Published online Jan 15, 2003. doi: 10.3748/wjg.v9.i1.179
Revised: July 16, 2002
Accepted: July 22, 2002
Published online: January 15, 2003
AIM: To elucidate the role of NF-κB activation in the development of multiple organ dysfunction (MOD) during acute obstructive cholangitis (AOC) in rats.
METHODS: Forty-two Wistar rats were divided into three groups: the AOC group, the group of bile duct ligation (BDL group), and the sham operation group (SO group). All the animals in the three groups were killed in the 6th and 48th hour after operation. Morphological changes of vital organs were observed under light and electron microscopy. NF-κB activation was determined with Electrophoretic Mobility Shift Assay (EMSA). Arterial blood gas analyses and the serum levels of lactate dehydrogenase (LDH), alanine aminotransferase (ALT), blood urea nitrogen (BUN) and creatinine were performed. The concentrations of TNF-α and IL-6 in plasma were also measured.
RESULTS: The significant changes of histology and ultrastructure of vital organs were observed in AOC group. By contrast, in BDL group, all the features of organs damage were greatly reduced. Expression of NF-κB activation in various tissues increased in AOC group when compared to other two groups. At 6 h, the arterial pH in three groups was 7.52 ± 0.01, 7.46 ± 0.02, and 7.45 ± 0.02, and the blood pCO2 was 33.9 ± 0.95 mmHg, 38.1 ± 0.89 mmHg, 38.9 ± 0.94 mmHg, there was difference in three groups (P < 0.05). At 48 h, the blood pHvalues in three groups was 7.33 ± 0.07, 7.67 ± 0.04, and 7.46 ± 0.03, and blood HCO3- was 20.1 ± 1.29 mmol·L-1, 26.7 ± 1.45 mmol·L-1 and 27.4 ± 0.35 mmol·L-1, there was also difference in three groups (P < 0.05). In AOC group, Levels of LDH, ALT, BUN and creatinine were 16359.9 ± 2278.8 nkat·L-1, 5796.2 ± 941.9 nkat·L-1, 55.7 ± 15.3 mg/dl, and 0.72 ± 0.06 mg/dl, which were higher than in SO group (3739.1 ± 570.1 nkat·L-1, 288.4 ± 71.7 nkat·L-1, 12.5 ± 2.14 mg/dl, and 0.47 ± 0.03 mg/dl) (P < 0.05). Levels of plasma TNF-α and IL-6 in AOC at 48 h were 429 ± 56.62 ng·L-1 and 562 ± 57 ng·L-1, which increased greatly when compared to BDL group (139 ± 16 ng·L-1, 227 ± 43 ng·L-1) and SO group (74 ± 10 ng·L-1, 113 ± 19 ng·L-1) (P < 0.05).
CONCLUSION: The pathological damages and the NF-κB activation of many vital organs exised during AOC. These findings have an important implication for the role of NF-κB activation in MOD during AOC.
- Citation: Tu B, Gong JP, Feng HY, Wu CX, Shi YJ, Li XH, Peng Y, Liu CA, Li SW. Role of NF-κB in multiple organ dysfunction during acute obstructive cholangitis. World J Gastroenterol 2003; 9(1): 179-183
- URL: https://www.wjgnet.com/1007-9327/full/v9/i1/179.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i1.179
In humans with acute obstructive cholangitis (AOC) or other sepsis, the onset of multiple organ dysfunction (MOD), especially involving the liver, the heart, the lungs, and the kidneys, is a well known complication that is associated with a high mortality rate[1-10]. MOD in either humans or animals appears to emerge as a consequence of progressive development of activation of mononuclear phagocytes system and an unregulated release into the blood of a variety of proinflammatory mediators (interleukins, cytokines, chemokines)[11-14]. NF-κB is highly activated at sites of inflammation in diverse diseases and can induce transcrition of proinflammatory cytokines[15-17]. For example, NF-κB is overexpressed in neutrophi, peripheral blood mononuclear cells (PBMC), dendritic cells (DC), and Kupffer cell, and so on. Its activity may enhance recruitment of inflammatory cells and production of proinflammatory mediators like IL-1, IL-6, IL-8, and TNF-α[18-21]. These events may be associated with the development of MOD.
In our original study of patients with AOC, the changes of NF-κB activation were documented[1], but evidence of MOD and the effects of NF-κB were not assessed. In the current studies, we observed the pathological changes of the damages of many vital organs and correlated the role of NF-κB activation with MOD in animal model with AOC.
E. coli and type IV of collagenase were obtained from Sigma Chemical Company (St. Louis, Mo.). The kits of TNF-α and IL-6 were obtained from Beijing Bang Bing Co.. Other reagents were purchased from Ke Hua Co. or Zhong Sheng Co..
Forty-two male Wistar rats, weighing 250-300 g, were obtained from the Laboratory Animal Center of Chongqing University of Medical Science. The animals were fed with standard rat food and water ad libitum for 1 wk before use and kept in a climate-controlled environment with a 12 h light-dark cycle. The animals were handled in accordance with the guidelines set by the Experimental Animals Society of Chongqing University of Medical Science. These animals were randomized into three groups: the AOC group, the group of bile duct ligation (BDL), and sham operation (SO). All the animals in these groups were killed in the 6th and 48th hour after operation. Seven rats from each group at each time point were examined.
All rats were starved overnight and underwent an upper midline laparotomy with an intraperitoneal injection of 30 mg·kg-1 sodium pentobarbital for anesthesia. In AOC group, a median incision was made on the upper abdomen. The common bile duct was mobilized and doubly ligated. 0.2 ml of the E. coli suspension (5 × 1012 cfu·L-1) was injected into the ligated common bile duct. In BDL group, the common bile duct was doubly ligated but no E. coli suspension was injected. In SO group, neither E. coli suspension injection nor common bile duct ligation was done, but only routine operative procedure was performed.
Morphological changes of liver, heart, lungs, and kidneys were observed by light microscope and transmission electron microscope (TEM). These samples from different organs were fixed with 10% buffered formalin or 2.5% glutaraldehyde immediately. For optical microscopy, the tissue blocks were embedded in paraffin, and the sections were stained with hematoxylin and eosin (H&E). For TEM, the tissue blocks were embedded in Epon 618 resin and ultrathin sections were stained with uranyl acetate and lead citrate. A transmission electron microscope (JEM-2000) was used.
Isolation of nuclear proteins Nuclear proteins were isolated as previously described[1,22]. In brief, the liver, heart, lungs, and kidneys tissues were placed in 0.8 mL of ice-cold hypotonic buffer [10 mmol·L-1 HEPES (pH7.9), 10 mL KCl, 0.1 mmol·L-1 EDTA, 0.1 mmol·L-1 ethylene glycol tetraacetic acid, 1 mmol·L-1 DTT; Protease inhibitors (aprotinin, pepstatin, and leupeptin, 10 mg·L-1 each)]. The homogenates were incubated on ice for 20 min, vortexed for 20 s after adding 50 μL of 10 per cent Nonidet P-40, and then centrifuged for 1 minute at 4 °C in an Eppendorf centrifuge. Supernatants were decanted, the nuclear pellets after a single wash with hypotonic buffer without Nonidet P-40 were suspended in an ice-cold hypertonic buffer [20 mmol·L-1 HEPES (pH7.9), 0.4 mol·L-1 NaCl, 1 mmol·L-1 EDTA, 1 mmol·L-1 DTT; Protease inhibitors], incubated on ice for 30 min at 4 °C, mixed frequently, and centrifuged for 15 min at 4 °C. The supernatants were collected as nuclear extracts and stored at -70 °C. Concentrations of total proteins in the samples were determined according to the method of Bradford.
Electrophoretic mobility shift assay (EMSA) NF-κB binding activity was performed in a 10-uL binding reaction mixture containing 1 × binding buffer [50 mg·L-1 of double-stranded poly (dI-dC), 10 mmol·L-1 Tris-HCl (pH7.5), 50 mmol·L-1 NaCl, 0.5 mmol·L-1 EDTA, 0.5 mmol·L-1 DTT, 1 mmol·L-1 MgCl2, and 100 mL·L-1 glycerol], 5 μg of nuclear protein, and 35 fmol of double-stranded NF-κB consensus oligonucleotide (5’-AGTTGAGGGGACTTTCCCAGG-3’) that was endly labeled with γ-32 P(111TBq mmol-1 at 370GBq L-1) using T4 polynucleotide kinase. The binding reaction mixture was incubated at room temperature for 20 min and analyzed by electrophoresis on 7 per cent nondenaturing polyacrylamide gels. After electrophoresis the gels were dried by Gel-Drier (Bio-Rad Laboratories, Hercules, CA) and exposed to Kodak X-ray films at -70 °C. The binding bands were quantified by scanning densitometer of a Bio-Image Analysis System.
In some animals, a carotid artery catherior was placed through an anterior cervical area, and arterial blood samples were collected to measure blood lactate, pH, pO2, pCO2, and HCO3-using a blood gas analyer.
Blood was obtained from the inferior vena cava at the time of sacrifice, heart, liver, kidney injury were assessed by measuring th e seru m lactate deh y dro g en ase (LDH), alanin e aminotransferase (ALT), blood urea nitrogen (BUN) and creatinine, respectively, which were performed with an Automatic Biochemical Analyser.
The concentrations of TNF-α and IL-6 in plasma were measured by a commercially available enzyme-linked immunosorbent assay (ELISA) according to the manufacture instructions which has a low detection limit of 50 ng·L-1. Briefly, microtitre plates were coated with anti TNF-α or IL-6 mAb overnight at room temperature on a plate shaker and then, after they had been blocked, samples were added. The detecting antibody was biotinylated anti TNF-α or IL-6. The results were determined at 492 nm with DG 3022 Enzyme Linkage Essay Instrument.
The results are presented as means ± SEM. Data sets were analyzed with a one-way ANOVA. The differences were regarded significant when the P value was less than < 0.05.
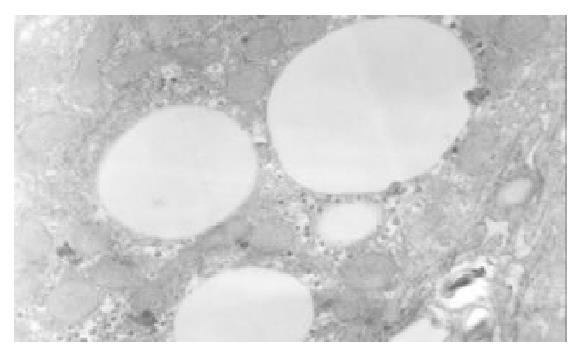
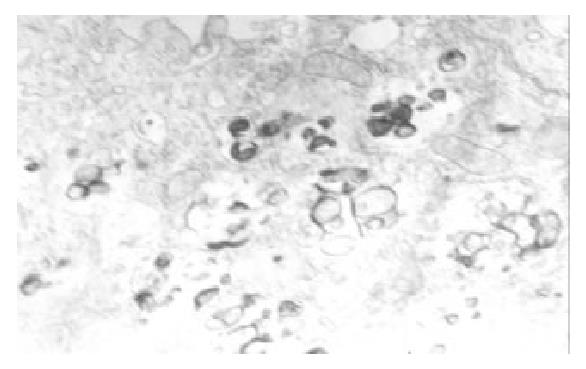
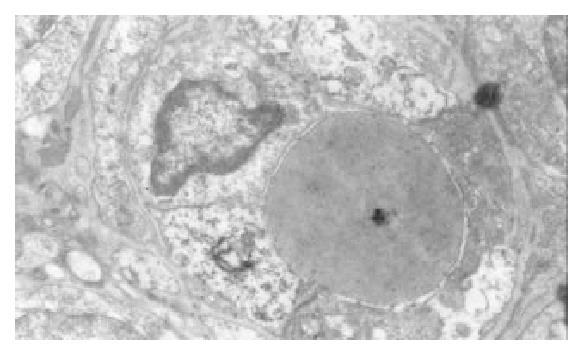
In AOC group, in the liver, there was multifocal and patchy lytic necrosis. hepatocytes showed swelling and partly fatty degeneration, focal cytoplasmic degeneration and many myelin figures could be seen in the cytoplasm (Figure 1), Kupffer cells showed proliferation and many myelin figures in the cytoplasm (Figure 2). In the lungs, polymorphonuclears neutrophil (PMN) aggregated in alveolar capillary. In the heart, mitochondria were swollen or even vacuolated (Figure 3). In the kidneys, there was extensive fusion of foot processes of podocytes in glomeruli. The cells had lost their cell membranes and exhibited mitochondrial swelling together with intracellular edema in proximal convoluted tubules (Figure 4).
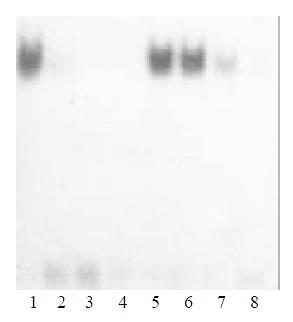
In AOC group, The NF-κB activity increased significantly in liver, nearly fivefold over other organs after 6 h. At 48 h, the NF-κB activity increased also significantly in lung and heart besides liver (Figure 5). In BDL group and SO group, the active form of NF-κB was minimal in hepatic tissue and other tissues.
In AOC group, arterial blood gases showed early respiratory alkalosis and late metabolic acidosis. At 6 h there was a mild respiratory alkalosis, with the arterial pHrising from 7.45 ± 0.02 to 7.52 ± 0.01, the blood pCO2 fell from a value of 37.9 ± 0.86 to 34.23 ± 0.89. At 48 h, similar group showed evidence of metabolic acidosis, with the blood pHvalues falling from 7.46 ± 0.003 to 7.33 ± 0.007, and blood HCO3- (mmol·L-1) falling from 27.4 ± 0.35 to 20.1 ± 1.29. In contrast, in BDL group, the blood pHand pCO2 values were the same as those values obtained in SO group (Table 1).
| Parameter | Early Phase (6 h) | Late Phase (48 h) | ||||
| AOC | BDL | SO | AOC | BDL | SO | |
| pH | 7.52 ± 0.01a | 7.46 ± 0.02 | 7.45 ± 0.02 | 7.33 ± 0.07a | 7.67 ± 0.04 | 7.46 ± 0.03 |
| pCO2 (mmHg) | 33.9 ± 0.95a | 38.1 ± 0.89 | 38.9 ± 0.94 | 40.4 ± 4.23 | 37.8 ± 3.51 | 37.5 ± 0.72 |
| HCO3- (mmol/L) | 26.6 ± 0.63 | 28.3 ± 0.86 | 27.8 ± 1.04 | 20.1 ± 1.57a | 26.7 ± 1.45 | 27.82 ± 1.25 |
| pO2 (mmHg) | 105.1 ± 6.4 | 108.3 ± 4.2 | 106.5 ± 5.8 | 67.3 ± 6.9a | 104.7 ± 5.3 | 110.7 ± 4.6 |
Biochemical parameters in three groups were showed in Table 2.
| Parameter | Early Phase (6 h) | Late Phase (48 h) | ||||
| AOC | BDL | AOC | BDL | AOC | BDL | |
| LDH (nkat·L-1) | 13632.7 ± 891.8a | 4107.4 ± 951.9 | 3655.7 ± 576.8 | 16359.9 ± 2278.8a | 6793 ± 885.1c | 3742.4 ± 570.1 |
| ALT (nkat·L-1) | 2213.8 ± 391.7a | 343.4 ± 103.3 | 311.7 ± 91.7 | 5796.2 ± 941.9a | 955.2 ± 175c | 288.4 ± 75 |
| BUN (mg/dl) | 16.3 ± 13.3 | 12.9 ± 2.8 | 11.8 ± 2.2 | 55.7 ± 15.3a | 16.7 ± 4.6 | 12.5 ± 2.14 |
| Cr (mg/dl) | 0.48 ± 0.03 | 0.42 ± 0.02 | 0.41 ± 0.03 | 0.72 ± 0.06a | 0.51 ± 0.03 | 0.47 ± 0.03 |
In AOC group, Levels of plasma TNF-α and IL-6 increased greatly in 6 h and 48 h. Levels of two cytokines were over 4-fold and 5-fold higher than that in other two groups. In BDL group, the levels of TNF-α and IL-6 in 48 h increased modestly when compared to that in SO group (P < 0.05). Low levels of TNF-α and IL-6 was detectable in plasama in SO group (Table 3).
AOC in humans often leads to progressive MOD, which is still associated with a high mortality rate[1-5]. Recent studies showed NF-κB is rapidly in response to many pathologic signals that may be relevant during surgical trauma, including cytokines, adhesion molecules, endotoxin, hypoxia, and shear[23-27]. Activation of NF-κB results in the transcrition of genes that can participate in the inflammatory reaction by inducing the production of cytokines, immunoreceptors, and cell adhesion molecules[28-32]. These cytokines and proinflammatory mediators are therefore a potentially attractive target inducing MOD during sepsis and endotoxemia[33-47]. Information on the role of NF-κB in sepsis, AOC and MOD is limited but shows that NF-κB is increased during inflammation and sepsis[1,18].
The role of NF-κB activation in sepsis and in complication such as MOD is a debatable issue. Pennington et al[20] observed the degree of NF-κB activation with severity of acute appendicitis and found that NF-κB binding activity is elevated in these patients and correlates with symptoms longer than 24 hours. Arnalich et al[18] determined NF-κB activation in peripheral blood monouclear cells of 34 patients with severe sepsis and serial concentrations of inflammary cytokines and resulted the prognosis value of early measrement of NF-κB activity in patients with severe sepsis. Gong and Paterson et al[1,20] determined NF-κB activation in mononuclear and neutrophils from critically ill patients and compared NF-κB activation with circulating concentrations of IL-6, IL-8 and soluble intercellular adhension molecule (sICAM)-1, and found NF-κB activation in patients systemic inflammaty response syndrome, which increased makedly before death. However, Chen et al[48] observed intrahepatic changes in TNF-α and NF-κB activation in Sprague-Dawley rats with cecal ligation and puncture, and their results implied NF-κB activation was not linked to the outcome in sepsis. In our original study of patients with AOC, the changes of NF-κB activation were documented, but evidence of MOD and the effects of NF-κB were not assessed. So it would be helpful to further analyze the expression with the inflamed tissues. There is, however, no published information about a key role of NF-κB in development of multiple organ dysfunction during biliary infection. In this study, we investigated the role NF-κB in the development of MOD in rats with AOC.
The present study shows a correlation among the pathological damages of many vital organs, NF-κB activation and release of proinflammatory cytokines. This is only one published investigation about the correlation of NF-κB activation and MOD during AOC. The present study demonstrated that NF-κB activation plays a key role during AOC. The finding that prompt surgical inflammary condition of the inflammary focus results in a rapid normalization of NF-κB activation adds further validity to this assay.
Perhape other important finding of this study was the marked difference in NF-κB levels among various organs during AOC. During AOC, Expression of NF-κB was observed first in liver at 6 h. At 48 h, NF-κB also expressed in the lung, the heart, and the kidney besides the liver. The liver was the main organ which was injured by bacteria during AOC, liver and other organs influence each other in their function, the liver plays a key role in host defense. Matuschak et al reported that the liver failure affected on the incidence and resolution of the adult respiratory distress syndrome. Seki et al[49] Hepatocytes produce acute phase protein and complement in bacterial infections. KCs are activated by various bacterial stimuli, including LPS and bacterial superantigens, and produce IL-12 and other monokines. So the liver plays a crucial role in the first line of defense against bacterial defections[50-52]. However, if this defense system is inadequately activated, sepsis and shock associated with MOD takes place. It was found in our previous study that when liver was injured, especially KCs function failed, gram-negative bacteria normally restricted to the biliary tract invaded the bloodstream and were trapped in vital organs, and NF-κB activation occurred, eventually MOD ensued. Further clinical trials are indicated to confirm that this “molecular biology” marker indeed will be a useful clinical tool in the management of the patients with AOC[53-56].
In conclusion, we have shown the expression of NF-κB and the pathological changes of the damages occurred in many vital organs, especially in liver during AOC. These findings have an important implication for the role of NF-κB activation in MOD during AOC.
Edited by Liu HX
| 1. | Gong JP, Liu CA, Wu CX, Li SW, Shi YJ, Li XH. Nuclear factor kB activity in patients with acute severe cholangitis. World J Gastroenterol. 2002;8:346-349. [PubMed] [Cited in This Article: ] |
| 2. | Zhi QH. New development of biliary surgery in China. World J Gastroenterol. 2000;6:187-192. [PubMed] [Cited in This Article: ] |
| 3. | Kimmings AN, van Deventer SJ, Rauws EAJ K, Gouma DJ. Systemic inflammatory response in acute cholangitis and after subsequent treatment. Eur J Surg. 2000;166:700-705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Lillemoe KD. Surgical treatment of biliary tract infections. Am Surg. 2000;66:138-144. [PubMed] [Cited in This Article: ] |
| 6. | Parker SJ, Watkins PE. Experimental models of gram-negative sepsis. Br J Surg. 2001;88:22-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 154] [Cited by in F6Publishing: 155] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Tabrizi AR, Zehnbauer BA, Freeman BD, Buchman TG. Genetic markers in sepsis. J Am Coll Surg. 2001;192:106-117; quiz 145-146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Jackson GD, Dai Y, Sewell WA. Bile mediates intestinal pathology in endotoxemia in rats. Infect Immun. 2000;68:4714-4719. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Islam AF, Moss ND, Dai Y, Smith MS, Collins AM, Jackson GD. Lipopolysaccharide-induced biliary factors enhance invasion of Salmonella enteritidis in a rat model. Infect Immun. 2000;68:1-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Erwin PJ, Lewis H, Dolan S, Tobias PS, Schumann RR, Lamping N, Wisdom GB, Rowlands BJ, Halliday MI. Lipopolysaccharide binding protein in acute pancreatitis. Crit Care Med. 2000;28:104-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Kordzaya DJ, Goderdzishvili VT. Bacterial translocation in obstructive jaundice in rats: role of mucosal lacteals. Eur J Surg. 2000;166:367-374. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Kimmings AN, van Deventer SJ, Obertop H, Rauws EA, Huibregtse K, Gouma DJ. Endotoxin, cytokines, and endotoxin binding proteins in obstructive jaundice and after preoperative biliary drainage. Gut. 2000;46:725-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 129] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Bone-Larson CL, Simpson KJ, Colletti LM, Lukacs NW, Chen SC, Lira S, Kunkel SL, Hogaboam CM. The role of chemokines in the immunopathology of the liver. Immunol Rev. 2000;177:8-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Ito Y, Machen NW, Urbaschek R, McCuskey RS. Biliary obstruction exacerbates the hepatic microvascular inflammatory response to endotoxin. Shock. 2000;14:599-604. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Zhao S, Qi Y, Liu X, Jiang Q, Liu S, Jiang Y, Jiang Z. Activation of NF-kappa B in bronchial epithelial cells from children with asthma. Chin Med J (Engl). 2001;114:909-911. [PubMed] [Cited in This Article: ] |
| 16. | West MA, Clair L, Kraatz J, Rodriguez JL. Endotoxin tolerance from lipopolysaccharide pretreatment induces nuclear factor-kappaB alterations not present in C3H/HeJ mice. J Trauma. 2000;49:298-305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Reddy SA, Huang JH, Liao WS. Phosphatidylinositol 3-kinase as a mediator of TNF-induced NF-kappa B activation. J Immunol. 2000;164:1355-1363. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 154] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Paterson RL, Galley HF, Dhillon JK, Webster NR. Increased nuclear factor kappa B activation in critically ill patients who die. Crit Care Med. 2000;28:1047-1051. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 83] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Arnalich F, Garcia-Palomero E, López J, Jiménez M, Madero R, Renart J, Vázquez JJ, Montiel C. Predictive value of nuclear factor kappaB activity and plasma cytokine levels in patients with sepsis. Infect Immun. 2000;68:1942-1945. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 203] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 20. | Pennington C, Dunn J, Li C, Ha T, Browder W. Nuclear factor kappaB activation in acute appendicitis: a molecular marker for extent of disease. Am Surg. 2000;66:914-918; discussion 918-919;. [PubMed] [Cited in This Article: ] |
| 21. | Foulds S, Galustian C, Mansfield AO, Schachter M. Transcription factor NF kappa B expression and postsurgical organ dysfunction. Ann Surg. 2001;233:70-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Rensing H, Jaeschke H, Bauer I, Pätau C, Datene V, Pannen BH, Bauer M. Differential activation pattern of redox-sensitive transcription factors and stress-inducible dilator systems heme oxygenase-1 and inducible nitric oxide synthase in hemorrhagic and endotoxic shock. Crit Care Med. 2001;29:1962-1971. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Kono H, Wheeler MD, Rusyn I, Lin M, Seabra V, Rivera CA, Bradford BU, Forman DT, Thurman RG. Gender differences in early alcohol-induced liver injury: role of CD14, NF-kappaB, and TNF-alpha. Am J Physiol Gastrointest Liver Physiol. 2000;278:G652-G661. [PubMed] [Cited in This Article: ] |
| 24. | Ninomiya-Tsuji J, Kishimoto K, Hiyama A, Inoue J, Cao Z, Matsumoto K. The kinase TAK1 can activate the NIK-I kappaB as well as the MAP kinase cascade in the IL-1 signalling pathway. Nature. 1999;398:252-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 955] [Cited by in F6Publishing: 938] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 25. | Hedin KE, Kaczynski JA, Gibson MR, Urrutia R. Transcription factors in cell biology, surgery, and transplantation. Surgery. 2000;128:1-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 26. | Stärkel P, Horsmans Y, Sempoux C, De Saeger C, Wary J, Lause P, Maiter D, Lambotte L. After portal branch ligation in rat, nuclear factor kappaB, interleukin-6, signal transducers and activators of transcription 3, c-fos, c-myc, and c-jun are similarly induced in the ligated and nonligated lobes. Hepatology. 1999;29:1463-1470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Liu Y, Wang Y, Yamakuchi M, Isowaki S, Nagata E, Kanmura Y, Kitajima I, Maruyama I. Upregulation of toll-like receptor 2 gene expression in macrophage response to peptidoglycan and high concentration of lipopolysaccharide is involved in NF-kappa b activation. Infect Immun. 2001;69:2788-2796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | Jiang Q, Akashi S, Miyake K, Petty HR. Lipopolysaccharide induces physical proximity between CD14 and toll-like receptor 4 (TLR4) prior to nuclear translocation of NF-kappa B. J Immunol. 2000;165:3541-3544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 249] [Cited by in F6Publishing: 259] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 29. | Adib-Conquy M, Adrie C, Moine P, Asehnoune K, Fitting C, Pinsky MR, Dhainaut JF, Cavaillon JM. NF-kappaB expression in mononuclear cells of patients with sepsis resembles that observed in lipopolysaccharide tolerance. Am J Respir Crit Care Med. 2000;162:1877-1883. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 132] [Cited by in F6Publishing: 134] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 30. | Abraham E, Arcaroli J, Shenkar R. Activation of extracellular signal-regulated kinases, NF-kappa B, and cyclic adenosine 5'-monophosphate response element-binding protein in lung neutrophils occurs by differing mechanisms after hemorrhage or endotoxemia. J Immunol. 2001;166:522-530. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Belich MP, Salmerón A, Johnston LH, Ley SC. TPL-2 kinase regulates the proteolysis of the NF-kappaB-inhibitory protein NF-kappaB1 p105. Nature. 1999;397:363-368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 176] [Cited by in F6Publishing: 187] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 32. | Choi JH, Ko HM, Kim JW, Lee HK, Han SS, Chun SB, Im SY. Platelet-activating factor-induced early activation of NF-kappa B plays a crucial role for organ clearance of Candida albicans. J Immunol. 2001;166:5139-5144. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Han DW. The clinical sine of subsequent liver injury induced by gut derived endotoxemia. Shijie Huaren Xiaohua Zazhi. 1999;7:1055-1058. [Cited in This Article: ] |
| 34. | Lin E, Calvano SE, Lowry SF. Inflammatory cytokines and cell response in surgery. Surgery. 2000;127:117-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 388] [Cited by in F6Publishing: 376] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 35. | Li SW, Gong JP, Wu CX, Shi YJ, Liu CA. Lipopolysaccharide induced synthesis of CD14 proteins and its gene expression in hepatocytes during endotoxemia. World J Gastroenterol. 2002;8:124-127. [PubMed] [Cited in This Article: ] |
| 36. | Hardaway RM. A review of septic shock. Am Surg. 2000;66:22-29. [PubMed] [Cited in This Article: ] |
| 37. | Sindram D, Porte RJ, Hoffman MR, Bentley RC, Clavien PA. Synergism between platelets and leukocytes in inducing endothelial cell apoptosis in the cold ischemic rat liver: a Kupffer cell-mediated injury. FASEB J. 2001;15:1230-1232. [PubMed] [Cited in This Article: ] |
| 38. | Wu RQ, Xu YX, Song XH, Chen LJ, Meng XJ. Adhesion molecule and proinflammatory cytokine gene expression in hepatic sinusoidal endothelial cells following cecal ligation and puncture. World J Gastroenterol. 2001;7:128-130. [PubMed] [Cited in This Article: ] |
| 39. | Baldwin AS. Series introduction: the transcription factor NF-kappaB and human disease. J Clin Invest. 2001;107:3-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 773] [Cited by in F6Publishing: 763] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 40. | Assy N, Jacob G, Spira G, Edoute Y. Diagnostic approach to patients with cholestatic jaundice. World J Gastroenterol. 1999;5:252-262. [PubMed] [Cited in This Article: ] |
| 41. | Blunck R, Scheel O, Müller M, Brandenburg K, Seitzer U, Seydel U. New insights into endotoxin-induced activation of macrophages: involvement of a K+ channel in transmembrane signaling. J Immunol. 2001;166:1009-1015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 102] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 42. | Tak PP, Firestein GS. NF-kappaB: a key role in inflammatory diseases. J Clin Invest. 2001;107:7-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3011] [Cited by in F6Publishing: 2989] [Article Influence: 130.0] [Reference Citation Analysis (0)] |
| 43. | Ling YL, Meng AH, Zhao XY, Shan BE, Zhang JL, Zhang XP. Effect of cholecystokinin on cytokines during endotoxic shock in rats. World J Gastroenterol. 2001;7:667-671. [PubMed] [Cited in This Article: ] |
| 44. | Gordon H. Detection of alcoholic liver disease. World J Gastroenterol. 2001;7:297-302. [PubMed] [Cited in This Article: ] |
| 45. | Bai XY, Jia XH, Cheng LZ, Gu YD. Influence of IFN alpha-2b and BCG on the release of TNF and IL-1 by Kupffer cells in rats with hepatoma. World J Gastroenterol. 2001;7:419-421. [PubMed] [Cited in This Article: ] |
| 46. | Wang LS, Zhu HM, Zhou DY, Wang YL, Zhang WD. Influence of whole peptidoglycan of bifidobacterium on cytotoxic effectors produced by mouse peritoneal macrophages. World J Gastroenterol. 2001;7:440-443. [PubMed] [Cited in This Article: ] |
| 47. | Zuo GQ, Gong JP, Liu CA, Li SW, Wu XC, Yang K, Li Y. Expression of lipopolysaccharide binding protein and its receptor CD14 in experimental alcoholic liver disease. World J Gastroenterol. 2001;7:836-840. [PubMed] [Cited in This Article: ] |
| 48. | Chen J, Raj N, Kim P, Andrejko KM, Deutschman CS. Intrahepatic nuclear factor-kappa B activity and alpha 1-acid glycoprotein transcription do not predict outcome after cecal ligation and puncture in the rat. Crit Care Med. 2001;29:589-596. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 49. | Seki S, Habu Y, Kawamura T, Takeda K, Dobashi H, Ohkawa T, Hiraide H. The liver as a crucial organ in the first line of host defense: the roles of Kupffer cells, natural killer (NK) cells and NK1.1 Ag+ T cells in T helper 1 immune responses. Immunol Rev. 2000;174:35-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 272] [Cited by in F6Publishing: 284] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 50. | Wu RQ, Xu YX, Song XH, Chen LJ, Meng XJ. Relationship between cytokine mRNA expression and organ damage following cecal ligation and puncture. World J Gastroenterol. 2002;8:131-134. [PubMed] [Cited in This Article: ] |
| 51. | Gong JP, Wu CX, Liu CA, Li SW, Shi YJ, Li XH, Peng Y. Liver sinusoidal endothelial cell injury by neutrophils in rats with acute obstructive cholangitis. World J Gastroenterol. 2002;8:342-345. [PubMed] [Cited in This Article: ] |
| 52. | Gong JP, Dai LL, Liu CA, Wu CX, Shi YJ, Li SW, Li XH. Expression of CD14 protein and its gene in liver sinusoidal endothelial cells during endotoxemia. World J Gastroenterol. 2002;8:551-554. [PubMed] [Cited in This Article: ] |
| 53. | Shang D, Guan FL, Jin PY, Chen HL, Cui JH. Effect of combined therapy of Yinchenhao Chengqi decoction and endoscopic sphincterotomy for endotoxemia in acute cholangitis. World J Gastroenterol. 1998;4:443-445. [PubMed] [Cited in This Article: ] |
| 54. | Tiscornia OM, Hamamura S, Lehmann ES, Otero G, Waisman H, Tiscornia-Wasserman P, Bank S. Biliary acute pancreatitis: a review. World J Gastroenterol. 2000;6:157-168. [PubMed] [Cited in This Article: ] |
| 55. | Gong JP, Wu CX, Liu CA, Li SW, Shi YJ, Yang K, Li Y, Li XH. Intestinal damage mediated by Kupffer cells in rats with endotoxemia. World J Gastroenterol. 2002;8:923-927. [PubMed] [Cited in This Article: ] |
| 56. | Zhang WZ, Chen YS, Wang JW, Chen XR. Early diagnosis and treatment of severe acute cholangitis. World J Gastroenterol. 2002;8:150-152. [PubMed] [Cited in This Article: ] |