Peer-review started: August 24, 2016
First decision: September 27, 2016
Revised: October 24, 2016
Accepted: November 21, 2016
Article in press: November 22, 2016
Published online: January 18, 2017
In the last decades the prevalence of non-alcoholic fatty liver disease (NAFLD) has increased as a consequence of the childhood obesity world epidemic. The liver damage occurring in NAFLD ranges from simple steatosis to steatohepatitis, fibrosis and cirrhosis. Recent findings reported that fatty liver disease is related to early atherosclerosis and cardiac dysfunction even in the pediatric population. Moreover, some authors have shown an association between liver steatosis and cardiac abnormalities, including rise in left ventricular mass, systolic and diastolic dysfunction and epicardial adipose tissue thickness. In this editorial, we provide a brief overview of the current knowledge concerning the association between NAFLD and cardiac dysfunction.
Core tip: Recently, growing scientific evidences suggest that obese children with non-alcoholic fatty liver disease are more predisposed to cardiovascular disease. Interestingly, this association seems to be independent from adiposity. In fact, based on recent findings, it has been proposed that liver steatosis plays an independent role in determining early atherosclerosis and cardiac dysfunction.
- Citation: Di Sessa A, Umano GR, Miraglia del Giudice E, Santoro N. From the liver to the heart: Cardiac dysfunction in obese children with non-alcoholic fatty liver disease. World J Hepatol 2017; 9(2): 69-73
- URL: https://www.wjgnet.com/1948-5182/full/v9/i2/69.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i2.69
Currently, non-alcoholic fatty liver disease (NAFLD) represents the major cause of chronic liver disease in childhood and is considered a multisystem disease that affects many extra-hepatic organs[1]. Experimental evidence suggests that children with NAFLD have a higher risk of developing end stage liver disease than the general population of United States of same age and gender[2]. Moreover, NAFLD has emerged as an independent risk factor for cardiovascular diseases (CVD)[3,4], including coronary artery disease and cardiac dysfunction[5-8].
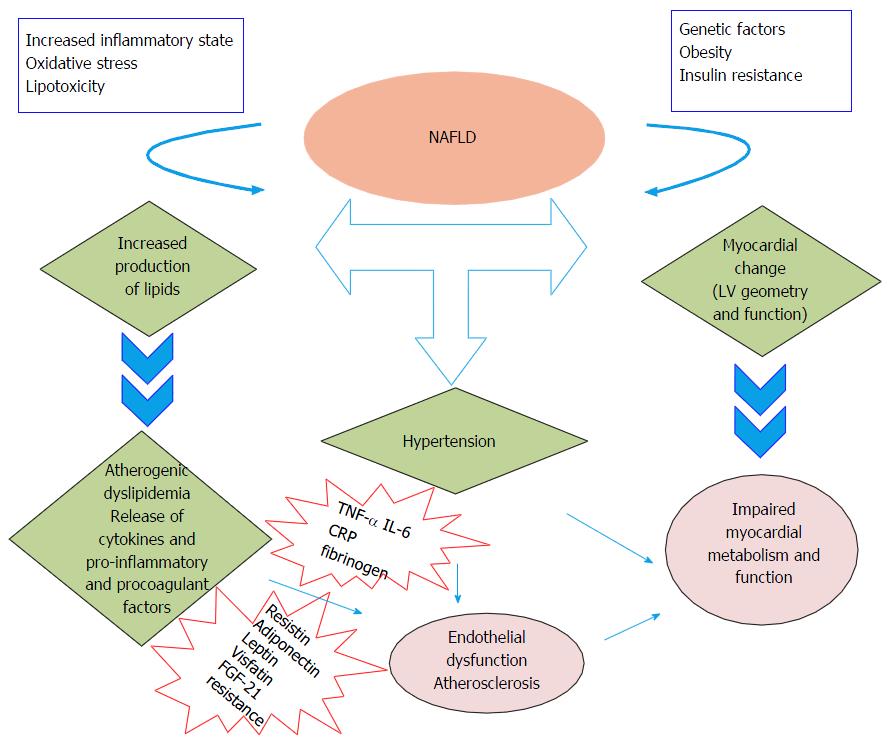
The molecular mechanisms linking NAFLD to cardiovascular complications are still poorly understood[6,8]. Children with NAFLD display increased free fatty acids that may lead to myocardial lipid accumulation with consequent impairments in myocardial substrate metabolism and efficiency and, finally, cardiac dysfunction[7,8]. Moreover, the presence of a low-grade inflammatory state in these patients contributes to the release of several mediators that amplify this condition[6,8]. Therefore, it has been hypothesized that intra-hepatic fat might exert a key pathogenetic role in developing cardio-metabolic complications (Figure 1).
In the last 20 years, NAFLD has become the most common liver disease in pediatrics[1], as result of the increased prevalence of early onset obesity[2-4]. Although NAFLD develops in the context of insulin resistance related to obesity, it is possible that a parental effect exists. As suggested by experimental studies in rats, in fact, paternal and maternal obesity during preconception could lead to obesity, glucose metabolism abnormalities and liver steatosis in the offspring[5].
NAFLD represents an independent risk factor for CVD as it is associated with dyslipidemia, insulin resistance and alterations of cardiac function independent of the degree of obesity[3,4].
Recent studies[2,3,6] have shown that atherosclerosis and alterations of cardiac function may occur already during childhood, as demonstrated by the presence of early onset subclinical atherosclerosis as measured by impaired flow-mediated vasodilation and increased carotid artery intimal medial thickness as well as by the presence of abnormalities in myocardial structure and function in obese children and adolescents[3,4] (Table 1).
| Ref. | Study design and methods | Population (n) | Main findings |
| Bonci et al[4] | Systematic review and meta-analysis Systematic literature search for papers from January 2000 to September 2014 | 12 observational studies: 9 studies based on adult population and 3 studies performed in pediatric population were selected | Children with NAFLD were not different from those without for LV mass Both children with and without NAFLD presented an increased LV mass compared to controls However children with NAFLD presented higher E/e’ ratio rather those without NAFLD |
| D’Adamo et al[7] | Cross-sectional study NAFLD diagnosis performed by MRI Evaluation of VAT Lipoprotein particle characterized by MRS | Mean age 14.6 yr Obese African American (33) Obese Hispanic (33) | In multiple regression analyses liver fat accumulation resulted independently and significantly related to large VLDL concentrations |
| Sert et al[14] | Cross-sectional study NAFLD diagnosis performed by ultrasound and elevated serum alanine aminotransferase Pulsed and tissue doppler Echocardiography | Mean age 13.3 yr Healthy (68) Obese with NAFLD and elevated ALT (97) | NAFLD children showed increased CIMT and abnormalities of both LV structure and function LV CIMT and LV mass were positively related to HOMA-IR in obese children with NAFLD |
| Alp et al[15] | Cross-sectional study NAFLD diagnosis performed by liver biopsy Echocardiography Tissue doppler Echocardiography | Obese without NAFLD and low ALT (83) Mean age 12 yr Healthy (150) Obese with NAFLD at United States (93) Obese without NAFLD at United States (307) | NAFLD group had increased epicardial fat thickness, end-systolic thickness of the interventricular septum, and larger LV mass, as well as LV systolic and diastolic dysfunction |
| Pacifico et al[18] | Cross-sectional study NAFLD diagnosis performed by MRI | Mean age 12.5 yr Healthy (18) | Children with NAFLD presented signs of left ventricular dysfunction compared to children without NAFLD Subjects with a more severe NASH had a worse cardiac dysfunction |
| Singh et al[19] | Liver biopsy for NASH in 41 subjects Echocardiography Cross-sectional study NAFLD diagnosis performed by MRS Echocardiography | Obese with NAFLD at MRI (54) Obese without NAFLD at MRI (54) Mean age 15 yr Lean (14) Obese with Intrahepatic triglyceride content (15) Obese with increased Intrahepatic triglyceride content (15) | Obese adolescents with NAFLD show a worse systolic and diastolic functions rather than lean and obese adolescents without NAFLD independent from anthropometric parameters and blood pressure |
Despite this evidence, the relationship between NAFLD and cardiovascular alterations is still poorly understood. Moreover, it is unclear whether there is a causal relationship between intra-hepatic fat accumulation and alterations of cardiac dynamics or whether the two phenomena are just independent complications of obesity.
It is possible that intra-hepatic fat accumulation may be a pathogenic determinant of CVD. In fact, NAFLD can lead to atherosclerosis by causing an abundant secretion from the liver of lipoproteins [large very low density lipoproteins (VLDL)][7], which, in obese individuals with NAFLD, are abundant in oxidized fatty acids[8,9]. The higher concentration of large VLDL results in a high concentration in plasma of very small LDL, which in turn are a major contributor to the atherosclerotic plaque[7], and their accumulation within the plaque would ultimately lead to ischemic events. NAFLD per se, in fact, is a hyperlipidemic state in which adipose tissue insulin resistance[10] and enhanced hepatic de novo lipogenesis[11] lead to an abnormal accumulation of fat in the liver, turning the hepatocytes in a fat producing factory.
It is important to remember that myocardial atherogenesis occurs very early in life. Seminal studies in the Bogalusa cohort showed that atherosclerosis often begins in pediatric age[12], as demonstrated by the fact that fatty streaks are detected already in the aorta and the coronary arteries of children[6,13]. Since NAFLD can begin during childhood in obese children, it is reasonable to think that it can be an important determinant of these early events observed already in the pediatric population.
While, the association between NAFLD and atherosclerosis could be easily explained by the abundance of circulating lipids present in obese children with NAFLD, it is more difficult to explain the relationship between NAFLD and cardiac function and geometry[14,15]. It has been reported that adolescents with NAFLD show an impaired systolic and diastolic function and an increased left ventricular mass compared to both healthy controls and age and gender matched obese adolescents without NAFLD[14,15] (Table 1).
To explain this observation several pathogenic mechanisms have been hypothesized, including the role of the liver as a generator of circulating mediators that could be involved in the cardiac remodeling[3,11,16,17]. In fact, the presence of a low-grade inflammatory state in patients obese patients with NAFLD and insulin resistance contributes to release of several cytokines and adipokines (e.g., IL-6, TNF-alpha, visfatin, FGF-21, adiponectin, resistin, leptin) that amplify this condition and worsen the metabolic phenotype[3,11,17]. Whether the trigger for this condition, usually refereed to as “sterile inflammation”, is NAFLD or insulin resistance per se is unclear, but a large body of evidence suggests that inflammatory cytokines may be the link among fatty liver, insulin resistance and myocardial changes[3,17]. In fact, adiponectin, a strong insulin sensitizer, seems to be decreased in patients with NAFLD and some studies have suggested that low adiponectin levels may affect cardiac function and atherogenic risk. In contrast, patients with NAFLD experience also an increased production of pro-inflammatory and pro-atherogenic cytokines (IL-6, IL-12, TNF-alpha), which in turn worsens insulin resistance, mostly through the down-regulation of insulin-receptor-substrate and by affecting gluconeogenesis[3,17], these compounds could also affect the cardiac morphology and dynamics. More importantly, some data suggest that fibroblast growth factor 21 (FGF-21), a protein synthetized and secreted by the liver in high amounts in obese subjects with fatty liver, might play a role in cardiac hypertrophy[16]. Some investigators have speculated that FGF-21 resistance occurring in NAFLD could led to cardiac damage in NAFLD patients[16].
On the other hand, given that NAFLD is associated with high systolic blood pressure[18] it could be also argued that changes in myocardial structure might be the consequence of high blood pressure[18]. Against the latter hypothesis, there is the evidence that changes in cardiac morphology observed in children with NAFLD do not resemble the cardiac adaptation consequence of high blood pressure[19]. In fact, hypertension increases left ventricular (LV) mass and changes heart morphology as a result of overload. Recent findings reported that obese children both with and without NAFLD showed no differences in LV mass and posterior wall thickness, while children with NAFLD were more likely to present low LV strain rate - a load - independent parameter that expresses LV elastance and deformation-than those without NAFLD. Therefore, the authors suggested that NAFLD affects myocardial fiber organization leading to systolic and diastolic dysfunction[19].
Besides the large amount of literature suggesting an association between NAFLD and CVD, the pathophysiologic mechanisms underlying these associations are far from being clear, therefore, in the future more studies should be focused on this area of research to unravel those mechanisms and to develop novel therapeutic strategies.
