Published online Sep 21, 2017. doi: 10.3748/wjg.v23.i35.6457
Peer-review started: June 16, 2017
First decision: July 17, 2017
Revised: July 27, 2017
Accepted: August 15, 2017
Article in press: August 15, 2017
Published online: September 21, 2017
To describe the indications, technique and outcomes of the novel surgical procedure of duodenum and ventral pancreas preserving subtotal pancreatectomy (DVPPSP).
Data collected retrospectively from 43 patients who underwent DVPPSP and TP between 2009 and 2015 in our single centre were analysed. For enrolment, only patients with low-grade pancreatic neoplasms, such as pancreatic neuroendocrine tumors, intraductal papillary mucinous neoplasms (IPMNs), and solid pseudo-papillary tumors, were included. Ten DVPPSP (group 1) and 13 TP (group 2) patients were selected in this study.
There were no significant differences in age, gender, comorbidities, preoperative symptoms, American Society of Anesthesiologists score or indications for surgery between the two groups. The most common indication was IPMN for DVPPSP and TP (60% vs 85%, P = 0.411). Compared with the TP group, the DVPPSP group had comparable postoperative morbidities (P = 0.405) and mortalities (both nil), but significantly shorter operative time (232 ± 19.6 min vs 335 ± 32.3 min, P < 0.001). DVPPSP preserved better long-term pancreatic function with less supplementary therapy (P < 0.001) and better quality of life (QoL) after surgery, including better scores in social (P = 0.042) and global health (P = 0.047) on functional scales and less appetite loss (P = 0.049) on the symptom scale.
DVPPSP is a feasible and safe procedure that could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas; DVPPSP had better metabolic function and QoL after surgery.
Core tip: Although total pancreatectomy (TP) can be performed safely, the long-term metabolic complications prevent its application. Herein, we report our experience of duodenum and ventral pancreas preserving subtotal pancreatectomy (DVPPSP), which could be an alternative procedure to TP for low-grade pancreatic neoplasms, with a focus on the surgical indications, techniques and outcomes. Our results indicate that DVPPSP is a feasible and safe procedure that could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas, with a better metabolic function and quality of life after surgery.
- Citation: Wang X, Tan CL, Song HY, Yao Q, Liu XB. Duodenum and ventral pancreas preserving subtotal pancreatectomy for low-grade malignant neoplasms of the pancreas: An alternative procedure to total pancreatectomy for low-grade pancreatic neoplasms. World J Gastroenterol 2017; 23(35): 6457-6466
- URL: https://www.wjgnet.com/1007-9327/full/v23/i35/6457.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i35.6457
Parenchyma-sparing procedures are increasingly performed for low-grade pancreatic neoplasms, such as intraductal papillary mucinous neoplasms (IPMNs), neuroendocrine tumors (NETs), and pseudo-papillary tumors (SPTs)[1,2]. These procedures preserve the pancreatic parenchyma and decrease the risk of long-term endocrine and exocrine dysfunction[3,4]. However, according to different reports, in these low-grade diseases, the percentages of total pancreatectomy (TP) range from 5% to 28% because these diseases frequently involve the entire gland[5-7]. The indications for primary elective TP are typically these pancreatic diseases. Although TP could be performed safely in many centres, the long-term metabolic complications that include brittle diabetes and unmanageable steatorrhea prevent its application. Additionally, wide resection of the total pancreas and duodenum after TP could lead to a reduced quality of life (QoL), which makes patients anguished. The conventional parenchyma-sparing procedures, such as enucleation and central pancreatectomy, are unable to substitute TP for lesions involving the head, body and tail of the pancreas.
As a function preserving procedure, Thayer et al[8] reported a complete dorsal pancreatectomy with preservation of the ventral pancreas (the proximal duodenum was resected for ischemia) in 2002. Duodenum-preserving pancreatic head resection was introduced into surgical practice in 1972. This surgical method has been well developed by Doctor Beger et al[9] in past decades. The rationale to apply a duodenum-preserving pancreatic resection is to avoid resection of the gastric antrum, to preserve the duodenum and the extrahepatic biliary duct for low-grade lesions. This procedure has low short-term postoperative morbidity and mortality, and maintenance of the endocrine and exocrine functions in the long-term after surgery. A significant superiority of the duodenum-preserving procedure regarding overall improvement of QoL was reported[10]. Herein, we report our experience of duodenum and ventral pancreas preserving subtotal pancreatectomy (DVPPSP), which could be an alternative procedure to TP for selected patients with low-grade pancreatic neoplasms. The aim of our present study was mainly to describe the indications, operative technique and outcomes of the novel surgical procedure compared with TP.
From January 2009 to January 2015, patients who underwent DVPPSP for low-grade pancreatic neoplasms (such as NETs, IPMNs and SPTs) were identified in our institution. To evaluate the outcomes of DVPPSP compared with TP, patients who underwent TP for low-grade pancreatic neoplasms were also identified during this period. Surgeries for pancreatic ductal adenocarcinoma and chronic pancreatitis determined on postoperative pathology were excluded. The selected patients were divided into two groups as follows: DVPPSP group (group 1) and TP group (group 2). The groups were analysed regarding age, gender, type of comorbidities, body mass index (BMI), American Society of Anesthesiologists score (ASA), operative time, blood transfusion and postoperative data (histology of pancreatic disease, postoperative mortality and morbidity, postoperative length of hospital stay). The postoperative mortality rate included all deaths within 30 d after surgery. The morbidity rate included all complications following surgery until discharge. Major postoperative morbidities were defined and graded using the criteria recommended by the International Study Group of Pancreatic Surgery, including postoperative pancreatic fistula, delayed gastric emptying, and postpancreatectomy haemorrhage[11-13]. Biliary leak was defined as drainage of any volume of fluid from percutaneous drains or a wound consistent with bile, which was defined by a bilirubin concentration greater than the serum concentration. Enteric leaks were identified using radiographic contrast imaging. Fluid collection in the intra-abdominal or pleural regions was determined via radiographic imaging, which was differentiated from abscess by positive microbial cultures. Pneumonia was diagnosed based on chest X-ray changes following antibiotic therapy.
Follow-up examinations were collected from the store of medical information centre in the hospital and from the results of follow-up by letters and telephone at the time of this study. The endocrine and exocrine controls were assessed by episodes of hyperglycaemia/day, daily dosage of insulin, pancreatic enzyme replacement. The QoL of patients were evaluated with the European Organization for Research and Treatment of Cancer Quality of life Questionnaire (EORTC QLQ-C30) version 3.0. The questionnaires were requested to be filled in by the patients themselves via mailing or completing in the clinic. The patients who had been dead or had tumor recurrence during the study were excluded from the analysis of QoL. This study was approved by the Ethics Committee of Sichuan University.
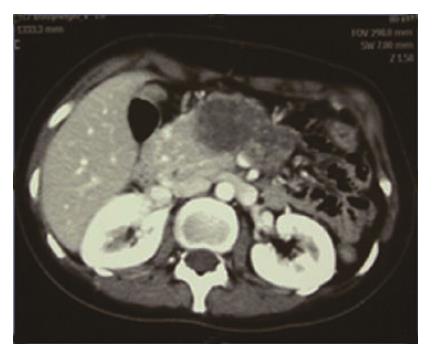
DVPPSP was an alternative operative technique to TP of low-grade pancreatic tumor arising from the body and tail region but across the neck region of the pancreas (Figure 1). Contrast-enhanced computed tomography (CT), magnetic resonance imaging (MRI), or/and endoscopic ultrasound (EUS) were routinely performed to evaluate the lesions. Furthermore, DVPPSP was finally considered after intraoperative evaluation of the lesion, which confirmed negative for neoplasm of ventral pancreas based on palpation and intraoperative ultrasonography. Frozen sectioning was routinely performed to achieve negative margins in the present study. If invasive carcinoma was found in the frozen section of the stump, the DVPPSP was immediately converted to TP with formal lymphadenectomy.
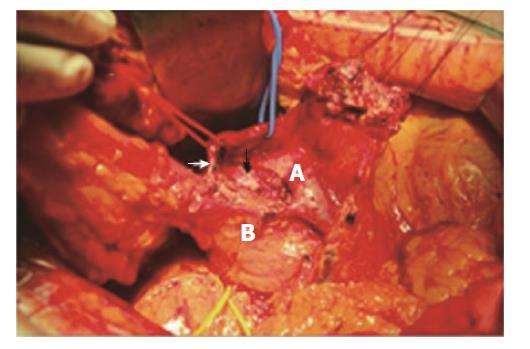
The surgical procedures were performed by one group of experienced surgeons in our department of pancreatic surgery. We performed a complete Kocher manoeuvre to mobilize the duodenum, the pancreatic head and uncinate process from the posterior connective tissue membrane. There was a call for intraoperative ultrasound to confirm that the ventral pancreas was negative for neoplasm. Then, the neck and body of the pancreas was freed from the common hepatic artery, portal vein, and superior mesenteric vein. The gastrocolic trunk was divided and ligated at its confluence. Then, we dissected and taped the gastroduodenal artery (GDA). The anterior superior pancreaticoduodenal artery (ASPD) and other small branches of GDA in front of the cephalic pancreas could be resected to expose the common bile duct (CBD) at the upper edge of the pancreas and to completely resect the neoplasm. We preserved the GDA and the posterior superior pancreaticoduodenal artery (PSPD) (Figure 2). The transection of the cephalic side of the pancreas was begun at the edge of the neoplasm and was continued caudally. The posterior transection plane was along the anterior side of the CBD (Figure 2). Inferiorly, we dissected and exposed the CBD from the resecting pancreas toward the major papilla to achieve complete resection of the neoplasm.
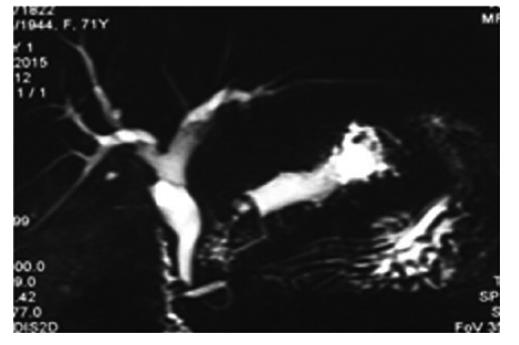
If the neoplasm involved the entire dorsal pancreas, such as IPMN that involved the whole dorsal duct (including the Santorini duct) but ventral duct (Figure 3), a complete dorsal pancreatectomy was needed to achieve radical resection of the tumor. The embryological fusion plane between the ventral and the dorsal pancreas was confirmed by autopsy[14] and was described as a clear fibrous septum[8]. These anatomical characteristics made the complete dorsal pancreatectomy procedure theoretically feasible. However, the plane was difficult to identify in our study during surgery. Instead, we continued pancreatic transection and exposed the whole distal CBD (except its last centimetre) to achieve a complete dorsal pancreatectomy and we the confluence of the CBD with the ventral duct. The dorsal pancreatic duct was divided and ligated 3 mm away from the duodenal lumen and was free of neoplasia on frozen section examination. The anterior inferior pancreaticoduodenal artery (AIPD) could be included in the resection site if necessary. Then, we identified the main pancreatic duct (Wirsung duct) in the stump of the residual pancreas and ligated this duct. The stump was negative for tumor on frozen sectioning, which was routinely performed in the present study.
Parenchyma sutures and tissue sealant were used in selected cases. Bipolar cautery, ultrasound scalpel and the suture technique using 4-0 absorbable sutures (Ethicon, Inc) were used for haemostasis and pancreatostasis. It was worth noting that bipolar cautery was not performed in the deep areas near the Wirsung duct or other important structures (CBD or major vessels) due to presumed heat injury. Pa-renchymal sutures and tissue sealant were used for cases in which haemostasis and pancreatostasis were not satisfied exclusively using bipolar cautery and ultrasound scalpel. Finally, we routinely placed at least one drain adjacent to the cut surface.
Drain amylase analysis was performed from postoperative day one to three and then every other day. For patients without a fistula, we progressively withdrew drainage starting on postoperative day three and finally removed the drain on postoperative day five. Postoperative octreotide was routinely used for seven days to decrease the secretion of the pancreas. We routinely performed abdominal EUS before finally removing the drain. The long-term follow-up should be performed after DVPPSP, even if the stump is negative.
The Pearson χ2 test was used for categorical variables. Fisher’s exact test was used in cases with a variable count < 5. For continuous variables, Student’s t test was used for normally distributed variables and the Wilcoxon rank-sum test was used for non-normally distributed variables. P < 0.05 was considered statistically significant. All analyses were performed using SPSS version 18.0 software on a personal computer (SPSS Inc., Chicago, IL, United States).
DVPPSP was performed for 10 patients, and TP was performed for 33 patients between January 2009 and January 2015 in our department. Patients with chronic pancreatitis, pancreatic cancers (PC) and pancreatic metastases were excluded in this study. Of these, twenty patients who underwent TP, including 2 with chronic pancreatitis, 16 with PC, and 2 with pancreatic metastases from renal cell cancer, were excluded in our present study. Finally, ten DVPPSP (group 1) and 13 TP (group 2) patients were selected in this study.
The preoperative characteristics of the patients undergoing DVPPSP and TP are summarized in Table 1. There were no significant differences in age, gender, comorbidities, preoperative symptoms, ASA score or indications for surgery between the two groups. The median age was 49 in the DVPPSP group and 56 in the TP group. Four male patients (40%) were in the DVPPSP group, and 7 males (54%) were in the TP group. In the DVPPSP and TP groups, the majority of patients were symptomatic (100% vs 85%), and abdominal pain (40% vs 55%) was the most common symptom. The ASA III was given to 3 patients in DVPPSP and TP group. The pathologic features of the lesions in the DVPPSP and TP groups are shown in Table 1. The most common indication for DVPPSP or TP was IPMN (6/10, 60% vs 11/13, 85%). All the 6 IPMNs who underwent DVPPSP were main duct type (MD-IPMN). The 11 IPMNs in the TP group comprised 9 MD-IPMN, 1 mixed-type (MT-IPMN) and 1 multifocal type. According to the 2010 WHO classification, one out of 6 IPMN in the DVPPSP group and 5 out of 11 IPMN in the TP group were detected as invasive carcinoma (16.7% vs 45.5%, P = 0.333). The 2 NETs in the DVPPSP group and the 1 NET in the TP group were classified as G2.
| Patient characteristics | DVPPST(n = 10) | TP (n = 13) | P vaule |
| Age (range, yr) | 49 ± 16.9 (24-71) | 56 ± 10.1 (40-70) | 0.256 |
| Gender (%) | 0.680 | ||
| Male | 4 (40) | 7 (54) | |
| Female | 6 (60) | 6 (46) | |
| Major comorbidity | |||
| CAD | 0 | 1 | 1.000 |
| COPD | 1 | 2 | 1.000 |
| DM | 2 | 3 | 1.000 |
| Hypertension | 3 | 3 | 1.000 |
| Preoperative symptoms | |||
| Incidental | 0 | 2 (15) | 0.486 |
| Symptomatic (%) | 10 (100) | 11 (85) | |
| Abdominal pain | 4 (40) | 6 (55) | 1.000 |
| Pancreatitis | 1 | 4 | 0.339 |
| Weight loss | 1 | 4 | 0.339 |
| Gastrointestinal symptoms | 4 | 3 | 0.65 |
| ASA score | 1.000 | ||
| I/II | 7 | 10 | |
| III | 3 | 3 | |
| Pathology (%) | 0.411 | ||
| IPMN | 6 (60) | 11 (85) | |
| Low-grade moderate-grade dysplasia | 2 | 1 | 0.515 |
| High-grade dysplasia | 3 | 4 | 0.644 |
| Invasive carcinoma | 1 (16.7) | 5 (45.5) | 0.333 |
| Neuroendocrine tumor | 2 | 1 | |
| G 2 | 2 | 1 | 1.000 |
| SPT | 2 | 1 | |
| Total invasive malignancy | 1 (10) | 5 (38.5) | 0.179 |
The intra-operative and postoperative short-term outcomes of the two groups are summarized in Table 2. None of the parameters listed were significantly different between the two groups except the operative time, which was significantly shorter in the DVPPSP group compared with the TP group (232 min vs 335 min, P < 0.001). The total morbidities were 20% (2/10) and 38% (5/13) in the DVPPSP and TP group, respectively. There was no significant difference in the post-operative morbidity between the two groups, including delay gastric emptying (DGE) and biliary fistula. Clinical pancreatic fistula (grade B or C) was not found in either group. There were no reoperations or readmissions in either group. The mortalities were nil in both groups. Although there was no significant difference, the post-operative hospital stay days (LOS) appeared to be slightly shorter in the DVPPSP group (9.7 d vs 11.7 d, P = 0.318). The mean follow-up lengths were 26.6 and 33.9 months in the DVPPSP and TP groups, respectively. There were 2 out of 10 patients in the DVPPSP group and 5 out of 13 patients in the TP group proven to have recurrences (20% vs 38.5%, P = 0.405) (Table 2). Two out of 6 IPMNs in the DVPPSP group were shown to have recurrence at 28 and 36 mo after surgery separately, although negative margins were detected by intra-operative frozen sections. A total of 5 out of 11 IPMNs in the TP group were shown to have recurrence at 16, 26, 30, 34, 50 mo after surgery separately (2/6, 33.3% vs 5/11, 45.5%, P = 1.000).
| Operative characteristics | DVPPSP(n = 10) | TP (n = 13) | P vaule |
| Intraoperative transfusion (U) | 0.20 ± 0.63 (0-2) | 0.54 ± 1.05 (0-3) | 0.379 |
| Operative time (min) | 232 ± 19.6 (215-255) | 335 ± 32.3 (280-400) | < 0.001 |
| Postoperative characteristics | |||
| DGE | 0 | 1 | 1.000 |
| Biliary fistula | 0 | 1 | 1.000 |
| Pancreatic fistula (B and C) | 0 | 0 | — |
| Overall morbidity | 2 | 5 | 0.405 |
| Major morbidity (≥ grade 3) | 1 | 2 | 1 |
| Reoperation | 0 | 0 | — |
| Readmission (30 d) | 0 | 0 | — |
| LOS | 9.7 ± 3.8 (7-20) | 11.7 ± 5.2 (8-26) | 0.318 |
| Mortality | 0 | 0 | — |
| Recurrence1(%) | 2 (20%) | 5 (38.5%) | 0.405 |
| IPMN | 2/6 | 5/11 | 1.000 |
The differences in replacement therapy are sum-marized in Table 3. The mean follow-up lengths were 26.6 and 33.9 mo in the DVPPSP and TP groups, respectively. There were significant differences in replacement therapy between the two groups. The mean enzyme replacements were 0.9 cps/d vs 9.2 cps/d (P < 0.001) in the DVPPSP and TP groups, respectively. The total insulin doses were 6.4 U/d vs 29.7 U/d (P < 0.001). No patients had hyperglycaemia after insulin treatment in the DVPPSP group, whereas five patients (38%) in the TP group still had hyperglycaemia occasionally (P = 0.046). There were still 2 patients (20%) having diarrhea and steatorrhea occasionally after replacement treatment in the DVPPSP group, compared with 4 patients (31%) in the TP group (P = 0.660). The long term results regarding pancreatic endocrine function after DVPPSP are summarized in Table 4. Of the 10 patients who had DVPPSP, seven patients had no diabetes before surgery. There were no patients with new-onset diabetes. Of the 3 patients who had diabetes before surgery in the DVPPSP group, only one patient (1/3, 33%) had the diabetes worsen after surgery. This patient changed treatment with oral medication to treatment with insulin. The quality of life (QoL) according the EORTC QLQQ-C30 is summarized in Table 5.
| Parameters | DPPSP(n = 10) | TP (n = 13) | P vaule |
| Enzymes replacement (cps/d) | 0.9 ± 2.0 | 9.2 ± 2.2 | < 0.001 |
| Total insulin dose (U/d) | 6.4 ± 14.0 | 29.7 ± 9.3 | < 0.001 |
| Diarrhea or steatorrhea | 2 | 4 | 0.660 |
| Hyperglycemia | 0 | 5 | 0.046 |
| Parameters | DVPPSP(n = 8) | TP (n = 8) | P vaule |
| Functional scale | |||
| Physical | 95.0 ± 9.3 (80-100) | 97.5 ± 7.1 (80-100) | 0.554 |
| Working ability | 100 | 100 | — |
| Cognitive | 100 | 100 | — |
| Emotional | 98.4 ± 2.9 (93.8-100) | 92.2 ± 8.0 (75-100) | 0.057 |
| Social | 95.8 ± 7.7 (83.3-100) | 85.4 ± 10.7 (66.7-100) | 0.042 |
| Global QoL | 96.9 ± 6.2 (83.3-100) | 88.5 ± 8.9 (75-100) | 0.047 |
| Symptom scale | |||
| Fatigue | 4.2 ± 8.3 (0-22.2) | 11.1 ± 11.7 (0-33.3) | 0.196 |
| Nausea and vomiting | 0 | 6.3 ± 12.4 (0-33.3) | 0.197 |
| Pain | 0 | 0 | — |
| Appetite loss | 0 | 20.8 ± 24.8 (0-66.7) | 0.049 |
| Dyspnea | 0 | 0 | — |
| Sleep disturbance | 4.2 ± 11.8 (0-33.3) | 12.5 ± 17.2 (0-33.3) | 0.281 |
| Constipation | 0 | 4.2 ± 11.8 (0-33.3) | 0.351 |
| Diarrhea | 4.2 ± 11.8 (0-33.3) | 12.5 ± 24.8 (0-66.7) | 0.405 |
| Financial strain | 0 | 8.3 ± 15.4 (0-33.3) | 0.170 |
A total 16 patients were qualified to complete questions about the EORTC QLQ-C30 at the time of this study. Each group included 8 patients. Due to the recurrence of IPMNs, two patients in the DVPPSP group and 5 patients in the TP group mentioned above were excluded from the inquiry. As presented in Table 5, patients in the DVPPSP group could have a higher quality of life status after surgery compared with the TP group. A high scale score in the global health, physical, working ability, emotional, cognitive and social functioning represented a high quality of life status. Regarding the symptoms and financial impact of the disease, the low scale score indicated no important problems. There were significant differences existing in social (P = 0.042) and global health (P = 0.047) on functional scale. There was a significant difference existing in appetite loss (P = 0.049) on the symptom scale.
Although TP could be performed safely as reported by different authors in the literature, patients would suffer from the pain of replacement therapy throughout their lives[15-17]. When faced with benign or low-grade malignant disease with long life expectancy such as pNETs, IPMNs and SPTs, the need for a proper treatment has to be balanced with the risk of long term impairment of exocrine/endocrine function of the gland. Herein, we described the outcomes after 10 DVPPSPs performed for low-grade malignant disease compared with 13 TPs performed for the same spectrum of disease, showing that DVPPSP is safe and effective for preserving the exocrine/endocrine function of the gland. This procedure could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas.
It is a difficult question when we find the low-grade malignant neoplasm originating from the distal pancreas across the pancreatic neck. TP might bring negative margins but be accompanied by a loss of exocrine/endocrine function. When choosing distal pancreatectomy, positive margins might be inevitable. We used to choose primary or complete TP for this type of neoplasm in our department 8 years ago. After the first DVPPSP was performed successfully, this procedure became our first choice when negative margins could be achieved at the pancreatic head. Intraoperative EUS and frozen sectioning are indispensable to decide where to perform limited pancreatic resection and to achieve negative margins. It is worth noting that only patients with benign or low-grade pancreatic neoplasms are selected as candidates for DVPPSP. The patients with such neoplasms could obtain long disease-free life expectancy if negative margins are achieved[18-20]. If invasive features or any doubts about the low-grade character of the stump were found in the frozen section, DVPPSP was immediately converted to TP with formal lymphadenectomy.
Moreover, diseases such as IPMN might predispose the entire gland, especially for the type of main duct, so detailed examination (such as endoscopic ultrasonography) could be needed before DVPPSP to detect the condition of the main duct[21]. DVVPSP is suitable for disease with a normal Wirsung duct in the ventral pancreas. If the entire duct is involved, the ventral pancreas should not be preserved. In this case, duodenum preserving total/subtotal pancreatic resection might be the best choice[22].
Due to the biological features of low-grade malignant neoplasms, normal interstitial space exists between the neoplasm and the peri-pancreatic tissue. This space is the key prerequisite to perform DVPPSP successfully. According to Yoshihiro’s research[14] based on autopsy specimens, the dorsal pancreas makes up the pancreatic neck, body, and tail, as well as the anterior segment of the head, whereas the ventral pancreas comprises the posterior segment of the head and uncinate process. Moreover, Thayer et al[8] described the embryonic fusion plane of the two segments as a clear fibrous septum. These anatomic features make the duodenum and ventral pancreas preserving subtotal pancreatectomy (DVPPSP) a theoretically feasible procedure. As this plane was difficult to identify by some researchers[23] and by us in practice, we performed the pancreatic transection along the anterior side of the CBD and exposed the entire distal CBD (except 1-2 cm from the major papilla) to achieve negative margins. The confluence of the CBD with the ventral duct and ventral pancreas was carefully preserved.
A case of complete dorsal pancreatectomy was pre-sented previously[8], with the first part of the duodenum resected due to ischemic damage. The gastroduodenal artery (GDA) was ligated in that procedure, while both the gastroduodenal artery and the posterior pancreaticoduodenal arterial arcade were preserved in our series. Additionally, the Kocher manoeuvre was suggested to increase the risk of duodenal ischemia in another previous case report[23]. However, we performed a complete Kocher manoeuvre to make the potential haemorrhage easier to control and to make the surgical procedure smoother during resection of the cephalic side of the pancreas. The duodenum was not found to be cyanotic in our present study with 10 DVPPSP cases. Careful dissection and reservation of the GDA and the posterior pancreaticoduodenal arterial arcade appeared to be essential for preservation of the duodenum in DVPPSP. The successful preservation of the duodenum prevents reconstruction in the upper digestive tract.
Our results (Table 2) also demonstrated that, compared with the TP group, DVPPSP had comparable short-term postoperative morbidities. Postoperative pancreatic fistula (POPF) is the most common complication after pancreatectomy[24,25]. However, clinical POPF (Grade B or C) was not detected in the 10 patients who underwent DVPPSP according to the revised definition by the International Study Group on Pancreatic Fistula (ISGPF)[26]. DVPPSP appears to be a safe and feasible procedure for selected low-grade pancreatic neoplasms based on our results. As shown in Table 2, 33.3% IPMN in the DVPPSP group and 45.5% IPMN in the TP group were shown to have recurrences (P = 1.000). The rate of postoperative recurrence of IPMN appeared slightly high compared with previous reports (0%-30%)[27-29]. The malignant component was suggested to be associated with tumor recurrence[29,30]. The high rate of malignancy (high-grade dysplasia or invasive carcinoma, 13/17, 76.5%; Table 1) of IPMN in our study might play a role in this recurrence, which was reported by others[29,31,32] to range from 35.7% to 68%. Furthermore, the small number of patients prevented us from making strong conclusions.
Given the long life expectancy after surgery for these diseases, the postoperative long-term pancreatic function and QoL become a major concern. Compared with the TP group, we found that DVPPSP did pre-serve better long-term pancreatic function with less supplementary therapy and resulted in better QoL after surgery in the follow-up of our study. No new-onset diabetes occurred in the DVPPSP group in the follow-up. Only one out of three patients had diabetes worsen, as shown in Table 4. This reservation could be attributed to less loss of the pancreatic parenchyma in DVPPSP.
In recent years, several investigators have advocated that postoperative QoL is as significant a clinical outcome as morbidity and mortality. The QoL of DVPPSP compared with TP in this study appeared to be better no matter replacement therapy or survey of quality of life. The high dependence of pancreatic enzyme replacement and insulin mainly negatively impacted the social and global quality of life in TP patients. The diabetes after TP could cause a negative impact on QoL[33]. More patients in the TP group felt a loss of appetite compared with patients in the DVPPSP group, perhaps because of manual changes of the digestive tract. The enterogastric reflux was considered an unavoidable consequence after reconstruction in the upper digestive tract[34]. The great advantage of DVPPSP is preservation of the natural digestive channel. Other reports have demonstrated better QoL in duodenum preserving pancreatic surgery[35-37].
Our study is limited by the small number of cases because of the infrequent indications for DVPPSP. Some questions need to be researched further. A major limitation of the present study was its retrospective nature, which prevented us from making strong conclusions. Quality of life metrics were administered only once and were not compared with preoperative baseline measurements.
In conclusion, DVPPSP is a feasible and safe pro-cedure that could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas, with a better metabolic function and QoL after surgery.
Parenchyma-sparing procedures are increasingly performed for low-grade pancreatic neoplasms, such as intraductal papillary mucinous neoplasms (IPMNs), neuroendocrine tumors, and pseudo-papillary tumors. These procedures preserve the pancreatic parenchyma and decrease the risk of long-term endocrine and exocrine dysfunction. The conventional parenchyma-sparing procedures, such as enucleation and central pancreatectomy, are unable to substitute for total pancreatectomy (TP) for lesions involving the head, body and tail of the pancreas. Herein, we report our experience of duodenum and ventral pancreas preserving subtotal pancreatectomy (DVPPSP), which could be an alternative procedure to TP for low-grade pancreatic neoplasms.
Although TP could be performed safely as reported by different authors in studies, patients would suffer from the pain of replacement therapy throughout their lives. These results showed that DVPPSP is safe and effective for preserving the exocrine/endocrine function of the gland, with a better metabolic function and QoL after surgery. DVPPSP could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas.
This study described the indications, operative technique and outcomes of the novel surgical procedure DVPPSP. Furthermore, comparisons between DVPPSP with TP were presented in the present study. The findings indicate that DVPPSP is a feasible and safe procedure and could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas, with a better metabolic function and QoL after surgery.
DVPPSP is a feasible and safe procedure. It could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas, with a better metabolic function and QoL after surgery.
The DVPPSP is a parenchyma-sparing procedure and could be an alternative to TP for low-grade neoplasms arising from the body and tail region but across the neck region of the pancreas.
The present study explored a new surgical technique so called “duodenum and ventral pancreas preserving subtotal pancreatectomy” as a choice of treatment for low-grade pancreatic neoplasms, such as IPMN, neuroendocrine tumors and pseudo-papillary tumors. The results showed DVPPSP was superior to total pancreatectomy by shorter operative time, better postoperative pancreatic function and better quality of life. But there was no detail pathological examination information of surgical specimens and follow-up data about tumor recurrence in the study. AS mentioned in the result of this article, why the rate of postoperative recurrence of IPMN was so high, 2 out of 6 for DVPPSP and 5 out of 11.
Manuscript source: Unsolicited manuscript
P-Reviewer: Zhang CW S-Editor: Qi Y L-Editor: E-Editor:
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Zhang CW S- Editor: Qi Y L- Editor: A
E- Editor: Ma YJ
| 1. | Faitot F, Gaujoux S, Barbier L, Novaes M, Dokmak S, Aussilhou B, Couvelard A, Rebours V, Ruszniewski P, Belghiti J. Reappraisal of pancreatic enucleations: A single-center experience of 126 procedures. Surgery. 2015;158:201-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Briggs CD, Mann CD, Irving GR, Neal CP, Peterson M, Cameron IC, Berry DP. Systematic review of minimally invasive pancreatic resection. J Gastrointest Surg. 2009;13:1129-1137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Hüttner FJ, Koessler-Ebs J, Hackert T, Ulrich A, Büchler MW, Diener MK. Meta-analysis of surgical outcome after enucleation versus standard resection for pancreatic neoplasms. Br J Surg. 2015;102:1026-1036. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 4. | Chua TC, Yang TX, Gill AJ, Samra JS. Systematic Review and Meta-Analysis of Enucleation Versus Standardized Resection for Small Pancreatic Lesions. Ann Surg Oncol. 2016;23:592-599. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Bilimoria KY, Talamonti MS, Tomlinson JS, Stewart AK, Winchester DP, Ko CY, Bentrem DJ. Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors: analysis of 3851 patients. Ann Surg. 2008;247:490-500. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 260] [Cited by in F6Publishing: 285] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 6. | Sauvanet A. Intraductal papillary mucinous neoplasms of the pancreas: indication, extent, and results of surgery. Surg Oncol Clin N Am. 2008;17:587-606, ix. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Benhaim R, Oussoultzoglou E, Saeedi Y, Mouracade P, Bachellier P, Lang H. Pancreatic metastasis from clear cell renal cell carcinoma: outcome of an aggressive approach. Urology. 2015;85:135-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Thayer SP, Fernández-del Castillo C, Balcom JH, Warshaw AL. Complete dorsal pancreatectomy with preservation of the ventral pancreas: a new surgical technique. Surgery. 2002;131:577-580. [PubMed] [Cited in This Article: ] |
| 9. | Beger HG, Rau BM, Gansauge F, Poch B. Duodenum-preserving subtotal and total pancreatic head resections for inflammatory and cystic neoplastic lesions of the pancreas. J Gastrointest Surg. 2008;12:1127-1132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Klempa I, Spatny M, Menzel J, Baca I, Nustede R, Stöckmann F, Arnold W. [Pancreatic function and quality of life after resection of the head of the pancreas in chronic pancreatitis. A prospective, randomized comparative study after duodenum preserving resection of the head of the pancreas versus Whipple’s operation]. Chirurg. 1995;66:350-359. [PubMed] [Cited in This Article: ] |
| 11. | Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3282] [Cited by in F6Publishing: 3393] [Article Influence: 178.6] [Reference Citation Analysis (0)] |
| 12. | Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1771] [Cited by in F6Publishing: 2043] [Article Influence: 120.2] [Reference Citation Analysis (0)] |
| 13. | Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1411] [Cited by in F6Publishing: 1660] [Article Influence: 97.6] [Reference Citation Analysis (0)] |
| 14. | Sakamoto Y, Nagai M, Tanaka N, Nobori M, Tsukamoto T, Nokubi M, Suzuki Y, Makuuchi M. Anatomical segmentectomy of the head of the pancreas along the embryological fusion plane: a feasible procedure? Surgery. 2000;128:822-831. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Heidt DG, Burant C, Simeone DM. Total pancreatectomy: indications, operative technique, and postoperative sequelae. J Gastrointest Surg. 2007;11:209-216. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Schmidt CM, Glant J, Winter JM, Kennard J, Dixon J, Zhao Q, Howard TJ, Madura JA, Nakeeb A, Pitt HA. Total pancreatectomy (R0 resection) improves survival over subtotal pancreatectomy in isolated neck margin positive pancreatic adenocarcinoma. Surgery. 2007;142:572-578; discussion 578-580. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | Watanabe Y, Ohtsuka T, Matsunaga T, Kimura H, Tamura K, Ideno N, Aso T, Miyasaka Y, Ueda J, Takahata S. Long-term outcomes after total pancreatectomy: special reference to survivors’ living conditions and quality of life. World J Surg. 2015;39:1231-1239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Sahora K, Fernández-del Castillo C, Dong F, Marchegiani G, Thayer SP, Ferrone CR, Sahani DV, Brugge WR, Warshaw AL, Lillemoe KD. Not all mixed-type intraductal papillary mucinous neoplasms behave like main-duct lesions: implications of minimal involvement of the main pancreatic duct. Surgery. 2014;156:611-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Yang M, Zeng L, Zhang Y, Su AP, Yue PJ, Tian BL. Surgical treatment and clinical outcome of nonfunctional pancreatic neuroendocrine tumors: a 14-year experience from one single center. Medicine (Baltimore). 2014;93:e94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Yu P, Cheng X, Du Y, Yang L, Xu Z, Yin W, Zhong Z, Wang X, Xu H, Hu C. Solid Pseudopapillary Neoplasms of the Pancreas: a 19-Year Multicenter Experience in China. J Gastrointest Surg. 2015;19:1433-1440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 21. | Uehara H, Ishikawa O, Ikezawa K, Kawada N, Inoue T, Takakura R, Takano Y, Tanaka S, Takenaka A. A natural course of main duct intraductal papillary mucinous neoplasm of the pancreas with lower likelihood of malignancy. Pancreas. 2010;39:653-657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Takada T, Yasuda H, Uchiyama K, Hasegawa H. Duodenum-preserving pancreatoduodenostomy. A new technique for complete excision of the head of the pancreas with preservation of biliary and alimentary integrity. Hepatogastroenterology. 1993;40:356-359. [PubMed] [Cited in This Article: ] |
| 23. | Scatton O, Sauvanet A, Cazals-Hatem D, Vullierme MP, Ruszniewski P, Belghiti J. Dorsal pancreatectomy: an embryology-based resection. J Gastrointest Surg. 2006;10:434-438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Correa-Gallego C, Brennan MF, Dʼangelica M, Fong Y, Dematteo RP, Kingham TP, Jarnagin WR, Allen PJ. Operative drainage following pancreatic resection: analysis of 1122 patients resected over 5 years at a single institution. Ann Surg. 2013;258:1051-1058. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 116] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 25. | Strobel O, Cherrez A, Hinz U, Mayer P, Kaiser J, Fritz S, Schneider L, Klauss M, Büchler MW, Hackert T. Risk of pancreatic fistula after enucleation of pancreatic tumours. Br J Surg. 2015;102:1258-1266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M; International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584-591. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2435] [Cited by in F6Publishing: 2372] [Article Influence: 338.9] [Reference Citation Analysis (1)] |
| 27. | White R, D’Angelica M, Katabi N, Tang L, Klimstra D, Fong Y, Brennan M, Allen P. Fate of the remnant pancreas after resection of noninvasive intraductal papillary mucinous neoplasm. J Am Coll Surg. 2007;204:987-993; discussion 993-995. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 128] [Cited by in F6Publishing: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 28. | Chari ST, Yadav D, Smyrk TC, DiMagno EP, Miller LJ, Raimondo M, Clain JE, Norton IA, Pearson RK, Petersen BT. Study of recurrence after surgical resection of intraductal papillary mucinous neoplasm of the pancreas. Gastroenterology. 2002;123:1500-1507. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 401] [Cited by in F6Publishing: 334] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 29. | Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183-197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1714] [Cited by in F6Publishing: 1540] [Article Influence: 128.3] [Reference Citation Analysis (0)] |
| 30. | Marchegiani G, Mino-Kenudson M, Ferrone CR, Morales-Oyarvide V, Warshaw AL, Lillemoe KD, Castillo CF. Patterns of Recurrence After Resection of IPMN: Who, When, and How? Ann Surg. 2015;262:1108-1114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 31. | Kim SC, Park KT, Lee YJ, Lee SS, Seo DW, Lee SK, Kim MH, Jang SJ, Byun JH, Han DJ. Intraductal papillary mucinous neoplasm of the pancreas: clinical characteristics and treatment outcomes of 118 consecutive patients from a single center. J Hepatobiliary Pancreat Surg. 2008;15:183-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Emerson RE, Randolph ML, Cramer HM. Endoscopic ultrasound-guided fine-needle aspiration cytology diagnosis of intraductal papillary mucinous neoplasm of the pancreas is highly predictive of pancreatic neoplasia. Diagn Cytopathol. 2006;34:457-462. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Epelboym I, Winner M, DiNorcia J, Lee MK, Lee JA, Schrope B, Chabot JA, Allendorf JD. Quality of life in patients after total pancreatectomy is comparable with quality of life in patients who undergo a partial pancreatic resection. J Surg Res. 2014;187:189-196. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 34. | Chan DC, Fan YM, Lin CK, Chen CJ, Chen CY, Chao YC. Roux-en-Y reconstruction after distal gastrectomy to reduce enterogastric reflux and Helicobacter pylori infection. J Gastrointest Surg. 2007;11:1732-1740. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Keck T, Adam U, Makowiec F, Riediger H, Wellner U, Tittelbach-Helmrich D, Hopt UT. Short- and long-term results of duodenum preservation versus resection for the management of chronic pancreatitis: a prospective, randomized study. Surgery. 2012;152:S95-S102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 36. | Zheng Z, Xiang G, Tan C, Zhang H, Liu B, Gong J, Mai G, Liu X. Pancreaticoduodenectomy versus duodenum-preserving pancreatic head resection for the treatment of chronic pancreatitis. Pancreas. 2012;41:147-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Lü WP, Shi Q, Zhang WZ, Cai SW, Jiang K, Dong JH. A meta-analysis of the long-term effects of chronic pancreatitis surgical treatments: duodenum-preserving pancreatic head resection versus pancreatoduodenectomy. Chin Med J (Engl). 2013;126:147-153. [PubMed] [Cited in This Article: ] |