Published online Nov 14, 2017. doi: 10.3748/wjg.v23.i42.7618
Peer-review started: July 5, 2017
First decision: August 30, 2017
Revised: September 12, 2017
Accepted: September 26, 2017
Article in press: September 26, 2017
Published online: November 14, 2017
To explore the differences in the responses of left-sided colorectal cancer (LSCRC) and right-sided colon cancer (RSCC) to traditional Chinese medicine (TCM).
Patients with postoperative stage I-III colorectal cancer (CRC) were enrolled and divided into the LSCRC with or without TCM and RSCC with or without TCM groups depending on the primary tumor side and TCM administration. Patients in the TCM group were given TCM for at least 6 mo. Our research adopted disease-free survival (DFS) as the primary endpoint. We applied a Cox proportional hazards regression model for the multivariate factor analysis using Stata 12.0 and SPSS 22.0 software for data analysis.
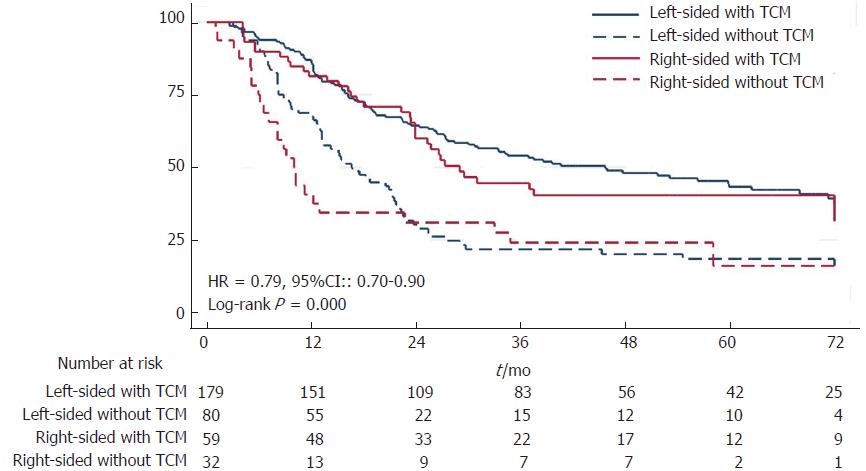
Of the 817 patients included in our study, 617 had LSCRC (TCM group, n = 404; Non-TCM group, n = 213), and 200 had RSCC (TCM group, n = 132; Non-TCM group, n = 68). The 6-year DFS for patients with LSCRC was 56.95% in the TCM group and 41.50% in the Non-TCM group (P = 0.000). For patients with RSCC, the 6-year DFS was 52.92% in the TCM group and 37.19% in the Non-TCM group (P = 0.003). Differences between LSCRC and RSCC were not statistically significant regardless of TCM ingestion.
Patients with either LSCRC or RSCC and who took TCM experienced longer DFS; furthermore, patients with RSCC benefited more from TCM in DFS.
Core tip: In this prospective, observational, multicenter, cohort study, we compared disease-free survival (DFS) of patients with postoperative stage I-III left- and right-sided colorectal cancers who were stratified by ingestion of TCM. The data analysis confirmed that TCM effectively prolonged DFS of patients with stage II-III on both sides, especially individuals with stage III right-sided colon cancer.
- Citation: Liu SS, Shi Q, Li HJ, Yang W, Han SS, Zong SQ, Li W, Hou FG. Right- and left-sided colorectal cancers respond differently to traditional Chinese medicine. World J Gastroenterol 2017; 23(42): 7618-7625
- URL: https://www.wjgnet.com/1007-9327/full/v23/i42/7618.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i42.7618
Colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related death in America[1,2]. Resection is the gold-standard treatment for CRC, but 35% of individuals will develop recurrence or metastasis within the first few years after resection[3]. Therefore, preventing postoperative recurrence and metastasis is critical in treating stage I-III CRC. In China, traditional Chinese medicine (TCM) is a common anticancer approach along with chemotherapy and radiotherapy[4,5]. Our preliminary study also proved that chemotherapy coupled with TCM could further reduce the risk of recurrence and metastasis as well as prolong the disease-free survival (DFS) of patients with CRC[6]. Recently, more studies have proposed that location of primary tumor was related to recurrence, metastasis and the therapeutic effect[7-9]. However, there was no evidence regarding whether TCM exerts variable effects on CRC based on the side where the lesion is located. Therefore, we undertook this study to determine whether TCM can prolong the DFS of individuals with either left-sided colorectal cancer (LSCRC) or right-sided colon cancer (RSCC).
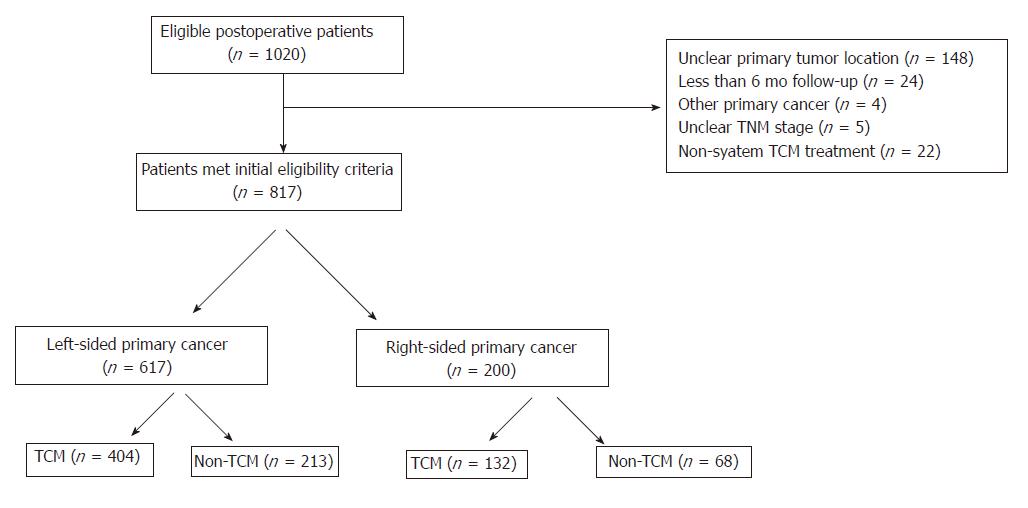
This was a retrospective, observational, multicenter, cohort study designed to elucidate whether primary tumor location is associated with a differential response to TCM. Eligible postoperative patients with stage I-III disease were screened at affiliated hospitals of Shanghai University of Traditional Chinese Medicine (Shanghai Municipal Hospital of Traditional Chinese Medicine, Shuguang Hospital and Yueyang Hospital) between April 2004 and November 2013. The study protocol was approved by these three individual ethics committees. A total 1020 patients were screened, among which 148 did not present a clear side of colon cancer, 4 presented other primary tumors, 24 were followed up for less than 6 mo, 5 presented an unclear TNM stage, and 22 were treated with non-systemic TCM medication. Notably, systematic TCM medication was defined as at least 6 mo of continuous TCM ingestion before relapse. Finally, 817 patients were included in our research (Figure 1) and divided into the following groups based on tumor location and TCM status: LSCRC with TCM, LSCRC without TCM, RSCC with TCM and RSCC without TCM. All the included patients were followed up by outpatient visits, returning visits or telephone follow-up every 6 mo; clinical data, including age, gender, colon cancer location, surgical pathology, histodifferentiation, TNM stage, lymph nodes examined in surgical specimen, chemotherapy, radiotherapy, comorbidities (including hypertension, diabetes, heart disease, and stroke), period of TCM, time to recurrence and metastasis or cancer-related death, were collected at each follow-up visit. The median follow-up for RSCC was 53.0 mo in the TCM group and 34.3 mo in the Non-TCM group; for LSCRC, the median follow-up was 54.3 mo in the TCM group and 38.5 mo in the Non-TCM group. Follow-up was completed for up to 6 years or until the patients either relapsed or died.
DFS, which is defined as the time from surgical resection to relapse, cancer-related death or the last follow-up (whichever occurred first), was evaluated using Kaplan-Meier curves and log-rank tests. Baseline characteristics were analyzed using Pearson’s χ2 test. Propensity score matching was created using logistic regression to model the probability that a patient exhibited a specific characteristic based on gender, age, location, histodifferentiation, TNM stage, lymph node status, chemotherapy, radiotherapy and comorbidities; this matching was conducted to test the stability of our research. A 1:1 match with a random matching order and 0.1 caliper was performed between the TCM and Non-TCM groups in LSCRC and RSCC, respectively, and a 2:1 match was conducted between LSCRC and RSCC within the TCM and Non-TCM groups, respectively; additionally, replacements were not allowed. In addition, we applied multivariate regression analyses for multicollinearity diagnosis and Cox proportional hazards regression model for multivariate factor analysis. Hypothesis testing was conducted using a two-sided alpha set to a 5% level of significance. All analyses were performed using Stata 12.0 and SPSS 22.0 software. The statistical methods used in this study were reviewed by Weibing Wang from the Department of Epidemiology, School of Public Health, Fudan University.
TCM prescriptions were determined by attending physicians on the basis of syndrome differentiation, and their composition, dose were modified every two weeks to tailor them to the distinctive symptom complex. The herbs were processed as a decoction for administration twice per day (200 mL per session). Notably, TCM treatment must have been continually managed for at least six months before relapse for inclusion in the TCM group and was ceased at the patient’s request, by the physician or in an instance of relapse.
The primary tumor side was identified using postoperative pathology. LSCRC was defined as a primary tumor located between the splenic flexure and the rectosigmoid junction, whereas RSCC was defined as a primary site originating between the cecum and the proximal two-thirds of the transverse colon[10].
Among the 817 patients, 617 had LSCRC (TCM group, n = 404; Non-TCM group, n = 213), and 200 had RSCC (TCM group, n = 132; Non-TCM group, n = 68). Subjects with LSCRC were more likely to be male than those with RSCC. Patients were commonly older than 60 years old and were less likely to have a stroke. Most patients have received chemotherapy but very few have undergone radiotherapy. Other characteristics such as histodifferentiation, TNM stage, lymph node status, diabetes, hypertension, and heart disease were evenly distributed among the groups and showed no statistically significant differences. The baseline characteristics after propensity score matching were shown in Supplementary Tables 1 and 2.
| Left-sided | Right-sided | ||||
| TCM ,n = 404 | Non-TCM ,n = 213 | TCM,n = 132 | Non-TCM,n = 68 | P value | |
| Gender | 0.035a | ||||
| Man | 207 | 126 | 63 | 28 | |
| Woman | 197 | 87 | 69 | 40 | |
| Age (yr) | 0.027a | ||||
| < 60 | 163 | 70 | 41 | 17 | |
| ≥ 60 | 241 | 143 | 91 | 51 | |
| Histodifferentiatio, n | 0.293 | ||||
| Poorly | 47 | 19 | 18 | 8 | |
| Moderately | 252 | 123 | 80 | 34 | |
| Well | 9 | 7 | 6 | 2 | |
| Unknown | 96 | 64 | 28 | 24 | |
| Lympho node metastasis | 0.125 | ||||
| Yes | 176 | 74 | 57 | 32 | |
| No | 228 | 139 | 75 | 36 | |
| TNM stage | 0.331 | ||||
| I | 77 | 38 | 19 | 8 | |
| II | 148 | 95 | 54 | 28 | |
| III | 179 | 80 | 59 | 32 | |
| Chemotherapy | 0.000a | ||||
| Yes | 332 | 149 | 97 | 44 | |
| No | 72 | 64 | 35 | 24 | |
| Radiotherapy | 0.011a | ||||
| Yes | 44 | 19 | 5 | 1 | |
| No | 360 | 194 | 127 | 67 | |
| Diabetes | 0.995 | ||||
| Yes | 61 | 33 | 21 | 10 | |
| No | 343 | 180 | 111 | 58 | |
| Hypertension | 0.872 | ||||
| Yes | 131 | 76 | 44 | 22 | |
| No | 273 | 137 | 88 | 46 | |
| Heart disease | 0.367 | ||||
| Yes | 38 | 30 | 15 | 7 | |
| No | 366 | 183 | 117 | 61 | |
| Stroke | 0.049a | ||||
| Yes | 22 | 13 | 1 | 2 | |
| No | 382 | 200 | 119 | 66 | |
| Left-sided colorectal cancer | Right-sided colon cancer | |||||
| Univariate | Multivariate | Univariate | Multivariate | |||
| P value | P value | HR (95%CI:) | P value | P value | HR (95%CI:) | |
| Gender | 0.024a | 0.079 | 0.81 (0.63-1.02) | 0.339 | 0.023a | 0.63 (0.42-0.94) |
| Age | 0.955 | 0.792 | 1.04 (0.80-1.34) | 0.712 | 0.612 | 1.12 (0.72-1.76) |
| Histodifferentiation | 0.648 | 0.016a | 1.16 (1.03-1.31) | 0.685 | 0.407 | 1.09 (0.89-1.33) |
| TNM stage | 0.000a | 0.000a | 2.39 (1.96-2.90) | 0.000a | 0.000a | 2.63 (1.85-3.72) |
| TCM | 0.000a | 0.000a | 0.53 (0.41-0.67) | 0.003a | 0.000a | 0.47 (0.31-0.71) |
| Diabetes | 0.948 | 0.716 | 0.94 (0.66-1.32) | 0.240 | 0.200 | 0.67 (0.36-1.24) |
| Hypertention | 0.650 | 0.120 | 1.24 (0.94-1.64) | 0.019a | 0.005a | 0.51 (0.31-0.81) |
| Heart disease | 0.710 | 0.988 | 1.00 (0.66-1. 50) | 0.461 | 0.155 | 1.57 (0.84-2.93) |
| Stroke | 0.171 | 0.091 | 0.60 (0.33-1.09) | 0.681 | 0.449 | 1.34 (0.63-2.83) |
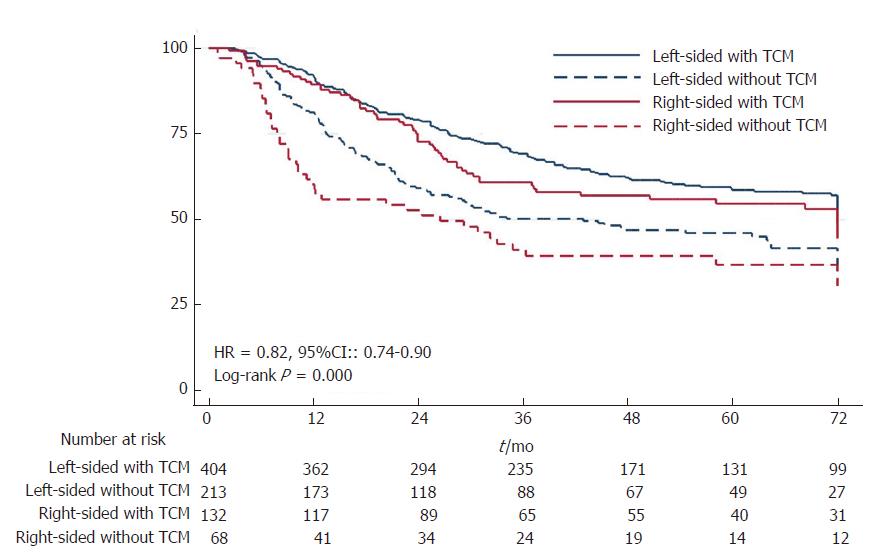
TCM conferred higher 1-6 year DFS rates on patients with LSCRC (91.98% at 1, 78.95% at 2, 69.15% at 3, 62.04% at 4, 58.45% at 5, and 56.95% at 6 years) than on LSCRC patients who did not receive TCM (81.22%, 59.05%, 50.05%, 46.92%, 46.12%, and 41.50%, respectively). The 1-6 year DFS rates of patients with RSCC in the TCM group were 89.35%, 72.82%, 60.68%, 56.77%, 54.43%, and 52.92%, respectively, whereas in the Non-TCM group, the DFS rates were 60.29%, 52.76%, 41.39%, 39.51%, 37.19%, and 37.19%, respectively (Figure 2). DFS was significantly improved by TCM not only in patients with LSCRC (HR = 0.59, P = 0.000) but also in those with RSCC (HR = 0.56, P = 0.003) (Supplementary Figures 1 and 2). However, the LSCRC and RSCC TCM groups showed similar DFS rates (HR = 0.84, P = 0.239) as did the LSCRC and RSCC Non-TCM groups (HR = 0.76, P = 0.129) (Supplementary Figures 3 and 4). The above results were relatively unchanged after propensity score matching (Supplementary Figures 5, 6, 7 and 8).
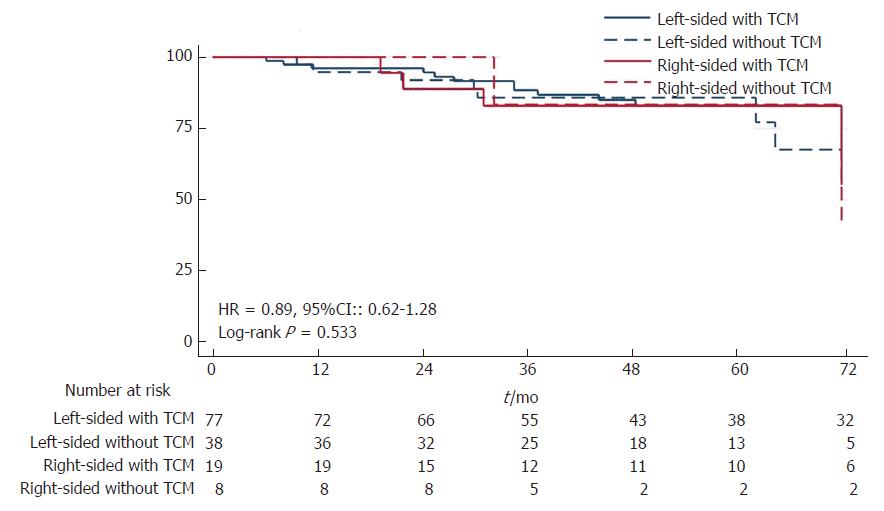
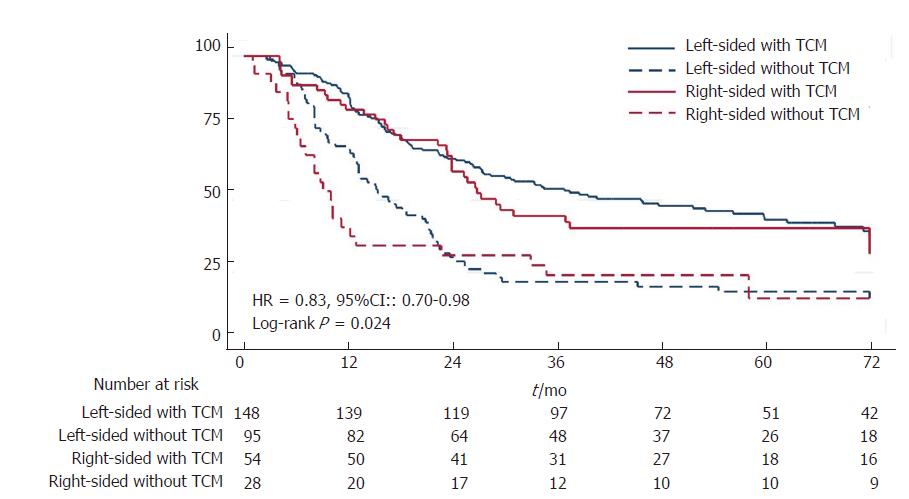
For patients with stage I disease, TCM did not exhibit an obvious advantage in extending DFS in patients with either LSCRC or RSCC (Figure 3; Supplementary Figures 9 and 10). TCM significantly prolonged DFS of patients with stage II LSCRC (HR = 0.60, 95%CI: 0.40-0.89, P = 0.011), whereas patients with stage II RSCC in the TCM group showed longer DFS than those in the Non-TCM group; however, this difference was not significant (HR = 0.56, 95%CI: 0.29-1.07, P = 0.077) (Figure 4; Supplementary Figures 11 and 12). For stage III disease, TCM was effective for patients with either LSCRC (HR = 0.44, 95%CI: 0.32-0.61, P = 0.000) or RSCC (HR = 0.47, 95%CI: 0.28-0.79, P = 0.004) (Figure 5; Supplementary Figures 13 and 14).
The multivariate regression analyses showed no multicollinearity among variables in this cox analysis (Supplementary Figures 15 and 16). TCM was an independent influencing factor for DFS of patients with either LSCRC (HR = 0.53, 95%CI: 0.41-0.67) or RSCC (HR = 0.47, 95%CI: 0.31-0.71); TNM stage was also an independent factor (HR = 2.39, 95%CI: 1.96-2.90 for LSCRC; HR = 2.63, 95%CI: 1.85-3.72 for RSCC). Histodifferentiation (HR = 1.16, 95%CI: 1.03-1.31) and hypertension (HR = 0.51, 95%CI: 0.31-0.81) were independent influencing factor for DFS of patients with LSCRC and RSCC, respectively (Table 2).
Recently, the sidedness of primary colon cancer was demonstrated to be a prognostic factor in survival. Because of their distinct biological characteristics, LSCRC and RSCC tend to be treated separately. To the best of our knowledge, this is the first study discussing the effects of TCM on LSCRC and RSCC separately. Our Cox analysis showed that TCM was an independent influencing factor on DFS for each side. Patients with LSCRC exhibited a relatively longer DFS than those with RSCC regardless of TCM administration, whereas patients with RSCC who took TCM gained a greater benefit regarding DFS-this partially narrowed the disparity in DFS between the different cancer sides.
Our study was somewhat similar to those of previous articles in that TCM coupled with chemotherapy was significantly effective in prolonging DFS of patients with CRC. Tao et al[11] L proved that compared to monochemotherapy, chemotherapy integrated with TCM obviously improved the prognosis of patients with stage II-III CRC by reducing recurrence and metastasis. Zhou et al[12] LY demonstrated that TCM effectively improved the quality of life, increased body weight and prolonged the survival of patients with CRC. Our preliminary study proposed that individuals with stage I CRC do not require TCM[6]. In this study, we found that patients with stage I CRC on either side did not benefit from TCM, whereas subjects with stage II-III LSCRC or RSCC who were administered TCM exhibited a distinct advantage in decreasing the risk of recurrence and metastasis; however, this advantage was not statistically significant in subjects with stage II RSCC. We thought that the primary reasons why TCM improved DFS of CRC on both sides lie in the advantages of TCM in attenuating toxicity, improving immunity and quality of life and enhancing medication sensitivity in patients with tumors, which can prevent metastasis and extend survival[13-17].
The different responses of LSCRC and RSCC to treatment have been previously reported. The GALGB/SWOG 80405 study, which investigated the effect of cetuximab and bevacizumab on cancer located on different sides, found that patients with LSCRC benefited more from cetuximab, whereas those with RSCC responded better to bevacizumab in terms of survival[18]. Moreover, Elsaleh et al[19] found that men with RSCC obtained increased benefits from adjuvant chemotherapy whereas men with LSCRC did not; one possible explanation may be partially due to the higher frequency of microsatellite instability (MSI) in RSCC which may be a prognostic factor for a more favorable response[19].
Whether due to differences in biological characteristics between the two sides or TCM producing a relatively better effect on RSCC, RSCC exhibited a greater benefit from TCM than LSCRC in our study; this finding is worth further study. Thus, differences between LSCRC and RSCC regarding embryological origin, blood supply, morphology, carbohydrate antigens and other factors should be considered[20]. In addition, RSCC was more commonly associated with RAS and BRAF mutations, a high CpG island methylator phenotype, mutagenic metabolites of cytochrome p450, MAPK signaling and MSI, whereas LSCRC was associated with APC, K-ras, DCC, p53 mutant EGFR signaling, Wnt signaling and HER1 and HER2 amplification which played a vital role in cancer generation and progression[21-24]. Interestingly, previous studies suggested that the prolonged survival of CRC patients by TCM was mediated by demethylating DNA, antagonizing gene mutations, targeting the MSI pathway and promoting apoptosis, which are more characteristics of RSCC[25-27].
There were some limitations in our study. Administration of TCM was tailored to each patient’s sysmptoms, signs and constitution. Although these highly individualized TCM prescriptions were adapted to the patients’ conditions to the greatest extent possible, the many different kinds and doses of herbs were difficult to be stratified in this paper[28]. In the future research, we are going to extract some core herbs used in treating CRC based on the primary tumor sides. In addition, TCM in our study was administered as a decoction, the quality of TCM herbs may differ based on the source region, season, and processing factories inevitably. We recommend granular or powder TCM formulations for future treatments. Another limitation lies in a lack of knowledge regarding the optimal period of TCM medication for patients with different TNM stages of CRC, which will be studied in our future research.
In conclusion, our study showed that TCM conferred longer DFS on patients with stage II-III CRC on both sides. Patients with LSCRC and RSCC responded differently to TCM; those with RSCC benefited more from TCM than those with LSCRC. Thus, TCM was recommended to postoperative patients with CRC of both sides, especially the right side. The mechanism of different responses of primary tumor location to TCM is worthy of further study.
The background, present status and significance of the study have been described detailedly in the section “Introduction” of the text.
The background, present status and significance of the study have been described detailedly in the section “Introduction” of the text.
The main objectives, the objectives that were realized, and the significance of realizing these objectives for future research in this field were described in the last sentence of “Introduction”, “Discussion”.
“Statistical analysis” has introduced the methods used in realizing the objectives of our manuscript in detail.
Research results have been detailedly described in the first and last paragraphs of “Discussion”.
The authors have addressed the above questions mainly in “Statistical analysis” and “Discussion”. Recently, the sidedness of primary colon cancer was demonstrated to be a prognostic factor in survival. Because of their distinct biological characteristics, LSCRC and RSCC tend to be treated separately. However, there was no evidence regarding whether TCM exerts variable effects on CRC based on the side where the lesion is located. This is the first study discussing the effects of TCM on LSCRC and RSCC separately. Our results showed that patients with LSCRC exhibited a relatively longer DFS than those with RSCC regardless of TCM administration, whereas patients with RSCC who took TCM gained a greater benefit regarding DFS. Because of their distinct biological characteristics and the therapeutic effect, LSCRC and RSCC should be treated separately in future. The DFS was evaluated using Kaplan-Meier curves and log-rank tests. The authors adopted propensity score matching to model the probability that a patient exhibited a specific characteristic based on gender, age, location, histodifferentiation, TNM stage, lymph node status, chemotherapy, radiotherapy and comorbidities to test the stability of the research. In addition, the authors applied multivariate regression analyses for multicollinearity diagnosis and Cox proportional hazards regression model for multivariate factor analysis.
Recent studies have proposed that location of primary tumor was related to recurrence, metastasis and the therapeutic effect. The author’s results indicated that patients with LSCRC and RSCC responded differently to TCM; those with RSCC benefited more from TCM than those with LSCRC. Thus, TCM was recommended to postoperative patients with CRC of both sides, especially the right side. In the future research, CRC should be treated separately based on the primary tumor sides.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Jeong KY, Mavridis K, Liao KF S- Editor: Chen K L- Editor: A E- Editor: Ma YJ
| 1. | Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11065] [Cited by in F6Publishing: 11879] [Article Influence: 1697.0] [Reference Citation Analysis (3)] |
| 2. | Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67:177-193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2526] [Cited by in F6Publishing: 2754] [Article Influence: 393.4] [Reference Citation Analysis (2)] |
| 3. | Wilhelmsen M, Kring T, Jorgensen LN, Madsen MR, Jess P, Bulut O, Nielsen KT, Andersen CL, Nielsen HJ. Determinants of recurrence after intended curative resection for colorectal cancer. Scand J Gastroenterol. 2014;49:1399-1408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Adams M, Jewell AP. The use of Complementary and Alternative Medicine by cancer patients. Int Semin Surg Oncol. 2007;4:10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Li W, Li C, Zheng H, Chen G, Hua B. Therapeutic targets of Traditional Chinese Medicine for colorectal cancer. J Tradit Chin Med. 2016;36:243-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Shi Q, Liu S, Li W, Zong S, Han S, Yang W, Li H, Hou F. Exploring the medication duration based on the effect of traditional Chinese medicine on postoperative stage I-III colorectal patients: a retrospective cohort study. Oncotarget. 2017;8:13488-13495. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Holch JW, Ricard I, Stintzing S, Modest DP, Heinemann V. The relevance of primary tumour location in patients with metastatic colorectal cancer: A meta-analysis of first-line clinical trials. Eur J Cancer. 2017;70:87-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 317] [Cited by in F6Publishing: 367] [Article Influence: 45.9] [Reference Citation Analysis (0)] |
| 8. | Benedix F, Kube R, Meyer F, Schmidt U, Gastinger I, Lippert H; Colon/Rectum Carcinomas (Primary Tumor) Study Group. Comparison of 17,641 patients with right- and left-sided colon cancer: differences in epidemiology, perioperative course, histology, and survival. Dis Colon Rectum. 2010;53:57-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 480] [Cited by in F6Publishing: 502] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 9. | Hansen IO, Jess P. Possible better long-term survival in left versus right-sided colon cancer - a systematic review. Dan Med J. 2012;59:A4444. [PubMed] [Cited in This Article: ] |
| 10. | Lu HJ, Lin JK, Chen WS, Jiang JK, Yang SH, Lan YT, Lin CC, Chang SC, Teng HW. Primary tumor location is an important predictive factor for wild-type KRAS metastatic colon cancer treated with cetuximab as front-line bio-therapy. Asia Pac J Clin Oncol. 2016;12:207-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Tao L, Zhu YJ, Lu XM, Gu Y, Zhao AG, Zheng J, Fu CG, Yang JK. [Clinical study on survival benefit for elderly patients with resected stage II or III colorectal cancer based on traditional Chinese medicine syndrome differentiation and treatment]. Zhong Xi Yi Jie He Xue Bao. 2010;8:1159-1164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Zhou LY, Shan ZZ, You JL. Clinical observation on treatment of colonic cancer with combined treatment of chemotherapy and Chinese herbal medicine. Chin J Integr Med. 2009;15:107-111. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Shi Q, Li W, Le QQ, Chen WT, Ren JL, Li Q, Hou FG. Attenuated effects of Jianpi Qushi herbs on patients receiving FOLFOX4 after colorectal cancer surgery: A meta-analysis. Chin J Integr Med. 2016;1-10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Li YR, Chen YQ, Wang H, Zhu P, Chen HJ, Yang BL, Gu YF. Meta - analysis of Chemotherapy Combined with Traditional Chinese Medicine Decoction in Cellular Immunity of Patients with Colorectal Cancer. Liaoning Journal of Traditional Chinese Medicine. 2016;2035-2041. [DOI] [Cited in This Article: ] |
| 15. | Qu YL, Yue GJ, Li JS, Huang H. Effect of Jinlong Capsules on Reversing Paclitaxel-resistance Vincritine-resistance and Enhancing Sensitivity in Human Cancer Cell Lines. Cancer Research on Prevention and Treatment. 2014;884-887. [DOI] [Cited in This Article: ] |
| 16. | Zhu YD. Clinical research on reducing recurrence and metastasis of II, III period colorectal cancer in the integrative medicine. Zhongguo Zhongliu Fangzhi Zazhi. 2016;23:212-213. [DOI] [Cited in This Article: ] |
| 17. | Qi YM, Wu SS, Shen MH, Ruan SM, Wu S, Guo KB, Huang AQ. Meta - analysis of TCM Therapy Combined with Chemotherapy on Survival Time of Patients with Colorectal Cancer at Stages III - IV. Zhongguo Zhongyiyao Keji Zazhi. 2014;32:2835-2838. [DOI] [Cited in This Article: ] |
| 18. | Venook A, Niedzwiecki D, Lenz HJ, Innocenti F, Mahoney M, O’Neil B, Shaw JE, Polite B, Hochster H, Atkins JN. CALGB/SWOG 80405: Phase III trial of irinotecan/5-FU/leucovorin (FOLFIRI) or oxaliplatin/5-FU/leucovorin (mFOLFOX6) with bevacizumab (BV) or cetuximab (CET) for patients (pts) with KRAS wild-type (wt) untreated metastatic adenocarcinoma of the colon or rectum (MCRC). J Clin Oncol. 2014;32:LBA 3. [Cited in This Article: ] |
| 19. | Elsaleh H, Joseph D, Grieu F, Zeps N, Spry N, Iacopetta B. Association of tumour site and sex with survival benefit from adjuvant chemotherapy in colorectal cancer. Lancet. 2000;355:1745-1750. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 406] [Cited by in F6Publishing: 438] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 20. | Bufill JA. Colorectal cancer: evidence for distinct genetic categories based on proximal or distal tumor location. Ann Intern Med. 1990;113:779-788. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 505] [Cited by in F6Publishing: 526] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 21. | Kim SE, Paik HY, Yoon H, Lee JE, Kim N, Sung MK. Sex- and gender-specific disparities in colorectal cancer risk. World J Gastroenterol. 2015;21:5167-5175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 274] [Cited by in F6Publishing: 268] [Article Influence: 29.8] [Reference Citation Analysis (4)] |
| 22. | Yamauchi M, Morikawa T, Kuchiba A, Imamura Y, Qian ZR, Nishihara R, Liao X, Waldron L, Hoshida Y, Huttenhower C. Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct dichotomy of proximal versus distal colorectum. Gut. 2012;61:847-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 428] [Cited by in F6Publishing: 465] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 23. | Chang LC, Yu YL. Dietary components as epigenetic-regulating agents against cancer. Biomedicine (Taipei). 2016;6:2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Padma VV. An overview of targeted cancer therapy. Biomedicine (Taipei). 2015;5:19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 203] [Cited by in F6Publishing: 232] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 25. | Zhang M, Zhu WF, Ji Q, Sun Z, Zhou Y, Zhang M, Peng SH. Research Progress of DNA Demethylation of Anti-tumor Traditional Chinese Medicines. Zhongguo Shiyan Fangjixue Zazhi. 2015;21:224-229. [Cited in This Article: ] |
| 26. | Liu XF, Jin HY, Ding YJ, Lu Y, Li L, Ding SQ, Liu F, Ni M, Wang J. Inhibitory effect of Chinese herbs with anti-mutation activity on a mismatch-repair-gene-deficient colorectal cancer cell line. Shijie Huaren Xiaohua Zazhi. 2007;15:2201-2204. [Cited in This Article: ] |
| 27. | Ho TF, Chang CC. A promising “TRAIL” of tanshinones for cancer therapy. Biomedicine (Taipei). 2015;5:23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Teschke R, Wolff A, Frenzel C, Eickhoff A, Schulze J. Herbal traditional Chinese medicine and its evidence base in gastrointestinal disorders. World J Gastroenterol. 2015;21:4466-4490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 73] [Cited by in F6Publishing: 73] [Article Influence: 8.1] [Reference Citation Analysis (2)] |