physical exam.
The hemoglobin of 13 gm/dL with interval decrease due to intravenous hydration. There is no significant leukocytosis and had thrombocytopenia. The renal function was well preserved. Patient was noted to have the elevated lipase at the time of the presentation. She had transaminitis and elevated alkaline phosphatase with the interval improvement during the hospitalization (Table 1). Her lipase was normal at the normal at the prior hospitalization before 3 mo.
| Laboratory test | Results Before 3 mo | Result Day 1 | Result Day 2 | Result Day 3 |
| Hemoglobin (g/dL) (12-16g/dL) | 11.2 | 13.3 | 10.9 | 10.6 |
| Hematocrit (%) (42%-51%) | 34.6 | 39.7 | 33.2% | 32.8 % |
| Leucocyte count (cells/μL) (4800-10800/μL) | 6200 | 4600 | 3400 | 2900 |
| Platelet count (cells/μL) (150000-400000/μL) | 170000 | 163000 | 135000 | 117000 |
| Blood urea nitrogen (mg/dL) (8-26 mg/dL) | 12 | 8 | 8 | 8 |
| Serum creatinine (mg/dL ) (0.5-1.5 mg/dL) | 1.2 | 0.8 | 0.6 | 0.4 |
| Serum albumin (g/dL) (3.2-4.6 g/dL) | 3.9 | 4.1 | 3.5 | 3.1 |
| Serum total bilirubin (mg/dl) (0.2-1.1 mg/dL) | 0.2 | 0.9 | 0.6 | 0.5 |
| Alkaline phosphatase (unit/L) (43-160 unit/L) | 68 | 254 | 207 | 169 |
| Serum alanine aminotransferase (unit/L) (5-40 unit/L) | 14 | 163 | 100 | 61 |
| Serum aspartate transaminase (unit/L) (9-36 unit/L) | 17 | 258 | 80 | 35 |
| Serum lipase (unit/L) (< 61 unit/L) | 38 | 238 |
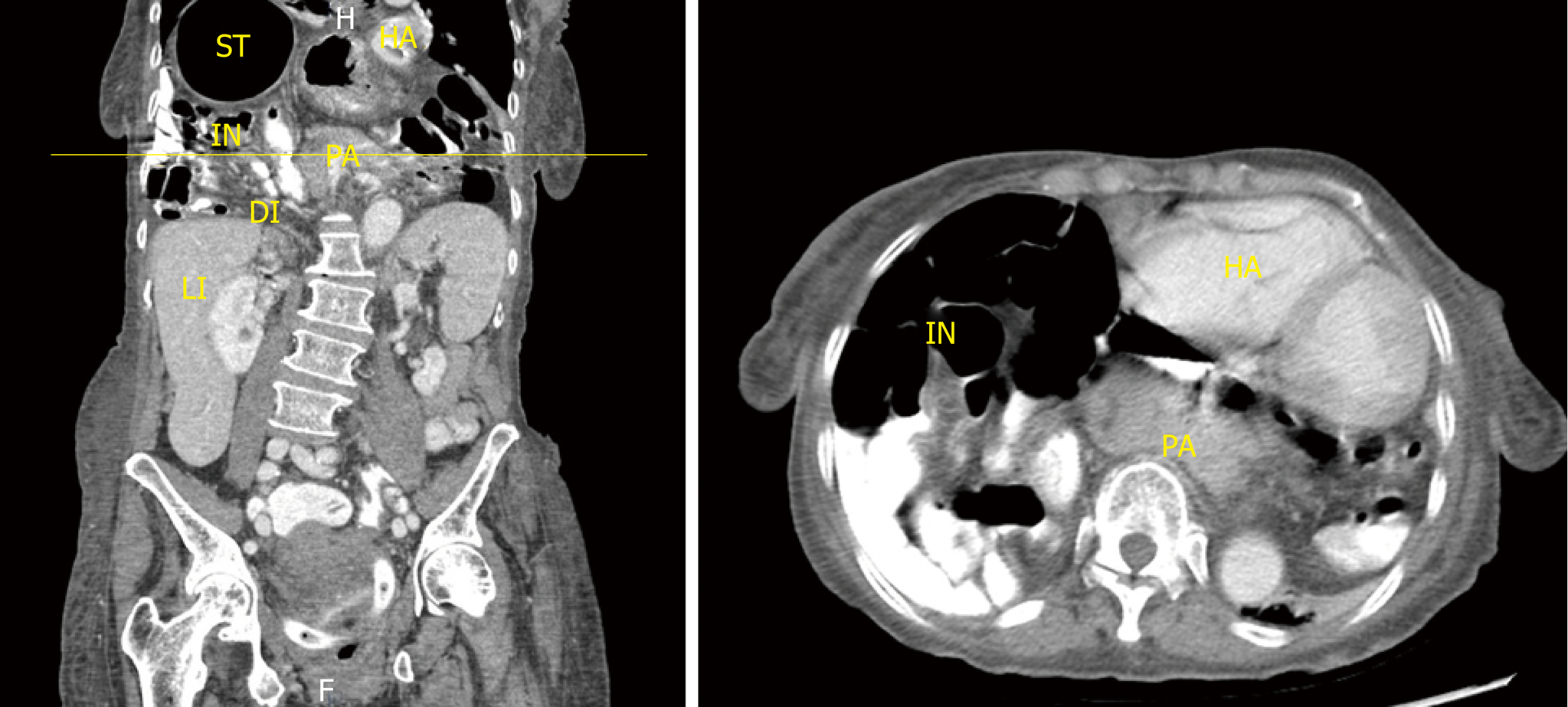
During the index hospitalization she had computed tomography (CT) of the chest and abdomen with oral and intravenous contrast were for the further evaluation (Figure 1) of persistent chest discomfort. CT chest revealed interval enlargement of a massive HH, containing stomach and much of the bowel as well as pancreas and distal extrahepatic biliary duct, probably responsible for obstructive effect upon same. Increased prominence of the pancreas consistent with pancreatitis. Compressive atelectasis in portions of lung adjacent to the hernia, and mass effect upon mediastinum. CT of the abdomen and pelvis with IV contrast reported as large HH causing obstructive effect with dilated biliary system along gall bladder wall edema and pancreatitis.
Ultrasound of the abdomen showed distended gallbladder, with layering sludge, and continued visibility of intrahepatic biliary ductal dilatation; extrahepatic ducts which were seen to be dilated and massive HH.
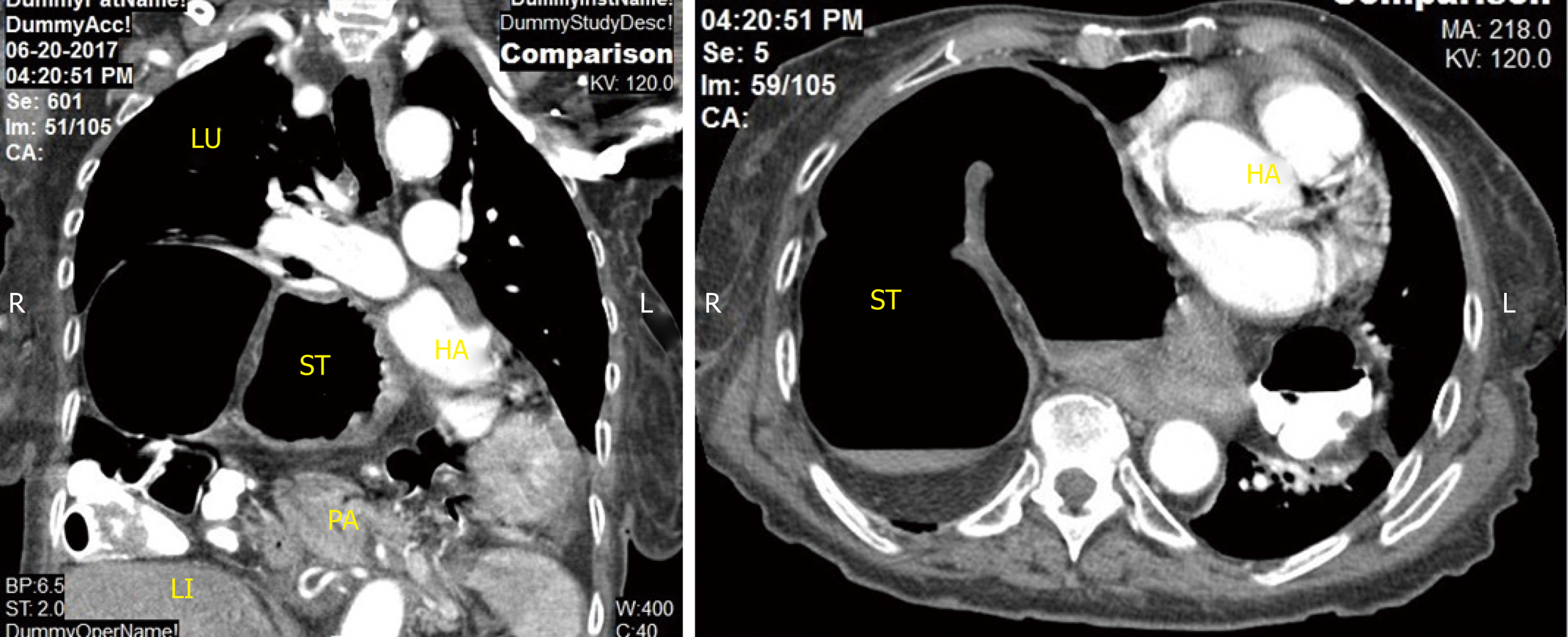
The CT of the chest (Figure 2) performed during the prior hospitalization revealed the large HH with herniation in to chest with the stomach and colon in the its content. The pancreas was not present in the hernia content.
The final diagnosis of the presented case is Pancreatitis and hepatitis as a complication of HH.
For the management of the acute pancreatitis patient was treated with Intravenous hydration with Lactated Ringer's Solution, analgesics along and intensive care monitoring during resuscitation. We acquired surgery consultation for large HH. In view of no signs of bowel obstruction and acute pancreatitis, no emergent or urgent intervention was recommended. The hydration therapy, monitoring the tolerance of the oral dietary intake and the incentive spirometry were the mainstay of the conservative management. The spirometry induced positive pressure is expected to reduce the HH. In view of the advanced age and the high risk from surgical complications, patient and the family perused palliative care. The interval CAT scan to review the reduction hernia content was planned but could not be done.
HH is defined as the trans-hiatal shifting of the abdominal contents into the chest which most commonly include stomach but parts of colon, small intestine, spleen, omentum can herniate along with stomach. Herniation of the pancreas is extremely rare because pancreatic head and duodenum are retroperitoneal and fixed by ligament of treitz[20]. But stretching of the transverse mesocolon due to increase in intra-abdominal pressure causes loosening of the posterior fascia resulting in pancreatic mobilization and herniation[7].
HH is commonly observed in the western population. Women are more effected than men and the percentage of the disease increases with age. However, a recent review of literature by Jäger et al[3] reported 16 cases of large HH with pancreatic involvement having equal numbers of males and females men and 12 cases occurring in patients more than 60 years of age. All patients were symptomatic and diagnosed with CT imaging of the abdomen except one who was asymptomatic and diagnosed on CT chest while being investigated for intractable cough[4].
Patient with HH are usually asymptomatic but sometimes complaint of retrosternal burning, dyspepsia, epigastric and chest pain, nausea, belching, cough and shortness of breath or symptoms of mechanical cholestasis such as jaundice, itching and loose stools[3,9,16]. The exact cause is not known in most of the patients, but congenital presence of diaphragmatic weakness or large hiatus contributes to the development of HH.
The complications of HH include hematemesis associated with esophageal ulcers, esophageal erosions, anemia, gastric or intestinal obstruction and perforation. Pancreatitis and hepatitis occurring with HH are extremely rare. Pancreatitis can occur because of repetitive pancreatic trauma in the diaphragmatic hernia, or ischemia of the pancreas resulting from stretching and traction on the vascular pedicle and partial or complete obstruction of the main pancreatic duct due to abnormal folding[5,6,8,17,18]. Hepatitis can occur due to volvulus of the biliary tree and causing obstruction of the common bile duct. Therefore, etiology of the acute pancreatitis can be from the biliary cholestasis and the vascular insufficiency. It happened in our case but resolved with conservative measures. The diagnosis includes proper history and physical examination, significant elevations of serum lipase and abnormal liver function tests and imaging suggesting of pancreatic inflammation and other relevant abnormalities as mentioned above in our case. We also suggest evaluation of the vascular insufficiency and biliary causes as the etiology for acute pancreatitis in cases of HH. The reduction of the pancreas along with the hernial content is key to the management in all etiology o the acute pancreatitis.
Medical management is done for mildly symptomatic HH with gastroesophageal reflux disease. Serious symptoms of HH like chest discomfort or odynophagia due to severe esophagitis seen with paraesophageal HH require surgical intervention[21].
We suggest incentive spirometry which will be help in expansion of the lungs due to increase in intrathoracic pressure and contribute towards reduction of the herniated contents back into the abdominal cavity. This will reduce the pancreas in the abdominal cavity and cure the inciting factors for the acute pancreatitis.
The surgical modalities include reduction of the HH, repair of the defective hiatal opening, and anti-reflux surgery like fundoplication using abdominal or thoracic approaches depending on the surgeon expertise and patient wishes[21,22]. Rarely biliary stenosis occur during trans-hiatal herniation of the pancreas and duodenum resulting in cholestasis and requiring endoscopic retrograde cholangiopancreatography[3].
We present a rare clinical scenario where our patient developed pancreatitis and transaminitis during pancreatic herniation. Cases of pancreatic herniation causing pancreatitis are rare and therefore ideal management is not well known[2,9]. Some cases were treated with HH surgery in the past[7] but in other cases conservative management including intravenous fluids, pain killers, diet as tolerated was done due to elevated risk of surgery or patient’s refusal of treatment[2,17]. Definitive surgical treatment is required in cases of incarcerated or perforated hernias or cases refractory to medical therapy. Patient with advanced age and multiple comorbidities are also considered poor surgical candidates[21,23]. However, elective repair is needed in younger population with low surgery risk to prevent the development of further serious complications[21].
Pancreatitis in our patient was managed with fluids, analgesia, antiemetics, and gradual advancement of diet as tolerated by the patient. Our patient did not have surgery since the patient only wanted conservative treatment. Other cases are reported in literature mentioning success of the conservative management in which the patients were not the surgical candidates or refused surgical treatment[9,17,19]. In addition, gastropexy with percutaneous endoscopic gastrostomy (PEG) can be used for fixation of the stomach to the anterior abdominal wall in patients with HHs who are poor surgical candidates or refuse more risky and extensive procedures[24]. It is known that insertion of PEG tube helps in anchoring of the stomach to the anterior abdominal wall and therefore decreases the risk of volvulus[24]. We recommended same technique for patients with pancreatic HH who are unable to undergo reparative operations. This appears to be simple procedure where PEG tethers the stomach to the abdominal wall and help prevent further migration of intra-abdominal organs in the thoracic cavity[21,24]. However, symptoms of dysphagia or GERD may not improve with gastropexy[24].
Any intervention in these patients require positive pressure ventilation with or without intubation depending on the clinical status. The positive pressure may assist in reduction of the herniated contents from the thoracic cavity back into the abdominal cavity and may help worsening of the herniation during the procedure.
HH, a common clinical disease, can present rarely with acute pancreatitis. The herniated pancreas in the thoracic cavity is a serious diagnostic and therapeutic challenge. The etiology of the pancreatitis in cases of HH can be vascular or biliary in origin and should be evaluated. Whenever biliary etiology is considered likely for the acute pancreatitis, possibility of the common bile duct stricture should be considered. After stabilization of the patient, elective surgical intervention remains the mainstay of the management. If patient is not amenable to any intervention, intension spirometry should be performed to prevent lung atelectasis. Definitive treatment will vary from case to case depending on the acuity of situation and comorbidities.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
Key words: Hiatal hernia; Pancreatitis; Hepatitis; Para-esophageal hernia, Gastropexy, pancreatic herniation, diaphragmatic hernia, Percutaneous endoscopic gastrostomy.
P- Reviewer: Osawa S, Skok P, Zhu YL S- Editor: Gong ZM L- Editor: A E- Editor: Zhang YL
| 1. | Awais O, Luketich JD. Management of giant paraesophageal hernia. Minerva Chir. 2009;64:159-168. [PubMed] [Cited in This Article: ] |
| 2. | Patel S, Shahzad G, Jawairia M, Subramani K, Viswanathan P, Mustacchia P. Hiatus Hernia: A Rare Cause of Acute Pancreatitis. Case Rep Med. 2016;2016:2531925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Jäger T, Neureiter D, Nawara C, Dinnewitzer A, Ofner D, Lamadé W. Intrathoracic major duodenal papilla with transhiatal herniation of the pancreas and duodenum: A case report and review of the literature. World J Gastrointest Surg. 2013;5:202-206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Katz M, Atar E, Herskovitz P. Asymptomatic diaphragmatic hiatal herniation of the pancreas. J Comput Assist Tomogr. 2002;26:524-525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Kafka NJ, Leitman IM, Tromba J. Acute pancreatitis secondary to incarcerated paraesophageal hernia. Surgery. 1994;115:653-655. [PubMed] [Cited in This Article: ] |
| 6. | Oliver MJ, Wilson AR, Kapila L. Acute pancreatitis and gastric volvulus occurring in a congenital diaphragmatic hernia. J Pediatr Surg. 1990;25:1240-1241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Chevallier P, Peten E, Pellegrino C, Souci J, Motamedi JP, Padovani B. Hiatal hernia with pancreatic volvulus: a rare cause of acute pancreatitis. AJR Am J Roentgenol. 2001;177:373-374. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Cuschieri RJ, Wilson WA. Incarcerated Bochdalek hernia presenting as acute pancreatitis. Br J Surg. 1981;68:669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Wang J, Thaker AM, Noor El-Nachef W, Watson RR. Transhiatal Herniation of the Pancreas: A Rare Cause of Acute Pancreatitis. ACG Case Rep J. 2017;4:e66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Maksoud C, Shah AM, DePasquale J, Baddoura W, Spira R. Transient pancreatic hiatal herniation causing acute pancreatitis--a literature review. Hepatogastroenterology. 2010;57:165-166. [PubMed] [Cited in This Article: ] |
| 11. | Shafiq M, Badshah MB, Badshah MB, Badshah MB, Watkins J. Pancreas herniation into the mediastinum: a case report. BMC Res Notes. 2017;10:450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Laleman W, Vanhoutte E, Vanbeckevoort D, Aerts R, Van Steenbergen W, Verslype C. A puzzling presentation of pancreatitis. Gut. 2008;57:1261, 1287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Lal A, Gupta P, Sinha SK. An unusual cause of abdominal pain in an elderly woman. Gastroenterology. 2015;148:e11-e12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Boyce K, Campbell W and Taylor M. Acute pancreatitis secondary to an incarcerated paraoesophageal hernia: a rare cause for a common problem. Clin Med Insights Case Rep. 2014;7:25-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Do D, Mudroch S, Chen P, Prakash R, Krishnamurthy P. A Rare Case of Pancreatitis From Pancreatic Herniation. J Med Cases. 2018;9:154-156. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Makhoul E, El Mir J, Loutfi T, Assaf Y. Hiatal hernia and acute pancreatitis. Int J Curr Res. 2018;10:68298-68300. [Cited in This Article: ] |
| 17. | Rozas MG, González MM. A rare complication of hiatal hernia. Gastroenterology. 2010;139:e1-e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Lu LX, Payne M, Theobald CN. Education and imaging. Gastroenterology: Diaphragmatic herniation and pancreatitis. J Gastroenterol Hepatol. 2015;30:653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Kumar P, Turp M, Fellows S, Ellis J. Pancreatic herniation: a rare cause of acute pancreatitis? BMJ Case Rep. 2013;2013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Suzuki K, Izumi Y, Ryotokuji T, Miura A, Kato T, Tokura M. Giant hiatal hernia with pancreatic prolapse: report of a case. Available from: http://www.sages.org/meetings/annual-meeting/abstracts-archive/giant-hiatal-hernia-with-pancreatic-prolapse-report-of-a-case. [Cited in This Article: ] |
| 21. | Kohn GP, Price RR, DeMeester SR, Zehetner J, Muensterer OJ, Awad Z, Mittal SK, Richardson WS, Stefanidis D, Fanelli RD; SAGES Guidelines Committee. Guidelines for the management of hiatal hernia. Surg Endosc. 2013;27:4409-4428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 245] [Cited by in F6Publishing: 237] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 22. | Pearson JB, Gray JG. Oesophageal hiatus hernia: long-term results of the conventional thoracic operation. Br J Surg. 1967;54:530-533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 19] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: operation or observation? Ann Surg. 2002;236:492-500; discussion 500-501. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 293] [Cited by in F6Publishing: 210] [Article Influence: 9.5] [Reference Citation Analysis (0)] |