Published online Sep 14, 2015. doi: 10.3748/wjg.v21.i34.10045
Peer-review started: March 7, 2015
First decision: April 13, 2015
Revised: May 5, 2015
Accepted: June 26, 2015
Article in press: June 26, 2015
Published online: September 14, 2015
Endoscopic ultrasound (EUS)-guided biliary drainage is accepted as a less invasive, alternative treatment for patients in whom endoscopic retrograde cholangiopancreatography has failed. Most patients with malignant hilar obstruction undergo EUS-guided hepaticogastrostomy. The authors present the case of a 77-year-old man with advanced hilar cholangiocarcinoma who had undergone a roux-en-Y hepaticojejunostomy several months prior. He developed progressive jaundice and a low-grade fever that persisted for one week. The enteroscopic-assisted endoscopic retrograde cholangiopancreatography failed, thus the patient was scheduled for EUS-guided biliary drainage. In order to obtain adequate drainage, both intrahepatic systems were drained. This report describes the technique used for bilateral drainage via a transgastric approach. Currently, only a few different techniques for EUS-guided right system drainage have been reported in the literature. This case demonstrates that bilateral EUS-guided biliary drainage is feasible and effective in patients with hilar cholangiocarcinoma, and thus can be used as an alternative to percutaneous biliary drainage.
Core tip: Endoscopic ultrasound-guided left system drainage via hepaticogastrostomy can be performed with > 90% technical and clinical success in patients with obstructive jaundice. A transgastric approach for endoscopic ultrasound-guided hepaticogastrostomy to drain both intrahepatic systems was successfully performed by manipulating the guidewire until it passed across the stricture point; the two systems were then bridged with a metal stent. The authors propose that this technique is feasible and effective for bilateral biliary drainage.
-
Citation: Prachayakul V, Aswakul P. Endoscopic ultrasound-guided biliary drainage: Bilateral systems drainage
via left duct approach. World J Gastroenterol 2015; 21(34): 10045-10048 - URL: https://www.wjgnet.com/1007-9327/full/v21/i34/10045.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i34.10045
Endoscopic ultrasound (EUS)-guided biliary drainage was first reported in 2001 by Giovannini et al[1]. A subsequent case series described by Burmester et al[2] in 2003 demonstrated the feasibility of this technique using two platforms depending on the route of approach: EUS-guided transpapillary and transgastric. Since then, this therapeutic intervention has become an alternative treatment for patients with malignant bile duct obstruction in whom endoscopic retrograde cholangiopancreatography (ERCP) has failed, and in patients who prefer internal rather than percutaneous biliary drainage. When performed by experienced endoscopists, this technique has technical and clinical success rates of 75%-100% and 65%-92%, respectively[3-9]. As a result, EUS-guided biliary drainage has become more popular.
EUS-guided rendezvous with a transpapillary approach or antegrade stent insertion or EUS-guided transgastric drainage (EUS-guided hepaticogastrostomy) may be useful for patients with malignant hilar obstruction in whom ERCP has failed[10]. The case reported here describes a 77-year-old man with advanced hilar cholangiocarcinoma who underwent surgical bypass and developed obstructive jaundice thought to be due to tumor recurrence at the anastomosis site. EUS-guided bilateral biliary drainage was performed after enteroscopic-assisted ERCP failed.
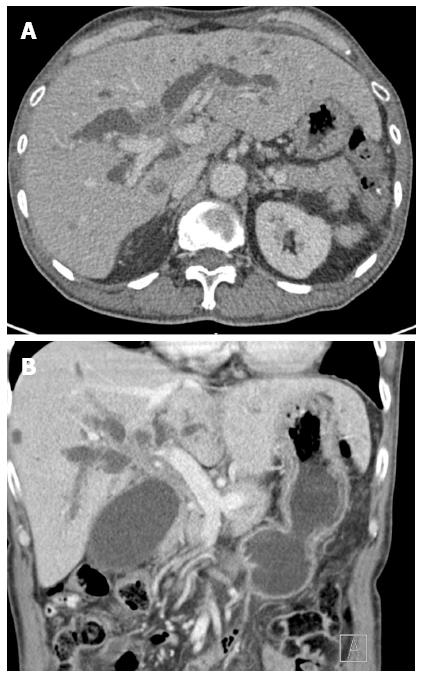
A 77-year-old man with hilar cholangiocarcinoma had undergone roux-en-Y hepaticojejunostomy several months prior. He subsequently developed progressive jaundice and a low-grade fever that persisted for a week. Liver function analyses showed hyperbilirubinemia with total bilirubin of 12.7 mg/dL (reference range: 0-1.5 mg/dL), a direct bilirubin level of 11.3 mg/dL (reference range: 0-1.2 mg/dL), and an elevated alkaline phosphatase level (395 U/L; reference range: 40-125 U/L). A computed tomography (CT) scan revealed a large, ill-defined, enhanced lesion in the hilar region that had invaded hepatic segment IV and caused bilateral intrahepatic duct dilation (Figure 1). Enteroscopic-assisted ERCP failed, and the patient was therefore scheduled for EUS-guided biliary drainage.
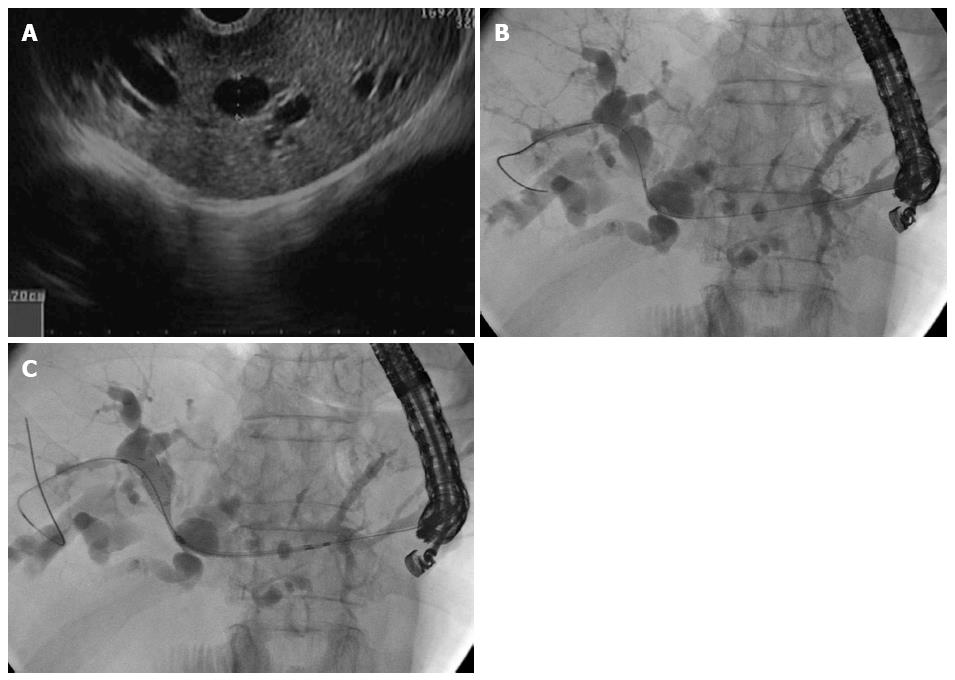
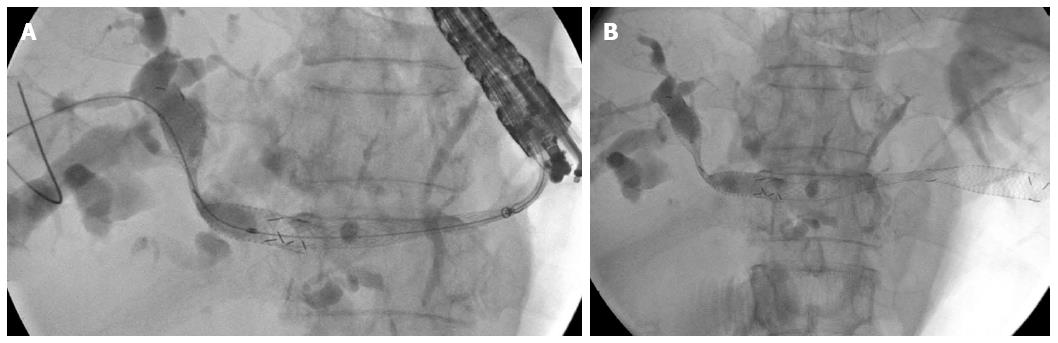
To obtain adequate drainage, the endoscopist aimed to drain both intrahepatic systems. After obtaining informed consent for this procedure, the patient was placed in a supine position under total intravenous anesthesia. A 19-gauge needle was used to puncture through the gastric cardia into hepatic segment II, and a purulent discharge was aspirated. A 0.025 ViZiguide (Terumo Medical Corp., Tokyo, Japan) was then inserted using a tapered-tip sphincterotome (PR-V234Q; Terumo Medical Corp.), and the guidewire was manipulated until it passed from the left through to the right intrahepatic duct (Figure 2). The neo-tract dilation was performed using 7.0, 8.5 and 10.0 Fr Soehendra dilating catheters. A 10 mm × 80 mm uncovered self-expanding metal stent was then inserted and deployed to connect the right and left systems (Figure 2B). Finally, a 10 mm × 100 mm covered self-expanding metal stent was deployed to form the bilo-enteric tract (Figure 3).
There were no immediate postoperative complications, and the patient was transferred to a regular ward. Nil per os was maintained for five days, and in the absence of eventful conditions, the patient was discharged after an additional three days. At the 6-wk follow-up, the patient was doing well with a normal total biliary level (1.2 mg/dL), but elevated alkaline phosphatase (247 U/L).
EUS-guided left system drainage via hepaticogastrostomy is a common procedure with > 90% technical and clinical success rates for patients with obstructive jaundice[11]. Typically, a transmural approach via the stomach is utilized, either by cauterization, non-cauterization/balloon dilation, or graded dilation, followed by stent insertion. In the case presented here, the right and left systems were completely separated by tumor invasion. Therefore, in order to drain the right system, a second stent was bridged across the stricture point at the common hepatic duct. In 2013, Park et al[12] reported a drainage procedure using direct access to the right intrahepatic duct via the duodenal bulb. More recently, Ogura et al[13] reported a case series of 11 patients who underwent right system drainage via a transgastric approach similar to the one reported here, though with the use of different instruments. The results of the present case provide further evidence that EUS-guided bilateral biliary drainage is feasible and effective for patients with hilar cholangiocarcinoma, and can be used as an alternative to percutaneous biliary drainage.
A 77-year-old male patient with type IV malignant hilar obstruction who presented with jaundice and fever.
Malignant tumor obstructing the hilar area causing bilateral biliary system blockage.
Cholangiocarcinoma, hepatocellular carcinoma, or mixed cholangio-hepatocellular carcinoma.
Hyperbilirubinemia with a total bilirubin level of 12.7 mg/dL and direct bilirubin of 11.3 mg/dL, and an elevated alkaline phosphatase level (395 U/L).
Computed tomography revealed a soft tissue mass involving the common hepatic duct and portions of the left intrahepatic duct resulting in upstream dilation of both systems.
Endoscopic ultrasound (EUS)-guided bilateral biliary drainage via a transgastric approach.
EUS-guided hepaticogastrostomy is commonly performed to drain the left system. In contrast, there are few reports demonstrating techniques to drain both intrahepatic systems via a single puncture site.
EUS-guided hepaticogastrostomy is a novel alternative treatment for biliary drainage in patients for whom endoscopic retrograde cholangiopancreatography has failed and who prefer internal rather than percutaneous biliary drainage or surgical bypass procedures.
EUS-guided hepaticogastrostomy for bilateral drainage of both hepatic systems is feasible if the guidewire is successfully manipulated to pass the stricture point from the left system across to the right.
This case report describes the successful use of EUS-guided bilateral biliary drainage in a patient with malignant hilar obstruction.
P- Reviewer: Galasso D, Steinbruck K, Xu Y S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33:898-900. [PubMed] [Cited in This Article: ] |
| 2. | Burmester E, Niehaus J, Leineweber T, Huetteroth T. EUS-cholangio-drainage of the bile duct: report of 4 cases. Gastrointest Endosc. 2003;57:246-251. [PubMed] [Cited in This Article: ] |
| 3. | Artifon EL, Aparicio D, Paione JB, Lo SK, Bordini A, Rabello C, Otoch JP, Gupta K. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46:768-774. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 152] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 4. | Khashab MA, Valeshabad AK, Afghani E, Singh VK, Kumbhari V, Messallam A, Saxena P, El Zein M, Lennon AM, Canto MI. A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci. 2015;60:557-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 145] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 5. | Dhir V, Artifon EL, Gupta K, Vila JJ, Maselli R, Frazao M, Maydeo A. Multicenter study on endoscopic ultrasound-guided expandable biliary metal stent placement: choice of access route, direction of stent insertion, and drainage route. Dig Endosc. 2014;26:430-435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 6. | Gupta K, Perez-Miranda M, Kahaleh M, Artifon EL, Itoi T, Freeman ML, de-Serna C, Sauer B, Giovannini M. Endoscopic ultrasound-assisted bile duct access and drainage: multicenter, long-term analysis of approach, outcomes, and complications of a technique in evolution. J Clin Gastroenterol. 2014;48:80-87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 104] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 7. | Iqbal S, Friedel DM, Grendell JH, Stavropoulos SN. Outcomes of endoscopic-ultrasound-guided cholangiopancreatography: a literature review. Gastroenterol Res Pract. 2013;2013:869214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Artifon EL, Ferreira FC, Sakai P. Endoscopic ultrasound-guided biliary drainage. Korean J Radiol. 2012;13 Suppl 1:S74-S82. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Song TJ, Lee SS, Park do H, Seo DW, Lee SK, Kim MH. Preliminary report on a new hybrid metal stent for EUS-guided biliary drainage (with videos). Gastrointest Endosc. 2014;80:707-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Prachayakul V, Aswakul P. Endoscopic ultrasound-guided biliary drainage as an alternative to percutaneous drainage and surgical bypass. World J Gastrointest Endosc. 2015;7:37-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 16] [Cited by in F6Publishing: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Fabbri C, Luigiano C, Lisotti A, Cennamo V, Virgilio C, Caletti G, Fusaroli P. Endoscopic ultrasound-guided treatments: are we getting evidence based--a systematic review. World J Gastroenterol. 2014;20:8424-8448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 90] [Cited by in F6Publishing: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 12. | Park SJ, Choi JH, Park do H, Choi JH, Lee SS, Seo DW, Lee SK, Kim MH. Expanding indication: EUS-guided hepaticoduodenostomy for isolated right intrahepatic duct obstruction (with video). Gastrointest Endosc. 2013;78:374-380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 13. | Ogura T, Sano T, Onda S, Imoto A, Masuda D, Yamamoto K, Kitano M, Takeuchi T, Inoue T, Higuchi K. Endoscopic ultrasound-guided biliary drainage for right hepatic bile duct obstruction: novel technical tips. Endoscopy. 2015;47:72-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |