Published online Sep 28, 2021. doi: 10.3748/wjg.v27.i36.6154
Peer-review started: February 25, 2021
First decision: April 29, 2021
Revised: May 13, 2021
Accepted: August 16, 2021
Article in press: August 16, 2021
Published online: September 28, 2021
Meckel’s diverticulum is a common asymptomatic congenital gastrointestinal anomaly. However, its presentation as an inverted Meckel's diverticulum is a rare complication, of which few cases have been reported in the literature.
Here, we report the case of a 33-year-old man with iron deficiency anemia without manifestation of gastrointestinal bleeding. An upper gastrointestinal endoscopy and total colonoscopy were performed, but no abnormalities were found within the observed area. Finally, a capsule endoscopy was performed and offered us a clue to subsequently confirm the diagnosis of inverted Meckel's diverticulum via computed tomography scan. Laparoscopic intestinal resection surgery was performed. The final pathology report described a Meckel’s diverticulum.
Since inverted Meckel's diverticulum is an uncommon disease and its clinical presentation is not specific, it may go undetected by capsule endoscopy. Successful diagnosis and treatment of this disease requires a high index of clinical suspicion.
Core Tip: Inverted Meckel’s diverticulum is an uncommon disease with a wide spectrum of accompanying nonspecific symptoms. We present, here, a case of iron deficiency anemia with negative endoscopic study, in which capsule endoscopy played a key role in confirming the diagnosis. Since inverted Meckel's diverticulum is an uncommon disease with few cases described in the literature, this report aims to contribute more information concerning the clinical characteristics as well as radiological and capsule endoscopy findings of inverted Meckel’s diverticulum that can help clinicians make the correct diagnosis.
- Citation: El Hajra Martínez I, Calvo M, Martínez-Porras JL, Gomez-Pimpollo Garcia L, Rodriguez JL, Leon C, Calleja Panero JL. Inverted Meckel’s diverticulum diagnosed using capsule endoscopy: A case report. World J Gastroenterol 2021; 27(36): 6154-6160
- URL: https://www.wjgnet.com/1007-9327/full/v27/i36/6154.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i36.6154
Meckel’s diverticulum is a common congenital gastrointestinal anomaly which is a remanent of the omphalomesenteric duct[1]. It is often within 100 cm of the ileocecal valve and located in the antimesenteric surface of the ileum[2]. According to autopsy studies, this condition is found in 0.3%-2% of the general population[3,4].
Patients with Meckel’s diverticulum are usually asymptomatic. However, up to 6.4% develop complications that require surgery[5]. The most common complications are gastrointestinal bleeding in association with ectopic gastric and/or pancreatic mucosa, intestinal obstruction, intussusceptions, diverticulitis or volvulus. The inversion of Meckel’s diverticulum is a rare complication with a pathophysiology not clearly understood, that can be a clinical challenge given its diagnostic difficulty. Moreover, the clinical presentation is nonspecific, the most frequent mode of presentation being intussusception, abdominal pain, anemia or gastrointestinal bleeding[6].
Although Meckel’s diverticulum is the most common congenital anomaly of the small bowel, inversion or invagination of the diverticulum is a rare occurrence. To date, there are only around 100 cases in the literature that demonstrate the presence of inverted Meckel’s diverticulum.
Herein, we present the case of iron deficiency anemia without manifestation of gastrointestinal bleeding, in which capsule endoscopy played a key role in the final diagnosis of inverted Meckel's diverticulum.
A 33-year-old male with no significant medical history presented to the emergency room with progressive weakness, easy fatigability and headache. He had no evidence of lower or upper gastrointestinal bleeding and he reported no abdominal pain, nausea, vomiting, anorexia, fever or weight loss.
The patient’s symptoms started 3 wk prior and had worsened over the last 4 d.
There was no significant medical history.
There was no significant medical history.
In the emergency room, the patient was clinically stable, with a normal temperature (36.7 °C). The patient exhibited an oxygen saturation level of 97% while he was breathing ambient air. His blood pressure was 102/61 mmHg and his heart rate was 91 beats per minute. The patient was awake, alert, and fully oriented. Physical examination revealed signs of pallor and an absence of lymphadenopathy, hepatosplenomegaly, bone tenderness or jaundice. Examination of the rectum revealed a few external hemorrhoids, but there was no blood or melena in the rectal vault; there were no skin tags, fissures or palpable masses.
The initial laboratory findings showed low hemoglobin levels (7 g/dL), a white blood cell count of 11250 per mm3, a platelet count of 221000 per mm3 and a C-reactive protein of 1.31 mg/dL. Two pints of packed red blood cells were therefore transfused and the patient was admitted to the gastroenterology department. Electrocardiography (ECG) showed sinus rhythm at 93 beats per minute and the results of the patient’s chest radiography were normal.
The patient’s next blood test, showed a mean corpuscular volume of 72.5 fl, a mean corpuscular hemoglobin of 25.6 pg, and a reticulocyte count of 1%. The patient’s iron level was 38 μg/dL, his ferritin level was 17 ng/mL, and his transferrin saturation was 9%. The hemolysis study was negative. Hence, the patient’s anemia was classified as iron deficiency anemia.
During this period, an upper gastrointestinal endoscopy and a colonoscopy were performed to study the patient’s anemia. The colonoscopy revealed internal hemorrhoids without any other relevant findings while the upper gastrointestinal endoscopy showed no abnormalities. The patient remained stable and was discharged and the study was completed on an outpatient basis with oral iron treatment.
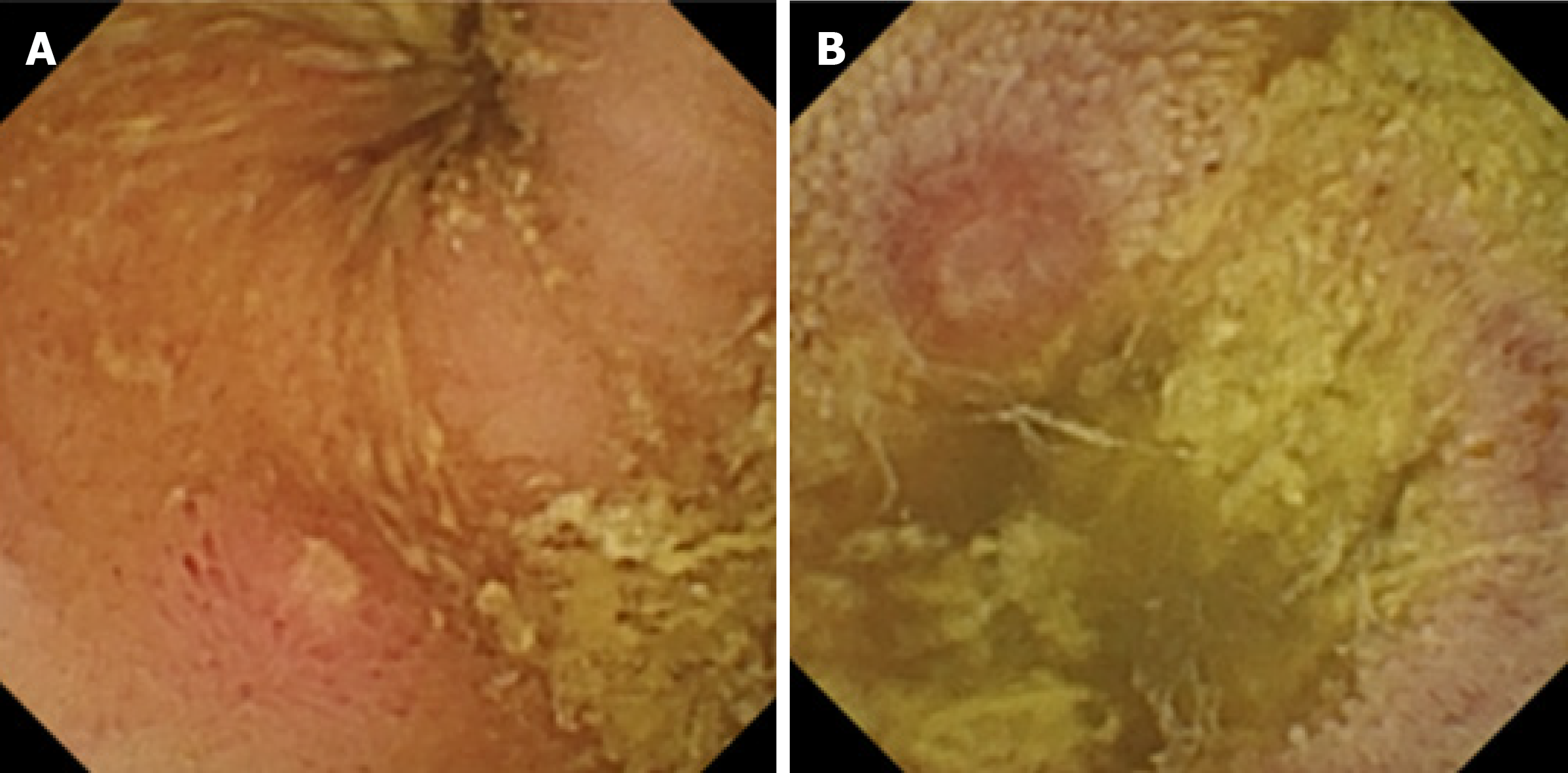
During his visit to the outpatient clinic 3 wk later, the patient remained anemic, with a hemoglobin level of 8.8 g/dL. The anemia study was completed with a capsule endoscopy, which revealed a lifted erosion and mild bulge in the ileum of approximately 8-9 mm in size (Figure 1). These findings of appearance of a subepithelial bulge in the ileum suggested an inverted Meckel diverticulum. Normal intestinal mucosa was seen on the surface of the tumor with a longer small intestine transit time suggestive of Meckel’s diverticulum. A technetium-99m pertechnetate radioisotope scintigraphy (Meckel’s scan) was performed and was negative. The patient subsequently underwent an ultrasound examination, which revealed no pathological findings. Finally, an abdominal computed tomography (CT) was performed and showed a central area of fat attenuation surrounded by a thick collar of soft tissue attenuation (Figure 2) suggestive of inverted Meckel’s diverticulum.
The patient was diagnosed with an inverted Meckel’s diverticulum and underwent a laparoscopic surgery. A large intraluminal polyp-like mass in the mid-ileum was observed. The remainder of the small bowel was normal to the level of the ligament of Treitz. A segmentary resection of the small bowel with adequate margin was performed and side-to-side anastomosis was carried out using a stapling device.
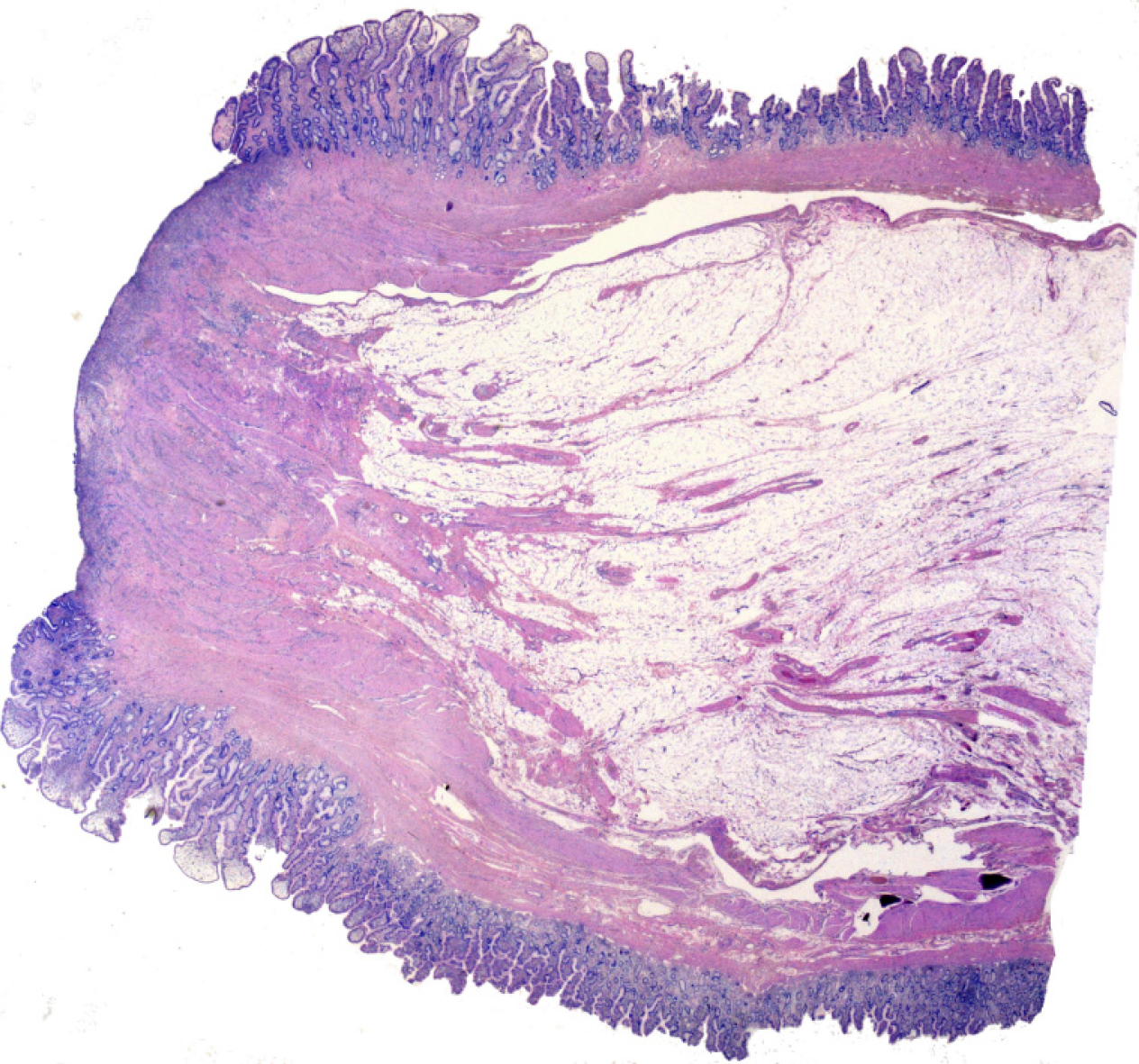
On gross examination, the specimen consisted of a segmental resection of the small bowel of 8 cm × 4 cm × 2.6 cm with a sausage-shaped polypoid lesion.
Histological examination (Figure 3) showed a polypoid lesion, with a central fatty and collagenous core lined with an intestinal type mucosa. A central area of ulceration was seen, with no presence of gastric or pancreatic heterotopia. The final pathology report described a Meckel’s diverticulum.
The patient was diagnosed with an inverted Meckel’s diverticulum and underwent a laparoscopic surgery. A large intraluminal polyp-like mass in the mid-ileum was observed. The remainder of the small bowel was normal to the level of the ligament of Treitz. A segmentary resection of the small bowel with adequate margin was performed and side-to-side anastomosis was carried out using a stapling device.
The patient had an uneventful postoperative course and was discharged 4 d after surgery.
Meckel’s diverticulum is the most common congenital anomaly in the gastrointestinal tract[1] and is often incidentally discovered during evaluations performed for other reasons, as it is usually an asymptomatic condition. However, complications can occur in up to 6.4% of patients[7]. These are more frequent in the pediatric population and mainly involve bowel obstruction with or without intussusception, gastrointestinal hemorrhage, diverticulitis and inflammation, and Littre hernia (hernia involving the bowel segment bearing Meckel's)[4,7].
Inverted Meckel’s diverticulum is an unusual condition that is not yet clearly understood and there are no more than 100 cases reported in literature.
It has been proposed that the mechanism that could produce the inversion is an abnormal peristaltic movement around an ulceration or ectopic tissue. Nevertheless, no ectopic tissue was found in 41% of patients with inverted Meckel’s diverticulum[6]. In this regard, tc-99m pertechnetate scintigraphy can help detect ectopic gastric mucosa and has been used for years as a diagnostic method for Meckel's diverticulum, especially in children, with a sensitivity of 92.1% and a specificity of 95.4%[8]. In adults, the sensitivity of this method is significantly less (54%)[9]. No cases of diagnosis of inverted Meckel's diverticulum by scintigraphy have been described, while there is only 1 case with gastric and pancreatic mucosa in the histopathological sample where the scintigraphy was negative[10]. Our patient’s scintigraphy was negative. Therefore, this suggests that a negative scan does not preclude the presence of ectopic mucosa and the diagnosis of possible inverted Meckel’s diverticulum.
This inversion of the Meckel’s diverticulum can lead to a complete intussusception of the bowel or compromise blood flow to that bowel, ulceration and then gastrointestinal bleeding. The bleeding can also be explained by repetitive mechanical trauma to the mucosa from the reversible intussusception.
As in our patient, anemia or gastrointestinal bleeding are the most frequent clinical manifestations, found in up to 80% of patients[6]. This usually leads to an upper and lower gastrointestinal endoscopy, where the cause of the bleeding cannot be found.
Other clinical manifestations which can occur are abdominal pain (68%) and intussusception (39%). The median age of presentation is 27.7 years, younger than that reported for Meckel’s diverticulum, which has been 33, with a male to female ratio of approximately 2.33:1[6].
Regarding the diagnostic tools, abdominal ultrasonography can contribute to the diagnosis, but often shows nonspecific findings such as thickened intestinal wall, fluid fille target or distended loops of bowel[11,12]. In our case, abdominal ultrasonography revealed no pathological findings.
One of the most useful tools is a CT scan. It usually shows a thickened small intestinal wall, with an elongated, intraluminal, fat-attenuating lesion[13], as in our case. In the case of intussusceptions, a CT scan is especially useful as it can reveal the characteristic “target sign”. Inverted Meckel’s diverticulum is sometimes confused with a lipoma on CT scans because it also consists of macroscopic fatty tissue. However, in most cases, abdominal CT scans provide useful information for the diagnosis and treatment of inverted Meckel's diverticulum[6].
Capsule endoscopy has recently been considered a useful diagnostic tool for diagnosing Meckel’s diverticulum[9,14,15]. However, the role of capsule endoscopy in the identification of Meckel’s diverticulum is not yet clear, with only a few case reports and case series available. Furthermore, in the case of inverted Meckel's diverticulum, the information is very limited, represented by only 2 case reports[16,17]. The capsule findings compatible with inverted Meckel's diverticulum were described as an elevated lesion with normal mucosa[16] or as pedunculated polyp[17].
In our case, the capsule endoscopy images were similar (a subepithelial protruding lesion in the ileum with the presence of blood, hematin, ulcer or erosion) and offered us a clue to subsequently confirm the diagnosis of inverted Meckel's diverticulum. In addition, the clinical suspicion due to the clinical characteristics (such as the fact that the patient was a young man with anemia) and a negative endoscopic study was of great importance for the diagnosis of inverted Meckel's diverticulum.
Regarding the risk of possible intestinal obstruction of the endoscopic capsule due to Meckel's diverticulum, no events have been described.
Surgery is the treatment of choice for symptomatic Meckel’s diverticulum. The general consensus is that it should be treated with resection. In the case of asymptomatic Meckel’s diverticulum, there is some debate. Resection is generally recommended for patients younger than 40-years-old, with diverticulum longer than 2 cm, diverticula with narrow necks, fibrous bands, and/or ectopic gastric tissue, and/or when the diverticulum appears thickened and inflamed[4,6,18].
It is important to note that in cases of anemia without abdominal pain, like that of our patient, it may take a long time for the patient to be diagnosed with inverted Meckel’s diverticulum, given that it is an unusual condition with a nonspecific clinical presentation. Capsule endoscopy is usually performed in those patients with anemia with a normal upper and lower gastrointestinal endoscopy. However, if clinicians are unaware of the characteristics of this lesion, it may go undetected since it is an uncommon disease. Therefore, this report aims to contribute more information concerning the clinical characteristics, radiological findings and especially, the capsule endoscopy findings of inverted Meckel’s diverticulum that can help clinicians suspect that this disease is present and enable them to establish a definitive diagnosis.
To date, inverted Meckel's diverticulum is a pathology that is still not completely well known, with few cases described in the literature. Its clinical presentation is not specific, its most frequent symptoms being anemia or lower gastrointestinal bleeding. Patients are often given an upper and lower gastrointestinal endoscopy which reveals no abnormalities and a subsequent capsule endoscopy. Therefore, increased awareness of the disease and a greater understanding of the features of this lesion in capsule endoscopy findings could ultimately help clinicians make the correct diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Camí MM, Racz I, Sulbaran MN S-Editor: Wang JL L-Editor: Filipodia P-Editor: Li JH
| 1. | Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med. 2006;99:501-505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 171] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 2. | Karadeniz Cakmak G, Emre AU, Tascilar O, Bektaş S, Uçan BH, Irkorucu O, Karakaya K, Ustundag Y, Comert M. Lipoma within inverted Meckel's diverticulum as a cause of recurrent partial intestinal obstruction and hemorrhage: a case report and review of literature. World J Gastroenterol. 2007;13:1141-1143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | WEINSTEIN EC, CAIN JC, REMINE WH. Meckel's diverticulum: 55 years of clinical and surgical experience. JAMA. 1962;182:251-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 74] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg. 2005;241:529-533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 347] [Cited by in F6Publishing: 322] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Cullen JJ, Kelly KA, Moir CR, Hodge DO, Zinsmeister AR, Melton LJ 3rd. Surgical management of Meckel's diverticulum. An epidemiologic, population-based study. Ann Surg. 1994;220:564-8; discussion 568. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 226] [Cited by in F6Publishing: 190] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Rashid OM, Ku JK, Nagahashi M, Yamada A, Takabe K. Inverted Meckel's diverticulum as a cause of occult lower gastrointestinal hemorrhage. World J Gastroenterol. 2012;18:6155-6159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 24] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore). 2018;97:e12154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 120] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 8. | Hosseinnezhad T, Shariati F, Treglia G, Kakhki VR, Sadri K, Kianifar HR, Sadeghi R. 99mTc-Pertechnetate imaging for detection of ectopic gastric mucosa: a systematic review and meta-analysis of the pertinent literature. Acta Gastroenterol Belg. 2014;77:318-327. [PubMed] [Cited in This Article: ] |
| 9. | Krstic SN, Martinov JB, Sokic-Milutinovic AD, Milosavljevic TN, Krstic MN. Capsule endoscopy is useful diagnostic tool for diagnosing Meckel's diverticulum. Eur J Gastroenterol Hepatol. 2016;28:702-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Dujardin M, de Beeck BO, Osteaux M. Inverted Meckel's diverticulum as a leading point for ileoileal intussusception in an adult: case report. Abdom Imaging. 2002;27:563-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | El-Dhuwaib Y, O'Shea S, Ammori BJ. Laparoscopic reduction of an ileoileal intussusception and resection of an inverted Meckel's diverticulum in an adult. Surg Endosc. 2003;17:1157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Karahasanoglu T, Memisoglu K, Korman U, Tunckale A, Curgunlu A, Karter Y. Adult intussusception due to inverted Meckel's diverticulum: laparoscopic approach. Surg Laparosc Endosc Percutan Tech. 2003;13:39-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Takagaki K, Osawa S, Ito T, Iwaizumi M, Hamaya Y, Tsukui H, Furuta T, Wada H, Baba S, Sugimoto K. Inverted Meckel's diverticulum preoperatively diagnosed using double-balloon enteroscopy. World J Gastroenterol. 2016;22:4416-4420. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Wu J, Huang Z, Wang Y, Tang Z, Lai L, Xue A, Huang Y. Clinical features of capsule endoscopy in 825 children: A single-center, retrospective cohort study. Medicine (Baltimore). 2020;99:e22864. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Lin L, Liu K, Liu H, Wu J, Zhang Y. Capsule endoscopy as a diagnostic test for Meckel's diverticulum. Scand J Gastroenterol. 2019;54:122-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Ibuka T, Araki H, Sugiyama T, Takada J, Kubota M, Shirakami Y, Shiraki M, Shimizu M, Suzui N, Miyazaki T. [A case of an elderly patient with inverted Meckel's diverticulum with small intestinal bleeding detected using capsule and double-balloon endoscopies]. Nihon Shokakibyo Gakkai Zasshi. 2017;114:2005-2011. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 17. | Payeras Capó MA, Ambrona Zafra D, Garrido Durán C. Inverted Meckel's diverticulum in an adult patient diagnosed via capsule endoscopy. Rev Esp Enferm Dig. 2018;110:210-211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Lequet J, Menahem B, Alves A, Fohlen A, Mulliri A. Meckel's diverticulum in the adult. J Visc Surg. 2017;154:253-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |