Published online Apr 7, 2017. doi: 10.3748/wjg.v23.i13.2424
Peer-review started: November 13, 2016
First decision: December 29, 2016
Revised: January 14, 2017
Accepted: February 17, 2017
Article in press: February 17, 2017
Published online: April 7, 2017
To present clinical characteristics, diagnosis and treatment strategies in elderly patients with biliary diseases.
A total of 289 elderly patients with biliary diseases were enrolled in this study. The clinical data relating to these patients were collected in our hospital from June 2013 to May 2016. Patient age, disease type, coexisting diseases, laboratory examinations, surgical methods, postoperative complications and therapeutic outcomes were analyzed.
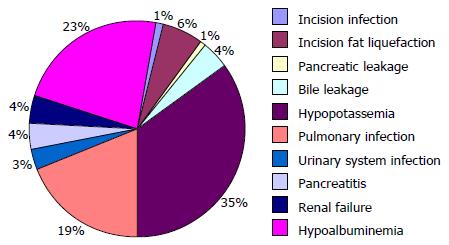
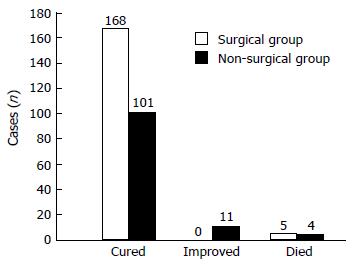
The average age of the 289 patients with biliary diseases was 73.9 ± 8.5 years (range, 60-102 years). One hundred and thirty-one patients (45.3%) had one of 10 different biliary diseases, such as gallbladder stones, common bile duct stones, and cholangiocarcinoma. The remaining patients (54.7%) had two types of biliary diseases. One hundred and seventy-nine patients underwent 9 different surgical treatments, including pancreaticoduodenectomy, radical resection of hilar cholangiocarcinoma and laparoscopic cholecystectomy. Ten postoperative complications occurred with an incidence of 39.3% (68/173), and hypopotassemia showed the highest incidence (33.8%, 23/68). One hundred and sixteen patients underwent non-surgical treatments, including anti-infection, symptomatic and supportive treatments. The cure rate was 97.1% (168/173) in the surgical group and 87.1% (101/116) in the non-surgical group. The difference between these two groups was statistically significant (χ2 = 17.227, P < 0.05).
Active treatment of coexisting diseases, management of indications and surgical opportunities, appropriate selection of surgical procedures, improvements in perioperative therapy, and timely management of postoperative complications are key factors in enhancing therapeutic efficacy in elderly patients with biliary diseases.
Core tip: With global prolongation of life expectancy, biliary diseases in elderly patients appear to be common and multifaceted. The purpose of this study was to determine the clinical characteristics and treatment strategies in elderly patients with biliary diseases in order to improve diagnosis and treatment. Active treatment of coexisting diseases, management of indications and surgical opportunities, appropriate selection of surgical procedures, improvements in perioperative therapy, and timely management of postoperative complications are key factors in enhancing therapeutic efficacy in elderly patients with biliary diseases.
- Citation: Zhang ZM, Liu Z, Liu LM, Zhang C, Yu HW, Wan BJ, Deng H, Zhu MW, Liu ZX, Wei WP, Song MM, Zhao Y. Therapeutic experience of 289 elderly patients with biliary diseases. World J Gastroenterol 2017; 23(13): 2424-2434
- URL: https://www.wjgnet.com/1007-9327/full/v23/i13/2424.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i13.2424
With global prolongation of life expectancy, the incidence of diseases in the aging population has increased. Since 1999, biliary diseases in elderly patients have become common and multifaceted in China, with a morbidity rate of 8%-11%[1].
Due to lowered stress response, an increase in coexisting diseases, rapid progression, and poor surgical tolerance, the risk of surgery for biliary diseases in elderly patients has increased[2,3]. In particular, a subset of elderly patients may be at higher risk of developing postoperative complications and increased mortality due to the loss of physiological function and physical reserves[4,5]. Therefore, there is an unmet clinical need to characterize biliary diseases in elderly patients, in order to improve diagnosis and treatment for these diseases[6-10].
In the present study, the clinical data of 289 elderly patients with biliary diseases admitted to our hospital over the past 3 years were summarized and analyzed.
A prospective study of 289 elderly patients with biliary diseases, aged 60-102 years, including 129 males (44.6%) and 160 females (55.4%), was conducted in the Department of General Surgery, Beijing Electric Power Hospital, State Grid Corporation of China, Capital Medical University from June 2013 to May 2016.
The inclusion criterion was a diagnosis of biliary disease in elderly patients. According to surgical indications or contraindications, patients were randomly assigned to the surgical group and the non-surgical group.
The exclusion criterion was patients who were voluntarily discharged from hospital due to refusal to cooperate with the assigned group therapy.
The study was approved by the Ethics Committee of Beijing Electric Power Hospital, State Grid Corporation of China, Capital Medical University, Beijing, China.
Following admission, blood samples were obtained from all patients for laboratory examinations, including routine blood test, high sensitivity C-reactive protein (hs-CRP) level[11,12], liver function, tumor markers, and blood clotting function.
Prior to treatment, all patients were examined by B ultrasound, computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP) to determine the presence of gallbladder or bile duct stones, inflammation or tumor. Double-layer structure of gallbladder wall revealed by B ultrasound suggested the existence of acute suppurative and gangrenous cholecystitis. Stones, inflammation, tumors of the gallbladder and bile duct, and thickness of the gallbladder wall can be determined by CT scanning[11]. MRCP helps to identify stones and obstruction of intrahepatic and extrahepatic bile ducts[13].
Based on the patient’s condition, electrocardiography (ECG), dynamic ECG, echocardiography, neck vascular ultrasound, head magnetic resonance angiography, and head and neck CT angiography were also performed[14,15].
According to the individual patient’s status, appropriate surgical procedures were selected, including pancreaticoduodenectomy, radical resection of hilar cholangiocarcinoma, and laparoscopic cholecystectomy (LC).
Non-surgical treatment strategies included, but were not limited to, anti-infection, symptomatic and supportive treatments.
SPSS 18.0 was used for statistical analysis[16]. The data from laboratory tests were expressed as mean ± SD, using the Student’s t-test for comparisons between the surgical and non-surgical groups. The rate (%) or constituent ratio was used for count data related to the distribution of age, disease types and coexisting diseases, surgical procedures, postoperative complications and therapeutic efficacy, and the χ2 test was used for comparisons between two groups. A P value < 0.05 was considered statistically significant.
The age of the 289 patients with biliary diseases ranged from 60 to 102 years, with an average age of 73.9 ± 8.5 years.
In the surgical group, the average age of patients was 72.1 ± 8.2 years, ranging from 60 to 95 years. The maximum age of patients undergoing open surgery was 95 years, and was 86 years for patients undergoing LC.
In the non-surgical group, the age of the patients ranged from 60 to 102 years, with an average age of 76.5 ± 8.2 years.
There was a significant difference in the age distribution between the two groups (P < 0.05), as shown in Table 1.
| Age (yr) | Surgical group | Non-surgical group | χ2 | P value |
| 60-69 | 75 (43.4) | 25 (21.6) | 23.376 | 0.000 |
| 70-79 | 64 (37.0) | 42 (36.2) | ||
| 80-89 | 30 (17.3) | 45 (38.8) | ||
| 90-99 | 4 (2.3) | 3 (2.6) | ||
| ≥ 100 | 0 (0.0) | 1 (0.9) | ||
| Total | 173 (100.0) | 116 (100.0) |
The 289 patients had 1 or 2 types of 10 different biliary diseases, including gallbladder stones, common bile duct stones, and cholangiocarcinoma (Table 2).
| Type of disease | Surgical group | Non-surgical group | χ2 | P value |
| Gallbladder stones | 133 (36.8) | 66 (32.7) | 0.308 | 0.016 |
| Common bile duct stones | 41 (11.4) | 23 (11.4) | ||
| Hepatolithiasis | 4 (1.1) | 7 (3.5) | ||
| Chronic cholecystitis | 36 (10.0) | 14 (6.9) | ||
| Acute cholecystitis | 92 (25.5) | 67 (33.2) | ||
| Gallbladder polyps | 8 (2.2) | 0 (0.0) | ||
| Acute cholangitis | 16 (4.4) | 16 (7.9) | ||
| Biliary pancreatitis | 15 (4.2) | 3 (1.5) | ||
| Biliary tract tumors | 12 (3.3) | 3 (1.5) | ||
| Gallbladder carcinoma | 4 (1.1) | 3 (1.5) |
One hundred and thirty-one (45.3%) patients had one type of biliary disease, and 158 (54.7%) patients had two types of biliary diseases. There was a significant difference in the distribution of types of disease (P < 0.05) in the surgical group compared with the non-surgical group (Table 2). However, there was no significant difference in the proportion of disease types (P > 0.05) between the two groups (Table 3).
| Group | n | One type of disease | Two types of diseases | χ2 | P value |
| Surgical | 173 | 71 (41.0) | 102 (59.0) | 3.198 | 0.074 |
| Non-surgical | 60 (51.7) | 56 (48.3) |
Among the 289 patients, 223 (77.2%) had 1-6 types of 13 various coexisting diseases, such as hypertension, coronary heart disease (CHD), and diabetes. Of these patients, 128 (57.4%) were in the surgical group, and 95 (42.6%) were in the non-surgical group. There was no significant difference between the two groups (P > 0.05; Table 4).
| Type of coexisting disease | Surgical group | Non-surgical group | χ2 | P value |
| Coronary heart disease | 40 (14.7) | 28 (13.5) | 17.526 | 0.131 |
| Atrial fibrillation | 8 (2.9) | 1 (0.5) | ||
| Hypertension | 84 (30.8) | 55 (26.4) | ||
| Diabetes | 33 (12.1) | 22 (10.6) | ||
| Renal insufficiency | 1 (0.4) | 5 (2.4) | ||
| Chronic bronchitis with emphysema | 5 (1.8) | 9 (4.3) | ||
| Portal hypertension | 3 (1.1) | 0 (0.0) | ||
| Pulmonary infection | 7 (2.6) | 10 (4.8) | ||
| Hypoalbuminemia | 9 (3.3) | 9 (4.3) | ||
| Anemia | 8 (2.9) | 5 (2.4) | ||
| Electrolyte disorder | 21 (7.7) | 21 (10.1) | ||
| Cerebral infarction | 30 (11.0) | 28 (13.5) | ||
| Hepatic insufficiency | 24 (8.8) | 15 (7.2) |
Using the t-test, it was found that the white blood cell count, percentage of neutrophils, prothrombin time and international normalized ratio at admission were significantly decreased (P < 0.05), whereas hemoglobin, albumin and total serum bilirubin were significantly increased in the surgical group compared with the non-surgical group (P < 0.05). There were no differences in the other test parameters between the two groups (P > 0.05; Table 5).
| Item | Surgical group, n = 173 | Non-surgical group, n = 116 | t | P value |
| Routine blood | ||||
| WBC (× 109/L) | 8.54 ± 4.77 | 10.41 ± 5.58 | -3.054 | 0.002a |
| N% | 71.94 ± 14.81 | 79.45 ± 13.55 | -4.450 | 0.000a |
| Hb (g/L) | 127.41 ± 20.44 | 121.00 ± 20.06 | 2.631 | 0.009a |
| hs-CRP (mg/L) | 50.02 ± 76.60 | 52.48 ± 58.76 | -0.288 | 0.774 |
| Liver function | ||||
| ALT (U/L) | 70.17 ± 103.96 | 94.13 ± 139.50 | -1.573 | 0.117 |
| AST (U/L) | 71.32 ± 115.81 | 105.00 ± 190.88 | -1.696 | 0.092 |
| TP (g/L) | 62.65 ± 8.33 | 62.06 ± 8.94 | -0.553 | 0.581 |
| Alb (g/L) | 36.59 ± 5.92 | 35.16 ± 5.75 | 2.030 | 0.043a |
| TB (μmol/L) | 51.74 ± 103.87 | 34.33 ± 37.06 | 2.021 | 0.044a |
| DB (μmol/L) | 21.99 ± 39.50 | 15.85 ± 23.37 | 1.659 | 0.098 |
| Tumor marker | ||||
| CA19-9 (U/mL) | 340.19 ± 1317.16 | 896.95 ± 6346.89 | -0.880 | 0.380 |
| CEA (ng/mL) | 2.76 ± 4.13 | 142.66 ± 1283.35 | -1.005 | 0.318 |
| Blood clotting function | ||||
| APTT (s) | 32.49 ± 5.20 | 32.59 ± 7.56 | -0.124 | 0.901 |
| PT (s) | 11.61 ± 1.38 | 12.12 ± 1.54 | -2.739 | 0.007a |
| INR | 1.05 ± 0.13 | 1.09 ± 0.14 | -2.318 | 0.021a |
| FIB (g/L) | 3.63 ± 1.21 | 3.69 ± 0.90 | -0.449 | 0.654 |
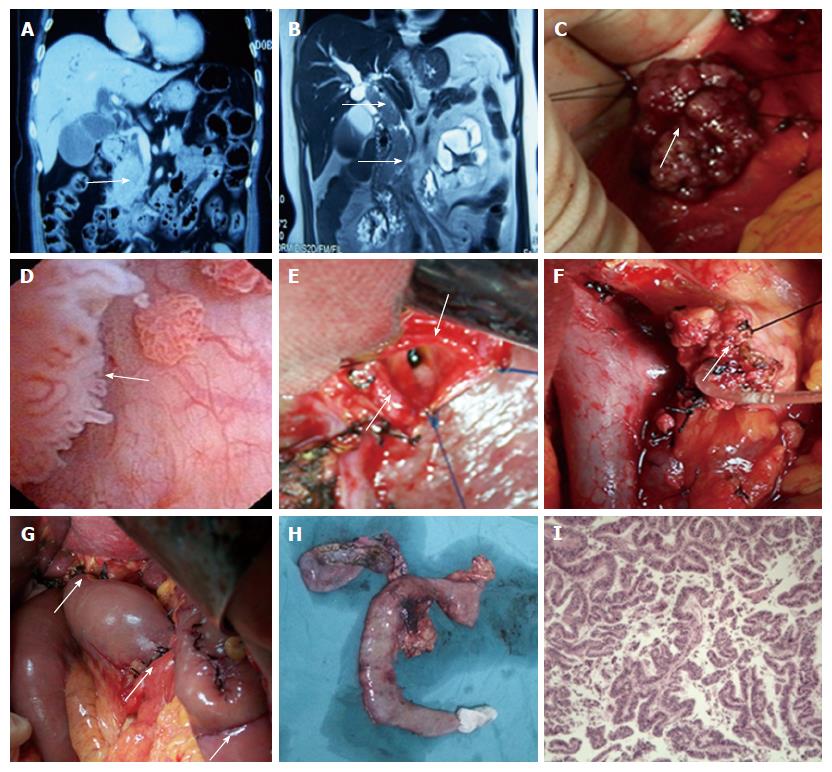
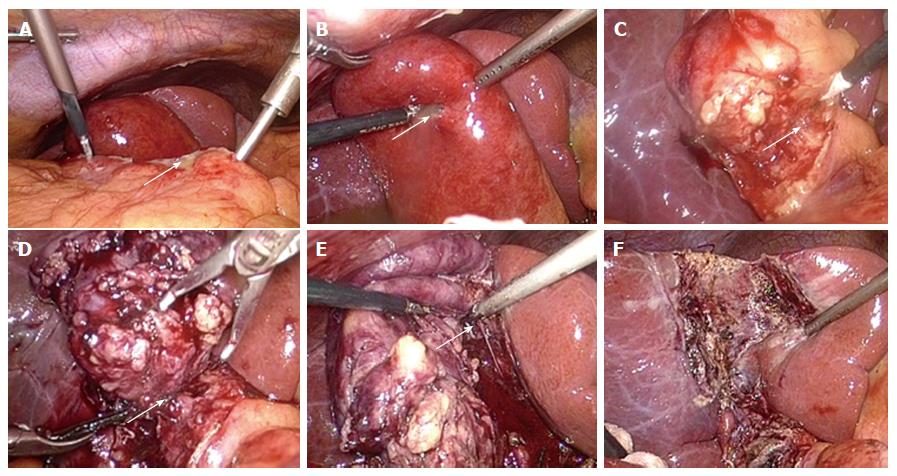
One hundred and seventy-three patients underwent surgical treatment with 1 of 9 different surgical procedures (Table 6), including pancreaticoduodenectomy (Figure 1), radical resection of hilar cholangiocarcinoma, and LC (Figure 2). Of these patients, 105 underwent simple LC, 7 of which were LC plus endoscopic sphincterotomy (EST) or endoscopic papillary balloon dilation (EPBD)[17-19]. The success rate was 100%, and none of the patients required conversion to laparotomy.
| Surgical procedure | n (%) |
| Pancreaticoduodenectomy | 6 (3.5) |
| Radical resection of hilar cholangiocarcinoma | 6 (3.5) |
| Radical resection of gallbladder carcinoma | 4 (2.3) |
| Hepatectomy | 4 (2.3) |
| Open cholecystectomy (OC) | 6 (3.5) |
| OC + common bile duct exploration + T-tube | 21 (12.1) |
| OC + transcystic common bile duct exploration | 14 (8.1) |
| Laparoscopic cholecystectomy (LC) | 105 (60.7) |
| LC + endoscopic sphincterotomy or endoscopic papillary balloon dilation | 7 (4.0) |
| Total | 173 (100.0) |
Ten types of postoperative complications were recorded, including pulmonary infection, hypopotassemia, incision fat liquefaction and others, with an incidence of 39.3% (68/173). Of these complications, hypopotassemia had the highest incidence (33.8%, 23/68), followed by hypoalbuminemia (22.1%), and pulmonary infection (19.1%) (Figure 3).
Among these 289 elderly patients, 269 (93.1%) patients were cured, 11 (3.8%) patients improved, and 9 patients (3.1%) died.
In the surgical group, 168 patients were cured, with a cure rate of 97.1% (168/173). Five patients died at 4, 6, 18, 31 and 100 d after surgery, with 3 who died due to acute myocardial infarction (AMI), 1 due to pulmonary embolism, and 1 due to multiple organ failure. The mortality rate was 2.9% in the surgical group (5/173).
In the non-surgical group, 101 patients were cured, with a cure rate of 87.1% (101/116), and 11 patients improved, with a rate of 9.5% (11/116). Four patients died due to multiple organ failure at 5, 6, 6 and 10 d after admission, resulting in a mortality rate of 3.4% (4/116).
A significant difference in the therapeutic effects between the surgical group and the non-surgical group was observed using the χ2 test (χ2 = 17.227, P < 0.05; Figure 4).
It is known that elderly people have a reduced response to stress, can be insensitive to pain, and have reduced abdominal muscle strength. In elderly patients with acute cholecystitis, acute suppurative cholangitis or other biliary diseases, clinical manifestations and pathological changes are often poorly correlated. These patients typically show mild symptoms, but have severe pathological alterations[20].
Due to decreased defense in the body, lower tension in the gallbladder wall, and difficulty in removing biliary stones, patients can have stones lodged in the neck of the gallbladder under stimulating conditions, e.g., a fatty diet. This can lead to an increase in internal pressure in the gallbladder, causing secondary infection and acute suppurative cholecystitis. In addition, small artery sclerosis in the gallbladder wall can result in an insufficient blood supply which can cause necrotic perforation of the gallbladder, biliary peritonitis, and even toxic shock. Therefore, elderly patients have the characteristics of acute onset and rapid progression of diseases.
Due to reduced immune function, increased incidence of biliary tract tumors and difficult early diagnosis in the elderly, the occurrence of jaundice may cause severe damage to vital organs and the immune system. Thus, elderly patients have a low surgical resection rate, an increase in postoperative complications and high mortality.
In this study, we found that 289 elderly patients had 1-2 types of 10 different biliary diseases. Of these patients, 45.3% had one type of biliary disease, and 54.7% had two types of biliary diseases. These findings indicated that many elderly patients have multiple biliary tract diseases.
It has been reported that morbidity due to coexisting diseases in elderly patients with biliary diseases is as high as 65%-90%[21]. From our current study, we found that 77.2% of patients had 1-6 types of 13 coexisting diseases, such as hypertension, CHD and diabetes. The incidence of coexisting diseases in the surgical group was 57.4%, and was 42.6% in the non-surgical group. No significant difference in coexisting diseases was observed between the two groups. Our study indicated that by actively managing coexisting diseases, surgery in elderly patients with biliary diseases is safe and feasible[22].
If hypertension coexists with biliary diseases[23-25], perioperative hypertension can enhance bleeding during surgery, induce myocardial ischemia, AMI, stroke, renal failure and other complications. It was recommended by the Anesthesiology Society of the Chinese Medical Association in 2014 that preoperative blood pressure should be maintained below 140/90 mmHg. Some researchers have also suggested that preoperative blood pressure should be below 135/85 mmHg, and remain stable for 1-2 wk. It is noteworthy that in the case of non-emergency surgery, patients should cease to use reserpine and anti-hypertensive drug No. 0 and switch to other anti-hypertensive drugs 7 d prior to surgery, as it is possible that use of these drugs can cause catecholamine depletion in the peripheral sympathetic nerve endings, which makes it difficult to improve and maintain blood pressure when low blood pressure occurs during surgery.
If patients with biliary diseases also have CHD[26-28], preoperative ECG, dynamic ECG and echocardiography should be performed before surgery. If cardiac dysfunction or arrhythmia can be controlled by drugs, and the ejection fraction is more than 60% with better cardiac compensatory function, surgical treatment can be considered. If patients have a history of cardiac dysfunction, surgery can only be performed when the illness has been stable for 1 mo. In patients with a history of AMI, surgery should only be performed when the illness has been stable for at least 6 mo. In the case of AMI, the blood levels of cardiac Troponin I (cTnI), brain-type natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP)[29-31] should be evaluated to determine the severity of myocardial injury and heart failure. If the patient has a history of bradycardia, a cardiac pacemaker should be implanted before surgery.
If patients with biliary diseases also have an old cerebral infarction[32-34], neck vascular ultrasound, head magnetic vascular imaging, or head and neck CT angiography should be performed. Carotid artery stenosis should be less than 50%, and pre-, intra- and post-operative blood pressure should be kept constant to avoid large fluctuations. This preventive measurement can effectively reduce the incidence of perioperative cerebral infarction and mortality.
In patients with coexisting diabetes[35,36], surgical stress can cause disorders of glucose metabolism and insulin resistance, and even produce ketone bodies or ketoacidosis. Therefore, the use of oral hypoglycemic agents and intermediate- or long-acting insulin should be stopped and switched to regular insulin. The expert consensus for the perioperative management of blood glucose, proposed by the Anesthesiology Society of the Chinese Medical Association in 2014, suggested that preoperative blood glucose should be below 10 mmol/L[35]. In addition, sustained high glucose blood levels can benefit the growth of bacteria, lower immune function, and result in abnormal neutrophil function with reduced phagocytosis. Antibiotics should be administered to prevent infection prior to surgery.
In elderly patients with biliary diseases combined with coexisting diseases, it is essential to manage indications and surgical opportunities.
In elderly patients with cholecystolithiasis, surgery can be determined based on the size of stones, gallbladder function, history of biliary colic, and whether the disease is complicated by cholangitis or pancreatitis. Surgery should be performed as soon as possible to avoid increased surgical risk due to increased patient age, disease progression and other coexisting diseases.
For patients with choledocholithiasis, surgery can be determined based on the size and number of stones and diameter of the common bile duct. Surgery should be carried out as soon as possible[37].
In patients with biliary tract tumors, surgery should be based on the site of obstruction, the degree of invasion and presence of distant metastasis. When favorable, surgery should be performed as early as possible, in order to improve quality of life and extend life expectancy[38].
In patients with acute cholangitis, conservative treatment should be actively considered in order to change emergency surgery to scheduled surgery as early as possible[39]. However, in elderly patients with acute obstructive suppurative cholangitis or acute gangrenous cholecystitis, emergency surgery should be performed as soon as possible to prevent the likely complications of sepsis and even toxic shock[40-42].
Our laboratory tests showed that the white blood cell count, percentage of neutrophils, prothrombin time and international normalized ratio at admission were significantly decreased (P < 0.05), whereas the levels of hemoglobin, albumin and total serum bilirubin were significantly increased in the surgical group compared with the non-surgical group (P < 0.05). These results suggested that the management of indications and surgical opportunities can significantly reduce surgical risk, and avoid unnecessary surgery, especially emergency surgery. Although the results of serum hs-CRP was not significantly different between the two groups (P > 0.05), dynamic monitoring of changes in hs-CRP may result in important reference values[11,12] for assessing the progression of acute cholecystitis and in choosing a suitable time window for surgery.
The choice of surgical procedure for biliary diseases in the elderly is crucial. It is important to avoid a long disease process or even a second operation following conservative surgery. On the other hand, the increased surgical risk due to aggressive surgery should also be prevented. For example, conservative surgery of acute gangrenous cholecystitis, such as percutaneous cholecystostomy[43,44], an alternative treatment for resolving acute inflammation, is theoretically suitable for patients in poor general condition, with a serious illness, unstable blood pressure during surgery, and other special circumstances. However, percutaneous cholecystostomy should be avoided for the reasons mentioned above. In our treatment group, none of the patients underwent percutaneous cholecystostomy.
Aggressive surgery, such as LC, should be selected with caution in patients with poor heart and pulmonary function before surgery, especially in the presence of emphysema. If LC must be performed, intraoperative pneumoperitoneum pressure should be controlled to below 10 mmHg to reduce the impact of pneumoperitoneum on heart and pulmonary function. There is no definitive view on the upper age limit for patients undergoing LC. The oldest patients were a 96-year-old reported by Lee et al[10] and a 102-year-old reported in China[45]. In our study, 112 patients underwent LC (including 7 patients who underwent LC + EST/EPBD)[46,47], with a success rate of 100%, and none of the patients were converted to laparotomy. The key to success is management of indications and the opportunity to perform LC.
It is important to skillfully separate inflammatory edema and adhesions in the neck of the gallbladder using a suction device, and to ligate or suture the enlarged, thickened and merged sheet-like cystic duct with silk thread during surgery. If necessary, removing the subtotal gallbladder wall and cauterizing the residual gallbladder mucosa can help to avoid bleeding in the gallbladder bed and increased surgery time.
Strengthen the function of the heart, lungs, kidneys and other important organs: In elderly patients with biliary diseases, it is important to frequently monitor ECG, central venous pressure, and urine volume. When necessary, the amount of urine per h should be recorded, and used as a guideline for the infusion volume and speed to prevent heart failure and pulmonary edema caused by excessive and fast infusion. Patients should be encouraged to take a deep breath, expectorate and change position, to maintain an unobstructed respiratory tract and to prevent respiratory tract infection. These measures can help to attenuate postoperative pulmonary atelectasis and pneumonia[48,49].
In patients with coexisting CHD, the serum levels of BNP, cTnI, myoglobin and creatine kinase isoenzyme MB should be monitored to identify heart failure and/or AMI. In patients with acute heart failure, besides the selective administration of digitalis and other positive inotropic drugs, appropriate use of diuretics can promote the discharge of absorbed interstitial fluid. In addition, the administration of a small dose of dopamine (0.5-2.0 μg/kg per min) can expand the renal and mesenteric vessels, increase renal blood flow and glomerular filtration rate, and then increase urinary output mainly by acting on dopamine receptors; the administration of a medium dose of dopamine (2.0-10.0 μg/kg per min) can directly act on β1 receptors, leading to an increase in myocardial contraction and cardiac output.
In patients with coexisting hypertension[50], besides the use of nitroglycerin and other antihypertensive drugs, increased blood pressure induced by pain[51] should be carefully monitored and, when necessary, analgesics should be administered or an analgesic pump used.
In patients with coexisting diabetes, blood glucose levels may fluctuate shortly after surgery due to the stress response, vasoactive drugs and other factors. Therefore, maintaining postoperative blood glucose at 6.0-10.0 mmol/L may reduce the incidence of postoperative complications[35].
Strengthen postoperative nutritional support: In elderly patients with biliary diseases, multiple coexisting diseases and poor physical condition, supplementation with glucose and vitamins, milk fat, amino acids, albumin and other nutritional support should be given after surgery. When necessary, total parenteral nutrition should be administered. During postoperative fasting, the necessary basic calorie count should be maintained at 25-30 kcal/kg per day. In patients undergoing major surgery, the calorie count should be increased by 30%-40%, and the ratio of calories to nitrogen should be kept at 120-150 kcal:1 g.
Maintain water, electrolyte and acid-base balance: In elderly patients with biliary diseases, an electrolyte imbalance can occur due to preoperative and postoperative fasting, the stress response caused by surgery, postoperative gastrointestinal decompression and biliary drainage. Therefore, various electrolytes should be supplied to maintain water, electrolyte and acid-base balance.
In addition, elderly patients often have a long history of aspirin administration. Due to its role in anti-platelet aggregation, the use of aspirin may interfere with normal coagulation function during the perioperative period. However, discontinuation of aspirin before surgery remains controversial[52,53]. We recommend discontinuation of aspirin 7-10 d prior to elective surgery in order to avoid the increased risk of surgery-related bleeding, given that the lifespan of platelets is reported to be 7 to 10 d[54]. If necessary, such as after coronary artery bypass surgery, low molecular weight heparin can be used as a substitute. In the case of emergency surgery, fibrinogen, prothrombin complex and plasma should be used to antagonize possible intraoperative and postoperative coagulopathy.
In elderly patients with biliary diseases, postoperative complications are common due to decreased defense capability, reduced immune function and coexisting diseases.
We identified 10 different postoperative complications in our study cohort, including pulmonary infection, hypopotassemia, incision fat liquefaction and others, with an incidence rate of 39.3% (68/173). Hypopotassemia (33.8%) showed the highest incidence, followed by hypoalbuminemia (22.1%) and pulmonary infection (19.1%). Hypopotassemia should be actively treated, and if necessary, potassium can be pumped into the blood vessels using a micro-infusion pump.
In order to prevent and treat postoperative pulmonary infection, patients should be asked to routinely inhale an aerosol, ensure early ambulation, maintain oral health care, and be tested by regular sputum culture to identify bacterial or fungal infections. If shortness of breath and difficult expectoration occur, the patient should be ventilated as soon as possible and respiratory secretions removed to maintain adequate ventilation. One should never wait until the emergence of respiratory failure before considering the use of a ventilator. In addition, it is necessary to prevent inhalation-induced pulmonary infection due to vomiting and aspiration caused by hypotonia of the lower esophageal sphincter.
Surgical treatment in elderly patients with biliary disease is safe and feasible[55-59]. According to the patient’s condition, active treatment of coexisting diseases, management of indications and surgical opportunities, appropriate selection of surgical procedures, improvements in perioperative therapy and timely management of postoperative complications are key factors in improving therapeutic efficacy in elderly patients with biliary diseases[60-62].
We thank Professor Yu-Min Zhang (Department of Anatomy, Physiology and Genetics, Uniformed Services University of the Health Sciences, United States) for critical reading of the manuscript.
With global prolongation of life expectancy, biliary diseases in elderly patients are common and multifaceted.
The purpose of this study was to determine the clinical characteristics and different treatment strategies for biliary diseases in elderly patients, in order to improve the diagnosis and treatment of biliary diseases in these patients.
Active treatment of coexisting diseases, management of indications and surgical opportunities, appropriate selection of surgical procedures, improved perioperative therapy and timely management of postoperative complications are key factors in enhancing therapeutic efficacy in elderly patients with biliary diseases.
Surgical treatment in elderly patients with biliary diseases is safe and feasible.
Biliary diseases in the elderly: Biliary diseases in elderly patients aged over 60 years.
The article studied an adequate sample size of elderly patients with biliary disease. A positive point of the study is that all patients underwent the same protocol and conducts. Currently, there is a more aggressive trend towards the surgical treatment of these patients based on data from the recent literature, using better imaging and endoscopic methods for diagnosis and surgical techniques.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sipahi AM S- Editor: Ma YJ L- Editor: Filipodia E- Editor: Zhang FF
| 1. | Zhang ZM, Song MM, Liu Z, Zhang C, Liu LM, Yu HW, Wan BJ, Liu ZX, Zhu MW, Wei WP. Clinical effect and analysis of laparoscopic cholecystectomy in elderly patients with acute calculous cholecystitis. Zhonghua Puwaike Shoushuxue Zazhi (Electronic Edition). 2016;10:466-468. [DOI] [Cited in This Article: ] |
| 2. | Pavlidis TE, Marakis GN, Symeonidis N, Psarras K, Ballas K, Rafailidis S, Sakantamis AK. Considerations concerning laparoscopic cholecystectomy in the extremely elderly. J Laparoendosc Adv Surg Tech A. 2008;18:56-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Tucker JJ, Yanagawa F, Grim R, Bell T, Ahuja V. Laparoscopic cholecystectomy is safe but underused in the elderly. Am Surg. 2011;77:1014-1020. [PubMed] [Cited in This Article: ] |
| 4. | Wagner D, Büttner S, Kim Y, Gani F, Xu L, Margonis GA, Amini N, Kamel IR, Pawlik TM. Clinical and morphometric parameters of frailty for prediction of mortality following hepatopancreaticobiliary surgery in the elderly. Br J Surg. 2016;103:e83-e92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901-908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1356] [Cited by in F6Publishing: 1370] [Article Influence: 97.9] [Reference Citation Analysis (0)] |
| 6. | Aprea G, Rocca A, Salzano A, Sivero L, Scarpaleggia M, Ocelli P, Amato M, Bianco T, Serra R, Amato B. Laparoscopic single site (LESS) and classic video-laparoscopic cholecystectomy in the elderly: A single centre experience. Int J Surg. 2016;33 Suppl 1:S1-S3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Han SJ, Lee TH, Kang BI, Choi HJ, Lee YN, Cha SW, Moon JH, Cho YD, Park SH, Kim SJ. Efficacy and Safety of Therapeutic Endoscopic Retrograde Cholangiopancreatography in the Elderly Over 80 Years. Dig Dis Sci. 2016;61:2094-2101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Fuks D, Duhaut P, Mauvais F, Pocard M, Haccart V, Paquet JC, Millat B, Msika S, Sielezneff I, Scotté M. A retrospective comparison of older and younger adults undergoing early laparoscopic cholecystectomy for mild to moderate calculous cholecystitis. J Am Geriatr Soc. 2015;63:1010-1016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Haltmeier T, Benjamin E, Inaba K, Lam L, Demetriades D. Early versus delayed same-admission laparoscopic cholecystectomy for acute cholecystitis in elderly patients with comorbidities. J Trauma Acute Care Surg. 2015;78:801-807. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Lee SI, Na BG, Yoo YS, Mun SP, Choi NK. Clinical outcome for laparoscopic cholecystectomy in extremely elderly patients. Ann Surg Treat Res. 2015;88:145-151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Ambe PC, Papadakis M, Zirngibl H. A proposal for a preoperative clinical scoring system for acute cholecystitis. J Surg Res. 2016;200:473-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Beliaev AM, Marshall RJ, Booth M. C-reactive protein has a better discriminative power than white cell count in the diagnosis of acute cholecystitis. J Surg Res. 2015;198:66-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Adam V, Bhat M, Martel M, da Silveira E, Reinhold C, Valois E, Barkun JS, Barkun AN. Comparison Costs of ERCP and MRCP in Patients with Suspected Biliary Obstruction Based on a Randomized Trial. Value Health. 2015;18:767-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Almutairi A, Sun Z, Poovathumkadavi A, Assar T. Dual Energy CT Angiography of Peripheral Arterial Disease: Feasibility of Using Lower Contrast Medium Volume. PLoS One. 2015;10:e0139275. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Paul J, Bauer RW, Maentele W, Vogl TJ. Image fusion in dual energy computed tomography for detection of various anatomic structures--effect on contrast enhancement, contrast-to-noise ratio, signal-to-noise ratio and image quality. Eur J Radiol. 2011;80:612-619. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Yu H, Zheng X, Zhang Z. Mechanism of Roux-en-Y gastric bypass treatment for type 2 diabetes in rats. J Gastrointest Surg. 2013;17:1073-1083. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (2)] |
| 17. | Zhang ZM, Yuan HM, Zhang C. Strategy of laparoscopy and choledochoscopy or duodenoscopy for the treatment of cholecystolithiasis combined choledocholithiasis. Zhonghua Xiaohua Waike Zazhi. 2015;14:280-283. [DOI] [Cited in This Article: ] |
| 18. | Lv S, Fang Z, Wang A, Yang J, Zhu Y. One-Step LC and ERCP Treatment of 40 Cases with Cholelithiasis Complicated with Common Bile Duct Stones. Hepatogastroenterology. 2015;62:570-572. [PubMed] [Cited in This Article: ] |
| 19. | Tonozuka R, Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Umeda J. Efficacy and safety of endoscopic papillary large balloon dilation for large bile duct stones in elderly patients. Dig Dis Sci. 2014;59:2299-2307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Zhang ZM, Liu Z, Wei WP, Tian ZH, Zhang C, Liu LM, Yu HW, Wan BJ, Deng H, Xie CH. Experience in diagnosis and treatment of biliary diseases in 197 elderly patients. Fubu Waike. 2015;28:337-341, 370. [DOI] [Cited in This Article: ] |
| 21. | Ma JG, Bai YZ. Analysis of surgical treatment of elderly patients with biliary diseases over 80 years old. Ningxia Yixue Zazhi. 2004;26:164-165. [DOI] [Cited in This Article: ] |
| 22. | Grant PJ, Cohn SL, Jaffer AK, Smetana GW. Update in perioperative medicine 2011. J Gen Intern Med. 2011;26:1358-1363. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Lonjaret L, Lairez O, Minville V, Geeraerts T. Optimal perioperative management of arterial blood pressure. Integr Blood Press Control. 2014;7:49-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 24. | Sear JW. Perioperative control of hypertension: when will it adversely affect perioperative outcome? Curr Hypertens Rep. 2008;10:480-487. [PubMed] [Cited in This Article: ] |
| 25. | Marik PE, Varon J. Perioperative hypertension: a review of current and emerging therapeutic agents. J Clin Anesth. 2009;21:220-229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Hoeks SE, Poldermans D. European Society of Cardiology 2009 guidelines for preoperative cardiac risk assessment and perioperative cardiac management in noncardiac surgery: key messages for clinical practice. Pol Arch Med Wewn. 2010;120:294-299. [PubMed] [Cited in This Article: ] |
| 27. | Cinello M, Nucifora G, Bertolissi M, Badano LP, Fresco C, Gonano N, Fioretti PM. American College of Cardiology/American Heart Association perioperative assessment guidelines for noncardiac surgery reduces cardiologic resource utilization preserving a favourable clinical outcome. J Cardiovasc Med (Hagerstown). 2007;8:882-888. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | McDonald MA, Braga JR, Li J, Manlhiot C, Ross HJ, Redington AN. A randomized pilot trial of remote ischemic preconditioning in heart failure with reduced ejection fraction. PLoS One. 2014;9:e105361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Cocking S, Landman T, Benson M, Lord R, Jones H, Gaze D, Thijssen DH, George K. The impact of remote ischemic preconditioning on cardiac biomarker and functional response to endurance exercise. Scand J Med Sci Sports. 2016; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Gil Martínez P, Mesado Martínez D, Curbelo García J, Cadiñanos Loidi J. Amino-terminal pro-B-type natriuretic peptide, inferior vena cava ultrasound, and biolectrical impedance analysis for the diagnosis of acute decompensated CHF. Am J Emerg Med. 2016;34:1817-1822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Stienen S, Salah K, Eurlings LW, Bettencourt P, Pimenta JM, Metra M, Bayes-Genis A, Verdiani V, Bettari L, Lazzarini V. Targeting N-Terminal Pro-Brain Natriuretic Peptide in Older Versus Younger Acute Decompensated Heart Failure Patients. JACC Heart Fail. 2016;4:736-745. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Henriksson KM, Farahmand B, Åsberg S, Edvardsson N, Terént A. Comparison of cardiovascular risk factors and survival in patients with ischemic or hemorrhagic stroke. Int J Stroke. 2012;7:276-281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 33. | Costello CA, Campbell BC, Perez de la Ossa N, Zheng TH, Sherwin JC, Weir L, Hand P, Yan B, Desmond PM, Davis SM. Age over 80 years is not associated with increased hemorrhagic transformation after stroke thrombolysis. J Clin Neurosci. 2012;19:360-363. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Kwon HM, Lynn MJ, Turan TN, Derdeyn CP, Fiorella D, Lane BF, Montgomery J, Janis LS, Rumboldt Z, Chimowitz MI. Frequency, Risk Factors, and Outcome of Coexistent Small Vessel Disease and Intracranial Arterial Stenosis: Results From the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) Trial. JAMA Neurol. 2016;73:36-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 35. | Dhatariya K, Levy N, Hall GM. The impact of glycaemic variability on the surgical patient. Curr Opin Anaesthesiol. 2016;29:430-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Membership of the Working Party; Barker P, Creasey PE, Dhatariya K, Levy N, Lipp A, Nathanson MH, Penfold N, Watson B, Woodcock T. Peri-operative management of the surgical patient with diabetes 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2015;70:1427-1440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 122] [Cited by in F6Publishing: 123] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 37. | Lupinacci RM, Nadal LR, Rego RE, Dias AR, Marcari RS, Lupinacci RA, Farah JF. Surgical management of gallbladder disease in the very elderly: are we operating them at the right time? Eur J Gastroenterol Hepatol. 2013;25:380-384. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Zhang ZM, Xing HL, Yuan HM, Liu Kai, Zhu JP, Su YM, Guo JX, Jiang N, Zhang ZC. Diagnosis and treatment for advanced hilar cholangiocarcinoma: experience of 24 cases. Zhongguo Yixue Qianyan. 2008;2:134-138. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Riall TS, Adhikari D, Parmar AD, Linder SK, Dimou FM, Crowell W, Tamirisa NP, Townsend CM, Goodwin JS. The risk paradox: use of elective cholecystectomy in older patients is independent of their risk of developing complications. J Am Coll Surg. 2015;220:682-690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Minaga K, Kitano M, Imai H, Yamao K, Kamata K, Miyata T, Omoto S, Kadosaka K, Yoshikawa T, Kudo M. Urgent endoscopic ultrasound-guided choledochoduodenostomy for acute obstructive suppurative cholangitis-induced sepsis. World J Gastroenterol. 2016;22:4264-4269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 15] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Qin YS, Li QY, Yang FC, Zheng SS. Risk factors and incidence of acute pyogenic cholangitis. Hepatobiliary Pancreat Dis Int. 2012;11:650-654. [PubMed] [Cited in This Article: ] |
| 42. | Singh A, Feng Y, Mahato N, Li J, Wu C, Gong J. Role of high-mobility group box 1 in patients with acute obstructive suppurative cholangitis-induced sepsis. J Inflamm Res. 2015;8:71-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Jung WH, Park DE. Timing of Cholecystectomy after Percutaneous Cholecystostomy for Acute Cholecystitis. Korean J Gastroenterol. 2015;66:209-214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 44. | Hu YR, Pan JH, Tong XC, Li KQ, Chen SR, Huang Y. Efficacy and safety of B-mode ultrasound-guided percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy for acute cholecystitis in elderly and high-risk patients. BMC Gastroenterol. 2015;15:81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 45. | Ru HY, Yin WS, Zhuang SH. Clinical application of laparoscopic cholecystectomy in elderly patients. Wujing Houqin Xueyuan Xuebao. 2015;24:382-383. [DOI] [Cited in This Article: ] |
| 46. | Bostanci EB, Ercan M, Ozer I, Teke Z, Parlak E, Akoglu M. Timing of elective laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreaticography with sphincterotomy: a prospective observational study of 308 patients. Langenbecks Arch Surg. 2010;395:661-666. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 47. | ElGeidie AA, ElShobary MM, Naeem YM. Laparoscopic exploration versus intraoperative endoscopic sphincterotomy for common bile duct stones: a prospective randomized trial. Dig Surg. 2011;28:424-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 48. | Griffiths R, Beech F, Brown A, Dhesi J, Foo I, Goodall J, Harrop-Griffiths W, Jameson J, Love N, Pappenheim K. Peri-operative care of the elderly 2014: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2014;69 Suppl 1:81-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 101] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 49. | Peden CJ, Grocott MP. National Research Strategies: what outcomes are important in peri-operative elderly care? Anaesthesia. 2014;69 Suppl 1:61-69. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 50. | Lien SF, Bisognano JD. Perioperative hypertension: defining at-risk patients and their management. Curr Hypertens Rep. 2012;14:432-441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 51. | Aubrun F, Gazon M, Schoeffler M, Benyoub K. Evaluation of perioperative risk in elderly patients. Minerva Anestesiol. 2012;78:605-618. [PubMed] [Cited in This Article: ] |
| 52. | Cuellar JM, Petrizzo A, Vaswani R, Goldstein JA, Bendo JA. Does aspirin administration increase perioperative morbidity in patients with cardiac stents undergoing spinal surgery? Spine (Phila Pa 1976). 2015;40:629-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 53. | Gerstein NS, Schulman PM, Gerstein WH, Petersen TR, Tawil I. Should more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndrome. Ann Surg. 2012;255:811-819. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 129] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 54. | Wolf AM, Pucci MJ, Gabale SD, McIntyre CA, Irizarry AM, Kennedy EP, Rosato EL, Lavu H, Winter JM, Yeo CJ. Safety of perioperative aspirin therapy in pancreatic operations. Surgery. 2014;155:39-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 55. | Dubecz A, Langer M, Stadlhuber RJ, Schweigert M, Solymosi N, Feith M, Stein HJ. Cholecystectomy in the very elderly--is 90 the new 70? J Gastrointest Surg. 2012;16:282-285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 56. | Cocorullo G, Falco N, Tutino R, Fontana T, Scerrino G, Salamone G, Licari L, Gulotta G. Open versus laparoscopic approach in the treatment of abdominal emergencies in elderly population. G Chir. 2016;37:108-112. [PubMed] [Cited in This Article: ] |
| 57. | Ozkan Z, Gul E, Kanat BH, Gundogdu Z, Gonen AN, Yazar FM, Bozan MB, Erol F. Is Surgery Safe in Gallstone-Related Acute Diseases in Elderly Patients? J Coll Physicians Surg Pak. 2016;26:471-475. [PubMed] [Cited in This Article: ] |
| 58. | Zhou Y, Zhang Z, Wu L, Li B. A systematic review of safety and efficacy of hepatopancreatoduodenectomy for biliary and gallbladder cancers. HPB (Oxford). 2016;18:1-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 59. | Park SY, Chung JS, Kim SH, Kim YW, Ryu H, Kim DH. The safety and prognostic factors for mortality in extremely elderly patients undergoing an emergency operation. Surg Today. 2016;46:241-247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 60. | Zhang ZM, Wei WP, Liu Z, Tian ZH, Zhang C, Liu LM, Yu HW, Wan BJ, Liu ZX, Zhu MW. Opportunity of laparoscopic cholecystectomy in elderly patients with acute calculous cholecystitis. Zhonghua Puwaike Shoushuxue Zazhi (Electronic Edition). 2016;10:406-409. [DOI] [Cited in This Article: ] |
| 61. | Zhang ZM, Tian ZH, Yuan HM, Zhang Chong, Liu Z, Liu LM. Strategy of minimally invasive surgery for patients with intrahepatic and extrahepatic bile duct stones. Shijie Huaren Xiaohua Zazhi. 2016;24:3757-3763. [DOI] [Cited in This Article: ] [Cited by in CrossRef: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 62. | Teixeira JP, Ribeiro C, Pinho A, Graça L, Moreira LM, Maia JC. Laparoscopic cholecystectomy in acute cholecystitis in the elderly. Hepatogastroenterology. 2014;61:18-21. [PubMed] [Cited in This Article: ] |