Moreover, we need to establish also whether NAFLD could be considered a marker of subclinical atherosclerosis as well as a cardiovascular risk factor even at a very early age. In fact, because of its strong relationship with CVD, NAFLD diagnosis could represent a red flag for the presence of high cardiovascular risk. In this scenario the prevention and treatment of NAFLD may play a crucial role in avoiding not only end-stage liver disease but also CVD.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Abenavoli L, Marchesini GM, Marzuillo P, Rocha R, Souza-Mello V S- Editor: Kong JX L- Editor: A E- Editor: Li D
| 1. | Loomba R, Sirlin CB, Schwimmer JB, Lavine JE. Advances in pediatric nonalcoholic fatty liver disease. Hepatology. 2009;50:1282-1293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 209] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 2. | Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58:1538-1544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 483] [Cited by in F6Publishing: 510] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 3. | Pacifico L, Chiesa C, Anania C, De Merulis A, Osborn JF, Romaggioli S, Gaudio E. Nonalcoholic fatty liver disease and the heart in children and adolescents. World J Gastroenterol. 2014;20:9055-9071. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 17] [Reference Citation Analysis (0)] |
| 4. | Bonci E, Chiesa C, Versacci P, Anania C, Silvestri L, Pacifico L. Association of Nonalcoholic Fatty Liver Disease with Subclinical Cardiovascular Changes: A Systematic Review and Meta-Analysis. Biomed Res Int. 2015;2015:213737. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Ornellas F, Souza-Mello V, Mandarim-de-Lacerda CA, Aguila MB. Programming of obesity and comorbidities in the progeny: lessons from a model of diet-induced obese parents. PLoS One. 2015;10:e0124737. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Pais R, Giral P, Khan JF, Rosenbaum D, Housset C, Poynard T, Ratziu V. Fatty liver is an independent predictor of early carotid atherosclerosis. J Hepatol. 2016;65:95-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | D’Adamo E, Northrup V, Weiss R, Santoro N, Pierpont B, Savoye M, O’Malley G, Caprio S. Ethnic differences in lipoprotein subclasses in obese adolescents: importance of liver and intraabdominal fat accretion. Am J Clin Nutr. 2010;92:500-508. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Santoro N, Caprio S, Giannini C, Kim G, Kursawe R, Pierpont B, Shaw MM, Feldstein AE. Oxidized fatty acids: A potential pathogenic link between fatty liver and type 2 diabetes in obese adolescents? Antioxid Redox Signal. 2014;20:383-389. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Santoro N, Caprio S, Feldstein AE. Oxidized metabolites of linoleic acid as biomarkers of liver injury in nonalcoholic steatohepatitis. Clin Lipidol. 2013;8:411-418. [PubMed] [Cited in This Article: ] |
| 10. | D’Adamo E, Cali AM, Weiss R, Santoro N, Pierpont B, Northrup V, Caprio S. Central role of fatty liver in the pathogenesis of insulin resistance in obese adolescents. Diabetes Care. 2010;33:1817-1822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 160] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 11. | Santoro N, Caprio S, Pierpont B, Van Name M, Savoye M, Parks EJ. Hepatic De Novo Lipogenesis in Obese Youth Is Modulated by a Common Variant in the GCKR Gene. J Clin Endocrinol Metab. 2015;100:E1125-E1132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | Zhang H, Zhang T, Li S, Li Y, Hussain A, Fernandez C, Harville E, Bazzano LA, He J, Chen W. Long-term Impact of Childhood Adiposity on Adult Metabolic Syndrome Is Modified by Insulin Resistance: The Bogalusa Heart Study. Sci Rep. 2015;5:17885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Lamotte C, Iliescu C, Libersa C, Gottrand F. Increased intima-media thickness of the carotid artery in childhood: a systematic review of observational studies. Eur J Pediatr. 2011;170:719-729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Sert A, Aypar E, Pirgon O, Yilmaz H, Odabas D, Tolu I. Left ventricular function by echocardiography, tissue Doppler imaging, and carotid intima-media thickness in obese adolescents with nonalcoholic fatty liver disease. Am J Cardiol. 2013;112:436-443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Alp H, Karaarslan S, Selver Eklioğlu B, Atabek ME, Altın H, Baysal T. Association between nonalcoholic fatty liver disease and cardiovascular risk in obese children and adolescents. Can J Cardiol. 2013;29:1118-1125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Santoro N, Caprio S. Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis in obese adolescents: a looming marker of cardiac dysfunction. Hepatology. 2014;59:372-374. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Abenavoli L, Peta V. Role of adipokines and cytokines in non-alcoholic fatty liver disease. Rev Recent Clin Trials. 2014;9:134-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 18. | Pacifico L, Di Martino M, De Merulis A, Bezzi M, Osborn JF, Catalano C, Chiesa C. Left ventricular dysfunction in obese children and adolescents with nonalcoholic fatty liver disease. Hepatology. 2014;59:461-470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 19. | Singh GK, Vitola BE, Holland MR, Sekarski T, Patterson BW, Magkos F, Klein S. Alterations in ventricular structure and function in obese adolescents with nonalcoholic fatty liver disease. J Pediatr. 2013;162:1160-1168, 1168.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |