Published online Apr 28, 2016. doi: 10.3748/wjg.v22.i16.4160
Peer-review started: December 20, 2015
First decision: December 30, 2015
Revised: January 20, 2016
Accepted: February 20, 2016
Article in press: February 22, 2016
Published online: April 28, 2016
AIM: To evaluate pain control in chronic pancreatitis patients who underwent total pancreatectomy with islet cell transplantation or intrathecal narcotic pump infusion.
METHODS: We recognized 13 patients who underwent intrathecal narcotic pump (ITNP) infusion and 57 patients who underwent total pancreatectomy with autologous islet cell transplantation (TP + ICT) for chronic pancreatitis (CP) pain control between 1998 and 2008 at Indiana University Hospital. All patients had already failed multiple other modalities for pain control and the decision to proceed with either intervention was made at the discretion of the patients and their treating physicians. All patients were evaluated retrospectively using a questionnaire inquiring about their pain control (using a 0-10 pain scale), daily narcotic dose usage, and hospital admission days for pain control before each intervention and during their last follow-up.
RESULTS: All 13 ITNP patients and 30 available TP + ICT patients were evaluated. The mean age was approximately 40 years in both groups. The median duration of pain before intervention was 6 years and 7 years in the ITNP and TP + ICT groups, respectively. The median pain score dropped from 8 to 2.5 (on a scale of 0-10) in both groups on their last follow up. The median daily dose of narcotics also decreased from 393 mg equivalent of morphine sulfate to 8 mg in the ITNP group and from 300 mg to 40 mg in the TP + ICT group. No patient had diabetes mellitus (DM) before either procedure whereas 85% of those who underwent pancreatectomy were insulin dependent on their last evaluation despite ICT.
CONCLUSION: ITNP and TP + ICT are comparable for pain control in patients with CP however with high incidence of DM among those who underwent TP + ICT. Prospective comparative studies and longer follow up are needed to better define treatment outcomes.
Core tip: Total pancreatectomy (TP) is the last resort offered to chronic pancreatitis (CP) patients with intractable pain when other interventions have failed. We wanted to compare pain control and rate of insulin-dependent diabetes in CP patients after TP and autologous islet cell transplantation (ICT) or intrathecal narcotic pump infusion, which is a relatively new and less invasive technique used for chronic analgesia in multiple other clinical settings. We found that pain control was similar between the two interventions after a median follow-up of 3 years yet the rate of insulin-dependent diabetes was still high in the surgical resection group despite the ICT.
- Citation: Mokadem M, Noureddine L, Howard T, McHenry L, Sherman S, Fogel EL, Watkins JL, Lehman GA. Total pancreatectomy with islet cell transplantation vs intrathecal narcotic pump infusion for pain control in chronic pancreatitis. World J Gastroenterol 2016; 22(16): 4160-4167
- URL: https://www.wjgnet.com/1007-9327/full/v22/i16/4160.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i16.4160
Abdominal pain remains the most common and difficult to treat complaint for patients with chronic pancreatitis as it can often be severe and debilitating. There is still lack of full understanding of the exact mechanism of pain in chronic pancreatitis (CP) and factors contributing to it are only partially defined[1-3]. The general goals of treatment include pain relief in addition to prevention and management of disease related complications such as pseudocysts, strictures, malabsorption (exocrine failure) and diabetes mellitus (endocrine failure). Opiates, however, remain the most frequently used analgesics in the background of all other treatment options. It is the generally acceptable approach to start with the least invasive intervention first, such as alcohol and smoking abstinence, and then advance in a stepwise manner as the method fails[4-6]. Total pancreatectomy (TP) is considered the final resort offering additional pain control to most patients with remaining intractable pain at the expense of developing insulin dependent diabetes. The addition of autologous islet cell transplantation (ICT) to TP has been shown to have variable success in prevention of insulin dependence from zero up to a maximum of 40% based on the performing center and the duration of follow up[7-9]. Neuroaxial blockage modalities such as spinal cord stimulation or intrathecal analgesia are among the newer modalities that may have a role in CP. Experience in this field, however, has been limited to case reports[10-12]. Among these, the intrathecal narcotic pump infusion (ITNP) is the most studied modality for control of intractable pain in cancer as well as non-cancer patients but with variable level of success[13-16]. The ITNP consists of a channeled catheter intrathecally (into the subarachnoidal space) that is connected to a small battery-powered programmable pump which is placed in the subcutaneous tissue of the abdominal wall. In our institution, we used a Medtronic Synchro MedII pump that possesses a 40 mL drug reservoir that is filled via a transcutaneous route under sterile conditions every 1-6 mo[17]. The literature has been scarce regarding its role and efficacy in patients with CP. In 2009, Kongkam et al[17] published a pilot study from the same center suggesting a promising role of ITNP in these patients.
Using hospital electronic records and the endoscopic retrograde cholangiopancreatography (ERCP) database at Indiana University Medical Center from 1998 to 2008, we identified 13 patients who underwent ITNP infusion and 57 patients who underwent TP + ICT for CP and control of pain. The goal was to assess pain control in a cohort of surgical patients that is at least two fold the previously reported cohort of ITNP patients. All patients were managed at the discretion of their gastroenterology treating physicians at Indiana University and different approaches were selected based on clinical judgment and patient preferences. When patients’ final decision was to undergo ITNP, the procedure was arranged and performed at Indiana University Hospital. On the other hand, when patients decided to proceed with TP + ICT, the surgery was arranged to be performed in one of three different surgical centers that offer this procedure- including Indiana University Hospital- based on patients’ preferences and proximity to their household. Patients with persistent evidence of increased duct pressure were offered surgical or endoscopic decompression procedures - as appropriate - before being considered for total resection. All patients available for follow up answered a phone call-based questionnaire inquiring about their pain level, their daily narcotic use and the number and duration of hospital admissions for pain control.
The phone call inquiry about pain control is part of the standard care provided by the gastroenterology group at Indiana University. Verbal informed consent was obtained from all patients before proceeding with the questions. The study design abides by the ethical guidelines of the “World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects”. Pain was assessed subjectively using a zero to ten scales (0 being no pain and 10 being maximum pain) before each procedure and on the last follow up available. All the daily narcotics used before and after the procedures were recorded and converted to milligram (mg) equivalent of oral morphine sulfate using a pharmacologic online converter http://www.globalrph.com/narcotic.cgi.
The number of in-hospital days per year for pain control was defined as the number of in-hospital admissions multiplied by the average duration of each admission (in days) divided by the total number of pain-years. This was recorded in each group before and after each intervention. Finally, the diabetes mellitus status, the average units of insulin used per day and the last HbA1C (glycosylated hemoglobin) were also recorded among the surgical group candidates on their last follow up.
All data are presented as median or mean ± standard deviation. Only P-values that are less than 0.05 were considered statistically significant. Experiments comparing two means were analyzed using Student’s t-test with Welch’s correction if appropriate.
The thirty patients who answered the phone call questionnaire constituted the surgery study group while no data was available from the remaining 27 surgical candidates. All 13 ITNP patients (5 male, 8 female) and the 30 TP + ICT patients (6 male, 24 female) contacted were Caucasians with a mean age of 40.6 years (± 9.6) and 39.9 years (± 14) respectively. The median duration of pain was 6 years (range 2-22) in the ITNP group and 7 years (range 1-21) in the TP + ICT group before each procedure. The median duration of follow up was 3 years in both groups with a range of 0.5 to 9 years in the ITNP group and 0.5 to 10 years in the TP + ICT group. The most common etiology of CP was idiopathic in the TP + ICT group (approximately 63%) followed by pancreatic divisum (approximately 17%), while it was pancreatic divisum (46%) followed by idiopathic in the ITNP group (approximately 23%). Alcohol constituted 15% of the ITNP group and approximately 7% of the surgery group (Table 1).
| Idiopathic | Pancreatic divisum | Alcohol induced | Gallstone induced | Auto-immune | |
| ITNP group | 6/13 (46.1) | 3/13 (23.1) | 1/13 (7.7) | 2/13 (15.4) | 1/13 (7.7) |
| TP + ICT group | 19/30 (63.3) | 5/30 (16.7) | 4/30 (13.3) | 2/30 (6.7) | 0/30 (0) |
One ITNP patient developed serious meningitis requiring permanent removal of the catheter and pump and was excluded from the study. Three surgical patients were reported dead by their families upon contact, leaving 12 ITNP and 27 TP + ICT patients for retrospective comparison. All patients underwent multiple interventions for attempted pain control before either procedures such as ERCP with sphincterotomy (100% in both groups), celiac plexus neurolysis (46% of ITNP and 50% of TP + ICT), enteral tube feeding for bowel rest (61% of ITNP and approximately 33% of TP + ICT), and surgery (approximately 61% in ITNP and approximately 33% in TP + ICT).
The most common surgical procedure performed was denervation (bilateral splanchnicectomy) in the ITNP group and decompression (Puestow procedure) in the TP + ICT group (Table 2).
| ERCP with sphincterotomy | Celiac Block (EUS or CT) | Jejunal or Gastro-Jejunal tube insertion | Surgeries (denervation or decompression) | |
| ITNP group | 13/13 (100) | 6/13 (46) | 8/13 (61) | 8/13 (61) |
| TP + ICT group | 30/30 (100) | 15/30 (50) | 10/30 (33) | 10/30 (33) |
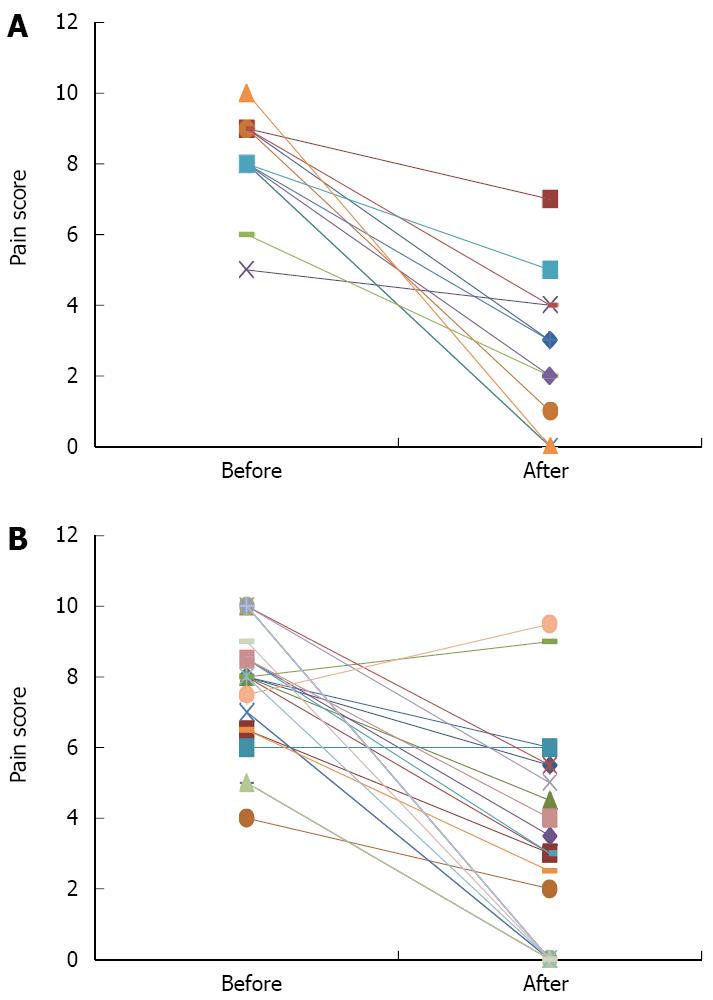
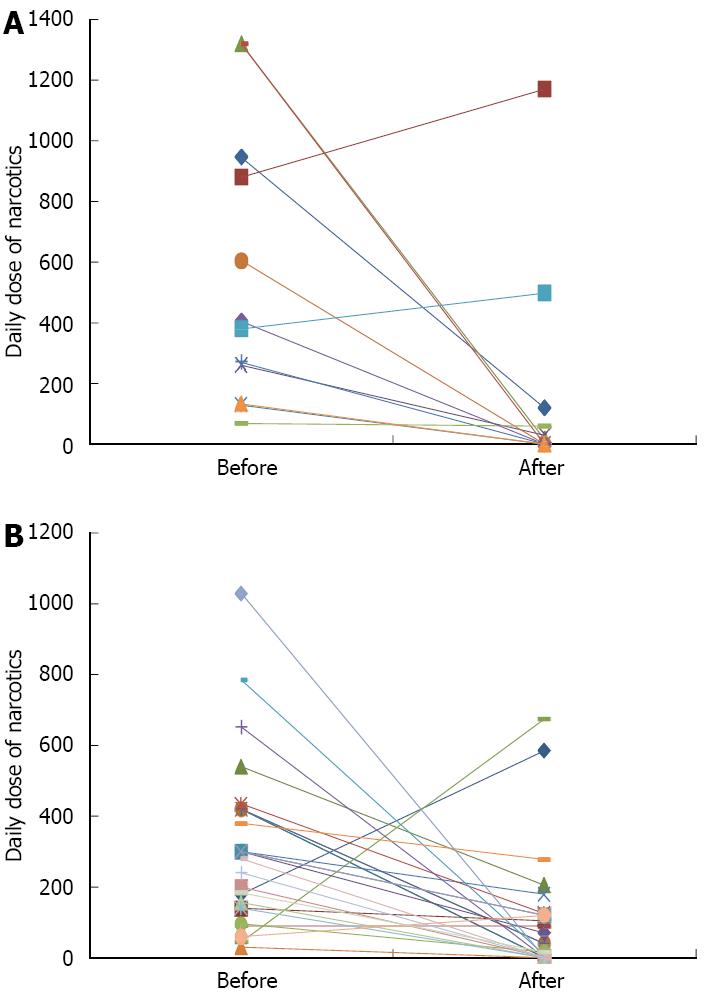
The pain score dropped from a mean of 8.1 (± 1.4) and a median of 8 before the ITNP to a mean of 2.5 (± 2.2) and a median of 2.5 on the last follow up (Figure 1A). Similarly, the pain score dropped from a mean of 8.0 (± 1.7) and a median of 8 before the TP+ICT to a mean of 2.7 (± 2.9) and a median of 2.5 on the last follow up (Figure 1B). No ITNP patients reported increase in their pain score and 3 out of 12 were still pain free on their last follow up (duration of last follow up was 0.5, 5, and 9 years respectively). Two TP + ICT patients reported worsening of their pain after surgery and one reported no change. 12 surgical patients were still pain free on their last follow up with a median duration of 4 years. The daily narcotics usage among ITNP patients decreased from a median of 393 mg equivalent of morphine sulfate and a mean of 553 mg (± 448) before intervention to a median of 8 mg and a mean of 158 mg (± 349) on their last clinic follow up, respectively (P < 0.05) (Figure 2A). Likewise, TP + ICT patients experienced a drop in their daily narcotics usage from a median of 300 mg equivalent of morphine sulfate and a mean of 316 mg (± 234) before surgery to a median of 40 mg and a mean of 104 mg (± 170) on their last clinic follow up, respectively (P < 0.05) (Figure 2B).
Two ITNP patients had increase in their oral daily narcotic requirements, one patient had very minimal decrease in his dose and six were narcotic free on their last follow up. The duration of follow up for these patients ranged from 0.5 to 7 years with a median of 1.5 years. The average dose of intrathecal morphine was 7.5 mg (2-10 mg). Three TP + ICT had increase in their daily narcotic requirements and 9 patients were narcotic free on their last follow up. The duration of follow up ranged from 1 to 10 years with a median of 4 years. These same 9 patients also reported zero pain (Figure 2A and B).
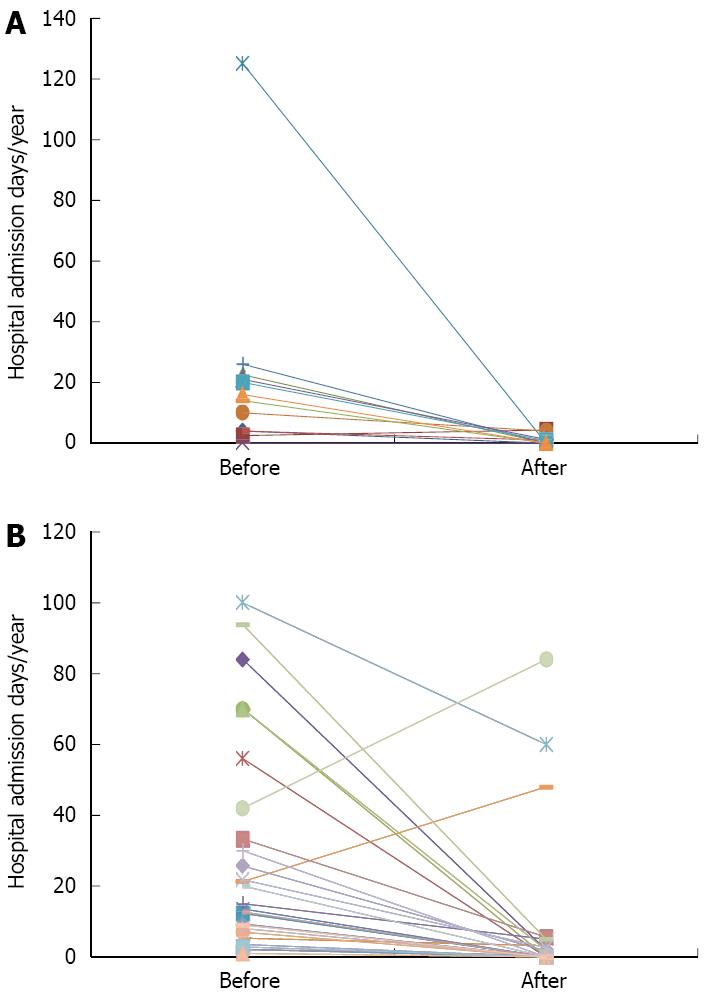
The number of in-hospital days per year (d/year) for pain control decreased from a mean of 22 d/year (± 34) and a median of 15 d/year before ITNP to a mean of 1 d/year (± 1.5) and a median of zero thereafter. Only one patient reported increase in his hospital admission days per year for pain control and 7 patients (64%) have not been admitted to the hospital for pain control as of their last follows up. Likewise, the number of hospital days dropped from a mean of 29 d/year (± 30) and a median of 15 d/year before total pancreatectomy to a mean of 8 d/year (± 2) and a median of zero on the last follow up. Two patients reported increase in their hospital admission days per year and 15 patients (55%) have not been admitted to the hospital for pain control as of their last follow up (Figure 3A and B).
No patient had diabetes mellitus before either intervention in both groups. Only 4 out of the 27 surgical patients (approximately 15%) were insulin free on their last follow up despite the autologous islet cell transplantation. The average insulin dose per day was 25 units among the new diabetics with a median of 21 units (range = 4-54 units). The last HbA1c reported by the TP + ICT patients had an average of 7.35% and a median of 6.6% (Table 3). There were 3 deaths in the TP + ICT group (10% mortality rate), 2 were due to sepsis occurring at 3 wk and 1 mo after surgery as reported by family. However, no further information was available for the third death case. One TP + ICT patient had abscess formation in the abdomen post-surgery requiring drainage. No other major surgical complications were reported by patients during the questionnaire; however, no surgical records were available for patients operated on at other institutions. No death to date occurred in our series among the ITNP group. Two out of the 13 patients who underwent the ITNP infusion had bacterial meningitis. One of them was serious enough to necessitate catheter and pump removal and was excluded from the study. One patient had CSF leak (7.7%) that was surgically repaired with no further reported complications.
| Number of patients with insulin independence | Average dose of insulin/day (units) | Average HbA1c | |
| Before TP + ICT | 30/30 (100%) | 0 | N/A |
| After TP + ICT | 4/27 (approximately 15%) | 25 | 7.35% |
Here we report two relatively similar series of patients with intractable pain due to chronic pancreatitis who underwent either an intrathecal narcotic pump infusion or total pancreatectomy with islet cell transplantation as a terminal procedure for pain control after failure of multiple other modalities. We considered two ITNP patients to have failed treatment because of higher narcotic use and increased hospital admission days upon their last follow up despite having lower pain scores.
Likewise, three TP + ICT patients can also be reported as failure due to worsening pain, higher narcotic use and increase in hospital admissions in 2 of them, and only higher narcotic use in the remaining one. Therefore, in our case series, success rate was observed as 77% (10/13) among the ITNP group and 80% (24/30) among the TP + ICT group for pain control. Most of the published case series reported a post-operative morbidity range (e.g. infections, anastomosis leak, etc.) between 25 and 68% but major complications constituted approximately 14%-18% based on their reporting[7,9,18]. Several series from single centers reported a peri-operative mortality rate (usually defined as mortality within 2 wk of surgery) of 0% to 3.5% from total pancreatectomy[7-9,18-20]. Our multi-center based data was incomplete as we were unable to record the morbidity and mortality among all 57 surgical patients. However, the thirty-day mortality, which may not reflect the exact peri-operative mortality, is found to be at best 3.5% (3 out of 57) and at worst 10% (3 out of 30). The rate of serious complications (like bacterial meningitis, CSF leak and pump or catheter migration) from intrathecal analgesia is not clear in the literature but reports vary from 0% to 20% depending on the center, the population studied, and duration of follow up[14-16]. Anderson et al[16] and Kumar et al[14] reported a success rate of 50% and 75% respectively using intrathecal morphine in patients with chronic non-malignant pain after an average duration of follow up of approximately 2 years. This, however, drops to 30% and 44% respectively when success rate is defined as more than 50% reduction in visual pain scores[14,16]. It is important to note that all our successful ITNP patients (10 out of 13) had more than 50% reduction in their pain scores with an average intrathecal morphine dose of 7.5 mg/d (range 2.5-10 mg/d).
Our results from TP + ICT have been consistent with several previous series reporting successful pain control and narcotic independence in 70%-80% of subjects within 6-12 mo after surgery[8,9,18,19]. Garcea et al[20] reported in a a series of 85 pts who underwent TP + ICT for CP that narcotic-free patients dropped from 90% after surgery to 40% at 1 year and ultimately to l6% at 5 years. On the other hand, Riediger et al[21] reported 87% improvement in pain control of 224 patients as far as 10 years after pancreatic head resection. However, 72% of these patients were back on narcotic medications despite using lower doses. Therefore, the success rate of pain control after pancreatectomy seems to depend largely on the definition of “success”[21]. Nonetheless, the most effective and most durable pancreatic surgeries performed for pain control in chronic pancreatitis seem to involve resection of the head of pancreas when compared with denervation or decompression procedures[18-21].
Our series had a 3 years median duration of follow up raising the question about the durability of the reported rate of 80%. The complete success of the autologous islet cell graft with resulting insulin independence has variably been reported to range from zero up to 40% within duration of follow up between 6 and 24 mo[8,9,18,19]. Garcea et al[20] again showed in his series that insulin independence dropped from 14.1% post engraftment to 5.9% after a median follow up duration of 8 years. However, there still might be a role for ICT in diabetes management after TP since there is evidence of partial graft function in patients with insulin-dependent diabetes after pancreatectomy but with relatively low insulin requirements. Therefore, ICT may probably add some protection against hypoglycemia events and long-term diabetes complications. However, this need to be evaluated independently[20,22]. Female gender, lower body weight and higher number of islet cells transplanted have been suggested to be positive predictive factors of graft survival[8,18,19]. Our data show a complete preservation of islet cells graft function in 15% of pts after a median follow up of 3 years (range 0.5-10 years) and an acceptable glucose control (average HbA1c 7.35%) with moderate insulin requirements (average 25 units/d) compared to patients with type 1 diabetes. Further follow-up of these patients is very important in order to assess for any further change in the islet cell graft viability and insulin requirements as in Garcea’s report[20]. The incidence of diabetes mellitus complications awaits further follow up. Positive outcomes were very similar among both treatment modalities (Table 4) but major limitations still exist in our series.
| ITNP | TP + ICT | Comparison | |
| Reversibility of the procedure | Yes | No | Different |
| Success rate for pain control | 77% | 80% | Similar |
| Residual narcotic dose usage (mg equivalent of oral morphine sulfate) | Mean = 158 mg/d | Mean = 104 mg/d | Similar |
| Median = 8 mg/d | Median = 40 mg/d | ||
| Percentage of patients with poor pain control | 16.7% | 11.1% | Similar |
| Percentage of patients with new insulin dependent diabetes | 0% | Approximately 85% | Different |
| Procedure related death | 0% | 10% | Different |
First, the study is retrospective as it will be difficult to prospectively design a large population study in patients with CP, especially when it involves very extensive surgery such as total pancreatectomy with islet cell transplantation a procedure performed in only few selected centers in the United States. Second, the ITNP and surgical interventions were performed in different institutions which make comparison more difficult given the variability in technical performance. This discrepancy was due to the fact that ITNP was offered at Indiana University Hospital by the treating gastroenterologist there as a one day procedure like all other interventions provided. However, when the ultimate decision was to go for TP + ICT and since some patients came from out-of-state, the surgical center was chosen based on proximity to patients’ homes and social support. Third, not all surgical patients were assessed due to the fact that many surgeries were performed in multiple institutions and medical records were not available to us for review. In addition, three years median duration of follow up is still considered modest for CP. Larger comparative series with longer duration of follow up are needed to better characterize the optimal management of intractable pain in patients with chronic pancreatitis.
In conclusion, our case series compared two advanced interventions offered to chronic pancreatitis patients who failed several conventional therapies and continued to have high reported levels of daily pain coupled with consumption of large dosages of narcotics. Total pancreatectomy is a morbid surgery associated with well-known short and long term peri-operative risks with insulin-dependent diabetes being one of its major sequelae. Based on our data, the addition of islet cell transplantation to total pancreatectomy may offer a protective effect from insulin dependence at least for few years. This surgical procedure is not readily accessible to many patients within the United States or around the world.
On the other hand, intrathecal narcotic pump infusion is a relatively newer, less invasive therapeutic technique that delivers significantly lower doses of narcotics to the spinal fluid, therefore minimizing major systemic side effects of narcotics such as tolerance and constipation. There is very limited data of its long term efficacy and complications in chronic pancreatitis patients but observations can be extrapolated from reported patients with central nervous system disorders. Based on our data, ITNP seems to have a promising role as it showed comparable effect to total pancreatectomy on pain control with the additional benefit of preserving glucose and insulin metabolism. Future prospective studies in selected patients with chronic pancreatitis will better define its future role in pain management.
We would like to thank all staff and personnel of the Division of Gastroenterology and Hepatology at Indiana University Medical Center who helped in the execution of this study.
Chronic pancreatitis (CP) patients who still have intractable abdominal pain despite undergoing several endoscopic and surgical interventions for analgesia are left with very few options short of having a complete resection of their pancreas. Total pancreatectomy is associated with adverse effect of insulin-dependent diabetes which may be reversed or delayed by performing islet cell transplantation via infusion of isolated islet cells into the portal system. However, this surgery carries a significant risk of morbidity and mortality and is usually reserved as the last resort for pain control in chronic pancreatitis.
Intrathecal narcotic pump infusion is a minimally invasive procedure aimed at delivering very low dose of narcotics to the spinal fluid through a small catheter for the purpose of analgesia with minimal narcotic’s side effects. This pump is currently used to manage severe pain in patients with refractory abdominal malignancies and in those with central nervous system injury and secondary spasms.
The authors examine - in a rare comparison - multiple markers of pain control in chronic pancreatitis patients who underwent either total pancreatectomy with islet cell transplantation or the less invasive yet relatively new procedure of intrathecal narcotic pump infusion.
The intrathecal narcotic pump (ITNP) infusion seems to have similar pain control to total pancreatectomy with islet cell transplantation (TP + ICT) with significant lower incidence of insulin-dependent diabetes. This modality may be considered as an option in chronic pancreatitis patients with intractable pain who refuse or do not qualify for total pancreatectomy.
This is a retrospective study of TP + ICT and ITNP for the control of intractable pain in CP. The aim is to evaluate pain control in patients with CP from a single center. Small series, but exceptionally well conducted, analyzed, and written. This is an important message that there may be a viable non-surgical alternative to TP and ICT for intractable pain in CP.
P- Reviewer: Bradley EL 3rd, Fu DL, Sperti C S- Editor: Gong ZM L- Editor: A E- Editor: Zhang DN
| 1. | Gachago C, Draganov PV. Pain management in chronic pancreatitis. World J Gastroenterol. 2008;14:3137-3148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 62] [Cited by in F6Publishing: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Warshaw AL, Banks PA, Fernández-Del Castillo C. AGA technical review: treatment of pain in chronic pancreatitis. Gastroenterology. 1998;115:765-776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 223] [Cited by in F6Publishing: 232] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 3. | Layer P, Yamamoto H, Kalthoff L, Clain JE, Bakken LJ, DiMagno EP. The different courses of early- and late-onset idiopathic and alcoholic chronic pancreatitis. Gastroenterology. 1994;107:1481-1487. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 518] [Cited by in F6Publishing: 420] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 4. | Steer ML, Waxman I, Freedman S. Chronic pancreatitis. N Engl J Med. 1995;332:1482-1490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 477] [Cited by in F6Publishing: 412] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 5. | Abdel Aziz AM, Lehman GA. Current treatment options for chronic pancreatitis. Curr Treat Options Gastroenterol. 2007;10:355-368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Singh VV, Toskes PP. Medical therapy for chronic pancreatitis pain. Curr Gastroenterol Rep. 2003;5:110-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Behrman SW, Mulloy M. Total pancreatectomy for the treatment of chronic pancreatitis: indications, outcomes, and recommendations. Am Surg. 2006;72:297-302. [PubMed] [Cited in This Article: ] |
| 8. | Wahoff DC, Papalois BE, Najarian JS, Kendall DM, Farney AC, Leone JP, Jessurun J, Dunn DL, Robertson RP, Sutherland DE. Autologous islet transplantation to prevent diabetes after pancreatic resection. Ann Surg. 1995;222:562-575; discussion 575-579. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 168] [Cited by in F6Publishing: 176] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Argo JL, Contreras JL, Wesley MM, Christein JD. Pancreatic resection with islet cell autotransplant for the treatment of severe chronic pancreatitis. Am Surg. 2008;74:530-536; discussion 536-537. [PubMed] [Cited in This Article: ] |
| 10. | Kapural L, Rakic M. Spinal cord stimulation for chronic visceral pain secondary to chronic non-alcoholic pancreatitis. J Clin Gastroenterol. 2008;42:750-751. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Paicius RM, Bernstein CA, Lempert-Cohen C. Peripheral nerve field stimulation in chronic abdominal pain. Pain Physician. 2006;9:261-266. [PubMed] [Cited in This Article: ] |
| 12. | Verheijen R, Slappendel R, Jansen JB, Crul BJ, van Dongen RT. [Intrathecal administration of morphine and bupivacaine in the treatment of severe pain in chronic pancreatitis]. Ned Tijdschr Geneeskd. 1996;140:1410-1412. [PubMed] [Cited in This Article: ] |
| 13. | Newsome S, Frawley BK, Argoff CE. Intrathecal analgesia for refractory cancer pain. Curr Pain Headache Rep. 2008;12:249-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Kumar K, Kelly M, Pirlot T. Continuous intrathecal morphine treatment for chronic pain of nonmalignant etiology: long-term benefits and efficacy. Surg Neurol. 2001;55:79-86; discussion 86-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 124] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Thimineur MA, Kravitz E, Vodapally MS. Intrathecal opioid treatment for chronic non-malignant pain: a 3-year prospective study. Pain. 2004;109:242-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 85] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Anderson VC, Burchiel KJ. A prospective study of long-term intrathecal morphine in the management of chronic nonmalignant pain. Neurosurgery. 1999;44:289-300; discussion 300-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 171] [Cited by in F6Publishing: 139] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Kongkam P, Wagner DL, Sherman S, Fogel EL, Whittaker SC, Watkins JL, McHenry L, Lehman GA. Intrathecal narcotic infusion pumps for intractable pain of chronic pancreatitis: a pilot series. Am J Gastroenterol. 2009;104:1249-1255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Rodriguez Rilo HL, Ahmad SA, D’Alessio D, Iwanaga Y, Kim J, Choe KA, Moulton JS, Martin J, Pennington LJ, Soldano DA. Total pancreatectomy and autologous islet cell transplantation as a means to treat severe chronic pancreatitis. J Gastrointest Surg. 2003;7:978-989. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Ahmad SA, Lowy AM, Wray CJ, D’Alessio D, Choe KA, James LE, Gelrud A, Matthews JB, Rilo HL. Factors associated with insulin and narcotic independence after islet autotransplantation in patients with severe chronic pancreatitis. J Am Coll Surg. 2005;201:680-687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 139] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | Garcea G, Weaver J, Phillips J, Pollard CA, Ilouz SC, Webb MA, Berry DP, Dennison AR. Total pancreatectomy with and without islet cell transplantation for chronic pancreatitis: a series of 85 consecutive patients. Pancreas. 2009;38:1-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Riediger H, Adam U, Fischer E, Keck T, Pfeffer F, Hopt UT, Makowiec F. Long-term outcome after resection for chronic pancreatitis in 224 patients. J Gastrointest Surg. 2007;11:949-959; discussion 959-960. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Webb MA, Illouz SC, Pollard CA, Gregory R, Mayberry JF, Tordoff SG, Bone M, Cordle CJ, Berry DP, Nicholson ML. Islet auto transplantation following total pancreatectomy: a long-term assessment of graft function. Pancreas. 2008;37:282-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |