Published online Jul 28, 2016. doi: 10.3748/wjg.v22.i28.6373
Peer-review started: April 1, 2016
First decision: May 12, 2016
Revised: May 25, 2016
Accepted: June 15, 2016
Article in press: June 15, 2016
Published online: July 28, 2016
Like the wars predating the First World War where human foot soldiers were deemed tools in the battlefield against an enemy, so too are the host immune cells of a patient battling a malignant gastric cancer. Indeed, the tumour microenvironment resembles a battlefield, where the patient’s immune cells are the defence against invading tumour cells. However, the relationship between different immune components of the host response to cancer is more complex than an “us against them” model. Components of the immune system inadvertently work against the interests of the host and become pro-tumourigenic while other components soldier on against the common enemy – the tumour cell.
Core tip: Many solid tumours are now being treated with immunotherapies and gastric cancer is no exception. Here we review the literature on molecular subtypes of gastric cancer and how they each have different immunological responses and hence may be differentially responsive to these immunotherapies. We emphasise that while treatment of gastric cancer may be benefited by immunotherapy we should try to target this based on molecular and immunological signatures of the individual patient. This will match the ideal therapy to the specific patient and is a step forward on the pathos precision medicine.
- Citation: Wang M, Busuttil RA, Pattison S, Neeson PJ, Boussioutas A. Immunological battlefield in gastric cancer and role of immunotherapies. World J Gastroenterol 2016; 22(28): 6373-6384
- URL: https://www.wjgnet.com/1007-9327/full/v22/i28/6373.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i28.6373
“Advances in medicine and agriculture have saved vastly more lives than have been lost in all the wars in history.”
Carl Sagan
Gastric cancer (GC) continues to be a significant cause of mortality globally, being the third leading cause of cancer-related death[1]. While there have been advances in the outcomes of many solid tumours[2-4], gastric adenocarcinoma, the predominant form of GC, has not shown the same degree of improvements in survival[5], despite aggressive multi-modality treatment[6]. Potent new immunotherapies induce host immune-mediated destruction of malignant cells and offer new hope in the battle against GC. Here we explore some of the positive and negative characteristics of the host immune response to the presence of a malignant cell.
It is incumbent on us to be aware that all cancers are not equal. The Cancer Genome Atlas (TCGA) Network has produced a landmark study using integrative genomics to molecularly phenotype four subtypes of GC[7] that are to some extent related to histological features of the disease. Previous studies suggest the histology of the tumour according to Lauren classification may explain some of the molecular heterogeneity of GC[8] but the host immune response to the cancer may also account for some of the differences. The TCGA study describes two particular subtypes both of which consist of predominantly intestinal type tumours that had a significant immunological association: the Epstein-Barr virus (EBV) subtype accounted for about 9%[7] of the GCs profiled and were characterised by a strong immune signature and; the MSI (Microsatellite Instability) subtype (22% of cancers in this study[7]), which had a high mutational load, also had a significant immune signature. While the other two GC subtypes [GS (Genomically Stable and predominantly diffuse) subtype and CIN (Chromosomal Instability subtype which are primarily intestinal in histology)] may have a host immunological response, this differed to the two immunogenic subtypes[7]. Here we explore some of the features of the immune response to GC to try and reconcile some of the clinical observations, such as differences in survival and also to explore the utility of immunotherapies for this particular cancer.
Currently, the immune context of GC comprises both anti- and pro-tumoural immune responses. The immune system includes inter-linked innate and adaptive arms, both have cellular and soluble effectors. The innate immune system cells respond to foreign antigens that are recognised via pathogen recognition receptors (PRR) for pathogen-associated molecular patterns (PAMPs) or danger associated molecular patterns (DAMPs)[9]. The PRR can recognise PAMPs or DAMPs derived from a diverse array of viruses, bacteria or tumour cells. The innate immune system is evolutionarily conserved and performs an immune surveillance role via cells [macrophages, dendritic cells (DCs), neutrophils and natural killer (NK) cells] and soluble factors such as, the complement system. There is considerable cross-talk between cells within the innate immune system as well as cross-talk with cells of the adaptive arm, for example, tissue resident DCs induce an adaptive immune response through antigen presentation[10]. The adaptive immune system recognizes and eliminates antigens; conventional T cells recognise antigen as peptide-major histocompatibility complex (MHC) on virus infected cells or tumour cells, whereas B cells recognise conformational antigen. Priming of naïve T and B cells to antigens occurs in the tissue draining lymph node of a particular organ. Effective antigen recognition and co-stimulation activates the antigen-specific T or B cell driving their proliferation and generation of effector and memory cells. Effector T cells traffic to the site of priming and participate in resolution of the threat/pathogen. Memory T cells reside in secondary lymphoid tissue (central memory), or the peripheral tissue (tissue resident memory cells) and can respond quickly to any future pathogen threat, termed “long term protective immunity”. In healthy individuals the immune system is remarkably effective at responding to and eradicating a diverse array of pathogen threats; however the immune system can be a double-edged sword in cancer, which has the ability to shape the immune response to facilitate tumour cell growth and survival rather than eliminating the tumour[11].
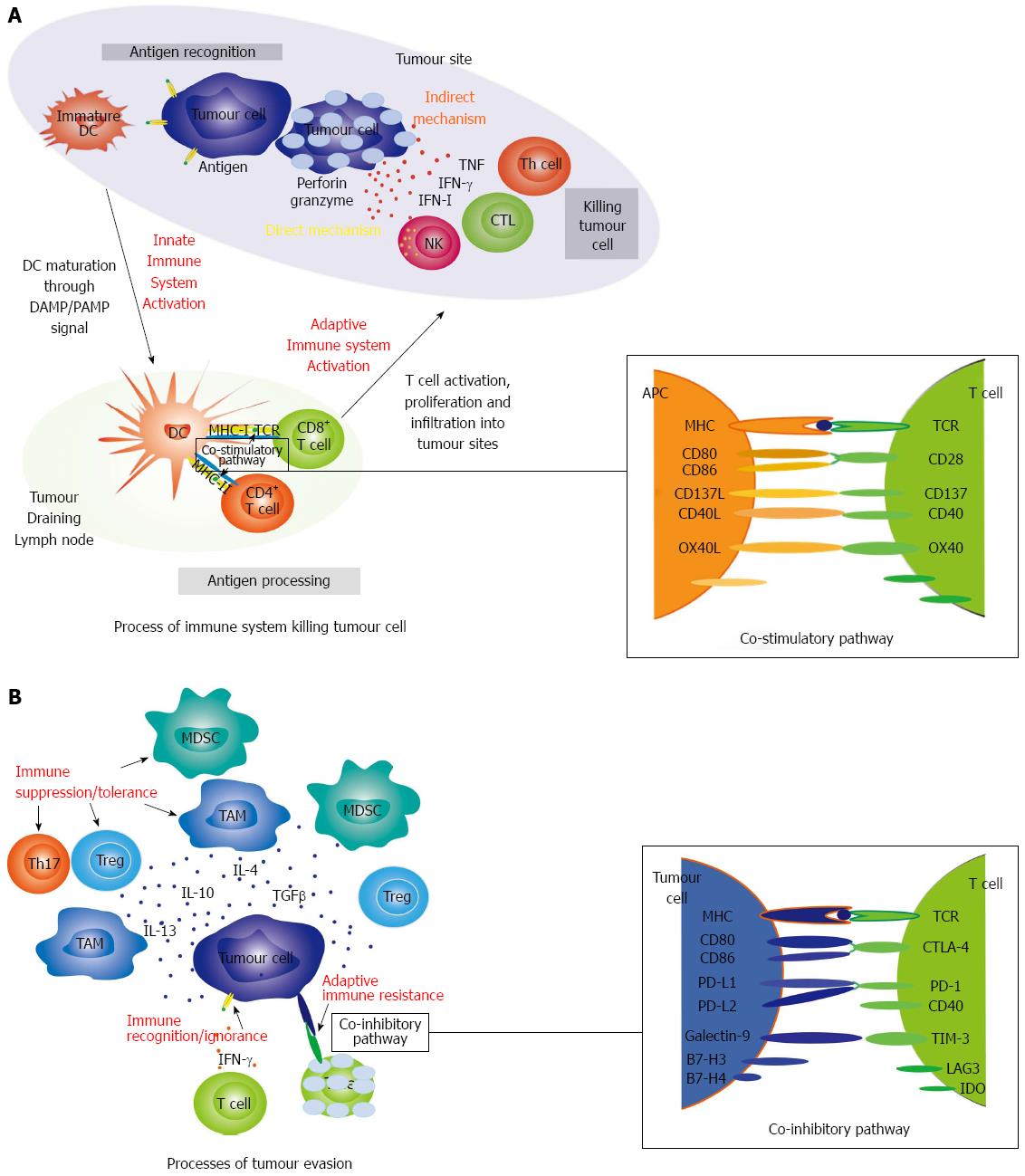
The immune system detects and eliminates tumour cells. This usually prevents cancer development through a process termed immune-surveillance[12,13]. Tumour-specific antigens (TSA) are antigens present only on tumour cells, while tumour-associated antigens (TAA) are antigens present on tumour cells as well as normal cells. Expression of TSA and TAA generally results from tumour-associated genetic mutations. Tumour-resident DCs constantly sample the microenvironment via endocytosis, they process the TSA or TAA as peptides and assemble them on MHC, either in the endoplasmic reticulum for MHC class I, or endosomes for MHC class II. The DC requires an activation signal, such as a DAMP or PAMP, in order to mature and subsequently increase peptide MHC expression levels. Activated DCs change chemokine receptor and adhesion molecule expression making them responsive to chemokines emanating from the tumour draining lymph node (TDLN). Having migrated to the TDLN, the mature DC presents TSA/TAA on MHC class I to CD8+ T cell, or on MHC class II to CD4+ T cells, priming an antigen-specific T cell response[14]. For successful activation, Cytotoxic T cells (CTLs) require two signals from antigen processing cells (APCs); (1) antigen presentation, T-cell receptor (TCR) binding to peptide-MHC class I molecules; and (2) co-stimulation, CD28 molecule on T cells binding to co-stimulatory molecules CD80 (B7-1) or CD86 (B7-2) on APCs. In the absence of signal 2, signal 1 induces immune tolerance to TAA/TSA. Signal 2 is only provided by mature DCs, as they express CD80/CD86 at higher levels. At this point, activated tumour-specific naïve T cells proliferate and form effector and memory T cells, as described for the pathogen response above. Tumour-specific CD8+ effector T cells, also termed CTLs, traffic from the TDLN to the tumour and attack tumour cells presenting cognate antigen, with the help of CD4+ helper T cells (Th cells), mainly Th1 cells. During the effector phase, T cells infiltrate the tumour (referred to as tumour infiltrating T lymphocytes or TILs) in response to chemokines, such as CX3CL1, CXCL9, CXCL10 and CCL5[15]. These TILs kill tumour cells by direct and indirect mechanisms. The direct mechanism utilises perforin and granzymes. Figure 1A outlines some of the aspects of antigen recognition, presentation and the effector immune cells (T cell and NK cell) killing of tumour cells. Tumour-specific CTL recognition of cognate antigen induces their activation and formation of an immune synapse (IS, a specialised molecular structure formed between a cytotoxic lymphocyte and a target cell) at the site of antigen recognition. Simultaneously, the CTL moves cytotoxic granules (containing perforin and granzymes) to the IS, these granules fuse with the CTL cell membrane and release their contents. Perforin polymerises and inserts into the tumour cell membrane forming a pore, this enables entry of granzyme B into the cytoplasm, which induces tumour cell apoptosis. Indirect mechanisms include secretion of cytokines including type I IFN, IFN-γ and TNF[16,17]. After clearance, surviving CD8+ T cells differentiate into T memory cells[18], which can retain anti-cancer properties and can enact faster and stronger anti-cancer immune response when they next encounter tumour cells.
Another cell type important in an early response to cancer is the NK cell. NK cells are part of the innate immune system that act non-specifically against tumour cells and can directly kill these cells. This type of anti-cancer immunity is reported in hematopoietic malignancies and solid tumours[19].
The “immune-editing” paradigm was proposed to explain how tumour cells influence the behaviour of innate and adaptive immune cells through an immunosuppression process to finally present as a clinical tumour[20]. The immune-editing mechanism, which is the most important process during immunosuppression, consists of three sequential phases: elimination, equilibrium, and escape[20-22]. During the elimination phase, the immune system destroys developing tumour cells. In the equilibrium phase, sufficient tumour cells survive the immune attack to maintain tumour size, but there is no obvious tumour progression. During this phase, the immune system sculpts the immunogenicity of genetically unstable tumour clones. Finally, in the escape phase immune resistant tumour clones emerge, proliferate and spread either locally or to distant sites.
Precisely how tumour cells evade the immune system (in the escape phase), as summarised in Figure 1B, is an area of active research, and can be broadly grouped into three main mechanisms including:
Immune recognition/ignorance: where tumour cells can control immune recognition via down-regulation of antigens and MHC molecules on the cell surface[23-25].
Immune suppression/tolerance: Where tumour-derived suppression mechanisms are driven via tumour-derived cytokines and influence the differentiation of immune effectors driving their functional polarization to suppressors. Immune suppressors include tumour associate macrophages (TAMs), myeloid-derived suppressor cells (MDSCs) and regulatory CD4+ T cells. Macrophages within the tumour microenvironment have been described as pro-tumourigenic as they support cancer initiation and progression, or anti-tumourigenic based on differentiation patterns into M1 or M2 subtypes[26,27]. M1 macrophages have a tumouricidal activity by producing pro-inflammatory cytokines, such as IL-1, IL-6, IL-23 and TNF. M2 macrophages possess a tumour-promoting capacity by producing IL-10 and TGF-β. TAMs frequently have a spectrum of differentiation and, through the balance of M1 and M2 macrophage subtypes in the tumour microenvironment, may influence aggressiveness of the tumour and prognosis of patients. There is generally a poor outcome if M2 macrophages predominate in the tumour microenvironment[28,29]. Tumour cells may also induce an M1 to M2 switch, mediated by TGF-β[30]. Several studies have identified an association with the density of TAMs in the microenvironment of GC and a poor outcome[31,32]. MDSCs are a group of activated but immature myeloid cells with strong immunosuppressive capacity that have been shown to support tumour cell growth, differentiation, and metastasis[33,34]. CD4+ T cell response to tumour-derived antigen in the context of TGF-β induces up-regulation of the key transcription factor (FoxP3) and regulatory T cells (Tregs) functional polarization. Tregs are powerful suppressors of the tumour-specific T cell responses (both CTL and effector CD4+ T cells) and can be found at increased numbers in patient TILs, both at the tumour margin and inside the tumour itself[35].
Adaptive immune resistance: where tumour cells can induce T cell inactivation through a process described as “adaptive immune resistance”[36]. When CTL’s recognise cognate antigens on tumour cells their effector mechanisms include secretion of IFN-γ, IFN-γ binding to tumour cell IFN-γR induces JAK-STAT signalling and up-regulation of tumour cell programmed death ligand-1 (PD-L1) expression. CTL recognition of antigen induces programmed death-1 (PD-1) expression. Binding of PD-L1 to its receptor PD-1 on T cells, delivers an inhibitory signal to the T cell IS and results in T cell paralysis. The over-arching result is tumour cell resistance to killing by T cells[36,37]. The molecules involved in the immune co-inhibitory pathways are called immune checkpoints. These molecules have an important normal physiological role, and are important in turning off the immune system once effective T cell effector function has been achieved (i.e., once antigen has been cleared). The checkpoint inhibitors include: PD-1 (also known as CD279) and its ligands PD-L1 (B7-H1; also known as CD274) and PD-L2 (B7-DC; also known as CD273); Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4, also known as CD152) and its ligands CD80 and CD86; T-cell immunoglobulin and mucin-domain containing-3 (TIM-3) and its ligand galectin-9; lymphocyte-activation gene 3 (LAG3, also known as CD223) and Indoleamine-pyrrole 2,3-dioxygenase (IDO). These pathways are discussed later as they have been transformed into successful immunotherapies in the war against cancer. Other components of the adaptive immune response are two subcategories of T cells, the Treg and Th17 cell. Tumour cells can induce Tregs, which in turn promote tumour progression by secreting TGF-β, as well as Th17 cells, which accelerate tumour progression by producing IL-17[38].
These are some of the physiological mechanisms that a tumour cell can exploit to survive, perpetuate and invade a host organism resulting in poor outcomes seen in many malignancies.
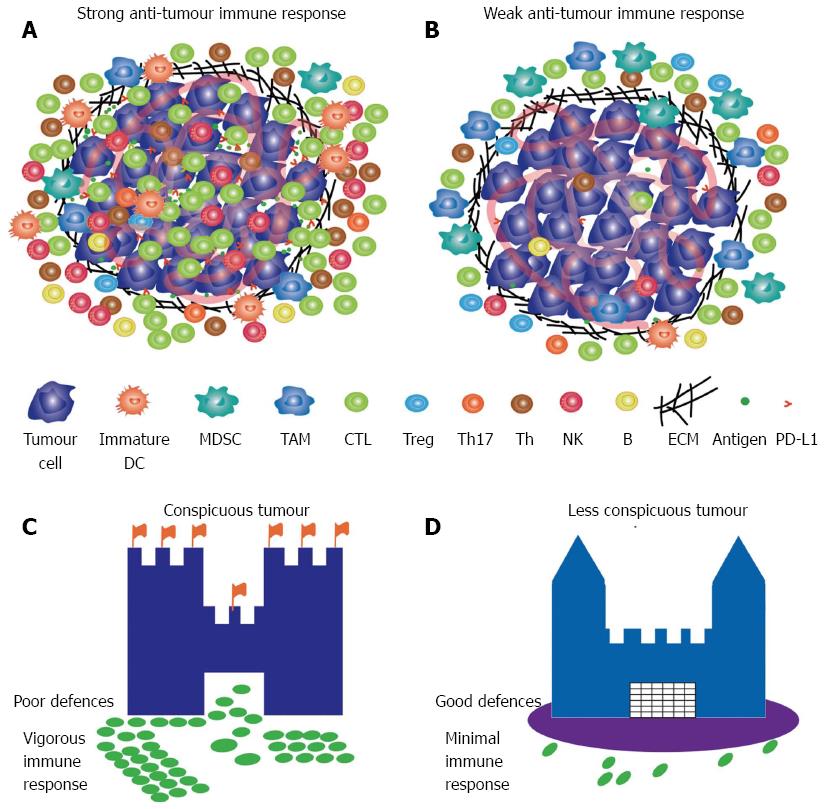
Integrated genomic analysis of GC showed that molecular subtypes have distinct signatures. The EBV and MSI subtypes have significant immune signatures (Figure 2A) compared to the CIN and GS subtypes (Figure 2B). It is recognised that MSI cancers result in increased tumour cell mutational load[39] and presentation of neo-antigens[40] resulting in an augmented host immune response with increased TILs[41-43], DCs and macrophages[44]. EBV-associated GC also has an increased density of TILs[41,45-47]. Despite a significant host immune response these tumours persist, likely due to immune escape mediated by over-expression of immune checkpoints, such as PD-L1 and PD-L2[7]. Llosa et al[48] found similar changes to the tumour microenvironment of MSI colorectal cancer. These MSI cancers showed up-regulation of immune checkpoints, such as PD-1, PD-L1, LAG-3, CTLA-4 and IDO. In colorectal cancer MSI-high specimens are often associated with high infiltration of CD3+, CD4+ and CD8+ cells and show more frequent infiltration by PD-1 positive intraepithelial lymphocytes compared to microsatellite stability samples[49]. Indeed, colorectal cancer is a good example of how the immunological reaction to the tumour has been used as a prognostic marker and may identify a group of cancers that can be targeted with specific immunotherapies[50,51]. The mechanisms for the robust immune response in the EBV subtype remain unclear, but are likely due to long term inflammation induced by the infection in the stomach[52].
An association between lymphocytic infiltration and survival in GC was first proposed over 100 years ago[53]. Since then numerous studies have shown an increased density of TILs is associated with favourable clinical outcomes in a variety of solid tumours[54-57], including GC[58]. This holds true for intratumoural B cells[42] and NK cells[59] in GC. However, GC expression of the checkpoint inhibitor PD-L1 is associated with poor clinical outcomes[60-66]. Tumour expression of PD-L1 is not universally a negative predictor as patients with ovarian cancer expressing high PD-1 (generally thought to be expressed by the immune cells) and PD-L1 levels in tumour cells as well as TILs having favourable prognosis[67]. These contrasting results are partially explained by methodological differences in the studies where most investigators report on the intra-tumoural immune component only and ignore the peri-tumoural context of the cancer or focus on particular components of the immune response in isolation and ignore the dynamic environment that is the tumour microenvironment. Importantly, another variable that is not factored in the GC literature is the molecular characteristics of the tumour cell itself. As described in the Asian Cancer Research Group study from Cristescu et al[68], tumours of the MSI subtype (similar to TCGA) have the best prognosis of the subtypes described in their study. Marrelli et al[69] confirm the favourable prognosis of MSI in non-cardia intestinal gastric tumours. Kim et al[70] investigated the type and density of TILs and macrophages in the MSI-high subgroup of GC and found that increased density of intra-tumoural CD8+ and FoxP3+ TILs was associated with a good prognosis. It was further shown that the balance of TILs and TAMs (M2-polarized macrophages) also showed favourable prognostic significance[71].
The immune system is an integral part of the tumour microenvironment and immune cell evasion by tumour cells has recently been highlighted as one of the hallmarks of cancer[11]. Promotion, or activation, of the immune system, referred to as “immunotherapy”, has also been proposed as an option for targeted treatment. Unlike chemotherapy, which uses potent drugs to eliminate tumour cells or control their growth, cancer immunotherapy involves boosting the immune system of a patient to eliminate or control a malignancy. Using the immune checkpoint inhibitors (ICIs), T-cells can be re-activated or maintained in an active state allowing them to recognize and eliminate tumour cells. Documented clinical responses of ICIs in a number of cancer types, especially in solid tumours, including melanoma, non-small cell lung cancer, renal cell carcinoma[2-4] have been reported and provide us with new anti-cancer strategies. The use of immunotherapy, especially the ICIs, for treating GC is still in its infancy with several clinical trials underway.
CTLA-4, one of the immune checkpoints, is expressed on the surface of T cells following recognition of antigen. T cell CTLA-4 has a higher affinity than CD28 for APC CD80/CD86. This transduces an inhibitory signal to T cells serving as a “brake” on T cell activation. Ipilimumab, an IgG1 antibody which blocks CTLA-4 activity, allows ongoing APC priming of antigen-specific T cells in the TDLN (i.e., brake removed). An additional proposed mechanism of ipilimumab action includes targeting of CTLA-4hi intra-tumoural Tregs tipping the balance of effector T cells: Treg in favour of an anti-tumour response. Ipilimumab was the first approved immune checkpoint therapy and has shown a survival benefit in advanced stage melanoma patients[72,73]. The repercussions of meddling with the physiologic processes governing immunity is an increase in a variety of immune related side effects, including skin lesions (rash, pruritus, and vitiligo), colitis, thyroiditis, hypophysitis, and hepatitis[74]. A clinical trial in GC patients with unresectable, locally advanced or metastatatic cancer following first line standard chemotherapy with a fluoropyrimidine/platinum combination (NCT01585987) has recently been completed however initial results are not promising with poorer PFS (secondary endpoint) in the ipilimumab treated group[75]. Tremelimumab, another anti-CTLA-4 monoclonal antibody, was investigated as a second-line treatment for patients with unselected metastatic gastric and oesophageal adenocarcinomas. The results were disappointing and among 18 recruited patients only one patient achieved a partial response[76].
A second immune checkpoint target is the PD-1/PD-L1 axis. PD-1 is present on the surface of activated T-cells, B-cells and monocytes whilst PD-L1 is found on the surface of tumour cells and antigen presenting cells (macrophages and DCs)[2]. Similarly PD-L2, expressed exclusively on DCs, is also a ligand for PD-1 and has been shown to inhibit T-cell activation, proliferation and cytokine production[77]. Checkpoint inhibitor antibodies directed to the PD-1/PD-L1 pathway are thought to largely rescue function of pre-existing tumour-specific TILs.
Anti-PD-1 (nivolumab, pembrolizumab) or anti-PD-L1 (MSB0010718C, BMS936559, MPDL3280A, Medi4736) agents are humanized monoclonal antibodies, which inhibit binding of PD-1 to PD-L1 and restore T cell activity. Due to promising results from initial clinical trials utilising these antibodies in melanoma and in other cancer types, they are currently being explored in GC. A phase I clinical trial (NCT01928394) using nivolumab in GC patients has been completed and initial results showed objective responses occurred in patients irrespective of PD-L1 status[78].
Pembrolizumab has been tested in GC patients selected based on immunohistochemical staining of PD-L1 (NCT01848834)[79,80] and initial results reported at ESMO 2014[79] with updated results presented at ASCO 2015[80]. Eligible patients had PD-L1 positive staining in stromal or ≥ 1% tumour nest cells. Based on these criteria this study observed a 40% rate of PD-L1 positive cancers and demonstrated manageable toxicity and promising antitumour activity in advanced GC[80]. When used in melanoma patients, a positive response was associated with expression of four specific immune signatures (presented as an abstract)[81]. These findings were recapitulated in the GC[82] patients suggesting that screening for expression of these signatures could be used as a method to best select patients who might benefit from this treatment. A large number of clinical trials testing these drugs in combination with standard chemotherapies are currently underway and have been reviewed in detail elsewhere[83].
Several anti-PD-L1 monoclonal antibodies, including Avelumab (MSB0010718C), Durvalumab (Medi4736) and Atezolizumab (MPDL3280A) and BMS936559, are under evaluation in digestive cancers, including GC[84]. GCs comprise only a small minority of the patients recruited to the early phase clinical trials currently underway and as such only limited data on their efficacy is currently available[85]. It is worth noting that therapeutic strategies should be carefully considered. Whilst targeting the PD-1/PD-L1 + PD-L2 checkpoint pathways should increase anti-tumour efficacy, this may come at the cost of increased “off tumour target” toxicity. Therapies targeting only PD-L1 whilst maintaining PD-L2 activity may result in decreased anti-tumour effects coupled with decreased toxicity. There are currently no PD-L2 specific inhibitors available.
Therapeutic strategies targeting both CTLA-4 and PD-1 in combination are currently being tested in GC in the hope of identifying synergistic effects. The CheckMate032 (NCT01928394) trial testing the effects of nivolumab as a sole agent, or in combination with ipilimumab in a variety of solid cancers, including GC, and in a refractory setting is currently recruiting. This combination has previously showed successful tumour regression in the setting of melanoma[86].
The molecular, genetic and immunological heterogeneity described by the TCGA highlights a need to stratify patients based on their likelihood of responding to different treatment options including immunotherapy. Despite this, many of the clinical trials described above recruited GC patients of all subtypes which, unfortunately may dilute out the potential positive effects of these therapies. EBV and MSI subtypes of GC are associated with a vigorous immunological reaction, as well as over-expression of immune checkpoints, highlighting these two subtypes of GC as particularly attractive candidates for immune checkpoint blockade, and indeed trials in these particular GC subtypes are underway.
The EBV subtype described by the TCGA[7] is characterised by a high prevalence of mutations in the PIK3CA suggesting a possible therapeutic role for PI3K inhibitors. This subtype is also associated with a high prevalence of DNA hypermethylation and amplifications in the genes CD274 and PDCD1LG2 which encode the immunosuppressive proteins PD-L1 and PDL-2, which highlights this subtype as an ideal candidate for immunotherapy[7,83]. A clinical phase II/III trial (NCT02488759, CheckMate358) plans to test the efficacy of nivolumab in subjects with virus- associated tumours including EBV-positive GC. This trial is currently in the recruitment phase. Given that most of these patients have concurrent immune infiltrate and harbour mutations in targetable genes, an adjuvant approach including a targeted therapy in conjunction with a PD-1 inhibitor such as pembrolizumab may be warranted. Such a treatment combination would need to be evaluated to ensure that the targeted therapy doesn’t directly inhibit immune effector cell signalling pathways.
The MSI TCGA GC subtype was characterised by high levels of microsatellite instability and elevated mutation rates[7]. Unsurprisingly gastrointestinal tumours that are MSI-H or mismatch repair deficiency, when compared to microsatellite stable tumours, have shown promising immune-related objective response rates (ORR; 40% vs 0%) and progression-free survival (PFS; 78% vs 11%) when treated with PD-1 inhibitor, pembrolizumab[87]. This emphasizes this subtype as a potential candidate for immunotherapy.
Genomic amplifications in receptor tyrosine kinases were a distinguishing feature of the CIN subtype as defined by TCGA[7]. Many of these are candidates for treatment with molecular targeted therapies. A phase I clinical trial testing the effects of Pembrolizumab in combination with ramucirumab (NCT02443324) is currently recruiting and may be particularly effective in this subgroup. This group was also enriched for TP53 mutations.
The GS TCGA subtype[7] (20% of all cases) comprised predominantly of tumours classified as diffuse GC, with poorer survival compared to the intestinal type GC, by the Lauren classification and was associated with mutations in CDH1 and RHOA genes as well as aneuploidy. At this stage it is unclear whether this subtype would benefit from existing immunotherapies and warrants specific investigation.
With the significant clinical benefits from immune checkpoint blockade drugs, novel opportunities are emerging for GC treatment. To improve effectiveness of GC immunotherapy, novel criteria based on different molecular and immunological subtypes to predict potential response and prognosis are needed. Galon et al[88,89] have established an “immunoscore” in colorectal cancer based on the number and location of CD3+ and CD8+ cells[90]. This type of classification could be useful in GC. While we have focused on the immune component of the tumour microenvironment we must not lose sight that GC remains heterogeneous and while we may co-opt the immune system in destroying some cancers others may have mechanisms of resistance to avoid this form of killing. Therefore combination therapies may be the way of the future and we will need to be cognizant of the ensuing toxicities these therapies may invoke. It is important to also recognize the microenvironmental and immunological impact of the more traditional chemotherapeutics[91]. Examples include oxaliplatin, a platinum drug used often in GC chemotherapy which induces immunogenic cell death and provides a release of tumour antigens[92].
In most communities GC is diagnosed late and subsequently has poor prognosis. There are now exciting new therapies that utilise the host’s immune system to fight back. However, data to date suggests we need to use these therapies judiciously to derive maximum benefit. GC is molecularly and immunologically heterogeneous, and this heterogeneity influences the tumour microenvironment in different ways. Returning to the battlefield analogy, the immunogenic or immune activating GC subtypes, EBV and MSI, are likely to be more conspicuous to the immune system by the expression of larger numbers of neo-antigens and other foreign epitopes that stimulate a vigorous immunological response that can be augmented by current therapies (Figure 2C), whereas the less immunogenic GCs, the CIN and GS subtypes, are more stealthy, with less antigen presentation providing a stronger defensive system against the host immune attack (Figure 2D). Like the battles in the wars of old, you need to choose your battlefield carefully and one of the key strategies, as enunciated by Sun Tzu, is to “know thy enemy”, which translates to understanding the molecular nature of the cancer you are treating.
Manuscript Source: Invited manuscript
Specialty Type: Gastroenterology and Hepatology
Country of Origin: Australia
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ciesielski M, Watari J S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18694] [Cited by in F6Publishing: 20838] [Article Influence: 2315.3] [Reference Citation Analysis (2)] |
| 2. | Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443-2454. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8900] [Cited by in F6Publishing: 9307] [Article Influence: 775.6] [Reference Citation Analysis (0)] |
| 3. | Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, Drake CG, Camacho LH, Kauh J, Odunsi K. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455-2465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5599] [Cited by in F6Publishing: 5891] [Article Influence: 490.9] [Reference Citation Analysis (0)] |
| 4. | Page DB, Postow MA, Callahan MK, Allison JP, Wolchok JD. Immune modulation in cancer with antibodies. Annu Rev Med. 2014;65:185-202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 358] [Cited by in F6Publishing: 394] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 5. | Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, Bannon F, Ahn JV, Johnson CJ, Bonaventure A. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385:977-1010. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1579] [Cited by in F6Publishing: 1613] [Article Influence: 179.2] [Reference Citation Analysis (0)] |
| 6. | Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric cancer: ESMO-ESSO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi57-vi63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 7. | Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4230] [Cited by in F6Publishing: 4299] [Article Influence: 429.9] [Reference Citation Analysis (2)] |
| 8. | Boussioutas A, Li H, Liu J, Waring P, Lade S, Holloway AJ, Taupin D, Gorringe K, Haviv I, Desmond PV. Distinctive patterns of gene expression in premalignant gastric mucosa and gastric cancer. Cancer Res. 2003;63:2569-2577. [PubMed] [Cited in This Article: ] |
| 9. | Palm NW, Medzhitov R. Pattern recognition receptors and control of adaptive immunity. Immunol Rev. 2009;227:221-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 501] [Cited by in F6Publishing: 496] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 10. | Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783-801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8061] [Cited by in F6Publishing: 8304] [Article Influence: 461.3] [Reference Citation Analysis (0)] |
| 11. | Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39812] [Cited by in F6Publishing: 42985] [Article Influence: 3306.5] [Reference Citation Analysis (4)] |
| 12. | Matsueda S, Graham DY. Immunotherapy in gastric cancer. World J Gastroenterol. 2014;20:1657-1666. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 64] [Cited by in F6Publishing: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Burnet FM. The concept of immunological surveillance. Prog Exp Tumor Res. 1970;13:1-27. [PubMed] [Cited in This Article: ] |
| 14. | Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245-252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10867] [Cited by in F6Publishing: 10541] [Article Influence: 405.4] [Reference Citation Analysis (0)] |
| 15. | Bindea G, Mlecnik B, Fridman WH, Pagès F, Galon J. Natural immunity to cancer in humans. Curr Opin Immunol. 2010;22:215-222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 133] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 16. | Thiery J, Keefe D, Boulant S, Boucrot E, Walch M, Martinvalet D, Goping IS, Bleackley RC, Kirchhausen T, Lieberman J. Perforin pores in the endosomal membrane trigger the release of endocytosed granzyme B into the cytosol of target cells. Nat Immunol. 2011;12:770-777. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 210] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 17. | Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H, Schlienger K, Liebman MN. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med. 2003;348:203-213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2457] [Cited by in F6Publishing: 2498] [Article Influence: 119.0] [Reference Citation Analysis (0)] |
| 18. | Radziewicz H, Uebelhoer L, Bengsch B, Grakoui A. Memory CD8+ T cell differentiation in viral infection: a cell for all seasons. World J Gastroenterol. 2007;13:4848-4857. [PubMed] [Cited in This Article: ] |
| 19. | Deng W, Gowen BG, Zhang L, Wang L, Lau S, Iannello A, Xu J, Rovis TL, Xiong N, Raulet DH. Antitumor immunity. A shed NKG2D ligand that promotes natural killer cell activation and tumor rejection. Science. 2015;348:136-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 186] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 20. | Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331:1565-1570. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3828] [Cited by in F6Publishing: 4142] [Article Influence: 318.6] [Reference Citation Analysis (0)] |
| 21. | Vesely MD, Kershaw MH, Schreiber RD, Smyth MJ. Natural innate and adaptive immunity to cancer. Annu Rev Immunol. 2011;29:235-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1312] [Cited by in F6Publishing: 1403] [Article Influence: 107.9] [Reference Citation Analysis (0)] |
| 22. | Mittal D, Gubin MM, Schreiber RD, Smyth MJ. New insights into cancer immunoediting and its three component phases--elimination, equilibrium and escape. Curr Opin Immunol. 2014;27:16-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 960] [Cited by in F6Publishing: 973] [Article Influence: 97.3] [Reference Citation Analysis (0)] |
| 23. | Bhatia A, Kumar Y. Cancer-immune equilibrium: questions unanswered. Cancer Microenviron. 2011;4:209-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Campoli M, Ferrone S. HLA antigen changes in malignant cells: epigenetic mechanisms and biologic significance. Oncogene. 2008;27:5869-5885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 285] [Cited by in F6Publishing: 301] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 25. | Ferrone S, Whiteside TL. Tumor microenvironment and immune escape. Surg Oncol Clin N Am. 2007;16:755-774, viii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3122] [Cited by in F6Publishing: 3589] [Article Influence: 256.4] [Reference Citation Analysis (0)] |
| 27. | Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, Gordon S, Hamilton JA, Ivashkiv LB, Lawrence T. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41:14-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3382] [Cited by in F6Publishing: 3978] [Article Influence: 397.8] [Reference Citation Analysis (0)] |
| 28. | Busuttil RA, George J, Tothill RW, Ioculano K, Kowalczyk A, Mitchell C, Lade S, Tan P, Haviv I, Boussioutas A. A signature predicting poor prognosis in gastric and ovarian cancer represents a coordinated macrophage and stromal response. Clin Cancer Res. 2014;20:2761-2772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | Ramanathan S, Jagannathan N. Tumor associated macrophage: a review on the phenotypes, traits and functions. Iran J Cancer Prev. 2014;7:1-8. [PubMed] [Cited in This Article: ] |
| 30. | Su S, Liu Q, Chen J, Chen J, Chen F, He C, Huang D, Wu W, Lin L, Huang W. A positive feedback loop between mesenchymal-like cancer cells and macrophages is essential to breast cancer metastasis. Cancer Cell. 2014;25:605-620. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 505] [Cited by in F6Publishing: 528] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 31. | Park JY, Sung JY, Lee J, Park YK, Kim YW, Kim GY, Won KY, Lim SJ. Polarized CD163+ tumor-associated macrophages are associated with increased angiogenesis and CXCL12 expression in gastric cancer. Clin Res Hepatol Gastroenterol. 2016;40:357-365. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 32. | Wu MH, Lee WJ, Hua KT, Kuo ML, Lin MT. Macrophage Infiltration Induces Gastric Cancer Invasiveness by Activating the β-Catenin Pathway. PLoS One. 2015;10:e0134122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Marvel D, Gabrilovich DI. Myeloid-derived suppressor cells in the tumor microenvironment: expect the unexpected. J Clin Invest. 2015;125:3356-3364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 657] [Cited by in F6Publishing: 758] [Article Influence: 84.2] [Reference Citation Analysis (0)] |
| 34. | Ugel S, De Sanctis F, Mandruzzato S, Bronte V. Tumor-induced myeloid deviation: when myeloid-derived suppressor cells meet tumor-associated macrophages. J Clin Invest. 2015;125:3365-3376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 349] [Cited by in F6Publishing: 405] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 35. | Savage PA, Malchow S, Leventhal DS. Basic principles of tumor-associated regulatory T cell biology. Trends Immunol. 2013;34:33-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 36. | Chen L, Han X. Anti-PD-1/PD-L1 therapy of human cancer: past, present, and future. J Clin Invest. 2015;125:3384-3391. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 842] [Cited by in F6Publishing: 1010] [Article Influence: 112.2] [Reference Citation Analysis (0)] |
| 37. | Park JJ, Omiya R, Matsumura Y, Sakoda Y, Kuramasu A, Augustine MM, Yao S, Tsushima F, Narazaki H, Anand S. B7-H1/CD80 interaction is required for the induction and maintenance of peripheral T-cell tolerance. Blood. 2010;116:1291-1298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 259] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 38. | Grivennikov SI, Wang K, Mucida D, Stewart CA, Schnabl B, Jauch D, Taniguchi K, Yu GY, Osterreicher CH, Hung KE. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature. 2012;491:254-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 888] [Cited by in F6Publishing: 957] [Article Influence: 87.0] [Reference Citation Analysis (0)] |
| 39. | Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, Bignell GR, Bolli N, Borg A, Børresen-Dale AL. Signatures of mutational processes in human cancer. Nature. 2013;500:415-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6762] [Cited by in F6Publishing: 6658] [Article Influence: 605.3] [Reference Citation Analysis (1)] |
| 40. | Rooney MS, Shukla SA, Wu CJ, Getz G, Hacohen N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell. 2015;160:48-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2009] [Cited by in F6Publishing: 2454] [Article Influence: 272.7] [Reference Citation Analysis (0)] |
| 41. | Chiaravalli AM, Feltri M, Bertolini V, Bagnoli E, Furlan D, Cerutti R, Novario R, Capella C. Intratumour T cells, their activation status and survival in gastric carcinomas characterised for microsatellite instability and Epstein-Barr virus infection. Virchows Arch. 2006;448:344-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 42. | Nosho K, Baba Y, Tanaka N, Shima K, Hayashi M, Meyerhardt JA, Giovannucci E, Dranoff G, Fuchs CS, Ogino S. Tumour-infiltrating T-cell subsets, molecular changes in colorectal cancer, and prognosis: cohort study and literature review. J Pathol. 2010;222:350-366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 358] [Cited by in F6Publishing: 380] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 43. | Phillips SM, Banerjea A, Feakins R, Li SR, Bustin SA, Dorudi S. Tumour-infiltrating lymphocytes in colorectal cancer with microsatellite instability are activated and cytotoxic. Br J Surg. 2004;91:469-475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 158] [Cited by in F6Publishing: 165] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 44. | Bauer K, Michel S, Reuschenbach M, Nelius N, von Knebel Doeberitz M, Kloor M. Dendritic cell and macrophage infiltration in microsatellite-unstable and microsatellite-stable colorectal cancer. Fam Cancer. 2011;10:557-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Haas M, Büttner M, Rau TT, Fietkau R, Grabenbauer GG, Distel LV. Inflammation in gastric adenocarcinoma of the cardia: how do EBV infection, Her2 amplification and cancer progression influence tumor-infiltrating lymphocytes? Virchows Arch. 2011;458:403-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 46. | Kuzushima K, Nakamura S, Nakamura T, Yamamura Y, Yokoyama N, Fujita M, Kiyono T, Tsurumi T. Increased frequency of antigen-specific CD8(+) cytotoxic T lymphocytes infiltrating an Epstein-Barr virus-associated gastric carcinoma. J Clin Invest. 1999;104:163-171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 47. | Akiba S, Koriyama C, Herrera-Goepfert R, Eizuru Y. Epstein-Barr virus associated gastric carcinoma: epidemiological and clinicopathological features. Cancer Sci. 2008;99:195-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 48. | Llosa NJ, Cruise M, Tam A, Wicks EC, Hechenbleikner EM, Taube JM, Blosser RL, Fan H, Wang H, Luber BS. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. 2015;5:43-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 889] [Cited by in F6Publishing: 1045] [Article Influence: 104.5] [Reference Citation Analysis (0)] |
| 49. | Gatalica Z, Snyder C, Maney T, Ghazalpour A, Holterman DA, Xiao N, Overberg P, Rose I, Basu GD, Vranic S. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomarkers Prev. 2014;23:2965-2970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 376] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 50. | Church SE, Galon J. Tumor Microenvironment and Immunotherapy: The Whole Picture Is Better Than a Glimpse. Immunity. 2015;43:631-633. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 51. | Mlecnik B, Bindea G, Angell HK, Maby P, Angelova M, Tougeron D, Church SE, Lafontaine L, Fischer M, Fredriksen T. Integrative Analyses of Colorectal Cancer Show Immunoscore Is a Stronger Predictor of Patient Survival Than Microsatellite Instability. Immunity. 2016;44:698-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 619] [Cited by in F6Publishing: 698] [Article Influence: 87.3] [Reference Citation Analysis (0)] |
| 52. | Raab-Traub N. Novel mechanisms of EBV-induced oncogenesis. Curr Opin Virol. 2012;2:453-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 53. | MacCarty WC, Mahle AE. Relation of differentiation and lymphocytic infiltration to postoperative longevity in gastric carcinoma. J Lab Clin Med. 1921;VI:473-480. [Cited in This Article: ] |
| 54. | Savas P, Salgado R, Denkert C, Sotiriou C, Darcy PK, Smyth MJ, Loi S. Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat Rev Clin Oncol. 2016;13:228-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 448] [Cited by in F6Publishing: 551] [Article Influence: 61.2] [Reference Citation Analysis (0)] |
| 55. | Baldan V, Griffiths R, Hawkins RE, Gilham DE. Efficient and reproducible generation of tumour-infiltrating lymphocytes for renal cell carcinoma. Br J Cancer. 2015;112:1510-1518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 56. | Wouters MC, Komdeur FL, Workel HH, Klip HG, Plat A, Kooi NM, Wisman GB, Mourits MJ, Arts HJ, Oonk MH. Treatment Regimen, Surgical Outcome, and T-cell Differentiation Influence Prognostic Benefit of Tumor-Infiltrating Lymphocytes in High-Grade Serous Ovarian Cancer. Clin Cancer Res. 2016;22:714-724. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 57. | Fortes C, Mastroeni S, Mannooranparampil TJ, Passarelli F, Zappalà A, Annessi G, Marino C, Caggiati A, Russo N, Michelozzi P. Tumor-infiltrating lymphocytes predict cutaneous melanoma survival. Melanoma Res. 2015;25:306-311. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 58. | Lee HE, Chae SW, Lee YJ, Kim MA, Lee HS, Lee BL, Kim WH. Prognostic implications of type and density of tumour-infiltrating lymphocytes in gastric cancer. Br J Cancer. 2008;99:1704-1711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 198] [Cited by in F6Publishing: 232] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 59. | Ishigami S, Natsugoe S, Tokuda K, Nakajo A, Che X, Iwashige H, Aridome K, Hokita S, Aikou T. Prognostic value of intratumoral natural killer cells in gastric carcinoma. Cancer. 2000;88:577-583. [PubMed] [Cited in This Article: ] |
| 60. | Huang B, Chen L, Bao C, Sun C, Li J, Wang L, Zhang X. The expression status and prognostic significance of programmed cell death 1 ligand 1 in gastrointestinal tract cancer: a systematic review and meta-analysis. Onco Targets Ther. 2015;8:2617-2625. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 61. | Zhang L, Qiu M, Jin Y, Ji J, Li B, Wang X, Yan S, Xu R, Yang D. Programmed cell death ligand 1 (PD-L1) expression on gastric cancer and its relationship with clinicopathologic factors. Int J Clin Exp Pathol. 2015;8:11084-11091. [PubMed] [Cited in This Article: ] |
| 62. | Wu C, Zhu Y, Jiang J, Zhao J, Zhang XG, Xu N. Immunohistochemical localization of programmed death-1 ligand-1 (PD-L1) in gastric carcinoma and its clinical significance. Acta Histochem. 2006;108:19-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 356] [Cited by in F6Publishing: 382] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 63. | Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, Chen L, Pardoll DM, Topalian SL, Anders RA. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res. 2014;20:5064-5074. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1633] [Cited by in F6Publishing: 1860] [Article Influence: 186.0] [Reference Citation Analysis (0)] |
| 64. | Thompson RH, Kuntz SM, Leibovich BC, Dong H, Lohse CM, Webster WS, Sengupta S, Frank I, Parker AS, Zincke H. Tumor B7-H1 is associated with poor prognosis in renal cell carcinoma patients with long-term follow-up. Cancer Res. 2006;66:3381-3385. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 660] [Cited by in F6Publishing: 673] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 65. | Thompson ED, Zahurak M, Murphy A, Cornish T, Cuka N, Abdelfatah E, Yang S, Duncan M, Ahuja N, Taube JM. Patterns of PD-L1 expression and CD8 T cell infiltration in gastric adenocarcinomas and associated immune stroma. Gut. 2016; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 289] [Cited by in F6Publishing: 328] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 66. | Tamura T, Ohira M, Tanaka H, Muguruma K, Toyokawa T, Kubo N, Sakurai K, Amano R, Kimura K, Shibutani M. Programmed Death-1 Ligand-1 (PDL1) Expression Is Associated with the Prognosis of Patients with Stage II/III Gastric Cancer. Anticancer Res. 2015;35:5369-5376. [PubMed] [Cited in This Article: ] |
| 67. | Darb-Esfahani S, Kunze CA, Kulbe H, Sehouli J, Wienert S, Lindner J, Budczies J, Bockmayr M, Dietel M, Denkert C. Prognostic impact of programmed cell death-1 (PD-1) and PD-ligand 1 (PD-L1) expression in cancer cells and tumor-infiltrating lymphocytes in ovarian high grade serous carcinoma. Oncotarget. 2016;7:1486-1499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 201] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 68. | Cristescu R, Lee J, Nebozhyn M, Kim KM, Ting JC, Wong SS, Liu J, Yue YG, Wang J, Yu K. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21:449-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1071] [Cited by in F6Publishing: 1332] [Article Influence: 148.0] [Reference Citation Analysis (0)] |
| 69. | Marrelli D, Polom K, Pascale V, Vindigni C, Piagnerelli R, De Franco L, Ferrara F, Roviello G, Garosi L, Petrioli R. Strong Prognostic Value of Microsatellite Instability in Intestinal Type Non-cardia Gastric Cancer. Ann Surg Oncol. 2016;23:943-950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 70. | Kim KJ, Lee KS, Cho HJ, Kim YH, Yang HK, Kim WH, Kang GH. Prognostic implications of tumor-infiltrating FoxP3+ regulatory T cells and CD8+ cytotoxic T cells in microsatellite-unstable gastric cancers. Hum Pathol. 2014;45:285-293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 71. | Kim KJ, Wen XY, Yang HK, Kim WH, Kang GH. Prognostic Implication of M2 Macrophages Are Determined by the Proportional Balance of Tumor Associated Macrophages and Tumor Infiltrating Lymphocytes in Microsatellite-Unstable Gastric Carcinoma. PLoS One. 2015;10:e0144192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 72. | Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711-723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10799] [Cited by in F6Publishing: 11099] [Article Influence: 792.8] [Reference Citation Analysis (0)] |
| 73. | Robert C, Thomas L, Bondarenko I, O’Day S, Weber J, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517-2526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3331] [Cited by in F6Publishing: 3269] [Article Influence: 251.5] [Reference Citation Analysis (0)] |
| 74. | Postow MA. Managing immune checkpoint-blocking antibody side effects. Am Soc Clin Oncol Educ Book. 2015;76-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 253] [Cited by in F6Publishing: 279] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 75. | Moehler MH, Kim YH, Tan IB, Balogh A, Sanchez TK, Bang YJ. Sequential ipilimumab (Ipi) versus best supportive care (BSC) following first-line chemotherapy (Ctx) in patients (pts) with unresectable locally advanced or metastatic gastric or gastro-esophageal junction (GEJ) cancer: A randomized, open-label, two-arm, phase II trial (CA184-162) of immunotherapy as a maintenance concept. J Clin Oncol. 2013;31suppl:abstr TPS4151. [Cited in This Article: ] |
| 76. | Ralph C, Elkord E, Burt DJ, O’Dwyer JF, Austin EB, Stern PL, Hawkins RE, Thistlethwaite FC. Modulation of lymphocyte regulation for cancer therapy: a phase II trial of tremelimumab in advanced gastric and esophageal adenocarcinoma. Clin Cancer Res. 2010;16:1662-1672. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 189] [Cited by in F6Publishing: 190] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 77. | Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252-264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8693] [Cited by in F6Publishing: 9313] [Article Influence: 776.1] [Reference Citation Analysis (0)] |
| 78. | Le DT, Bendell JC, Calvo E, Kim JW, Ascierto PA, Sharma P, Ott PA, Bono P, Jaeger D, Jeffry Evans TR. Safety and activity of nivolumab monotherapy in advanced and metastatic (A/M) gastric or gastroesophageal junction cancer (GC/GEC): Results from the CheckMate-032 study. J Clin Oncol. 2016;34 Suppl 4:abstr 6. [Cited in This Article: ] |
| 79. | Muro K, Bang Y, Shankaran V, Geva R, Catenacci DV, Gupta S, Eder JP, Berger R, Gonzalez EJ, Pulini J. A phase 1b study of pembrolizumab (Pembro; MK-3475) in patients (Pts) with advanced gastric cancer. Annals of Oncology. 2014;25:1-41. [DOI] [Cited in This Article: ] |
| 80. | Muro K, Bang YJ, Shankaran V, Geva R, Catenacci DV, Gupta S, Eder JP, Berger R, Gonzalez EJ, Ray A. Relationship between PD-L1 expression and clinical outcomes in patients (Pts) with advanced gastric cancer treated with the anti-PD-1 monoclonal antibody pembrolizumab (Pembro; MK-3475) in KEYNOTE-012. J Clin Oncol. 2015;33 Suppl 3:abstr 3. [Cited in This Article: ] |
| 81. | Ribas A, Robert C, Hodi FS, Wolchok JD, Joshua AM, Hwu WJ, Weber JS, Zarour HM, Kefford R, Loboda A. Association of response to programmed death receptor 1 (PD-1) blockade with pembrolizumab (MK-3475) with an interferon-inflammatory immune gene signature. J Clin Oncol. 2015;33 Suppl:abstr 3001. [Cited in This Article: ] |
| 82. | Shankaran V, Muro K, Bang YJ, Geva R, Catenacci DV, Gupta S, Eder JP, Berger R, Loboda A, Albright A. Correlation of gene expression signatures and clinical outcomes in patients with advanced gastric cancer treated with pembrolizumab (MK-3475). J Clin Oncol. 2015;33 Suppl; abstr 3026. [Cited in This Article: ] |
| 83. | Alsina M, Moehler M, Hierro C, Guardeño R, Tabernero J. Immunotherapy for Gastric Cancer: A Focus on Immune Checkpoints. Target Oncol. 2016; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 84. | de Guillebon E, Roussille P, Frouin E, Tougeron D. Anti program death-1/anti program death-ligand 1 in digestive cancers. World J Gastrointest Oncol. 2015;7:95-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 41] [Cited by in F6Publishing: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 85. | Raufi AG, Klempner SJ. Immunotherapy for advanced gastric and esophageal cancer: preclinical rationale and ongoing clinical investigations. J Gastrointest Oncol. 2015;6:561-569. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 32] [Reference Citation Analysis (0)] |
| 86. | Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM, Segal NH, Ariyan CE, Gordon RA, Reed K. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369:122-133. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3192] [Cited by in F6Publishing: 3187] [Article Influence: 289.7] [Reference Citation Analysis (0)] |
| 87. | Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med. 2015;372:2509-2520. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6096] [Cited by in F6Publishing: 6542] [Article Influence: 726.9] [Reference Citation Analysis (0)] |
| 88. | Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pagès C, Tosolini M, Camus M, Berger A, Wind P. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960-1964. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4318] [Cited by in F6Publishing: 4595] [Article Influence: 255.3] [Reference Citation Analysis (0)] |
| 89. | Galon J, Pagès F, Marincola FM, Thurin M, Trinchieri G, Fox BA, Gajewski TF, Ascierto PA. The immune score as a new possible approach for the classification of cancer. J Transl Med. 2012;10:1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 415] [Cited by in F6Publishing: 457] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 90. | Anitei MG, Zeitoun G, Mlecnik B, Marliot F, Haicheur N, Todosi AM, Kirilovsky A, Lagorce C, Bindea G, Ferariu D. Prognostic and predictive values of the immunoscore in patients with rectal cancer. Clin Cancer Res. 2014;20:1891-1899. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 237] [Cited by in F6Publishing: 261] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 91. | Kershaw MH, Devaud C, John LB, Westwood JA, Darcy PK. Enhancing immunotherapy using chemotherapy and radiation to modify the tumor microenvironment. Oncoimmunology. 2013;2:e25962. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 92. | Kroemer G, Galluzzi L, Kepp O, Zitvogel L. Immunogenic cell death in cancer therapy. Annu Rev Immunol. 2013;31:51-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1808] [Cited by in F6Publishing: 1896] [Article Influence: 172.4] [Reference Citation Analysis (0)] |