Published online Sep 21, 2018. doi: 10.3748/wjg.v24.i35.4000
Peer-review started: June 24, 2018
First decision: July 6, 2018
Revised: July 23, 2018
Accepted: August 1, 2018
Article in press: August 1, 2018
Published online: September 21, 2018
Hepatocellular carcinoma (HCC) is one of the most common and fatal cancer in the world. HCC frequently presents with advanced disease, has a high recurrence rate and limited treatment options, which leads to very poor prognosis. This warrants urgent improvement in the diagnosis and treatment. Liver biopsy plays very important role in the diagnosis and prognosis of HCC, but with technical advancements and progression in the field of imaging, clinical guidelines have restricted the role of biopsy to very limited situations. Biopsy also has its own problems of needle tract seeding of tumor, small risk of complications, technical and sampling errors along with interpretative errors. Despite this, tissue analysis is often required because imaging is not always specific, limited expertise and lack of advanced imaging in many centers and limitations of imaging in the diagnosis of small, mixed and other variant forms of HCC. In addition, biopsy confirmation is often required for clinical trials of new drugs and targeted therapies. Tissue biomarkers along with certain morphological features, phenotypes and immune-phenotypes that serve as important prognostic and outcome predictors and as decisive factors for therapy decisions, add to the continuing role of histopathology. Advancements in cancer biology and development of molecular classification of HCC with clinic pathological correlation, lead to discovery of HCC phenotypic surrogates of prognostic and therapeutically significant molecular signatures. Thus tissue characteristics and morphology based correlates of molecular subtypes provide invaluable information for management and prognosis. This review thus focuses on the importance of histopathology and resurgence of role of biopsy in the diagnosis, management and prognostication of HCC.
Core tip: Liver biopsy plays important roles in the diagnosis and prognosis of hepatocellular carcinoma. However biopsy related complications and limitations along with advancements in imaging have restricted its role to very limited situations. In recent time, studies on tissue biomarkers, molecular classifications and targeted therapies for hepatocellular carcinoma (HCC) with their clinic-pathologic correlations have highlighted that morphologic variants and subtypes can serve as importance surrogates of molecular signatures, thus renewing the interest in tissue analysis. Tumor biopsy thus is increasingly being recognized as an invaluable tool for the diagnosis, management and prognostication of HCC.
- Citation: Rastogi A. Changing role of histopathology in the diagnosis and management of hepatocellular carcinoma. World J Gastroenterol 2018; 24(35): 4000-4013
- URL: https://www.wjgnet.com/1007-9327/full/v24/i35/4000.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i35.4000
Hepatocellular carcinoma (HCC) is the sixth most common cancer in the world[1-4], with an increasing incidence each year. It is also one of the most lethal human malignant tumor with > 600000 deaths per year worldwide[1,4] making it the third leading cause of cancer related death[5,6]. Dismal prognosis of HCC is attributable to advanced disease at presentation, high rates of metastases and recurrence along with the limited and unsuccessful treatment options available[7,8]. Also, Amongst the primary liver cancers, HCC is the most common, accounting for 70%-85% of all the histological types[9,10]. Major risk factors of HCC are infection with hepatitis B and hepatitis C, excess alcohol intake, obesity, diabetes and metabolic diseases[7,11]. These risk factors cause repeated episodes or sustained state of inflammation, resulting in progressive fibrosis and cirrhosis, along with development of preneoplastic lesions with stem cells acting as a nidus for HCC[12,13]. Literature indicates that 70%-97% of patients with HCC have underlying cirrhosis of the liver at the time of diagnosis[14]. Poor clinical outcome makes it imperative to advance our understanding of HCC at the cellular level and improve methods for the early diagnosis and treatment particularly targeted therapies. HCC is diagnosed by the non-invasive methods of imaging and tumor markers and by the invasive techniques of biopsy and aspiration. Lesion biopsy in HCC, like other solid organs provide valuable information about the diagnosis, prognosis and in certain circumstances, guide about treatment decisions, however biopsy in the HCC and cirrhotic milieu is controversial and is superseded by imaging[6,15]. Certain biopsy limitations especially needle tract seeding, sampling errors and small risk of morbidity along with the technical advancements in imaging, undermined the importance of tissue analysis. This led most of the international guidelines on HCC to restrict the role of liver biopsy to characterize the lesions in non-cirrhotic liver or those with equivocal imaging. However, imaging technologies also have certain caveats, cautioning against abandon of histopathology assessment for HCC. Tumor histopathology, besides being an important diagnostic tool, plays numerous other important roles such as distinguishing from metastasis and other primary benign or preneoplastic lesions, in prognostication and influencing treatment decisions, which cannot be substituted by imaging techniques or tumor markers. With increasingly accumulating data on prognostic and therapeutic importance of specific phenotypes and distinct molecular-morphologic correlates, there is resurgence of interest in the role of tissue evaluation.
The recent diagnostic approach for HCC is based on imaging studies, restricting the role of histopathology to only certain situations. Clinical guidelines of American Association for the Study of Liver disease, European Association for the Study of the Liver (EASL) and Asian-Pacific Association for the Study of Liver have changed the diagnostic criteria for HCC[2,16-18], recommending radiology in view of the remarkable advances in techniques that have led to very high sensitivity and specificity for the diagnosis of HCC[19]. A recent systematic review and meta-analysis for studies comparing CT with extracellular contrast-enhanced MRI or gadoxetate-enhanced MRI in adults with cirrhosis and suspected HCC, found that all them performed better for HCC ≥ 2 cm in comparison to lesions < 1 cm. For all tumor sizes, studies showed significantly higher sensitivity for MRI over CT, with no difference in the specificity between techniques[20]. Typical imaging findings of intense uptake of contrast during the arterial phase followed by decreased enhancement and washout during the portal phases, based on the neo-arterial supply feeding the HCC, by even a single contrast enhanced imaging study is considered sufficiently specific for the diagnosis of HCC[2,16-18,21]. Thus, biopsy is not advocated for the diagnosis of HCC, if typical features are present on dynamic imaging technique[16-18,22].
Imaging techniques falter in certain situations and histopathology assessment becomes mandatory for the diagnosis of all equivocal lesions, irrespective of the size[6], reported in 10%-15% of patients[23]. Lesion in a cirrhotic patient that lacks typical imaging characteristics, histopathological evaluation is the recommended diagnostic tool. Imaging alone has been found to be insufficient to diagnose well-differentiated HCC.
Biopsy has advantage over imaging as comparison with non-lesional liver tissue provides vital information, particularly for the diagnosis of well-differentiated HCC. Horigome et al[24] reported that digital subtraction angiography and magnetic resonance imaging in the absence of biopsy, could diagnose HCC in only 58% of well-differentiated HCC. Dynamic imaging has been shown to have a sensitivity of 35%-71% in different series for tumors of less than 2 cm size[25-29], attributable to hypovascularity of small HCC. Another limitation of imaging is the requirement of pathologic diagnosis for all nodules developing in the non-cirrhotic background[6]. Also, false positives, as high as 33%[30,31], have been reported with the radiology techniques for diagnosing HCC. A study reported that many nodules detected by ultrasound were not found on computed tomography[32,33]. Similarly, 41% and 30.8% of the imaging based cases turned out to be non-HCC on biopsy or follow-up[30]. Without biopsy confirmation, these cases might get subjected to unnecessary transplantation, resection and other therapies. Strength of tissue analysis to determine the malignant potential and histogenesis of liver lesions is another major constraint with imaging. Combined hepato-cholangiocarcinoma (cHCC-CC) is difficult to diagnose and characterize by the imaging alone[34]. Lack of skill and absence of advance imaging technologies in many centers, are other constraints, requiring histopathology assessment for confirmation. Such limitations of imaging compel tissue confirmation in a significant number of cases.
Role of serum α-feto protein (AFP) in the diagnosis of HCC although controversial, is still recommended by certain guidelines[35]. In situations, where imaging is atypical, AFP levels are useful for diagnosing HCC when biopsy needs to be avoided in view of the risk of tumour seeding[36-38]. Studies have shown that increasing AFP levels before liver transplantation are associated with an increased risk of tumor recurrence and decreased survival following transplantation[39,40]. Serum AFP levels are not influenced by technical factors, skill, observer variability thus still has an important role in surveillance, diagnosis, prediction of outcome and monitoring treatment response[41].
The declining interest for biopsy is due to several issues. There are risks associated with the procedure, that include morbidity due to the most frequent complication, i.e., pain[42,43] and bleeding especially in patients with cirrhosis who are at a higher risk of this complication. Incidence of such minor complications is 5.9%[44]. Significant hemorrhage occurs in 0.5%[45]. There is slight risk of mortality[46,47], with incidence of 0.11% reported in experienced centers[48]. Evaluation of sixty-four series reporting 7649 TJLBs revealed minor and major complication rates to be 6.5% and 0.56%, respectively with mortality in adults to be 0.09%[49]. However, a large series of 16648 guided biopsies and 3035 therapeutic procedures performed in 13222 patients, overall mortality was reported in 0.06%[50].
Needle track seeding of malignant cells is another important concern, especially in patients who might otherwise benefit from liver transplantation. The reported incidence of tumor seeding following a liver biopsy ranges between 1.6%-5.1%[51-55], however one of the largest series has reported this complication in only 0.76% in their experience[19,56] In a systematic review and meta-analysis of eight observational studies, it was shown that the incidence of needle tract tumour seeding following biopsy of a HCC is 2.7% overall, or 0.9% per year[57]. Other studies have emphasized not to preclude the biopsy if management can be altered based on the biopsy interpretation, supporting this is the fact that 2.5% unnecessary surgery are conducted if the patient is not biopsied[58].
Technical challenges are another section which limits the utility of biopsy. Small lesions which are < 2 cm are often difficult to target, leading to high false-negatives[19]. Distinction of well-differentiated HCC from preneoplastic and regenerative focus is also a problem area. Characteristic histomorphologic profile in combination with reticulin stain and immunohistochemistry for HSP70 and Glutamine synthetase, can differentiate hepatocellular adenoma from HCC, however well-differentiated HCC is often difficult to distinguish[59-61]. Tumor heterogeneity, necrosis and inadequacy or failed sampling of the suspected lesion, all add to the inferior results of biopsy with the risk of mismanagement after diagnostic errors. Negative predictive value is very low in such setting (14%)[51,62,63].
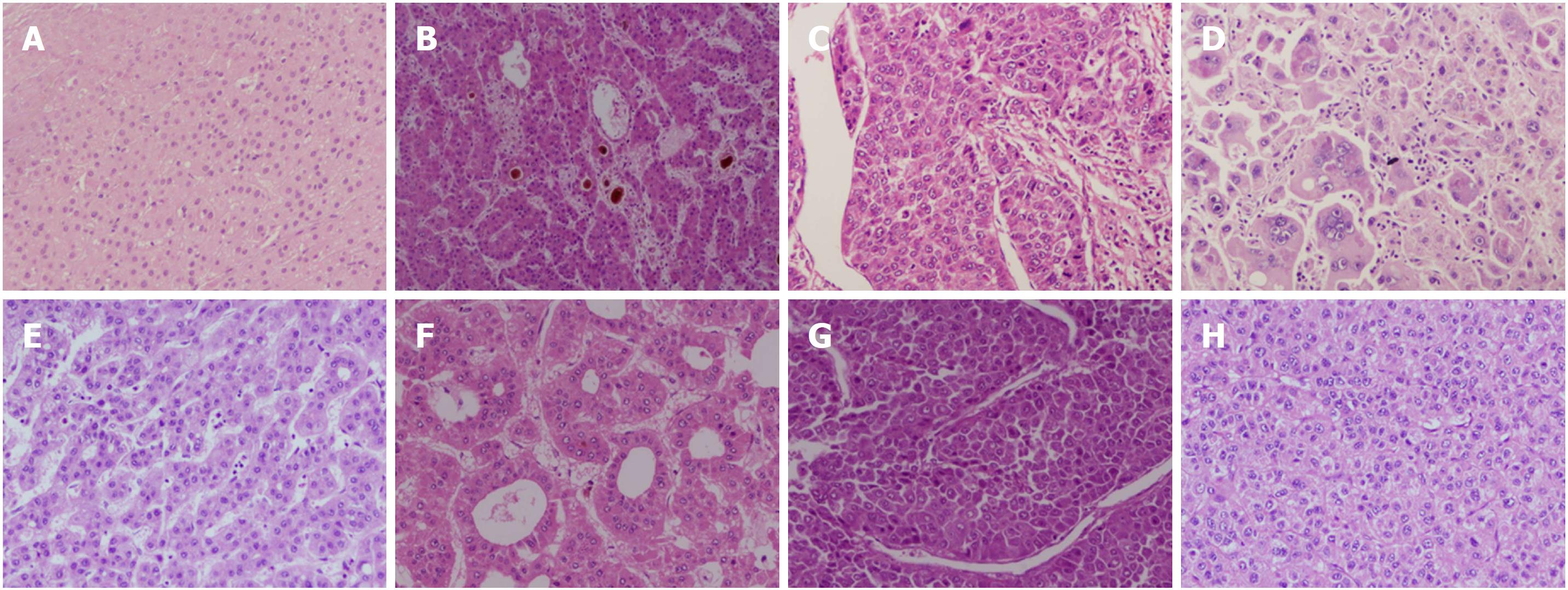
Tumor histopathology, besides being an important diagnostic tool, plays numerous other important roles such as distinguishing from other lesions, prognostication and influencing treatment decisions, which cannot be substituted by imaging techniques or tumour markers. Assessment of histological parameters in tumour resection specimens has been shown to predict recurrence and metastatic potential and thus indicate the need for salvage transplantation[64-67]. Biopsy tissue and archived blocks are important source for teaching, knowledge sharing, correlation with translational research and biomarker development. Several histopathology parameters had been extensively studied and shown to be significant predictors of prognosis, highlighting the role of tissue analysis in HCC. The most studied parameters which are also linked to prognosis are tumor number, size, cell differentiation and grade, presence of satellite nodules, pTNM stage[68]. (Figure 1)
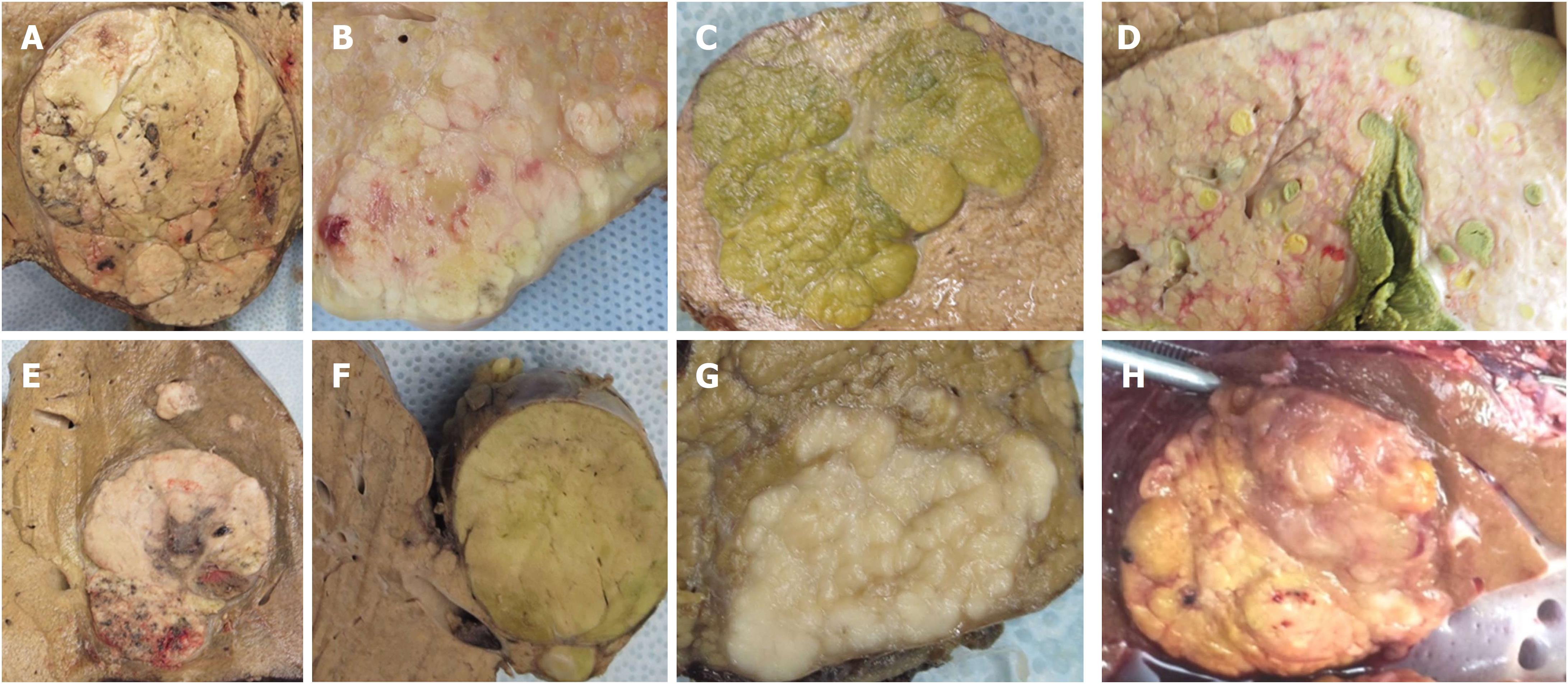
HCC is a heterogeneous tumor with varied gross and microscopic appearances. A study from Seoul had shown that gross features are also independent predictor of overall and disease-free survival regardless of tumor size. They classified 242 HCC resection specimens based on the gross appearance into vaguely nodular, expanding nodular, multinodular confluent, nodular with perinodular extension and infiltrative types[5]. Infiltrative type had the worse prognosis whereas vaguely nodular and expanding nodular had more favorable prognosis. Similar results in small HCC and in HCC > 10 cm[69,70] and in patients treated with RFA[5,71], verify that gross morphology is an important predictor of prognosis. (Figure 2)
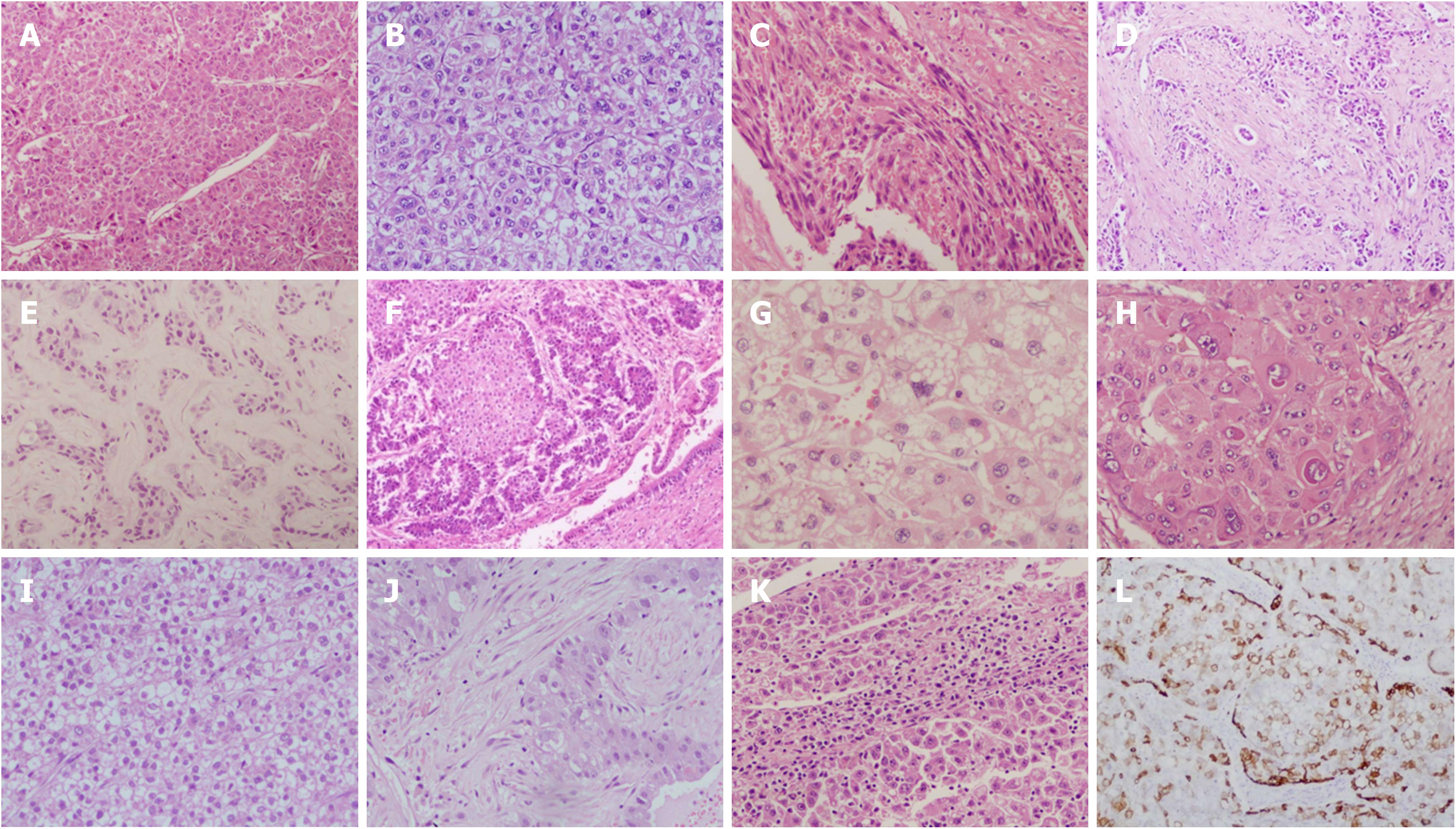
Four major growth patterns in HCC are trabecular (70%), solid (20%), pseudo glandular (10%) and macrotrabecular (1%)[72]. Of these, macrotrabecular pattern has recently been shown to have significant clinical relevance[73,74]. Morphology based segregation into histological subtypes[72,75] such as fibro lamellar carcinoma[76,77], lymphoepithelioma like carcinoma[78], steatohepatitis HCC[79], combined hepatocholangiocarcinoma[75], and histological subtype with stem cell markers[80,81] have independent prognostic importance. Others such as Clear cell HCC has been demonstrated to be smaller, better differentiated with lower rates of vascular invasion[82,83], whereas the sarcomatoid HCC is a poorly differentiated subtype[72]. Several recent studies have also highlighted distinctive clinical, biological and molecular characteristics associated with these phenotypes and subtypes, with creditable prognostic implications[84,85] (Figure 3).
In a recent study by Ziol et al[74] Macrotrabecular-massive is a newly described subtype of HCC, found in 12% of the cohort of 237 HCC surgical samples and 284 HCC liver biopsies. Authors have defined this entity by the presence of a predominant (> 50%) macrotrabecular architecture (more than 6 cells thick). This phenotype was associated with poor prognostic factors like tumor size, α-Feto protein (AFP) level, satellite nodules, and vascular invasion and was found to be an independent predictor of early and overall recurrence[74]. Lauwers et al[86] noted macrotrabecular -predominant architecture in 26.6% of their 425 cases of resected HCC. In comparison to the compact architecture they had worse overall survival. Prognostic information derived from phenotypes reemphasizes the potential benefits of biopsy add to reviving its importance[74].
Combined hepatocellular-cholangiocarcinoma (cHCC-CC) representing 0.4%-14.2% of primary liver cancers is an aggressive tumor associated with poor outcome[34,87-90]. Histopathological evaluation is crucial for diagnosis, as this entity lacks the typical imaging characteristics thus often misdiagnosed by radiology. cHCC-CC was first described by Allen and Lisa in 1949[91] was updated by Goodman in 1985[92]. In 2010, WHO classified it into classical subtype and subtypes with stem cell features[92]. In a study of sixty-two patients of cHCC-CC, stem cell subtypes (WHO criteria), were found in various amount and combinations in all of their patients with typical subtype in 16%, intermediate cell type in 83.9% and cholangiolocellular type (CLC) in 71%[93]. cHCC-CC has been shown in a study, to have 1-year and 3-year survival rates of 81.9% and 47% respectively, which suggest a better prognosis than CC but worse compared with HCC[88]. Similarly, another study has found 1, 3 and 5 year overall survival rates of 53%, 26% and 12% respectively, supporting their biological behavior intermediate between HCC and CC[90,94]. Knowledge of mixed tumor by biopsy evaluation prior to surgery, can guide the type of resection including the lymph node dissection. Recently, consensus terminology for primary liver carcinomas with both hepatocytic and cholangiocytic differentiation has been published[8] which emphasizes that stem cell phenotypes and features can coexist within combined HCC-CC and should be reported in a descriptive report. Sub classifying stem cells is not necessary. Presence of two other types of primary liver cancers - CLC and intermediate cell carcinoma were described, which may coexist with HCC, intrahepatic cholangiocarcinoma or cHCC-CC. Although the minimum cut-off of HCC and CC to qualify for the diagnosis of cHCC-CC is uncertain, the accepted criteria to qualify as CLC is > 80% of the tumor comprising CLC[8]. This phenotype is very important, with prognostic implications[93]. CLC exhibits increased expression of ABC transporters and is linked with a worse prognosis, chemo resistance, and an aggressive behavior[95]. Meta-analyses of twelve articles involving 1344 patients showed that the presence of cancer stem cells (CSCs) was significantly associated with a poor histological grade[96]. HCC expressing stem cells marker keratin 19 (K19), also known as HCC with “stem cell features” or “progenitor features” display immunohistochemical expression of K19 in > 5% of tumor cells[97,98]. This particular tumor subtype gene expression profile with oval cells and fetal hepatoblasts[97-99]. It has adverse clinical outcome with worse postoperative survival rate.
Small suspicious nodules are difficult to detect and characterize by the imaging modalities. Vascular characteristics and capsule formation are not completely developed hence such lesions lack the typical imaging characteristics. Histopathology evaluation is required in around 60% of such cases, for early and correct diagnosis[24]. Hepatocellular nodules were classified by the International working party in 1995[100] and further characterized by the International consensus group for hepatocellular neoplasia in 2009[101], which classified small HCC (< 2 cm in size) as early HCC and progressed HCC. (Figure 4)
Pathology based differentiation of HCC from other nodular lesion found in chronic liver disease such as large regenerative nodule, low grade dysplastic nodule (LGDN) and high grade dysplastic nodule (HGDN) has become one of the most important accomplishments and indications of biopsy, gaining importance in view of surveillance programs and early detection of HCC. Biopsy is often recommended for nodules 1.0 cm or larger to make a differential diagnosis between early HCC and a DN[102]. Immunohistochemsitry provides crucial support in such diagnostic dilemmas. Glypican-3, heat shock protein 70 and glutamine synthetase are used as single panel for delineation of HCC from other suspicious nodules[72]. LGDNs and large regenerative nodules (LRNs) are negative for the panel. In a study, all negative phenotype was noted in 100% of LRNs, 100% of LGDNs, 72.7% of HGDNs and 3.1% of early HCC[103-105]. Studies have shown that if two of these three stains are positive, the sensitivity and specificity for the detection of HCC is 60%-70% and 100% respectively[10]. Tommaso et al[104], has reported that addition of clathrin heavy chain to this panel, improved diagnostic accuracy to 84.3% for small HCCs. Hepatocyte paraffin 1, arginase 1, polyclonal CEA, CD10 and several other tissue markers that are frequently performed for confirmation of diagnosis, differentiation of HCC from metastatic carcinoma, identifying HCC in poorly differentiated and necrotic tumors as well as a protocol tissue based diagnosis confirmation before enrolment in phase III clinical trials of novel drugs[68,106,107].
Grading of HCC cellular differentiation, pathological tumor node metastasis stage and vessel invasion are reported as the most important histoprognostic features[22,72,108].
Edmondson and Steiner system of HCC (ES) grading, published in Cancer in 1954[109], is the most widely adopted classification[86]. It divides HCC into four grades based on histological differentiation with grade 1 being the best differentiated. Current three-tier classification of HCC into well-, moderately- and poorly differentiated HCC is also based on this system, combining architectural and nuclear features[110,111], pTNM staging based on 8th edition of AJCC staging, which is based on number, size and vessel invasion, provides crucial prognostic information, guides about therapeutic decisions and is an essential component of research and clinical studies. 8th ed. of pTNM lays emphasizes on separation of small HCC and on vessel invasion by modifying pT1 and pT4 respectively[112].
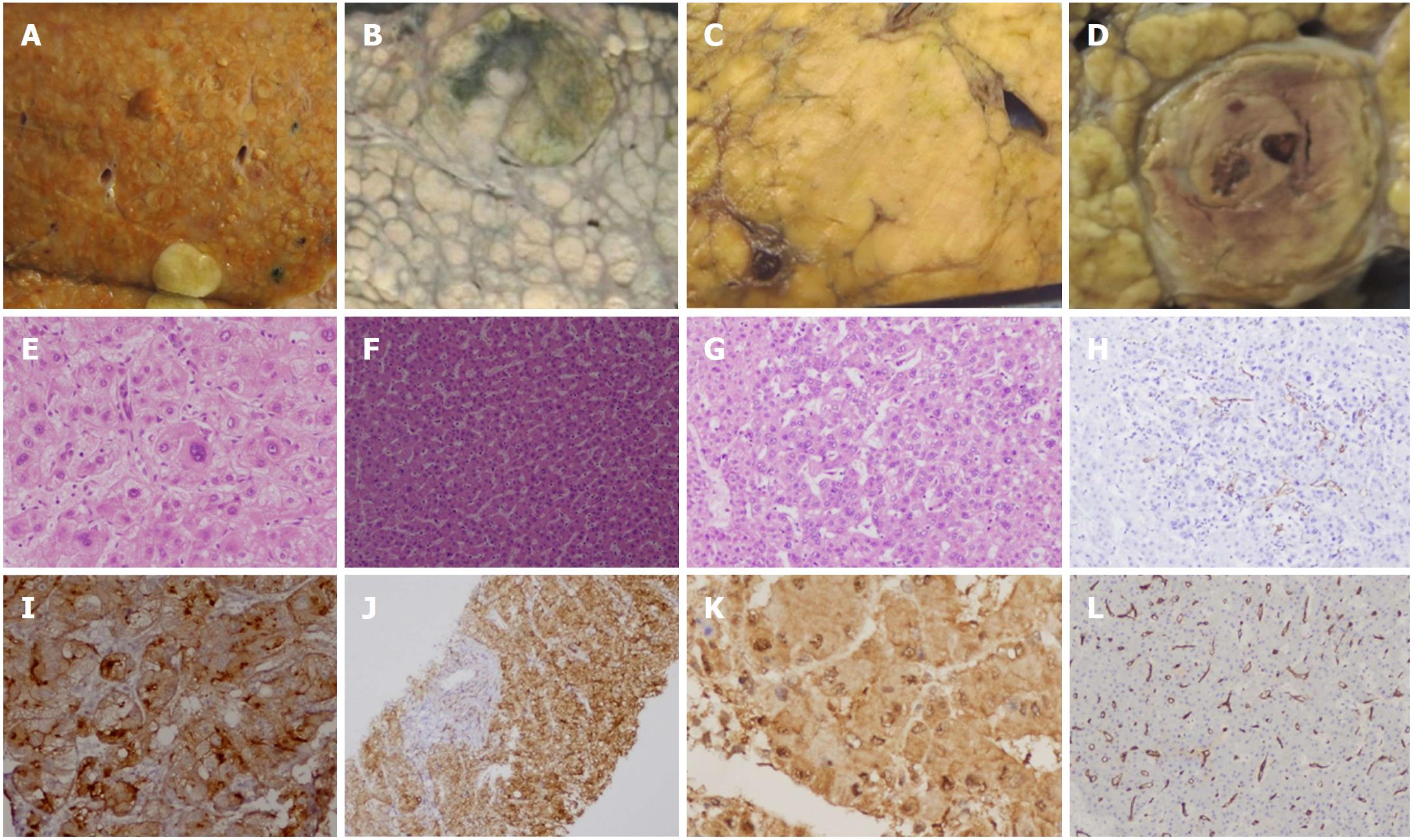
Macro vascular and Micro vascular (MVI) invasion is the major predictor of prognosis of HCC and are associated with more advanced tumor stage, disease progression, local invasion and distant metastasis[86,113]. Identification of MVI is feasible only on histopathological examination of resected surgical specimens[114]. Incidence of MVI after surgical resections and liver transplantation has been shown to be between 15% and 57%[114-116]. Pawlik et al[115], reported MVI to occur at the rates of 25%, 40%, 55% and 63% in HCC < 3, 3-5, 5-6.5, and > 6.5 cm. Similarly, Yamashita et al[117] has also shown 28.9% of the small HCC has MVI, with 1-year recurrence rates of 7.5% and 23.3% for patients without and with MVI. A systematic review of 20 observation studies investigating prognostic role of MVI in patients who had undergone liver transplantation or resection, highlight the adverse impact of MVI on disease free and overall survival[118]. Different studies have graded MVI based on the number of vessels invaded[119] as well as have sub typed them into adhesion, invasion and breakthrough types and found association with long-term survival[120]. Distance of embolized vessel from the main tumor has prognostic significance with 1 cm cut-off shown in studies to predict very poor outcome[121]. MVI detection helps to identify patients at risk of development of distant metastasis post-resection and guides for the need of adjuvant therapy[114]. There is an urgent need for prediction of MVI in biopsies to guide therapeutic strategy. However, currently neither the detection of MVI in biopsy is possible nor any validated surrogate markers of MVI are available[122]. A recent pilot study assessed the performance of IHC panel of three biomarkers of MVI (H4K16ac, H4K20me2, PIVKA-II) in a test set of 64 HCC surgical specimens and 42 core needle biopsies of HCC. In this study combination of PIVKA-II with H4K20me2 showed the best accuracy for prediction of mVI, with very high specificity and PPV in HCC core needle biopsies[123].
Several studies have highlighted the prognostic relevance of histological grade, stage and MVI[124-126]. Analysis of eighteen registries comprising 570 transplanted patients revealed MVI in 16% and poor differentiation of tumor in 12%. These features were significant risk factors for dismal cancer specific survival[127]. Similar, prognostic significance of MVI and grade 3, in predicting overall survival, disease free survival and recurrence, had been found in 151 patients transplanted for HCC, by Donat et al[124] and by Lauwers et al[86] in their 425 HCC resections. In a study of 116 patients of large HCC resection, MVI and ES grade were reported as predictors of early recurrence[128]. Poor differentiation in a single HCC or in the largest HCC in a pre-transplant biopsy indicates aggressive tumour biology associated with poor prognosis. Certain centers exclude transplantation and assign patients to other treatment modalities, based on such prognosis and management related effects of biopsy[129,130].
Several biomarkers have been investigated in HCC for prognostication and treatment decisions. K19 expressing HCCs show aggressive behavior, poor differentiation, high proliferative index and high recurrence rate[131-133]. Similarly, expression of stem cell marker CD133 is associated with higher tumor grade, advanced disease stage, higher recurrence rates and shorter overall survival[134]. EpCAM expression also demonstrates poor prognosis[5,134]. In a recent study, progressed HCC with > 5% tumor fraction expressing stem/progenitor cell markers CK19, EpCAM and CD133, displayed more aggressive behavior with increased likelihood of recurrence, chemo-resistance and metastasis[135].
Tumor tissue expression of high Wnt-1 shows correlation with nuclear B-catenin accumulation and increased rate of tumor recurrence. In a study of 142 patients of HCC, correlation of 3 groups: Biliary/stem cell marker positive group, Wnt/B-catenin signaling related marker positive, and both negative group was done with other prognostic features. Biliary/stem cell marker positive group demonstrated poor tumor differentiation, high frequency of portal vein invasion, intrahepatic metastasis and high proliferative activity[132].
HCC are hyper vascular and tumor angiogenesis is a known important prognostic factor. Immunohistochemical staining for endothelium specific markers CD31, CD34 or vWF allow semi quantitative assessment of micro vessel density, which is a significant prognostic indicator[136,68]. Li et al[137] performed meta-analysis of 12 articles comprising a total 1138 HCC patients. Survival outcomes showed positive correlation between poor prognosis and high micro vessel density levels.
Molecular markers with prognostic significance are analyzed by tissue markers and abundant literature is available on studies of phenotypic correlates. DNA ploidy, cell proliferation markers, Cell surface proteins Glypican-3, cytoskeleton proteins Fascin, enzymes Histone deacetylase, transcription factors BATF2, tumor suppressor genes TP53, adhesion molecule E-cadherin, cell cycle regulators, oncogenes, tumor angiogenesis related markers and several others related to Notch, Hippo, Hedgehog and other signaling pathways, have been analyzed in tissues and shown to be of prognostic significance[103,138].
IHC markers are also increasingly being used for the decisions of molecular targeted therapy and as a predictor of therapeutic response[22,139]. Six areas of genomic alterations which have targetable potential for HCC are TERT promoter mutation, p53 pathway, oxidative stress pathway, Wnt-B catenin pathway, epigenetic, AKT/mTOR and MAP kinase pathway[22]. Evaluation of c-MET at the tissue level had been related to response to Tivantinib[106,140,141] with several such phase II and phase III ongoing trials are linked to molecular analysis of tissue samples.
Immune biomarkers such as immune checkpoint-inhibiting antibodies anti-PD-1, anti-PD-L1 and anti-CTLA-4 are useful for decisions regarding adjuvant therapy[142-144]. PD-L1 can predict response to anti-PD-1 antibody. A recent study assessed 294 HCC samples for the expression of PD-1, PD-L1 and CTLA-4. High PD-L1 staining was associated with poor disease-free survival and simultaneous increased expression of PD-L1 and CD68+ TIL was reported to be an important prognostic factor related to immune checkpoint pathway in HCC[145,146]. Advances related to determination and response assessment to the targeted therapies are dependent on archived tissues in institutions and bio-banks. This further highlights the revival of importance of tissue procurement and analysis. Phase III studies of novel targeted therapies require biopsy confirmation of diagnosis, and assessment of treatment response as in a study of 30 patients of HCC treated by Radiofrequency ablation (RFA) and check point inhibitor[147].
Histopathological features can predict prognosis and lately, linkage of prognosis to distinct biological phenotypes has been demonstrated[84,85]. HCC phenotype may be associated with activation of specific oncogenic pathways thus histopathological parameters and molecular markers acting in concert can be very useful prognostic predictors[85]. HCC phenotypes are associated with distinct molecular pathways and such association is recently being the focus point due to the tremendous scope for advancement in HCC therapy. Transcriptomic classifications by Tan et al[84] and Calderaro et al[85] deserve special mention in this context.
In the study by Calderaro et al[85], CTNNB1 and TP53 defined two distinct tumor phenotypes in a large series of 343 cases of surgically resected HCC. Using pathology, immunohistochemistry, gene expression profiling and sequencing; patho-molecular correlates were classified into G1-G6 based on transcriptomics. Tumors associated with CTNNB1 mutations were large, well-differentiated, cholestatic, with microtrabecular/pseudo glandular pattern whereas TP53 mutated tumors were poorly differentiated, with multinucleated, pleomorphic cells arranged in compact pattern and displayed frequent vascular invasion. G1-G3 subclasses demonstrated correlation with histological features of poor differentiation, frequent macro vascular invasion, foci of clear cells, sarcomatous change, compact and macrotrabecular pattern, and foci of pleomorphic and multinucleated cells. Whereas G4-G6 subclasses, revealed low cell proliferation, association with small tumor size, lack of satellite nodules or micro vascular invasion, and tumors were well-differentiated.
In the study by Tan et al[84], 96 tumor tissues were used for the development of clinic pathological indices predictive of HCC molecular subclass. HCC transcriptome had been characterized into 3 subtypes S1-S3[148], determined by genome-wide transcriptome profiling, with potential therapeutic targets. S1 reflected aberrant activation of the WNT signaling pathway, S2 was characterized by proliferation as well as MYC and AKT activation, and S3 was associated with hepatocyte differentiation[46,148]. Predictive indices in the study by Tan et al[84] were validated in 99 HCC tumors. Phenotypic molecular correlation with S1-S3 based on transcriptomic analysis, revealed steatohepatitic HCC and immune cell infiltrates represented S1, macrotrabecular or compact pattern, lack of pseudo glands belonged to S2 and microtrabecular low histological grade and lack of steatohepatitis and clear cell patterns constituted S3 subclass. Macrotrabecular pattern/S2 showed activation of therapeutically targetable oncogene YAP and stemness markers EPCAM, keratin 19[84].
Similar histomorphology correlates of molecular characteristics were reported in scirrhous subtype and TSC1/ TSC2 mutations and steatohepatitis subtype with IL-6/ JAK/ STAT activation[85].
Histopathological evaluation of HCC tissue has time tested applications in the diagnosis and prognosis (Table 1). Pathology combined with immunohistochemistry is essential for the differentiation of HCC from preneoplastic lesions, from metastatic diseases and other primary liver tumors. Certain biopsy limitations especially needle tract seeding, sampling errors and small risk of morbidity along with the technical advancements in imaging, undermined the importance of tissue analysis. This led most of the international guidelines on HCC to restrict the role of liver biopsy to characterize the lesions in non-cirrhotic liver or those with equivocal imaging. Other advantages of biopsy including the role in prognostication, therapy decision, research and clinical trials along with teaching and archiving in biobank, all suffered indirectly due to lesser availability of tissue specimens. With increasingly accumulating data on prognostic and therapeutic importance of specific phenotypes and distinct molecular-morphologic correlates, there is resurgence of interest in the role of tissue evaluation. Analysis of tumor biopsies allows clinicians to fine tune therapies. Molecular subclasses with phenotypic surrogates will be valuable for predicting response to specific targeted therapies for HCC. HCC morphologic correlates of prognostically important molecular signatures need to be explored further to alleviate the HCC complications of recurrence, intra-hepatic and distant metastasis, responsible for dismal prognosis of HCC and to discover useful biomarkers (Table 2).
| Diagnostic | Prognostic/theragnostic |
| Distinguishing HCC from metastasis | Prognostic histomorpholic parameters-tumour grade, vessel invasion, pTNM stage |
| Distinguishing benign/preneoplastic lesions from HCC | Identification of Histological variants of prognostic importance |
| Diagnosis confirmation of small HCC | Tissue biomarkers-for prognostication |
| Diagnosis of liver nodules in non-cirrhotic background | Tissue biomarkers-for assessing presence of therapeutic targets and drug development |
| Diagnosis of atypical variants of HCC, which have atypical Imaging findings | Histologic surrogates of clinically relevant molecular signatures-for predicting prognosis |
| Combined HCC-CC | Histologic surrogates of clinically relevant molecular signatures-as predictors of potential responders for targeted therapies |
| Diagnosis confirmation of HCC in phase III trials of new drugs |
| Mandatory | Potentially necessary/helpful | Unwarranted |
| Lesion in a cirrhotic patient that lacks typical imaging characteristics | Well-differentiated HCC | HCC, if typical features are present on dynamic imaging technique |
| All nodules developing in the non-cirrhotic background | < 2 cm sized HCC, due to hypovascularity in small HCC and lack of typical imaging findings | AFP levels very high in the absence of other known causative tumours |
| Combined hepato-cholangiocarcinoma | Predictors of prognosis | Curative resection possible due to risk of needle tract seeding, if biopsied |
| Atypical variants of HCC | Teaching and biobanking | |
| Identifying stem cell phenotypes | Distinguishing HCC from regenerative nodule, dysplastic nodule, hepatic adenoma, FNH | |
| Phase III trials of novel drugs | Morphologic surrogates of molecular signatures | |
| Tissue biomarker development and studies | Surrogate biomarkers of MVI in liver biopsy |
Histopathological analysis of HCC plays very important role in the diagnosis, prognosis and management decisions. Despite the shortcomings of biopsy and advancements in imaging and molecular characterization of HCC, value of biopsy is unshaken, with several recent facets further empowering tissue analysis.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kanda T, Rodríguez-Perálvarez M, Tsoulfas G S- Editor: Wang XJ L- Editor: A E- Editor: Yin SY
| 1. | Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. Cancer J Clin. 2005;55:74-108. [DOI] [Cited in This Article: ] [Cited by in Crossref: 13286] [Cited by in F6Publishing: 13414] [Article Influence: 706.0] [Reference Citation Analysis (1)] |
| 2. | Song DS, Bae SH. Changes of guidelines diagnosing hepatocellular carcinoma during the last ten-year period. Clin Mol Hepatol. 2012;18:258-267. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Berretta M, Cavaliere C, Alessandrini L, Stanzione B, Facchini G, Balestreri L, Perin T, Canzonieri V. Serum and tissue markers in hepatocellular carcinoma and cholangiocarcinoma: clinical and prognostic implications. Oncotarget. 2017;8:14192-14220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20108] [Cited by in F6Publishing: 19772] [Article Influence: 2196.9] [Reference Citation Analysis (17)] |
| 5. | Lee Y, Park H, Lee H, Cho JY, Yoon YS, Choi YR, Han HS, Jang ES, Kim JW, Jeong SH. The Clinicopathological and Prognostic Significance of the Gross Classification of Hepatocellular Carcinoma. J Pathol Transl Med. 2018;52:85-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Agni RM. Diagnostic histopathology of hepatocellular carcinoma: A case-based review. Semin Diagn Pathol. 2017;34:126-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, Gores G. Hepatocellular carcinoma. Nat Rev Dis Primers. 2016;2:16018. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1401] [Cited by in F6Publishing: 1625] [Article Influence: 203.1] [Reference Citation Analysis (2)] |
| 8. | Brunt E, Aishima S, Clavien PA, Fowler K, Goodman Z, Gores G, Gouw A, Kagen A, Klimstra D, Komuta M. cHCC-CCA: Consensus terminology for primary liver carcinomas with both hepatocytic and cholangiocytic differentation. Hepatology. 2018;68:113-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 206] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 9. | McGlynn KA, London WT. The global epidemiology of hepatocellular carcinoma: present and future. Clin Liver Dis. 2011;15:223-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 356] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 10. | Pittman ME, Brunt EM. Anatomic pathology of hepatocellular carcinoma: histopathology using classic and new diagnostic tools. Clin Liver Dis. 2015;19:239-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118-1127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2881] [Cited by in F6Publishing: 2977] [Article Influence: 229.0] [Reference Citation Analysis (0)] |
| 12. | Ramakrishna G, Rastogi A, Trehanpati N, Sen B, Khosla R, Sarin SK. From cirrhosis to hepatocellular carcinoma: new molecular insights on inflammation and cellular senescence. Liver Cancer. 2013;2:367-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 146] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 13. | Khosla R, Rastogi A, Ramakrishna G, Pamecha V, Mukhopadhyay A, Vasudevan M, Sarin SK, Trehanpati N. EpCAM+ Liver Cancer Stem-Like Cells Exhibiting Autocrine Wnt Signaling Potentially Originate in Cirrhotic Patients. Stem Cells Transl Med. 2017;6:807-818. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Sarin SK, Thakur V, Guptan RC, Saigal S, Malhotra V, Thyagarajan SP, Das BC. Profile of hepatocellular carcinoma in India: an insight into the possible etiologic associations. J Gastroenterol Hepatol. 2001;16:666-673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Blechacz B, Mishra L. Biopsy for liver cancer: How to balance research needs with evidence-based clinical practice. Hepatology. 2015;62:1645. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-1022. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5972] [Cited by in F6Publishing: 6338] [Article Influence: 487.5] [Reference Citation Analysis (1)] |
| 17. | Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4:439-474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 732] [Cited by in F6Publishing: 813] [Article Influence: 58.1] [Reference Citation Analysis (0)] |
| 18. | European Association for Study of Liver. European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012;48:599-641. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 307] [Cited by in F6Publishing: 343] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 19. | Gonzalez SA, Keeffe EB. Diagnosis of hepatocellular carcinoma: role of tumor markers and liver biopsy. Clin Liver Dis. 2011;15:297-306, vii-vix. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Canzonieri V, Alessandrini L, Caggiari L, Perini T, Berretta M, Cannizzaro R, De Re V. Hepatocellular carcinoma: an overview of clinic-pathological and molecular perspectives. WCRJ. 2015;2:e485. [Cited in This Article: ] |
| 21. | Roberts LR, Sirlin CB, Zaiem F, Almasri J, Prokop LJ, Heimbach JK, Murad MH, Mohammed K. Imaging for the diagnosis of hepatocellular carcinoma: A systematic review and meta-analysis. Hepatology. 2018;67:401-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 244] [Cited by in F6Publishing: 283] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 22. | Gerbes A, Zoulim F, Tilg H, Dufour JF, Bruix J, Paradis V, Salem R, Peck-Radosavljevic M, Galle PR, Greten TF. Gut roundtable meeting paper: selected recent advances in hepatocellular carcinoma. Gut. 2018;67:380-388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 109] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 23. | Forner A, Vilana R, Ayuso C, Bianchi L, Solé M, Ayuso JR, Boix L, Sala M, Varela M, Llovet JM. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: Prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology. 2008;47:97-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 724] [Cited by in F6Publishing: 691] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 24. | Horigome H, Nomura T, Saso K, Itoh M, Joh T, Ohara H. Limitations of imaging diagnosis for small hepatocellular carcinoma: comparison with histological findings. J Gastroenterol Hepatol. 1999;14:559-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Peterson MS, Baron RL, Marsh JW Jr, Oliver JH 3rd, Confer SR, Hunt LE. Pretransplantation surveillance for possible hepatocellular carcinoma in patients with cirrhosis: epidemiology and CT-based tumor detection rate in 430 cases with surgical pathologic correlation. Radiology. 2000;217:743-749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 148] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 26. | Krinsky GA, Lee VS, Theise ND, Weinreb JC, Morgan GR, Diflo T, John D, Teperman LW, Goldenberg AS. Transplantation for hepatocellular carcinoma and cirrhosis: sensitivity of magnetic resonance imaging. Liver Transpl. 2002;8:1156-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 82] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 27. | Zacherl J, Pokieser P, Wrba F, Scheuba C, Prokesch R, Zacherl M, Längle F, Berlakovich GA, Mühlbacher F, Steininger R. Accuracy of multiphasic helical computed tomography and intraoperative sonography in patients undergoing orthotopic liver transplantation for hepatoma: what is the truth? Ann Surg. 2002;235:528-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Bhartia B, Ward J, Guthrie JA, Robinson PJ. Hepatocellular carcinoma in cirrhotic livers: double-contrast thin-section MR imaging with pathologic correlation of explanted tissue. AJR Am J Roentgenol. 2003;180:577-584. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 105] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 29. | Noguchi Y, Murakami T, Kim T, Hori M, Osuga K, Kawata S, Kumano S, Okada A, Sugiura T, Nakamura H. Detection of hepatocellular carcinoma: comparison of dynamic MR imaging with dynamic double arterial phase helical CT. AJR Am J Roentgenol. 2003;180:455-460. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Bialecki ES, Ezenekwe AM, Brunt EM, Collins BT, Ponder TB, Bieneman BK, Di Bisceglie AM. Comparison of liver biopsy and noninvasive methods for diagnosis of hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2006;4:361-368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 46] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 31. | Hayashi PH, Trotter JF, Forman L, Kugelmas M, Steinberg T, Russ P, Wachs M, Bak T, Kam I, Everson GT. Impact of pretransplant diagnosis of hepatocellular carcinoma on cadveric liver allocation in the era of MELD. Liver Transpl. 2004;10:42-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 77] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 32. | Schölmerich J, Schacherer D. Diagnostic biopsy for hepatocellular carcinoma in cirrhosis: useful, necessary, dangerous, or academic sport? Gut. 2004;53:1224-1226. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | Tanaka Y, Sasaki Y, Katayama K, Hiramatsu N, Ito A, Murata H, Enomoto N, Oshita M, Mochizuki K, Tsujii M. Probability of hepatocellular carcinoma of small hepatocellular nodules undetectable by computed tomography during arterial portography. Hepatology. 2000;31:890-898. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Wang AQ, Zheng YC, Du J, Zhu CP, Huang HC, Wang SS, Wu LC, Wan XS, Zhang HH, Miao RY. Combined hepatocellular cholangiocarcinoma: Controversies to be addressed. World J Gastroenterol. 2016;22:4459-4465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 37] [Cited by in F6Publishing: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 35. | Korean Liver Cancer Study Group and National Cancer Center, Korea. Practice guidelines for management of hepatocellular carcinoma 2009. Korean J Hepatol. 2009;15:391-423. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 216] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 36. | Jang HJ, Kim TK, Burns PN, Wilson SR. Enhancement patterns of hepatocellular carcinoma at contrast-enhanced US: comparison with histologic differentiation. Radiology. 2007;244:898-906. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 223] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 37. | Demirjian A, Peng P, Geschwind JF, Cosgrove D, Schutz J, Kamel IR, Pawlik TM. Infiltrating hepatocellular carcinoma: seeing the tree through the forest. J Gastrointest Surg. 2011;15:2089-2097. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 38. | Myung SJ, Yoon JH, Kim KM, Gwak GY, Kim YJ, Yu JW, Chung JW, Lee HS. Diffuse infiltrative hepatocellular carcinomas in a hepatitis B-endemic area: diagnostic and therapeutic impediments. Hepatogastroenterology. 2006;53:266-270. [PubMed] [Cited in This Article: ] |
| 39. | Farinati F, Marino D, De Giorgio M, Baldan A, Cantarini M, Cursaro C, Rapaccini G, Del Poggio P, Di Nolfo MA, Benvegnù L. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol. 2006;101:524-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 259] [Cited by in F6Publishing: 291] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 40. | Vibert E, Azoulay D, Hoti E, Iacopinelli S, Samuel D, Salloum C, Lemoine A, Bismuth H, Castaing D, Adam R. Progression of alphafetoprotein before liver transplantation for hepatocellular carcinoma in cirrhotic patients: a critical factor. Am J Transplant. 2010;10:129-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 189] [Cited by in F6Publishing: 186] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 41. | Toyoda H, Kumada T, Tada T, Sone Y, Kaneoka Y, Maeda A. Tumor Markers for Hepatocellular Carcinoma: Simple and Significant Predictors of Outcome in Patients with HCC. Liver Cancer. 2015;4:126-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 42. | Cresswell AB, Welsh FK, Rees M. A diagnostic paradigm for resectable liver lesions: to biopsy or not to biopsy? HPB (Oxford). 2009;11:533-540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Gilmore IT, Burroughs A, Murray-Lyon IM, Williams R, Jenkins D, Hopkins A. Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: an audit by the British Society of Gastroenterology and the Royal College of Physicians of London. Gut. 1995;36:437-441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 278] [Cited by in F6Publishing: 265] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 44. | Perrault J, McGill DB, Ott BJ, Taylor WF. Liver biopsy: complications in 1000 inpatients and outpatients. Gastroenterology. 1978;74:103-106. [PubMed] [Cited in This Article: ] |
| 45. | Knauer CM. Percutaneous biopsy of the liver as a procedure for outpatients. Gastroenterology. 1978;74:101-102. [PubMed] [Cited in This Article: ] |
| 46. | Kleiner DE. Hepatocellular carcinoma: Liver biopsy in the balance. Hepatology. 2018;68:13-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD; American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 2009;49:1017-1044. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1449] [Cited by in F6Publishing: 1419] [Article Influence: 94.6] [Reference Citation Analysis (0)] |
| 48. | McGill DB, Rakela J, Zinsmeister AR, Ott BJ. A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology. 1990;99:1396-1400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 468] [Cited by in F6Publishing: 486] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 49. | Kalambokis G, Manousou P, Vibhakorn S, Marelli L, Cholongitas E, Senzolo M, Patch D, Burroughs AK. Transjugular liver biopsy--indications, adequacy, quality of specimens, and complications--a systematic review. J Hepatol. 2007;47:284-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 280] [Cited by in F6Publishing: 290] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 50. | Giorgio A, Tarantino L, de Stefano G, Francica G, Esposito F, Perrotta A, Aloisio V, Farella N, Mariniello N, Coppola C. Complications after interventional sonography of focal liver lesions: a 22-year single-center experience. J Ultrasound Med. 2003;22:193-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 51. | Durand F, Regimbeau JM, Belghiti J, Sauvanet A, Vilgrain V, Terris B, Moutardier V, Farges O, Valla D. Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol. 2001;35:254-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 180] [Cited by in F6Publishing: 161] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 52. | Kim SH, Lim HK, Lee WJ, Cho JM, Jang HJ. Needle-tract implantation in hepatocellular carcinoma: frequency and CT findings after biopsy with a 19.5-gauge automated biopsy gun. Abdom Imaging. 2000;25:246-250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 110] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 53. | Kosugi C, Furuse J, Ishii H, Maru Y, Yoshino M, Kinoshita T, Konishi M, Nakagohri T, Inoue K, Oda T. Needle tract implantation of hepatocellular carcinoma and pancreatic carcinoma after ultrasound-guided percutaneous puncture: clinical and pathologic characteristics and the treatment of needle tract implantation. World J Surg. 2004;28:29-32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 54. | Liu YW, Chen CL, Chen YS, Wang CC, Wang SH, Lin CC. Needle tract implantation of hepatocellular carcinoma after fine needle biopsy. Dig Dis Sci. 2007;52:228-231. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 55. | Takamori R, Wong LL, Dang C, Wong L. Needle-tract implantation from hepatocellular cancer: is needle biopsy of the liver always necessary? Liver Transpl. 2000;6:67-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 60] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 56. | Chang S, Kim SH, Lim HK, Lee WJ, Choi D, Lim JH. Needle tract implantation after sonographically guided percutaneous biopsy of hepatocellular carcinoma: evaluation of doubling time, frequency, and features on CT. AJR Am J Roentgenol. 2005;185:400-405. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 57. | Silva MA, Hegab B, Hyde C, Guo B, Buckels JA, Mirza DF. Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis. Gut. 2008;57:1592-1596. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 343] [Cited by in F6Publishing: 342] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 58. | Torzilli G, Minagawa M, Takayama T, Inoue K, Hui AM, Kubota K, Ohtomo K, Makuuchi M. Accurate preoperative evaluation of liver mass lesions without fine-needle biopsy. Hepatology. 1999;30:889-893. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 249] [Cited by in F6Publishing: 255] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 59. | Roncalli M, Sciarra A, Tommaso LD. Benign hepatocellular nodules of healthy liver: focal nodular hyperplasia and hepatocellular adenoma. Clin Mol Hepatol. 2016;22:199-211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 60. | Nguyen TB, Roncalli M, Di Tommaso L, Kakar S. Combined use of heat-shock protein 70 and glutamine synthetase is useful in the distinction of typical hepatocellular adenoma from atypical hepatocellular neoplasms and well-differentiated hepatocellular carcinoma. Mod Pathol. 2016;29:283-292. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 61. | Lagana SM, Salomao M, Bao F, Moreira RK, Lefkowitch JH, Remotti HE. Utility of an immunohistochemical panel consisting of glypican-3, heat-shock protein-70, and glutamine synthetase in the distinction of low-grade hepatocellular carcinoma from hepatocellular adenoma. Appl Immunohistochem Mol Morphol. 2013;21:170-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 62. | Daneo V, Robecchi A Jr, Secondo G. [Monoarthritis of the knee, sacroileitis and ulcero-hemorrhagic colitis. Chronicity of the arthropathy and appearance of the rheumatoid factor in serum]. Reumatismo. 1967;19:340-345. [PubMed] [Cited in This Article: ] |
| 63. | Durand F, Belghiti J, Paradis V. Liver transplantation for hepatocellular carcinoma: role of biopsy. Liver Transpl. 2007;13:S17-S23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 64. | Kelley RK, Yao F. Salvage liver transplantation for recurrent hepatocellular carcinoma after radiofrequency ablation: a new strategy? J Hepatol. 2012;56:14-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 65. | N’Kontchou G, Aout M, Laurent A, Nahon P, Ganne-Carrié N, Grando V, Baghad I, Roulot D, Trinchet JC, Sellier N. Survival after radiofrequency ablation and salvage transplantation in patients with hepatocellular carcinoma and Child-Pugh A cirrhosis. J Hepatol. 2012;56:160-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 66. | Sala M, Fuster J, Llovet JM, Navasa M, Solé M, Varela M, Pons F, Rimola A, García-Valdecasas JC, Brú C, Bruix J; Barcelona Clinic Liver Cancer (BCLC) Group. High pathological risk of recurrence after surgical resection for hepatocellular carcinoma: an indication for salvage liver transplantation. Liver Transpl. 2004;10:1294-1300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 233] [Cited by in F6Publishing: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 67. | Scatton O, Zalinski S, Terris B, Lefevre JH, Casali A, Massault PP, Conti F, Calmus Y, Soubrane O. Hepatocellular carcinoma developed on compensated cirrhosis: resection as a selection tool for liver transplantation. Liver Transpl. 2008;14:779-788. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 68. | Qin LX, Tang ZY. The prognostic molecular markers in hepatocellular carcinoma. World J Gastroenterol. 2002;8:385-392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 226] [Cited by in F6Publishing: 230] [Article Influence: 10.5] [Reference Citation Analysis (1)] |
| 69. | Choi GH, Han DH, Kim DH, Choi SB, Kang CM, Kim KS, Choi JS, Park YN, Park JY, Kim DY. Outcome after curative resection for a huge hepatocellular carcinoma and prognostic significance of gross tumor classification. Am J Surg. 2009;198:693-701. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 70. | Shimada M, Rikimaru T, Hamatsu T, Yamashita Y, Terashi T, Taguchi K, Tanaka S, Shirabe K, Sugimachi K. The role of macroscopic classification in nodular-type hepatocellular carcinoma. Am J Surg. 2001;182:177-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 71. | Fu X, Mao L, Tang M, Yan X, Qiu Y, He J, Zhou T. Gross classification of solitary small hepatocellular carcinoma on preoperative computed tomography: Prognostic significance after radiofrequency ablation. Hepatol Res. 2016;46:298-305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 72. | Martins-Filho SN, Paiva C, Azevedo RS, Alves VAF. Histological Grading of Hepatocellular Carcinoma-A Systematic Review of Literature. Front Med (Lausanne). 2017;4:193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 91] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 73. | Mounajjed T, Chandan VS, Torbenson MS, SpringerLink (Online service). Surgical Pathology of Liver Tumors. . [Cited in This Article: ] |
| 74. | Ziol M, Poté N, Amaddeo G, Laurent A, Nault JC, Oberti F, Costentin C, Michalak S, Bouattour M, Francoz C. Macrotrabecular-massive hepatocellular carcinoma: A distinctive histological subtype with clinical relevance. Hepatology. 2018;68:103-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 141] [Article Influence: 23.5] [Reference Citation Analysis (1)] |
| 75. | Torbenson MS. Morphologic Subtypes of Hepatocellular Carcinoma. Gastroenterol Clin North Am. 2017;46:365-391. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 77] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 76. | Craig JR, Peters RL, Edmondson HA, Omata M. Fibrolamellar carcinoma of the liver: a tumor of adolescents and young adults with distinctive clinico-pathologic features. Cancer. 1980;46:372-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 77. | Klein WM, Molmenti EP, Colombani PM, Grover DS, Schwarz KB, Boitnott J, Torbenson MS. Primary liver carcinoma arising in people younger than 30 years. Am J Clin Pathol. 2005;124:512-518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 78. | Goldie AS, Fearon KC, Ross JA, Barclay GR, Jackson RE, Grant IS, Ramsay G, Blyth AS, Howie JC. Natural cytokine antagonists and endogenous antiendotoxin core antibodies in sepsis syndrome. The Sepsis Intervention Group. JAMA. 1995;274:172-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 162] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 79. | Salomao M, Yu WM, Brown RS Jr, Emond JC, Lefkowitch JH. Steatohepatitic hepatocellular carcinoma (SH-HCC): a distinctive histological variant of HCC in hepatitis C virus-related cirrhosis with associated NAFLD/NASH. Am J Surg Pathol. 2010;34:1630-1636. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 144] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 80. | Kim H, Choi GH, Na DC, Ahn EY, Kim GI, Lee JE, Cho JY, Yoo JE, Choi JS, Park YN. Human hepatocellular carcinomas with “Stemness”-related marker expression: keratin 19 expression and a poor prognosis. Hepatology. 2011;54:1707-1717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 249] [Cited by in F6Publishing: 251] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 81. | Fatourou E, Koskinas J, Karandrea D, Palaiologou M, Syminelaki T, Karanikolas M, Felekouras E, Antoniou E, Manesis EK, Delladetsima J. Keratin 19 protein expression is an independent predictor of survival in human hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2015;27:1094-1102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 82. | Li T, Fan J, Qin LX, Zhou J, Sun HC, Qiu SJ, Ye QH, Wang L, Tang ZY. Risk factors, prognosis, and management of early and late intrahepatic recurrence after resection of primary clear cell carcinoma of the liver. Ann Surg Oncol. 2011;18:1955-1963. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 83. | Xu W, Ge P, Liao W, Ren J, Yang H, Xu H, Sang X, Lu X, Zhong S, Mao Y. Edmondson grade predicts survival of patients with primary clear cell carcinoma of liver after curative resection: A retrospective study with long-term follow-up. Asia Pac J Clin Oncol. 2017;13:e312-e320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 84. | Tan PS, Nakagawa S, Goossens N, Venkatesh A, Huang T, Ward SC, Sun X, Song WM, Koh A, Canasto-Chibuque C. Clinicopathological indices to predict hepatocellular carcinoma molecular classification. Liver Int. 2016;36:108-118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 85. | Calderaro J, Couchy G, Imbeaud S, Amaddeo G, Letouzé E, Blanc JF, Laurent C, Hajji Y, Azoulay D, Bioulac-Sage P. Histological subtypes of hepatocellular carcinoma are related to gene mutations and molecular tumour classification. J Hepatol. 2017;67:727-738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 373] [Cited by in F6Publishing: 436] [Article Influence: 62.3] [Reference Citation Analysis (0)] |
| 86. | Lauwers GY, Terris B, Balis UJ, Batts KP, Regimbeau JM, Chang Y, Graeme-Cook F, Yamabe H, Ikai I, Cleary KR. Prognostic histologic indicators of curatively resected hepatocellular carcinomas: a multi-institutional analysis of 425 patients with definition of a histologic prognostic index. Am J Surg Pathol. 2002;26:25-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 152] [Cited by in F6Publishing: 155] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 87. | Kassahun WT, Hauss J. Management of combined hepatocellular and cholangiocarcinoma. Int J Clin Pract. 2008;62:1271-1278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 112] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 88. | Koh KC, Lee H, Choi MS, Lee JH, Paik SW, Yoo BC, Rhee JC, Cho JW, Park CK, Kim HJ. Clinicopathologic features and prognosis of combined hepatocellular cholangiocarcinoma. Am J Surg. 2005;189:120-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 143] [Cited by in F6Publishing: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 89. | Goodman ZD, Ishak KG, Langloss JM, Sesterhenn IA, Rabin L. Combined hepatocellular-cholangiocarcinoma. A histologic and immunohistochemical study. Cancer. 1985;55:124-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 9] [Reference Citation Analysis (0)] |
| 90. | Lin G, Toh CH, Wu RC, Ko SF, Ng SH, Chou WC, Tseng JH. Combined hepatocellular cholangiocarcinoma: prognostic factors investigated by computed tomography/magnetic resonance imaging. Int J Clin Pract. 2008;62:1199-1205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 91. | ALLEN RA, LISA JR. Combined liver cell and bile duct carcinoma. Am J Pathol. 1949;25:647-655. [PubMed] [Cited in This Article: ] |
| 92. | Theise ND, Park YN, Nakanuma Y. Combined hepatocellular cholangiocarcinoma. WHO Classification of Tumours of the Digestive System, 4th ed. IARC Press. 2010;225-227. [Cited in This Article: ] |
| 93. | Sasaki M, Sato H, Kakuda Y, Sato Y, Choi JH, Nakanuma Y. Clinicopathological significance of ‘subtypes with stem-cell feature’ in combined hepatocellular-cholangiocarcinoma. Liver Int. 2015;35:1024-1035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 94. | Zhou L, Rui JA, Wang SB, Chen SG, Qu Q, Chi TY, Wei X, Han K, Zhang N, Zhao HT. Outcomes and prognostic factors of cirrhotic patients with hepatocellular carcinoma after radical major hepatectomy. World J Surg. 2007;31:1782-1787. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 95. | Moeini A, Sia D, Zhang Z, Camprecios G, Stueck A, Dong H, Montal R, Torrens L, Martinez-Quetglas I, Fiel MI. Mixed hepatocellular cholangiocarcinoma tumors: Cholangiolocellular carcinoma is a distinct molecular entity. J Hepatol. 2017;66:952-961. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 96. | Ma YC, Yang JY, Yan LN. Relevant markers of cancer stem cells indicate a poor prognosis in hepatocellular carcinoma patients: a meta-analysis. Eur J Gastroenterol Hepatol. 2013;25:1007-1016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 97. | Govaere O, Roskams T. Pathogenesis and prognosis of hepatocellular carcinoma at the cellular and molecular levels. Clin Liver Dis. 2015;19:261-276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 98. | Bruix J, Gores GJ, Mazzaferro V. Hepatocellular carcinoma: clinical frontiers and perspectives. Gut. 2014;63:844-855. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 929] [Cited by in F6Publishing: 1055] [Article Influence: 105.5] [Reference Citation Analysis (1)] |
| 99. | Sherman M. Hepatocellular carcinoma: epidemiology, surveillance, and diagnosis. Semin Liver Dis. 2010;30:3-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 836] [Cited by in F6Publishing: 667] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 100. | International Working Party. Terminology of nodular hepatocellular lesions. Hepatology. 1995;22:983-993. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 284] [Cited by in F6Publishing: 287] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 101. | International Consensus Group for Hepatocellular Neoplasia. Pathologic diagnosis of early hepatocellular carcinoma: a report of the international consensus group for hepatocellular neoplasia. Hepatology. 2009;49:658-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 610] [Cited by in F6Publishing: 554] [Article Influence: 36.9] [Reference Citation Analysis (1)] |
| 102. | Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, Tateishi R, Han KH, Chawla YK, Shiina S. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11:317-370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 986] [Cited by in F6Publishing: 1335] [Article Influence: 190.7] [Reference Citation Analysis (0)] |
| 103. | Lo RC, Ng IO. Hepatocellular tumors: immunohistochemical analyses for classification and prognostication. Chin J Cancer Res. 2011;23:245-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 104. | Di Tommaso L, Destro A, Seok JY, Balladore E, Terracciano L, Sangiovanni A, Iavarone M, Colombo M, Jang JJ, Yu E. The application of markers (HSP70 GPC3 and GS) in liver biopsies is useful for detection of hepatocellular carcinoma. J Hepatol. 2009;50:746-754. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 229] [Cited by in F6Publishing: 203] [Article Influence: 13.5] [Reference Citation Analysis (3)] |
| 105. | Yamauchi N, Watanabe A, Hishinuma M, Ohashi K, Midorikawa Y, Morishita Y, Niki T, Shibahara J, Mori M, Makuuchi M. The glypican 3 oncofetal protein is a promising diagnostic marker for hepatocellular carcinoma. Mod Pathol. 2005;18:1591-1598. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 246] [Cited by in F6Publishing: 239] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 106. | Di Tommaso L, Roncalli M. Tissue Biomarkers in Hepatocellular Tumors: Which, When, and How. Front Med (Lausanne). 2017;4:10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 107. | European Association For The Study Of The Liver. European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908-943. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4059] [Cited by in F6Publishing: 4338] [Article Influence: 361.5] [Reference Citation Analysis (2)] |
| 108. | Tamura S, Kato T, Berho M, Misiakos EP, O’Brien C, Reddy KR, Nery JR, Burke GW, Schiff ER, Miller J. Impact of histological grade of hepatocellular carcinoma on the outcome of liver transplantation. Arch Surg. 2001;136:25-30; discussion 31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 193] [Cited by in F6Publishing: 196] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 109. | EDMONDSON HA, STEINER PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954;7:462-503. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 24] [Reference Citation Analysis (0)] |
| 110. | Bosman FT, World Health Organization. International Agency for Research on Cancer. WHO classification of tumours of the digestive system. 4th ed. International Agency for Research on Cancer. 2010;417. [Cited in This Article: ] |
| 111. | Alastair Burt, Linda Ferrell, Stefan Hubscher. MacSween’s pathology of the liver. In 7th ed. Churchill Livingstone. 2017;. [Cited in This Article: ] |
| 112. | Amin MB, Edge SB, Greene FL. AJCC Cancer Staging Manual. 8th ed. New York, Springer. 2017;. [DOI] [Cited in This Article: ] |
| 113. | Qin LX, Tang ZY. The prognostic significance of clinical and pathological features in hepatocellular carcinoma. World J Gastroenterol. 2002;8:193-199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 129] [Cited by in F6Publishing: 123] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 114. | Zhang X, Li J, Shen F, Lau WY. Significance of presence of microvascular invasion in specimens obtained after surgical treatment of hepatocellular carcinoma. J Gastroenterol Hepatol. 2018;33:347-354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 154] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 115. | Pawlik TM, Delman KA, Vauthey JN, Nagorney DM, Ng IO, Ikai I, Yamaoka Y, Belghiti J, Lauwers GY, Poon RT. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 2005;11:1086-1092. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 463] [Cited by in F6Publishing: 487] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 116. | Du M, Chen L, Zhao J, Tian F, Zeng H, Tan Y, Sun H, Zhou J, Ji Y. Microvascular invasion (MVI) is a poorer prognostic predictor for small hepatocellular carcinoma. BMC Cancer. 2014;14:38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 117. | Yamashita Y, Tsuijita E, Takeishi K, Fujiwara M, Kira S, Mori M, Aishima S, Taketomi A, Shirabe K, Ishida T. Predictors for microinvasion of small hepatocellular carcinoma ≤ 2 cm. Ann Surg Oncol. 2012;19:2027-2034. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 118. | Rodríguez-Perálvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20:325-339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 352] [Cited by in F6Publishing: 386] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 119. | Shindoh J, Andreou A, Aloia TA, Zimmitti G, Lauwers GY, Laurent A, Nagorney DM, Belghiti J, Cherqui D, Poon RT. Microvascular invasion does not predict long-term survival in hepatocellular carcinoma up to 2 cm: reappraisal of the staging system for solitary tumors. Ann Surg Oncol. 2013;20:1223-1229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 120. | Feng LH, Dong H, Lau WY, Yu H, Zhu YY, Zhao Y, Lin YX, Chen J, Wu MC, Cong WM. Novel microvascular invasion-based prognostic nomograms to predict survival outcomes in patients after R0 resection for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2017;143:293-303. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 121. | Cong WM, Bu H, Chen J, Dong H, Zhu YY, Feng LH, Chen J; Guideline Committee. Practice guidelines for the pathological diagnosis of primary liver cancer: 2015 update. World J Gastroenterol. 2016;22:9279-9287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 185] [Cited by in F6Publishing: 232] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 122. | Gouw AS, Balabaud C, Kusano H, Todo S, Ichida T, Kojiro M. Markers for microvascular invasion in hepatocellular carcinoma: where do we stand? Liver Transpl. 2011;17 Suppl 2:S72-S80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 123. | Poté N, Cauchy F, Albuquerque M, Cros J, Soubrane O, Bedossa P, Paradis V. Contribution of virtual biopsy to the screening of microvascular invasion in hepatocellular carcinoma: A pilot study. Liver Int. 2018;38:687-694. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 124. | Donat M, Alonso S, Pereira F, Ferrero E, Carrión L, Acin-Gándara D, Moreno E. Impact of Histological Factors of Hepatocellular Carcinoma on the Outcome of Liver Transplantation. Transplant Proc. 2016;48:1968-1977. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 125. | Li WX, Li Z, Gao PJ, Gao J, Zhu JY. Histological differentiation predicts post-liver transplantation survival time. Clin Res Hepatol Gastroenterol. 2014;38:201-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 126. | Yip VS, Gomez D, Tan CY, Staettner S, Terlizzo M, Fenwick S, Malik HZ, Ghaneh P, Poston G. Tumour size and differentiation predict survival after liver resection for hepatocellular carcinoma arising from non-cirrhotic and non-fibrotic liver: a case-controlled study. Int J Surg. 2013;11:1078-1082. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 127. | El-Fattah MA. Hepatocellular carcinoma biology predicts survival outcome after liver transplantation in the USA. Indian J Gastroenterol. 2017;36:117-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 128. | Zhou L, Rui JA, Wang SB, Chen SG, Qu Q. Early recurrence in large hepatocellular carcinoma after curative hepatic resection: prognostic significance and risk factors. Hepatogastroenterology. 2014;61:2035-2041. [PubMed] [Cited in This Article: ] |
| 129. | DuBay D, Sandroussi C, Sandhu L, Cleary S, Guba M, Cattral MS, McGilvray I, Ghanekar A, Selzner M, Greig PD. Liver transplantation for advanced hepatocellular carcinoma using poor tumor differentiation on biopsy as an exclusion criterion. Ann Surg. 2011;253:166-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 210] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 130. | Cillo U, Vitale A, Bassanello M, Boccagni P, Brolese A, Zanus G, Burra P, Fagiuoli S, Farinati F, Rugge M. Liver transplantation for the treatment of moderately or well-differentiated hepatocellular carcinoma. Ann Surg. 2004;239:150-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 253] [Cited by in F6Publishing: 272] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 131. | Lee JS, Heo J, Libbrecht L, Chu IS, Kaposi-Novak P, Calvisi DF, Mikaelyan A, Roberts LR, Demetris AJ, Sun Z. A novel prognostic subtype of human hepatocellular carcinoma derived from hepatic progenitor cells. Nat Med. 2006;12:410-416. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 729] [Cited by in F6Publishing: 719] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 132. | Tsujikawa H, Masugi Y, Yamazaki K, Itano O, Kitagawa Y, Sakamoto M. Immunohistochemical molecular analysis indicates hepatocellular carcinoma subgroups that reflect tumor aggressiveness. Hum Pathol. 2016;50:24-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 133. | Kim H, Park YN. Hepatocellular carcinomas expressing ‘stemness’-related markers: clinicopathological characteristics. Dig Dis. 2014;32:778-785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 134. | Chan AW, Tong JH, Chan SL, Lai PB, To KF. Expression of stemness markers (CD133 and EpCAM) in prognostication of hepatocellular carcinoma. Histopathology. 2014;64:935-950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 135. | Guo Z, Li LQ, Jiang JH, Ou C, Zeng LX, Xiang BD. Cancer stem cell markers correlate with early recurrence and survival in hepatocellular carcinoma. World J Gastroenterol. 2014;20:2098-2106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 66] [Cited by in F6Publishing: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 136. | Srivastava S, Wong KF, Ong CW, Huak CY, Yeoh KG, Teh M, Luk JM, Salto-Tellez M. A morpho-molecular prognostic model for hepatocellular carcinoma. Br J Cancer. 2012;107:334-339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 137. | Li Y, Ma X, Zhang J, Liu X, Liu L. Prognostic value of microvessel density in hepatocellular carcinoma patients: a meta-analysis. Int J Biol Markers. 2014;29:e279-e287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 138. | Zucman-Rossi J, Villanueva A, Nault JC, Llovet JM. Genetic Landscape and Biomarkers of Hepatocellular Carcinoma. Gastroenterology. 2015;149:1226-1239.e4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 744] [Cited by in F6Publishing: 829] [Article Influence: 92.1] [Reference Citation Analysis (0)] |
| 139. | Mekuria AN, Abdi AD. Potential Molecular Targets and Drugs for Treatment of Hepatocellular Carcinoma. J Cancer Sci Ther. 2017;9:12. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 140. | Rimassa L, Abbadessa G, Personeni N, Porta C, Borbath I, Daniele B, Salvagni S, Van Laethem JL, Van Vlierberghe H, Trojan J. Tumor and circulating biomarkers in patients with second-line hepatocellular carcinoma from the randomized phase II study with tivantinib. Oncotarget. 2016;7:72622-72633. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 141. | Rimassa L, Assenat E, Peck-Radosavljevic M, Pracht M, Zagonel V, Mathurin P, Rota Caremoli E, Porta C, Daniele B, Bolondi L. Tivantinib for second-line treatment of MET-high, advanced hepatocellular carcinoma (METIV-HCC): a final analysis of a phase 3, randomised, placebo-controlled study. Lancet Oncol. 2018;19:682-693. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 226] [Cited by in F6Publishing: 269] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 142. | Sia D, Jiao Y, Martinez-Quetglas I, Kuchuk O, Villacorta-Martin C, Castro de Moura M, Putra J, Camprecios G, Bassaganyas L, Akers N. Identification of an Immune-specific Class of Hepatocellular Carcinoma, Based on Molecular Features. Gastroenterology. 2017;153:812-826. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 475] [Cited by in F6Publishing: 572] [Article Influence: 81.7] [Reference Citation Analysis (0)] |
| 143. | Sideras K, Biermann K, Verheij J, Takkenberg BR, Mancham S, Hansen BE, Schutz HM, de Man RA, Sprengers D, Buschow SI. PD-L1, Galectin-9 and CD8+ tumor-infiltrating lymphocytes are associated with survival in hepatocellular carcinoma. Oncoimmunology. 2017;6:e1273309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 144. | Kudo M. Immune Checkpoint Blockade in Hepatocellular Carcinoma: 2017 Update. Liver Cancer. 2016;6:1-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 145. | Chang H, Jung W, Kim A, Kim HK, Kim WB, Kim JH, Kim BH. Expression and prognostic significance of programmed death protein 1 and programmed death ligand-1, and cytotoxic T lymphocyte-associated molecule-4 in hepatocellular carcinoma. APMIS. 2017;125:690-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 146. | Calderaro J, Rousseau B, Amaddeo G, Mercey M, Charpy C, Costentin C, Luciani A, Zafrani ES, Laurent A, Azoulay D. Programmed death ligand 1 expression in hepatocellular carcinoma: Relationship With clinical and pathological features. Hepatology. 2016;64:2038-2046. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 260] [Cited by in F6Publishing: 302] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 147. | Duffy AG, Ulahannan SV, Makorova-Rusher O, Rahma O, Wedemeyer H, Pratt D, Davis JL, Hughes MS, Heller T, ElGindi M. Tremelimumab in combination with ablation in patients with advanced hepatocellular carcinoma. J Hepatol. 2017;66:545-551. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 454] [Cited by in F6Publishing: 557] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 148. | Hoshida Y, Nijman SM, Kobayashi M, Chan JA, Brunet JP, Chiang DY, Villanueva A, Newell P, Ikeda K, Hashimoto M. Integrative transcriptome analysis reveals common molecular subclasses of human hepatocellular carcinoma. Cancer Res. 2009;69:7385-7392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 753] [Cited by in F6Publishing: 851] [Article Influence: 56.7] [Reference Citation Analysis (0)] |