Published online Jan 21, 2019. doi: 10.3748/wjg.v25.i3.287
Peer-review started: November 22, 2018
First decision: December 12, 2018
Revised: December 20, 2018
Accepted: December 27, 2018
Article in press: December 27, 2018
Published online: January 21, 2019
The Na+/Ca2+ exchanger (NCX) protein family is a part of the cation/Ca2+ exchanger superfamily and participates in the regulation of cellular Ca2+ homeostasis. NCX1, the most important subtype in the NCX family, is expressed widely in various organs and tissues in mammals and plays an especially important role in the physiological and pathological processes of nerves and the cardiovascular system. In the past few years, the function of NCX1 in the digestive system has received increasing attention; NCX1 not only participates in the healing process of gastric ulcer and gastric mucosal injury but also mediates the development of digestive cancer, acute pancreatitis, and intestinal absorption. This review aims to explore the roles of NCX1 in digestive system physiology and pathophysiology in order to guide clinical treatments.
Core tip: The Na+/Ca2+ exchange 1 protein (NCX1) is a membrane transporter and participates in the regulation of cellular Ca2+ homeostasis. As we known,NCX1 is expressed widely in various organs and tissues and plays an especially important role in the physiological and pathological processes of nerves and the cardiovascular system. This review aims to explore the roles of NCX1 in digestive system physiology and pathophysiology in order to guide clinical treatments.
- Citation: Liao QS, Du Q, Lou J, Xu JY, Xie R. Roles of Na+/Ca2+ exchanger 1 in digestive system physiology and pathophysiology. World J Gastroenterol 2019; 25(3): 287-299
- URL: https://www.wjgnet.com/1007-9327/full/v25/i3/287.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i3.287
Ca2+ is an important cellular signal. Changes in intracellular Ca2+ control various cellular processes that are relevant to the regulation of normal function and to the development of diseases. These processes include muscle contraction, blood coagulation, nerve excitation, angiogenesis, cell apoptosis[1-3], and the development of cancer[4,5]. The homeostasis of intracellular calcium is controlled by a variety of proteins and ion channels, including the plasma membrane Na+/Ca2+ exchanger (NCX). Members of the NCX family can exchange Na+ and Ca2+ in either direction depending on the transmembrane electrochemical gradients and membrane potential[6], and these exchangers have a two-way transport mode such that under physiological conditions, one Ca2+ ion exits and three Na+ ions enter the cell but the reverse transport occurs under special conditions (such as cancer or inflammation), that is, three Na+ ions exit and one Ca2+ ion enters[7]. The NCX family contains three separate gene products exhibiting differential expression: NCX1, NCX2, and NCX3. NCX1 is widely expressed in mammalian organs and tissues[8], and NCX2 and NCX3 are expressed mainly in nerves and skeletal muscle[9]. Numerous studies have shown that NCX1 is involved in a variety of physiological and pathophysiological processes. For example, in the cardiovascular system, NCX1 can control the contraction and relaxation of vascular smooth muscle[10], while NCX1 can regulate heart rhythm, which is related to arrhythmia[11,12], and participate in the regulation of myocardial ischemia-reperfusion injury[13]. In the nervous system, NCX1 regulates neurotransmitter release[14] and microglia-related functions[15], which is associated with cerebral ischemia-reperfusion and Alzheimer's disease[16,17]. In the urinary system, NCX1 is involved in renal Ca2+ reabsorption and associated with renal ischemia-reperfusion[18,19]. In the endocrine system, NCX1 can regulate insulin secretion[20]. In the immune system, NCX1 is associated with the development of systemic lupus erythematosus[21]. In recent years, NCX1 has been found to be expressed in all of the organs of the digestive system and play important roles in the physiological processes and digestive diseases (such as pancreatitis, gastric ulcer, and gastrointestinal cancers)[22-24], However, the mechanism and function of NCX1 in the gastrointestinal tract have not yet been completely elucidated, particularly relating to certain digestive diseases and tumors. This review intends to explore the roles of NCX1 in digestive system physiology and pathophysiology as well as current treatments utilizing NCX1-based therapeutics.
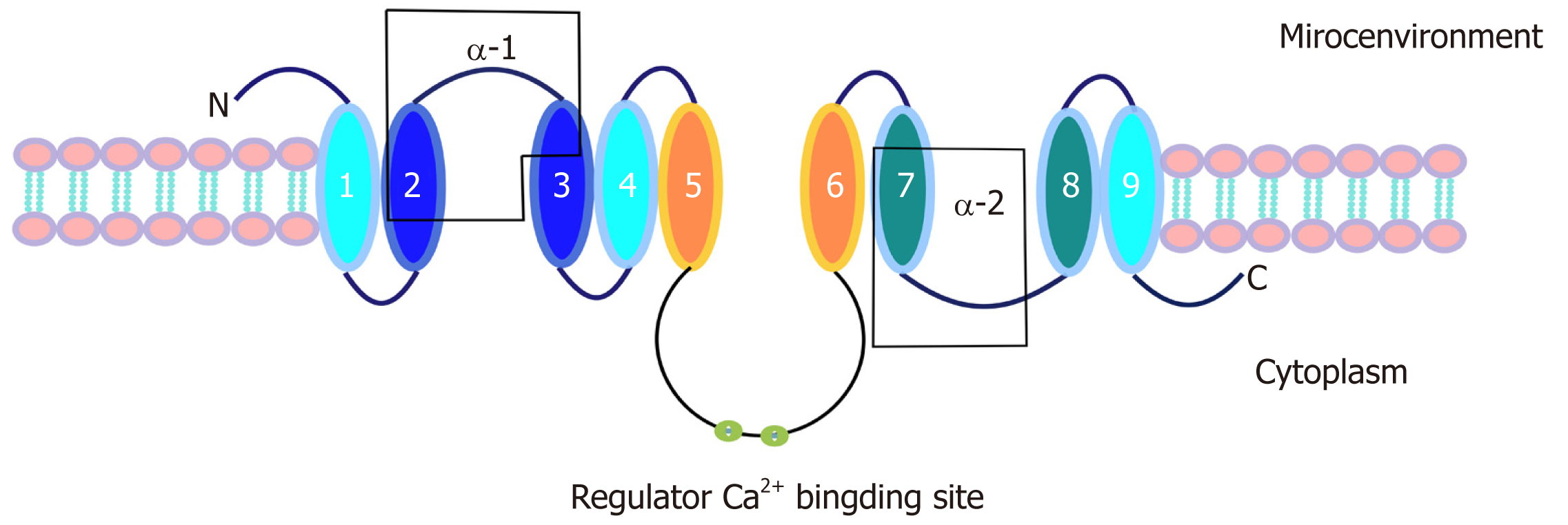
NCX1 is a transmembrane bidirectional transporter with a molecular weight of 110 kDa and consists of 970 amino acids. NCX1 has 9 transmembrane segments, forming a large central cytoplasmic loop between the 5th and 6th transmembrane segments[25,26]. In addition, the NCX1 transmembrane segment has two internal repeat regions, the α1 and α2 repeat regions [27]. The first half of the transmembrane segment, including the α-repeat region, may be involved in ion transport[28-30]. In contrast, the second half, which contains the central cytoplasmic ring, has an inhibitory effect on the entire sodium-calcium exchanger[31,32]. In addition, there are two binding sites that can regulate Na+ and Ca2+[33,34], and there is a secondary Ca2+ adapter site[35] (Figure 1).
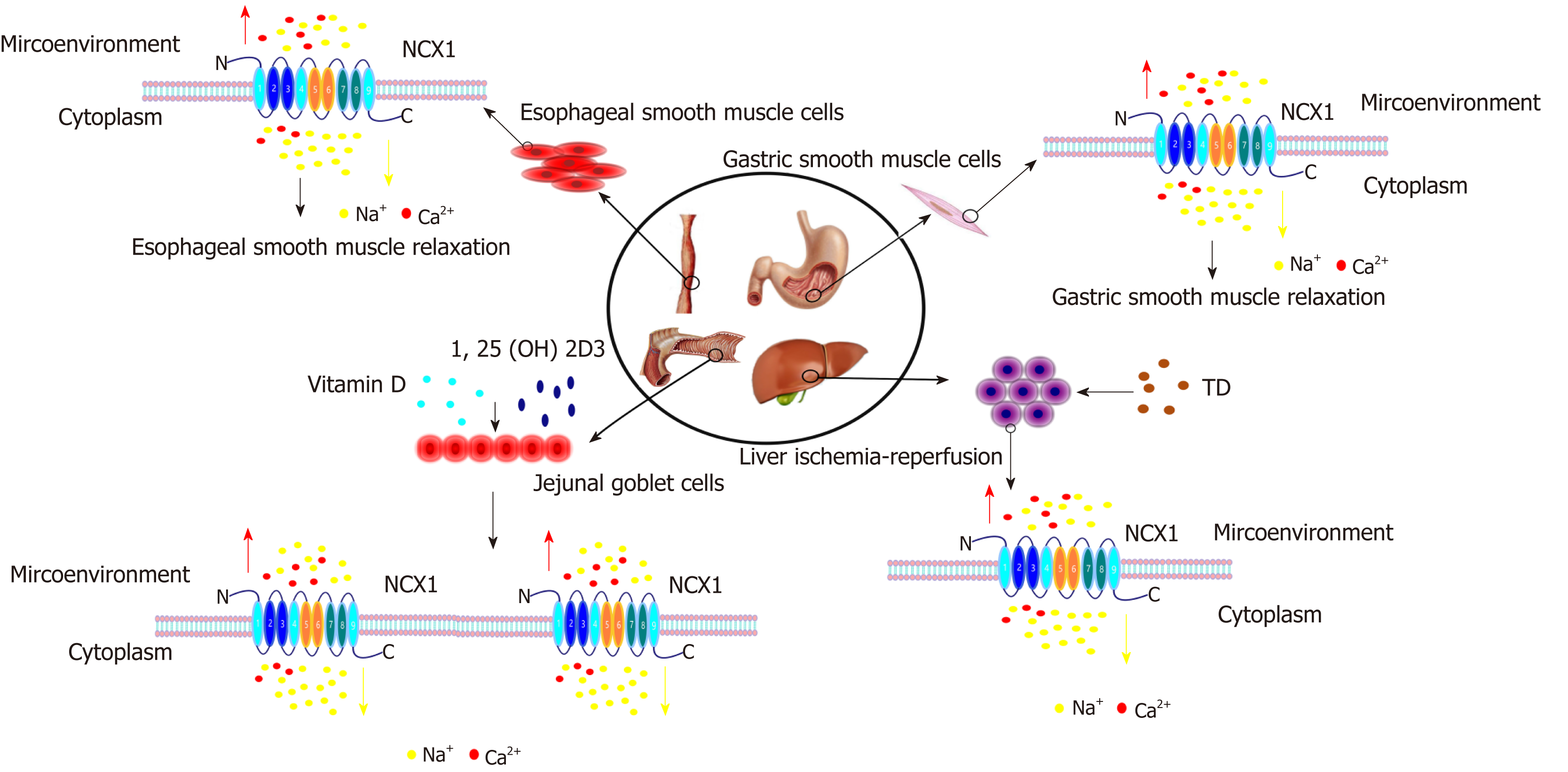
The esophagus is a muscular portion of the digestive tract that transports food from the pharynx to the stomach depending on the contraction of muscle. In normal conditions, the tension of the lower esophageal smooth muscle (LES) depends mainly on the intracellular Ca2+ concentration. A high concentration of intracellular Ca2+ can cause smooth muscle contraction, and a low concentration of Ca2+ causes smooth muscle relaxation[36]. However, the contraction of the esophageal body is mainly dependent on the gradient of extracellular calcium. The occurrence of esophagitis is also closely related to the regulation of Ca2+ in pathological conditions. Calcium channel blockers (CCBs) have been used in the treatment of esophageal-related diseases, such as achalasia[36,37]. Achalasia is a kind of neuropathy where the smooth muscle fiber is not relaxed or cannot relax completely, a partial loss of esophageal body peristalsis occurs, and the motility is not coordinated. Gelfond et al[38] first reported that use of the L-type CCB nifedipine can relax the esophageal smooth muscle to reduce the pressure of the lower esophageal sphincter by blocking the flow of calcium ions into the cells and intracellular calcium release, thereby achieving the purpose of treating achalasia. However, taking CCBs for a long time will cause the LES to become too relaxed and will lead to reflux esophagitis (RE)[39]. There is no definitive evidence as to whether NCX1 plays a regulatory role in RE. However, Kim et al[40] found that NCX1 is widely expressed in the esophageal muscle layer. Furthermore, the estrogen E2-induced inhibition of smooth muscle contraction in the esophagus and the mucus secretion in the esophageal mucosa are mainly achieved by downregulating the expression of calcium-related genes such as NCX1, CaBP-9k, and PMCA1 and decreasing the intracellular calcium level. It is suggested that NCX1 may play an important role in the regulation of contraction and relaxation in the LES. In addition, at present, our research group also confirmed that NCX1 expression was significantly increased along with the expression of TRPC6, TRPV4, and other acid-sensitive calcium channels that have a regulatory role in Barrett’s esophagus or reflux esophagitis caused by acid reflux or bile reflux. Interfering with NCX1 can significantly inhibit the release of inflammatory mediators and the expression of intestinal metaplasia genes caused by the aforementioned pathogenic factors. Therefore, NCX1 is likely to be an important treatment target for esophageal functional diseases.
NCX1 also plays an important role in the correlation between smoking and the pathogenesis of esophageal squamous cell carcinoma (ESCC)[41]. Clinical evidence showed that the expression of NCX1 in ESCC tissue was significantly higher than that in esophageal noncancerous tissue and demonstrated a positive correlation between the NCX1 expression level and the smoking status of ESCC patients. The tobacco-derived carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) can significantly enhance NCX1 expression in normal esophageal cells and human ESCC cells. NNK mediates an increase in the intracellular Ca2+ concentration through NCX1 activation and promotes the proliferation and migration of human ESCC cells[41]. These findings indicate that tobacco smoking could cause Ca2+ entry through enhanced expression and function of NCX1, finally resulting in the pathogenesis of ESCC. Furthermore, NCX1 is also involved in the proliferation and migration of ESCC cells. To elucidate the mechanism of NCX1 in ESCC, it is necessary to study the function of NCX1 in ESCC in the future.
The stomach, the main digestive organ of the human body, is connected to the esophagus and the duodenum. It is known that the plasma membrane Ca2+ -ATPase (PMCA), NCX, and the endoplasmic reticulum (ER) Ca2+ -ATPase are the main mechanisms for the transport of intracellular Ca2+ to the extracellular space of gastric smooth muscle cells[42,43]. Studies have shown that NCX1 is widely expressed in the antrum of guinea pigs, while NCX2 has higher expression in the fundus[44]. Researchers believe that different NCX subtypes, which have different physiological functions, are expressed in different parts of the stomach and regulate each other. NCX1 is mainly involved in gastric antral motility, while NCX2 mainly changes the intracellular Ca2+ homeostasis in fundus smooth muscle cells to control the contraction and relaxation of the fundus smooth muscle[44]. This information suggests that the NCX family may control the movement of the whole stomach by controlling the movement of the gastric antrum and fundus smooth muscle.
In a study of gastrointestinal motility diseases, Hagi et al[45] found that NO and PACAP act as important mediators of the transient and sustained relaxation in the mouse gastric fundus. A change in functional coupling and/or collaborative functions between NO signaling and PACAP signaling may cause intracellular Ca2+ concentration changes, thereby controlling gastric fundus relaxation in mice. The overexpression of NCX1 in smooth muscle may result in increased functional coupling and/or collaborative functions between NO signaling and PACAP signaling, resulting in the occurrence of functional gastrointestinal disorders[46]. Interestingly, studies on experimental gastric ulcer (GU) indicate that nitric oxide synthase (NOS) activity may be an important marker of neutrophil infiltration[47,48]. NO also contributes to ethanol-induced gastric ulceration and inflammatory bowel diseases (IBD) due to its role in the stimulation of cell proliferation in the gastric mucosa[49-51]. However, the overexpression of NCX1 in gastrointestinal smooth muscle may affect the function of the NO signaling pathway, and whether this change will promote GU and IBD process through the NO signaling pathway needs further study. It has also been reported that electric field stimulation (EFS) can induce sustained relaxation of the stomach fundus, but not other intestinal regions[52-54]. The study suggested that this sustained status may be closely related to the regulatory functions of NCX1 and NCX2. In the past few years, studies have shown that NCX1 and NCX2 are expressed in smooth muscles and neurons to regulate the relaxation and motility of the gastric fundus. Upon NCX1 or NCX2 heterozygosity deletion, the fundus relaxation and the gastric peristalsis can be enhanced by EFS[55]. Therefore, the NCX family may be an important treatment target for functional gastrointestinal diseases. In addition, Lajos V also found that NCX family members (NCX1, NCX2, and NCX3) are expressed extensively in human gastric myofibroblasts and participate in the regulation of intracellular calcium oscillations. Knockdown of NCX1 significantly inhibited the migration and proliferation of gastric myofibroblasts induced by insulin-like growth factor II (IGF-II)[22]. Gastric myofibroblasts are a kind of contractile, nonexcitatory cell induced by inflammatory factors such as transforming growth factor (TGF-β), and these cells are localized to the subepithelium throughout the whole gastrointestinal tract[56,57]. It is known that gastric myofibroblasts can not only regulate the secretion of extracellular matrix proteins and the formation of new blood vessels, promoting the healing process of ulcers[58,59], but also participate in the development of chronic gastritis and gastric cancer cell invasion and metastasis[60,61]. Further study on the role of NCX in gastrointestinal smooth muscle may elucidate the regulatory mechanisms of ulcer healing and tumor invasion and metastasis.
The expression of NCX1 protein has been detected in the small intestine, colon, and rectum[62,63], and it participates in the physiological regulation mechanism of intestinal calcium absorption, bicarbonate secretion, ileal smooth muscle movement and so on. The small intestine absorbs 90% of calcium[3,64,65]. Additionally, NCX1 mainly participates in the process of extracellular discharge of calcium ions from the basal membrane of intestinal epithelial cells. NCX1 can transport three Na+ ions into the cell and transport one Ca2+ ion out of the cell; this transport is regulated by vitamin D and 1,25-(OH)2D3[66], which can enhance the expression and activity of NCX on the basal membrane and promote the transport of Ca2+ from the cell to the outside[66]. Moreover, Wongdee et al found that vitamin D can upregulate the expression of the Ca2+ transporter gene NCX1, thus enhancing the Ca2+ transmembrane transport[67].
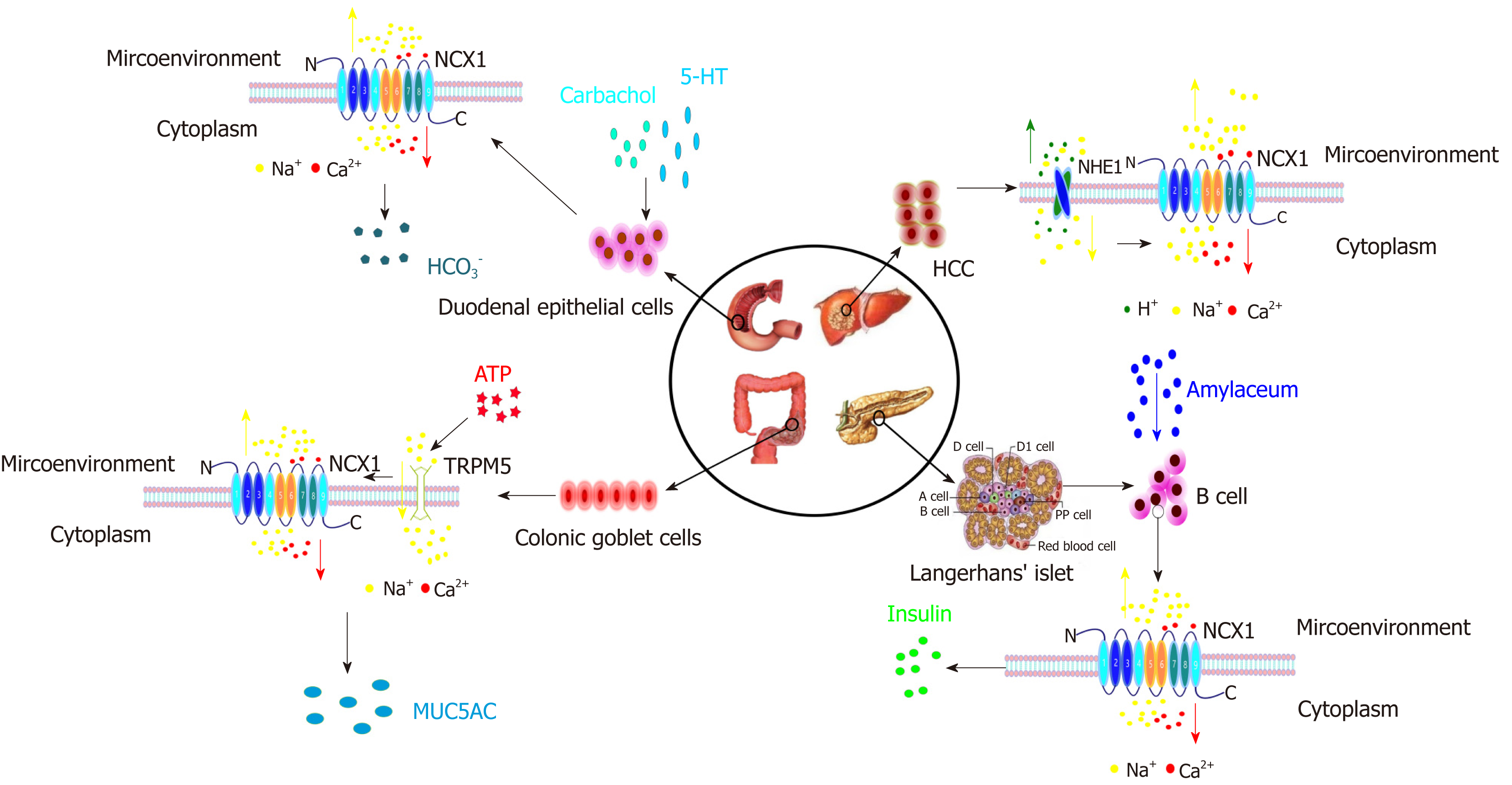
It is well known that the gastric acid defense barrier involves bicarbonate, and the hyposecretion of bicarbonate is one of the key mechanisms for the pathogenesis of duodenal ulcers. It has been reported that intracellular calcium signals can promote HCO3- secretion depending on the activation of the HCO3- secreting channel cystic fibrosis transmembrane conductance regulator (CFTR) or on the activation of the intermediate-conductance Ca2+ activated K+ channel (IKCa2+), which provide a driving force for HCO3- secretion[68]. However, NCX1 may be the key to the regulation of intracellular calcium changes. Dong et al found that the NCX1 protein is functionally expressed in the mouse duodenal mucosal epithelium, and a dynamic calcium ion experiment determined that the reverse regulation mode of NCX1 occurs, causing Na+ efflux and Ca2+ entry to regulate HCO3- secretion[69]. Subsequent research confirmed that the muscarinic receptor agonists carbachol and 5-hydroxytryptamine (5-HT) can increase the intracellular calcium concentration and promote duodenal bicarbonate secretion after stimulating mouse duodenal mucosal or epithelial cells and confirmed that disturbing or inhibiting the function of NCX1 can obviously block the intracellular calcium change and promote bicarbonate secretion[70]. These results suggest that NCX1 and its mediated Ca2+ influx play a critical and extensive role in regulating the secretion of HCO3- in the duodenal mucosa. Other studies have shown that NCX1 and NCX2 are also involved in ileal smooth muscle contraction and ileal motility regulation[71]. Nishiyama et al found that NCX2 regulates ileal motility primarily by controlling the sensitivity of acetylcholine (AchE) and substance P (SP) in smooth muscle[71]. Compared with that in the wild-type model, the contraction amplitude induced by AchE and SP after NCX2 knockout was significantly reduced; although NCX1 also plays a role in the regulation of ileal contraction, this decline was not evident in the NCX1 knockout model[71]. This finding suggests that NCX2 plays a more important role than NCX1 in ileal movement.
NCXs (NCX1 and NCX2) are also widely expressed in colonic smooth muscle and the myenteric plexus layers[72]. Nishiyama et al showed that NCX1 overexpression in the mouse distal colon enhanced the relaxation amplitude induced by EFS, suggesting that NCX1 can affect the distal colonic smooth muscle movement in mice[71]. Furthermore, it was found that the secretion of the mucin MUC5AC induced by ATP depends on the influx of Ca2+ into colonic goblet cells and that ATP requires the activation of TRPM5 channels to increase intracellular Na+, which activates the NCX reverse transport mode and increases intracellular Ca2+ uptake; thus, inhibiting NCX can significantly reduce the MUC5AC secretion in goblet cells[73]. There is also evidence that the NCX family may also be involved in the pathogenesis of diarrhea. Although NCX1 and NCX2 were found to be expressed in the myenteric nerve plexus of the proximal colon and the colon transversum as well as longitudinal and annular muscular layers, the function of NCX1 and NCX2 in intermuscular neurons may be different from that in smooth muscle[74]. Kazuhiro et al have found that in a diarrhea model induced with magnesium sulfate or 5-HT, the diarrhea in NCX2 heterozygous knockout mice (NCX2 HET) was more serious than that in wild-type mice (WT), but the diarrhea in NCX1 heterozygous knockout mice (NCX1 HET) showed no significant changes from that of WT[75]. Magnesium sulfate-induced diarrhea was exacerbated in NCX2 HET by decreasing normal and soft fecal materials and increasing watery fecal materials, however, PGE2-induced diarrhea in NCX1 HET and NCX2 HET was similar to that in the WT[75]. The researchers believe that this finding may be due to the mechanism of 5-HT-induced diarrhea involving stimulation of the 5-HT3 receptor in myenteric plexus neurons and its downstream cholinergic and tachykinin excitatory pathways[76,77]. However, PGE2 acts directly on smooth muscle and stimulates fluid accumulation to induce diarrhea[78,79]. Therefore, NCX2 rather than NCX1 in the myenteric plexus may play a critical role in the occurrence and development of diarrhea. Further study of NCX may provide new targets for the diarrhea caused by gastrointestinal dysfunction.
NCX1 is functionally expressed in the β-cells, acinar cells, and ductal cells of the rat pancreas and has a distinct pattern of distribution in pancreatic ducts depending on their size and proximity to acini[80]. Two splicing variants of NCX1, NCX1.3 and NCX1.7, are mainly expressed in rat pancreatic cells[81-84]; however, three other variants, NCX1.2, NCX1.9, and NCX1.13, were also found in guinea pigs, hamsters and mice. In the past few years, studies have proved that different types of NCX1 have different expression levels between different species.
The physiological functions of the pancreas include secreting various digestive enzymes and insulin. Normally, the intracellular ATP/ADP ratio increases after pancreatic β-cells uptake glucose, via the closure of K+-ATP channels, causing β-cell depolarization and inducing extracellular calcium influx through calcium channels in the membrane; the intracellular calcium increase causes fusion of the vesicular membrane containing insulin with the cytoplasmic membrane and the subsequent secretion of insulin from cells via vesicular exocytosis[85]. It has been found that both the voltage-dependent calcium channel (CaV) and the intracellular IP3-sensitive calcium pool are important in insulin secretion regulation in the past few years[86], but the role of the NCX family in this process is just beginning to be evaluated.
In normal pancreatic islet β-cells, NCX1 is mainly responsible for Ca2+ efflux from cells. The aim is to control the Ca2+ concentration within the normal physiological range in order to accurately control the insulin release level[83,87]. In native pancreatic ducts, the NCX1 expression level is downregulated by acetylcholine and secretin but upregulated by insulin[80]; as the main physiological stimulant of insulin release, glucose has the reverse regulatory effect on the transcription, expression, and activity of NCX[88].
Pathologically, NCX also has a regulatory mechanism affecting the insulin secretion from the β-cells of diabetic patients. In the past few years, research has shown that NCX overexpression can lead to ER stress and Ca2+ release from the ER, thus promoting β-cell apoptosis, reducing β-cell proliferation, and decreasing insulin secretion[88]. Herchuelz et al[89] found that heterozygous inactivation of NCX1 (Ncx1+/-) leads to an increase in β-cell function and a 5-fold increase in both β-cell mass and proliferation. The mutation also increases the β-cell resistance to hypoxia, and Ncx1+/- islets show a 2-4 times higher rate of curing diabetes than Ncx1+/+ islets when transplanted into diabetic animals. However, in some cases, NCX may change into the reverse regulation mode to promote Ca2+ entry, prolonging the duration of the peak electrical activity associated with glucose and increasing insulin release[90]. In summary, the different NCX1 expression and transport modes can regulate insulin secretion, so selective inhibition of NCX1 may improve insulin secretion, which provides more theoretical evidence for novel glucose-sensitive insulinotropic drugs for type 2 diabetes that target NCX1.
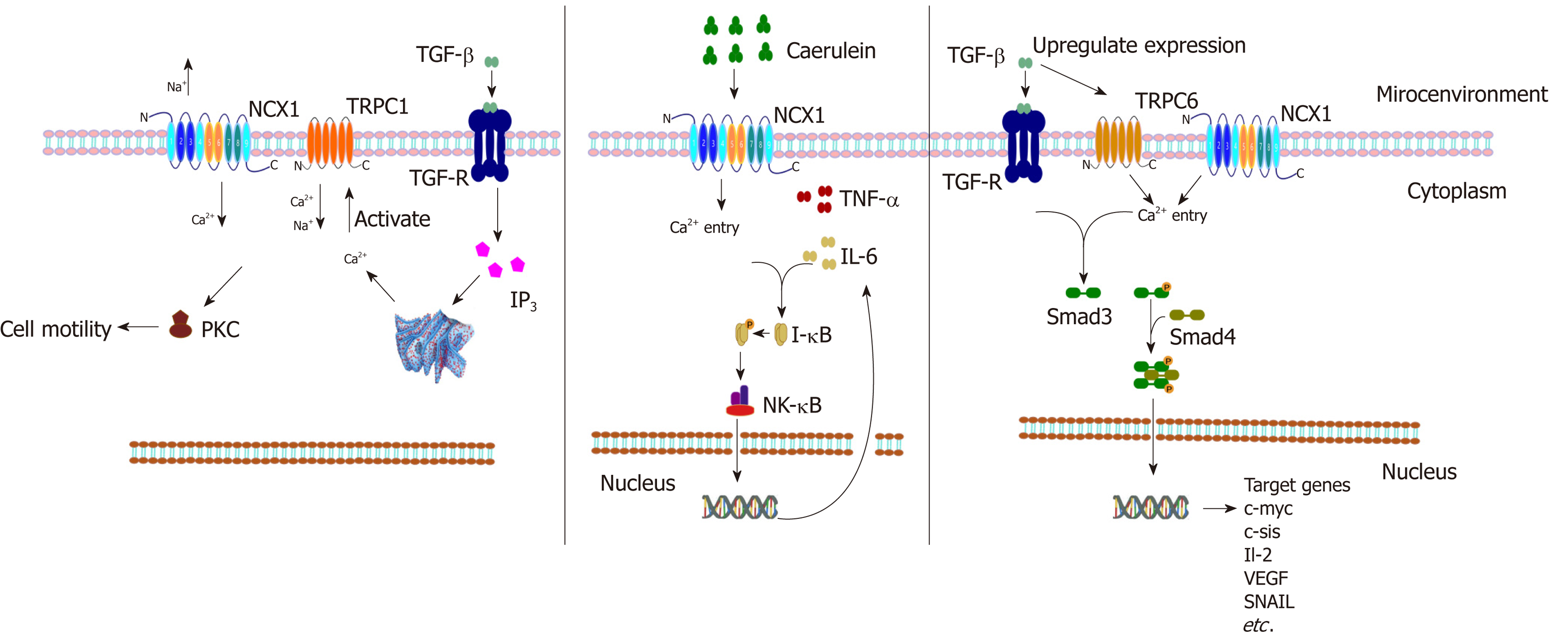
In addition to regulating physiological insulin secretion, the Ca2+ homeostasis is also a key factor leading to pancreatitis, hypercalcemia, pancreatic cancer, and other diseases. Pancreatitis is one of the most common acute abdomen problems, and the pathogenesis is the abnormal accumulation of intracellular Ca2+ (calcium overload) to promote excessive activation of trypsinogen, resulting in pancreatic autodigestive injury[91]. Previous studies have reported that the calcium overload in acute pancreatitis may be related to calcium channels such as CRAC/TRPV1/TRPV3[92,93]; however, it has recently been found that the NCX1 reverse regulation mode may also be involved in this overload. Yu et al confirmed that the mRNA and protein expression of NCX1 in tissues of acute pancreatitis induced by cerulein was significantly increased in cell experiments and animal experiments[94]. The authors found that the expression of inflammatory mediators such as TNF-α and interleukin-6 (IL-6) caused by cerulein was decreased significantly after treatment with KB-R7943 (a specific inhibitor of NCX1)[94]. This finding suggests that NCX1 may play a critical role in the occurrence and development of acute pancreatitis. In addition, pancreatic cancer is a kind of cancer with high malignancy and poor prognosis, and duct cell carcinoma is the main pathological type of pancreatic cancer[95,96]. However, it is generally accepted that alterations in TGF-β signaling and its downstream SMAD pathway play an important role in pancreatic cancer development[97]. The study by Chow et al found that TRPC1 and NCX1 are expressed and functional in pancreatic cancer cells. TGF-β activates TRPC1 and NCX1 channels to mediate a cytoplasmic Ca2+ concentration increase in pancreatic cancer cells, which activates the downstream PKC/SMAD4 pathway to regulate pancreatic cancer cell motility[98]. These results suggest that NCX1 may be involved in the malignant biological behavior regulation of pancreatic cancer (Figure 2).
Although NCX1 is expressed in normal livers, liver fibrosis, and liver cancer, the transcription levels and regulation modes are different under these three conditions, suggesting that NCX may have different functions and effects in the development of hepatitis, liver fibrosis, and liver cancer[99]. In the study of liver ischemia-reperfusion injury, intracellular calcium accumulation is a critical mechanism of cell apoptosis and injury[100]. NCX mainly adopts the forward control mode in ischemic-reperfusion injury. Trisulfated disaccharide (TD) can transport excess intracellular calcium out of the cell by activating NCX1, thus reducing the serum levels of inflammation markers (TNF-α, IL-6, and IL-10) and the lipid peroxidation after liver injury[101].
Hepatic fibrosis is a necessary process in the progression from chronic hepatitis to cirrhosis. The activation and proliferation of hepatic stellate cells (HSCs) are the central link of hepatic fibrosis. Nakamura et al found that the NCX mRNA and protein expression levels were significantly upregulated in response to the activation of rat HSCs induced by CCl4[102]. It was also reported that NCX expression is upregulated in cirrhotic tissue, although the specific mechanism is not clear; NCX may be a new target in liver fibrosis or cirrhosis research[93].
Finally, in hepatocellular carcinoma (HCC) research, our research group has published articles confirming that the expression of NCX1 is obviously upregulated in hepatoma cells and tissues and that NCX1 can affect the intracellular calcium level to affect the cytokines TGF-β or IL-6 in the malignant behavior of hepatoma cells. A study found that TGF-β can upregulate the expression of NCX1 and the transient receptor potential channel TRPC6 in hepatoma cells and further induce intracellular calcium activation in HCC to promote the formation of a complex between NCX1 and TRPC6, thus activating the downstream SMAD pathway, which can regulate HCC malignant biological behaviors such as migration and invasion[103]. Not only was the phosphorylation of Smad proteins dependent on TRPC6 and NCX1, but also the Smad signaling, especially the phosphorylation of Smad2, augmented the expression of TRPC6 and NCX1. At the same time the upregulated expression of TRPC6 and NCX1 can be strongly correlated with the stage and pathologic grade of HCC, which may become useful biomarkers for monitoring disease progression of liver cancer patients[103,104]. In a related study of IL-6 and liver cancer, it was also confirmed that an intracellular pH regulator (NHE1), NCX1, and calmodulin (CaM) coexisted in the same lipid-crossing structure of the cell membrane and that their expression levels were upregulated in liver cancer tissues[105] (Figure 2). Moreover, IL-6 activated NHE1 to promote H+ excretion and an NCX1-induced external Ca2+ influx, and NHE1 pumped H+ in exchange for Na+ influx to promote NCX1 activation, which enhanced the interaction between NCX1 and CaM, thus promoting the occurrence and development of liver cancer[106]. The above findings provide the basis for the important role of NCX in hepatic carcinogenesis and also provide a new possibility for drug development for early intervention in inflammation-associated tumors.
In summary, the NCX1 channel protein regulates the Ca2+ signaling pathway via its forward/reverse modes in the digestive system and regulates the cell function, thus participating in the occurrence and development of digestive system diseases (Figures 3 and 4). The functions of NCX1 in inflammation-associated digestive diseases (such as inflammatory bowel disease and hepatitis ) will become a new research hotspot. NCX1 could be a new molecular marker for the digestive system disease diagnosis and treatment, and drug development targeting NCX1 will represent a new direction of the treatment of digestive system diseases.
We thank Professor Biguang Tuo (Department of Gastroenterology, Affiliated Hospital to Zunyi Medical College) for highly professional services.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Dong H, Sandow SL, Touil-Boukoffa C S- Editor: Gong ZM L- Editor: Wang TQ E- Editor: Huang Y
| 1. | Berridge MJ, Lipp P, Bootman MD. The versatility and universality of calcium signalling. Nat Rev Mol Cell Biol. 2000;1:11-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4077] [Cited by in F6Publishing: 4018] [Article Influence: 167.4] [Reference Citation Analysis (0)] |
| 2. | Clapham DE. Calcium signaling. Cell. 2007;131:1047-1058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2811] [Cited by in F6Publishing: 2902] [Article Influence: 181.4] [Reference Citation Analysis (0)] |
| 3. | Hoenderop JG, Nilius B, Bindels RJ. Calcium absorption across epithelia. Physiol Rev. 2005;85:373-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 633] [Cited by in F6Publishing: 557] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 4. | Rachow S, Zorn-Kruppa M, Ohnemus U, Kirschner N, Vidal-y-Sy S, von den Driesch P, Börnchen C, Eberle J, Mildner M, Vettorazzi E, Rosenthal R, Moll I, Brandner JM. Occludin is involved in adhesion, apoptosis, differentiation and Ca2+-homeostasis of human keratinocytes: implications for tumorigenesis. PLoS One. 2013;8:e55116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Zeng F, Chen X, Cui W, Wen W, Lu F, Sun X, Ma D, Yuan Y, Li Z, Hou N, Zhao H, Bi X, Zhao J, Zhou J, Zhang Y, Xiao RP, Cai J, Zhang X. RIPK1 Binds MCU to Mediate Induction of Mitochondrial Ca2+ Uptake and Promotes Colorectal Oncogenesis. Cancer Res. 2018;78:2876-2885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Khananshvili D. Sodium-calcium exchangers (NCX): molecular hallmarks underlying the tissue-specific and systemic functions. Pflugers Arch. 2014;466:43-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Khananshvili D. The SLC8 gene family of sodium-calcium exchangers (NCX) - structure, function, and regulation in health and disease. Mol Aspects Med. 2013;34:220-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 152] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 8. | Liao J, Li H, Zeng W, Sauer DB, Belmares R, Jiang Y. Structural insight into the ion-exchange mechanism of the sodium/calcium exchanger. Science. 2012;335:686-690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 202] [Cited by in F6Publishing: 178] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 9. | Papa M, Canitano A, Boscia F, Castaldo P, Sellitti S, Porzig H, Taglialatela M, Annunziato L. Differential expression of the Na+-Ca2+ exchanger transcripts and proteins in rat brain regions. J Comp Neurol. 2003;461:31-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 99] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Blaustein MP, Leenen FH, Chen L, Golovina VA, Hamlyn JM, Pallone TL, Van Huysse JW, Zhang J, Wier WG. How NaCl raises blood pressure: a new paradigm for the pathogenesis of salt-dependent hypertension. Am J Physiol Heart Circ Physiol. 2012;302:H1031-H1049. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 174] [Cited by in F6Publishing: 175] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 11. | Antoons G, Willems R, Sipido KR. Alternative strategies in arrhythmia therapy: evaluation of Na/Ca exchange as an anti-arrhythmic target. Pharmacol Ther. 2012;134:26-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Herrmann S, Lipp P, Wiesen K, Stieber J, Nguyen H, Kaiser E, Ludwig A. The cardiac sodium-calcium exchanger NCX1 is a key player in the initiation and maintenance of a stable heart rhythm. Cardiovasc Res. 2013;99:780-788. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Ohtsuka M, Takano H, Suzuki M, Zou Y, Akazawa H, Tamagawa M, Wakimoto K, Nakaya H, Komuro I. Role of Na+-Ca2+ exchanger in myocardial ischemia/reperfusion injury: evaluation using a heterozygous Na+-Ca2+ exchanger knockout mouse model. Biochem Biophys Res Commun. 2004;314:849-853. [PubMed] [Cited in This Article: ] |
| 14. | Roome CJ, Power EM, Empson RM. Transient reversal of the sodium/calcium exchanger boosts presynaptic calcium and synaptic transmission at a cerebellar synapse. J Neurophysiol. 2013;109:1669-1680. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Noda M, Ifuku M, Mori Y, Verkhratsky A. Calcium influx through reversed NCX controls migration of microglia. Adv Exp Med Biol. 2013;961:289-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Morimoto N, Kita S, Shimazawa M, Namimatsu H, Tsuruma K, Hayakawa K, Mishima K, Egashira N, Iyoda T, Horie I, Gotoh Y, Iwasaki K, Fujiwara M, Matsuda T, Baba A, Komuro I, Horie K, Takeda J, Iwamoto T, Hara H. Preferential involvement of Na⁺/Ca²⁺ exchanger type-1 in the brain damage caused by transient focal cerebral ischemia in mice. Biochem Biophys Res Commun. 2012;429:186-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Annunziato L, Pignataro G, Di Renzo GF. Pharmacology of brain Na+/Ca2+ exchanger: from molecular biology to therapeutic perspectives. Pharmacol Rev. 2004;56:633-654. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 241] [Cited by in F6Publishing: 254] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 18. | Moor MB, Haenzi B, Legrand F, Koesters R, Hynes NE, Bonny O. Renal Memo1 Differentially Regulates the Expression of Vitamin D-Dependent Distal Renal Tubular Calcium Transporters. Front Physiol. 2018;9:874. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Yamashita J, Kita S, Iwamoto T, Ogata M, Takaoka M, Tazawa N, Nishikawa M, Wakimoto K, Shigekawa M, Komuro I, Matsumura Y. Attenuation of ischemia/reperfusion-induced renal injury in mice deficient in Na+/Ca2+ exchanger. J Pharmacol Exp Ther. 2003;304:284-293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Hamming KS, Soliman D, Webster NJ, Searle GJ, Matemisz LC, Liknes DA, Dai XQ, Pulinilkunnil T, Riedel MJ, Dyck JR, Macdonald PE, Light PE. Inhibition of beta-cell sodium-calcium exchange enhances glucose-dependent elevations in cytoplasmic calcium and insulin secretion. Diabetes. 2010;59:1686-1693. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Vasques ER, Cunha JEM, Kubrusly MS, Coelho AM, Sanpietri SN, Nader HB, Tersariol ILS, Lima MA, Chaib E, D'Albuquerque LAC. The M-RNA, expression of SERCA2 and NCX1 in the process of pharmacological cell protection in experimental acute pancreatitis induced by taurocholate. Arq Bras Cir Dig. 2018;31:e1352. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Kemény LV, Schnúr A, Czepán M, Rakonczay Z Jr, Gál E, Lonovics J, Lázár G, Simonka Z, Venglovecz V, Maléth J, Judák L, Németh IB, Szabó K, Almássy J, Virág L, Geisz A, Tiszlavicz L, Yule DI, Wittmann T, Varró A, Hegyi P. Na+/Ca2+ exchangers regulate the migration and proliferation of human gastric myofibroblasts. Am J Physiol Gastrointest Liver Physiol. 2013;305:G552-G563. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Xu J, Jiang Y, Xie R, Wen G, Dong H, Tuo B. Su1578 Expression and Functional Role of Ncx1 in Human Hepatocellular Carcinoma. Gastroenterology. 2012;142:S-970-S-970. [Cited in This Article: ] |
| 24. | Tang B, Chow JY, Dong TX, Yang SM, Lu DS, Carethers JM, Dong H. Calcium sensing receptor suppresses human pancreatic tumorigenesis through a novel NCX1/Ca(2+)/β-catenin signaling pathway. Cancer Lett. 2016;377:44-54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Plain F, Turnbull D, Fraser NJ, Fuller W. Understanding the rules governing NCX1 palmitoylation. Channels (Austin). 2017;11:377-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Reilly L, Howie J, Wypijewski K, Ashford ML, Hilgemann DW, Fuller W. Palmitoylation of the Na/Ca exchanger cytoplasmic loop controls its inactivation and internalization during stress signaling. FASEB J. 2015;29:4532-4543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 27. | Nicoll DA, Ren X, Ottolia M, Phillips M, Paredes AR, Abramson J, Philipson KD. What we know about the structure of NCX1 and how it relates to its function. Ann N Y Acad Sci. 2007;1099:1-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Nicoll DA, Hryshko LV, Matsuoka S, Frank JS, Philipson KD. Mutation of amino acid residues in the putative transmembrane segments of the cardiac sarcolemmal Na+-Ca2+ exchanger. J Biol Chem. 1996;271:13385-13391. [PubMed] [Cited in This Article: ] |
| 29. | Doering AE, Nicoll DA, Lu Y, Lu L, Weiss JN, Philipson KD. Topology of a functionally important region of the cardiac Na+/Ca2+ exchanger. J Biol Chem. 1998;273:778-783. [PubMed] [Cited in This Article: ] |
| 30. | Iwamoto T, Uehara A, Imanaga I, Shigekawa M. The Na+/Ca2+ exchanger NCX1 has oppositely oriented reentrant loop domains that contain conserved aspartic acids whose mutation alters its apparent Ca2+ affinity. J Biol Chem. 2000;275:38571-38580. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 87] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Li Z, Nicoll DA, Collins A, Hilgemann DW, Filoteo AG, Penniston JT, Weiss JN, Tomich JM, Philipson KD. Identification of a peptide inhibitor of the cardiac sarcolemmal Na(+)-Ca2+ exchanger. J Biol Chem. 1991;266:1014-1020. [PubMed] [Cited in This Article: ] |
| 32. | Matsuoka S, Nicoll DA, He Z, Philipson KD. Regulation of cardiac Na(+)-Ca2+ exchanger by the endogenous XIP region. J Gen Physiol. 1997;109:273-286. [PubMed] [Cited in This Article: ] |
| 33. | Levitsky DO, Nicoll DA, Philipson KD. Identification of the high affinity Ca(2+)-binding domain of the cardiac Na(+)-Ca2+ exchanger. J Biol Chem. 1994;269:22847-22852. [PubMed] [Cited in This Article: ] |
| 34. | Matsuoka S, Nicoll DA, Hryshko LV, Levitsky DO, Weiss JN, Philipson KD. Regulation of the cardiac Na(+)-Ca2+ exchanger by Ca2+. Mutational analysis of the Ca(2+)-binding domain. J Gen Physiol. 1995;105:403-420. [PubMed] [Cited in This Article: ] |
| 35. | Reyes RC, Verkhratsky A, Parpura V. Plasmalemmal Na+/Ca2+ exchanger modulates Ca2+-dependent exocytotic release of glutamate from rat cortical astrocytes. ASN Neuro. 2012;4:pii: e00075. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 36. | Liu JF, Lu HL, Wen SW, Wu RF. Effects of acetylcholine on sling and clasp fibers of the human lower esophageal sphincter. J Gastroenterol Hepatol. 2011;26:1309-1317. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Hoogerwerf WA, Pasricha PJ. Pharmacologic therapy in treating achalasia. Gastrointest Endosc Clin N Am. 2001;11:311-324, vii. [PubMed] [Cited in This Article: ] |
| 38. | Gelfond M, Rozen P, Keren S, Gilat T. Effect of nitrates on LOS pressure in achalasia: a potential therapeutic aid. Gut. 1981;22:312-318. [PubMed] [Cited in This Article: ] |
| 39. | Kellerman R, Kintanar T. Gastroesophageal Reflux Disease. Prim Care. 2017;44:561-573. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 40. | Kim K, Lee D, Ahn C, Kang HY, An BS, Seong YH, Jeung EB. Effects of estrogen on esophageal function through regulation of Ca2+-related proteins. J Gastroenterol. 2017;52:929-939. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Wen J, Pang Y, Zhou T, Qi X, Zhao M, Xuan B, Meng X, Guo Y, Liu Q, Liang H, Li Y, Dong H, Wang Y. Essential role of Na+/Ca2+ exchanger 1 in smoking-induced growth and migration of esophageal squamous cell carcinoma. Oncotarget. 2016;7:63816-63828. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 42. | Wray S, Burdyga T. Sarcoplasmic reticulum function in smooth muscle. Physiol Rev. 2010;90:113-178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 43. | Webb RC. Smooth muscle contraction and relaxation. Adv Physiol Educ. 2003;27:201-206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 212] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 44. | Sakai Y, Kinoshita H, Saitou K, Homma I, Nobe K, Iwamoto T. Functional differences of Na+/Ca2+ exchanger expression in Ca2+ transport system of smooth muscle of guinea pig stomach. Can J Physiol Pharmacol. 2005;83:791-797. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Hagi K, Azuma YT, Nakajima H, Shintani N, Hashimoto H, Baba A, Takeuchi T. Involvements of PHI-nitric oxide and PACAP-BK channel in the sustained relaxation of mouse gastric fundus. Eur J Pharmacol. 2008;590:80-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 46. | Fujimoto Y, Hayashi S, Azuma YT, Mukai K, Nishiyama K, Kita S, Morioka A, Nakajima H, Iwamoto T, Takeuchi T. Overexpression of Na+/Ca2+ exchanger 1 display enhanced relaxation in the gastric fundus. J Pharmacol Sci. 2016;132:181-186. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 47. | Coskun T, Yeğen BC, Alican I, Peker O, Kurtel H. Cold restraint stress-induced gastric mucosal dysfunction. Role of nitric oxide. Dig Dis Sci. 1996;41:956-963. [PubMed] [Cited in This Article: ] |
| 48. | Neurath MF. Cytokines in inflammatory bowel disease. Nat Rev Immunol. 2014;14:329-342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1545] [Cited by in F6Publishing: 1684] [Article Influence: 168.4] [Reference Citation Analysis (1)] |
| 49. | Li Y, Wang WP, Wang HY, Cho CH. Intragastric administration of heparin enhances gastric ulcer healing through a nitric oxide-dependent mechanism in rats. Eur J Pharmacol. 2000;399:205-214. [Cited in This Article: ] |
| 50. | Soufli I, Toumi R, Rafa H, Touil-Boukoffa C. Overview of cytokines and nitric oxide involvement in immuno-pathogenesis of inflammatory bowel diseases. World J Gastrointest Pharmacol Ther. 2016;7:353-360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 210] [Cited by in F6Publishing: 219] [Article Influence: 27.4] [Reference Citation Analysis (5)] |
| 51. | Boutemine IM, Amri M, Amir ZC, Fitting C, Mecherara-Idjeri S, Layaida K, Sennoun N, Berkane S, Cavaillon JM, Touil-Boukoffa C. Gastro-protective, therapeutic and anti-inflammatory activities of Pistacia lentiscus L. fatty oil against ethanol-induced gastric ulcers in rats. J Ethnopharmacol. 2018;224:273-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 52. | Mukai K, Takeuchi T, Toyoshima M, Satoh Y, Fujita A, Shintani N, Hashimoto H, Baba A, Hata F. PACAP- and PHI-mediated sustained relaxation in circular muscle of gastric fundus: findings obtained in PACAP knockout mice. Regul Pept. 2006;133:54-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 53. | Mulè F, Serio R. NANC inhibitory neurotransmission in mouse isolated stomach: involvement of nitric oxide, ATP and vasoactive intestinal polypeptide. Br J Pharmacol. 2003;140:431-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 54. | Baccari MC, Calamai F. Modulation of nitrergic relaxant responses by peptides in the mouse gastric fundus. Regul Pept. 2001;98:27-32. [PubMed] [Cited in This Article: ] |
| 55. | Azuma YT, Hayashi S, Nishiyama K, Kita S, Mukai K, Nakajima H, Iwamoto T, Takeuchi T. Na(+) /Ca(2+) exchanger-heterozygote knockout mice display increased relaxation in gastric fundus and accelerated gastric transit in vivo. Neurogastroenterol Motil. 2016;28:827-836. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 56. | Hinz B, Phan SH, Thannickal VJ, Galli A, Bochaton-Piallat ML, Gabbiani G. The myofibroblast: one function, multiple origins. Am J Pathol. 2007;170:1807-1816. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1455] [Cited by in F6Publishing: 1520] [Article Influence: 89.4] [Reference Citation Analysis (0)] |
| 57. | Desmoulière A, Chaponnier C, Gabbiani G. Tissue repair, contraction, and the myofibroblast. Wound Repair Regen. 2005;13:7-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 644] [Cited by in F6Publishing: 626] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 58. | Nishida T, Tsuji S, Kimura A, Tsujii M, Ishii S, Yoshio T, Shinzaki S, Egawa S, Irie T, Yasumaru M, Iijima H, Murata H, Kawano S, Hayashi N. Endothelin-1, an ulcer inducer, promotes gastric ulcer healing via mobilizing gastric myofibroblasts and stimulates production of stroma-derived factors. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1041-G1050. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 59. | Chai J, Norng M, Tarnawski AS, Chow J. A critical role of serum response factor in myofibroblast differentiation during experimental oesophageal ulcer healing in rats. Gut. 2007;56:621-630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 60. | Guo X, Oshima H, Kitmura T, Taketo MM, Oshima M. Stromal fibroblasts activated by tumor cells promote angiogenesis in mouse gastric cancer. J Biol Chem. 2008;283:19864-19871. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 163] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 61. | McCaig C, Duval C, Hemers E, Steele I, Pritchard DM, Przemeck S, Dimaline R, Ahmed S, Bodger K, Kerrigan DD, Wang TC, Dockray GJ, Varro A. The role of matrix metalloproteinase-7 in redefining the gastric microenvironment in response to Helicobacter pylori. Gastroenterology. 2006;130:1754-1763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 62. | Kim JA, Yang H, Hwang I, Jung EM, Choi KC, Jeung EB. Expression patterns and potential action of the calcium transport genes Trpv5, Trpv6, Ncx1 and Pmca1b in the canine duodenum, kidney and uterus. In Vivo. 2011;25:773-780. [PubMed] [Cited in This Article: ] |
| 63. | Hwang I, Jung EM, Yang H, Choi KC, Jeung EB. Tissue-specific expression of the calcium transporter genes TRPV5, TRPV6, NCX1, and PMCA1b in the duodenum, kidney and heart of Equus caballus. J Vet Med Sci. 2011;73:1437-1444. [PubMed] [Cited in This Article: ] |
| 64. | Wasserman RH. Vitamin D and the dual processes of intestinal calcium absorption. J Nutr. 2004;134:3137-3139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 118] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 65. | Bronner F. Recent developments in intestinal calcium absorption. Nutr Rev. 2009;67:109-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 66. | Khuituan P, Wongdee K, Jantarajit W, Suntornsaratoon P, Krishnamra N, Charoenphandhu N. Fibroblast growth factor-23 negates 1,25(OH)2D3-induced intestinal calcium transport by reducing the transcellular and paracellular calcium fluxes. Arch Biochem Biophys. 2013;536:46-52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 67. | Wongdee K, Charoenphandhu N. Vitamin D-enhanced duodenal calcium transport. Vitam Horm. 2015;98:407-440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 68. | Xie R, Dong X, Wong C, Vallon V, Tang B, Sun J, Yang S, Dong H. Molecular mechanisms of calcium-sensing receptor-mediated calcium signaling in the modulation of epithelial ion transport and bicarbonate secretion. J Biol Chem. 2014;289:34642-34653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 69. | Dong H, Sellers ZM, Smith A, Chow JY, Barrett KE. Na(+)/Ca(2+) exchange regulates Ca(2+)-dependent duodenal mucosal ion transport and HCO(3)(-) secretion in mice. Am J Physiol Gastrointest Liver Physiol. 2005;288:G457-G465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 70. | Smith AJ, Chappell AE, Buret AG, Barrett KE, Dong H. 5-Hydroxytryptamine contributes significantly to a reflex pathway by which the duodenal mucosa protects itself from gastric acid injury. FASEB J. 2006;20:2486-2495. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 71. | Nishiyama K, Azuma YT, Morioka A, Yoshida N, Teramoto M, Tanioka K, Kita S, Hayashi S, Nakajima H, Iwamoto T, Takeuchi T. Roles of Na(+)/Ca(2+) exchanger isoforms NCX1 and NCX2 in motility in mouse ileum. Naunyn Schmiedebergs Arch Pharmacol. 2016;389:1081-1090. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 72. | Nishiyama K, Morioka A, Kita S, Nakajima H, Iwamoto T, Azuma YT, Takeuchi T. Na/Ca(2+) exchanger 1 transgenic mice display increased relaxation in the distal colon. Pharmacology. 2014;94:230-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 73. | Mitrovic S, Nogueira C, Cantero-Recasens G, Kiefer K, Fernández-Fernández JM, Popoff JF, Casano L, Bard FA, Gomez R, Valverde MA, Malhotra V. TRPM5-mediated calcium uptake regulates mucin secretion from human colon goblet cells. Elife. 2013;2:e00658. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 74. | Nishiyama K, Azuma YT, Kita S, Azuma N, Hayashi S, Nakajima H, Iwamoto T, Takeuchi T. Na⁺/Ca²⁺ exchanger 1/2 double-heterozygote knockout mice display increased nitric oxide component and altered colonic motility. J Pharmacol Sci. 2013;123:235-245. [PubMed] [Cited in This Article: ] |
| 75. | Nishiyama K, Tanioka K, Azuma YT, Hayashi S, Fujimoto Y, Yoshida N, Kita S, Suzuki S, Nakajima H, Iwamoto T, Takeuchi T. Na+/Ca2+ exchanger contributes to stool transport in mice with experimental diarrhea. J Vet Med Sci. 2017;79:403-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 76. | Briejer MR, Schuurkes JA. 5-HT3 and 5-HT4 receptors and cholinergic and tachykininergic neurotransmission in the guinea-pig proximal colon. Eur J Pharmacol. 1996;308:173-180. [PubMed] [Cited in This Article: ] |
| 77. | Tuladhar BR, Costall B, Naylor RJ. 5-HT3 and 5-HT4 receptor-mediated facilitation of the emptying phase of the peristaltic reflex in the marmoset isolated ileum. Br J Pharmacol. 1996;117:1679-1684. [PubMed] [Cited in This Article: ] |
| 78. | Rivière PJ, Farmer SC, Burks TF, Porreca F. Prostaglandin E2-induced diarrhea in mice: importance of colonic secretion. J Pharmacol Exp Ther. 1991;256:547-552. [PubMed] [Cited in This Article: ] |
| 79. | Wardle TD, Hall L, Turnberg LA. Inter-relationships between inflammatory mediators released from colonic mucosa in ulcerative colitis and their effects on colonic secretion. Gut. 1993;34:503-508. [PubMed] [Cited in This Article: ] |
| 80. | Ankorina-Stark I, Amstrup J, Novak I. Regulation of the Na+/Ca2+ exchanger in rat pancreatic ducts. J Membr Biol. 2002;186:43-53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 81. | Quednau BD, Nicoll DA, Philipson KD. Tissue specificity and alternative splicing of the Na+/Ca2+ exchanger isoforms NCX1, NCX2, and NCX3 in rat. Am J Physiol. 1997;272:C1250-C1261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 330] [Cited by in F6Publishing: 320] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 82. | Hamming KS, Riedel MJ, Soliman D, Matemisz LC, Webster NJ, Searle GJ, MacDonald PE, Light PE. Splice variant-dependent regulation of beta-cell sodium-calcium exchange by acyl-coenzyme As. Mol Endocrinol. 2008;22:2293-2306. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 83. | Herchuelz A, Diaz-Horta O, van Eylen F. Na/Ca exchange and Ca2+ homeostasis in the pancreatic beta-cell. Diabetes Metab. 2002;28:3S54-60; discussion 3S108-12. [PubMed] [Cited in This Article: ] |
| 84. | Van Eylen F, Bollen A, Herchuelz A. NCX1 Na/Ca exchanger splice variants in pancreatic islet cells. J Endocrinol. 2001;168:517-526. [PubMed] [Cited in This Article: ] |
| 85. | Rorsman P, Renström E. Insulin granule dynamics in pancreatic beta cells. Diabetologia. 2003;46:1029-1045. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 603] [Cited by in F6Publishing: 554] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 86. | Bruce JI, Yang X, Ferguson CJ, Elliott AC, Steward MC, Case RM, Riccardi D. Molecular and functional identification of a Ca2+ (polyvalent cation)-sensing receptor in rat pancreas. J Biol Chem. 1999;274:20561-20568. [PubMed] [Cited in This Article: ] |
| 87. | Herchuelz A, Diaz-Horta O, Van Eylen F. Na/Ca exchange in function, growth, and demise of beta-cells. Ann N Y Acad Sci. 2002;976:315-324. [PubMed] [Cited in This Article: ] |
| 88. | Herchuelz A, Kamagate A, Ximenes H, Van Eylen F. Role of Na/Ca exchange and the plasma membrane Ca2+-ATPase in beta cell function and death. Ann N Y Acad Sci. 2007;1099:456-467. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 89. | Herchuelz A, Pachera N. The Na+/Ca2+ exchanger and the Plasma Membrane Ca2+-ATPase in β-cell function and diabetes. Neurosci Lett. 2018;663:72-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 90. | Van Eylen F, Horta OD, Barez A, Kamagate A, Flatt PR, Macianskiene R, Mubagwa K, Herchuelz A. Overexpression of the Na/Ca exchanger shapes stimulus-induced cytosolic Ca(2+) oscillations in insulin-producing BRIN-BD11 cells. Diabetes. 2002;51:366-375. [PubMed] [Cited in This Article: ] |
| 91. | Petersen OH, Tepikin AV, Gerasimenko JV, Gerasimenko OV, Sutton R, Criddle DN. Fatty acids, alcohol and fatty acid ethyl esters: toxic Ca2+ signal generation and pancreatitis. Cell Calcium. 2009;45:634-642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 92. | Gerasimenko JV, Gryshchenko O, Ferdek PE, Stapleton E, Hébert TO, Bychkova S, Peng S, Begg M, Gerasimenko OV, Petersen OH. Ca2+ release-activated Ca2+ channel blockade as a potential tool in antipancreatitis therapy. Proc Natl Acad Sci U S A. 2013;110:13186-13191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 137] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 93. | Vigna SR, Shahid RA, Liddle RA. Ethanol contributes to neurogenic pancreatitis by activation of TRPV1. FASEB J. 2014;28:891-896. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 94. | Yu SY, Xie R, Chen YY, Yang SM, Zhu B. Role of sodium-calcium exchanger-1 in development of rat acute pancreatitis. Di-San Junyi Daxue Xuebao. 2015;37:1325-1330. [DOI] [Cited in This Article: ] |
| 95. | Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8283] [Cited by in F6Publishing: 8159] [Article Influence: 509.9] [Reference Citation Analysis (0)] |
| 96. | Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ, Wiebke EA, Wiesenauer CA, Baumgardner JA, Cummings OW, Jacobson LE, Broadie TA, Canal DF, Goulet RJ Jr, Curie EA, Cardenes H, Watkins JM, Loehrer PJ, Lillemoe KD, Madura JA. Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch Surg. 2004;139:718-25; discussion 725-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 269] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 97. | Truty MJ, Urrutia R. Basics of TGF-beta and pancreatic cancer. Pancreatology. 2007;7:423-435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 98. | Dong H, Shim KN, Li JM, Estrema C, Ornelas TA, Nguyen F, Liu S, Ramamoorthy SL, Ho S, Carethers JM, Chow JY. Molecular mechanisms underlying Ca2+-mediated motility of human pancreatic duct cells. Am J Physiol Cell Physiol. 2010;299:C1493-C1503. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 99. | Xu JY, Jiang YX, Xie R, Jin H, Wen GR, Tuo BG. The expression of NCX1 and its effect on proliferation and migration of hepatocellular carcinoma cells through regulation of intracellular Ca2+. Zhongguo Aizheng Zazhi. 2016;26:735-742. [DOI] [Cited in This Article: ] |
| 100. | Guan LY, Fu PY, Li PD, Li ZN, Liu HY, Xin MG, Li W. Mechanisms of hepatic ischemia-reperfusion injury and protective effects of nitric oxide. World J Gastrointest Surg. 2014;6:122-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 121] [Cited by in F6Publishing: 119] [Article Influence: 11.9] [Reference Citation Analysis (1)] |
| 101. | Vasques ER, Cunha JE, Coelho AM, Sampietre SN, Patzina RA, Abdo EE, Nader HB, Tersariol IL, Lima MA, Godoy CM, Rodrigues T, Chaib E, D'Albuquerque LA. Trisulfate Disaccharide Decreases Calcium Overload and Protects Liver Injury Secondary to Liver Ischemia/Reperfusion. PLoS One. 2016;11:e0149630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 102. | Nakamura T, Arii S, Monden K, Furutani M, Takeda Y, Imamura M, Tominaga M, Okada Y. Expression of the Na+/Ca2+ exchanger emerges in hepatic stellate cells after activation in association with liver fibrosis. Proc Natl Acad Sci U S A. 1998;95:5389-5394. [PubMed] [Cited in This Article: ] |
| 103. | Xu J, Yang Y, Xie R, Liu J, Nie X, An J, Wen G, Liu X, Jin H, Tuo B. The NCX1/TRPC6 Complex Mediates TGFβ-Driven Migration and Invasion of Human Hepatocellular Carcinoma Cells. Cancer Res. 2018;78:2564-2576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 104. | Tian Y, Zhu MX. A novel TRPC6-dependent mechanism of TGF-β-induced migration and invasion of human hepatocellular carcinoma cells. Sci China Life Sci. 2018;61:1120-1122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 105. | Rusolo F, Pucci B, Colonna G, Capone F, Guerriero E, Milone MR, Nazzaro M, Volpe MG, Di Bernardo G, Castello G, Costantini S. Evaluation of selenite effects on selenoproteins and cytokinome in human hepatoma cell lines. Molecules. 2013;18:2549-2562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 106. | Xu J, Ji B, Wen G, Yang Y, Jin H, Liu X, Xie R, Song W, Song P, Dong H, Tuo B. Na+/H+ exchanger 1, Na+/Ca2+ exchanger 1 and calmodulin complex regulates interleukin 6-mediated cellular behavior of human hepatocellular carcinoma. Carcinogenesis. 2016;37:290-300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |