Published online Aug 28, 2015. doi: 10.3748/wjg.v21.i32.9656
Peer-review started: April 24, 2015
First decision: May 18, 2015
Revised: June 2, 2015
Accepted: July 8, 2015
Article in press: July 8, 2015
Published online: August 28, 2015
AIM: To investigate the anastomotic complications of esophagojejunostomy (EJS) after laparoscopic total gastrectomy (LTG), we reviewed retrospective studies.
METHODS: A literature search was conducted in PubMed for studies published from January 1, 1994 through January 31, 2015. The search terms included “laparoscopic,”“total gastrectomy,” and “gastric cancer.” First, we selected 16 non-randomized controlled trials (RCTs) comparing LTG with open total gastrectomy (OTG) and conducted an updated meta-analysis of anastomotic complications after total gastrectomy. The Newcastle-Ottawa scoring system (NOS) was used to assess the quality of the non-RCTs included in this study. Next, we reviewed anastomotic complications in 46 case studies of LTG to compare the various procedures for EJS.
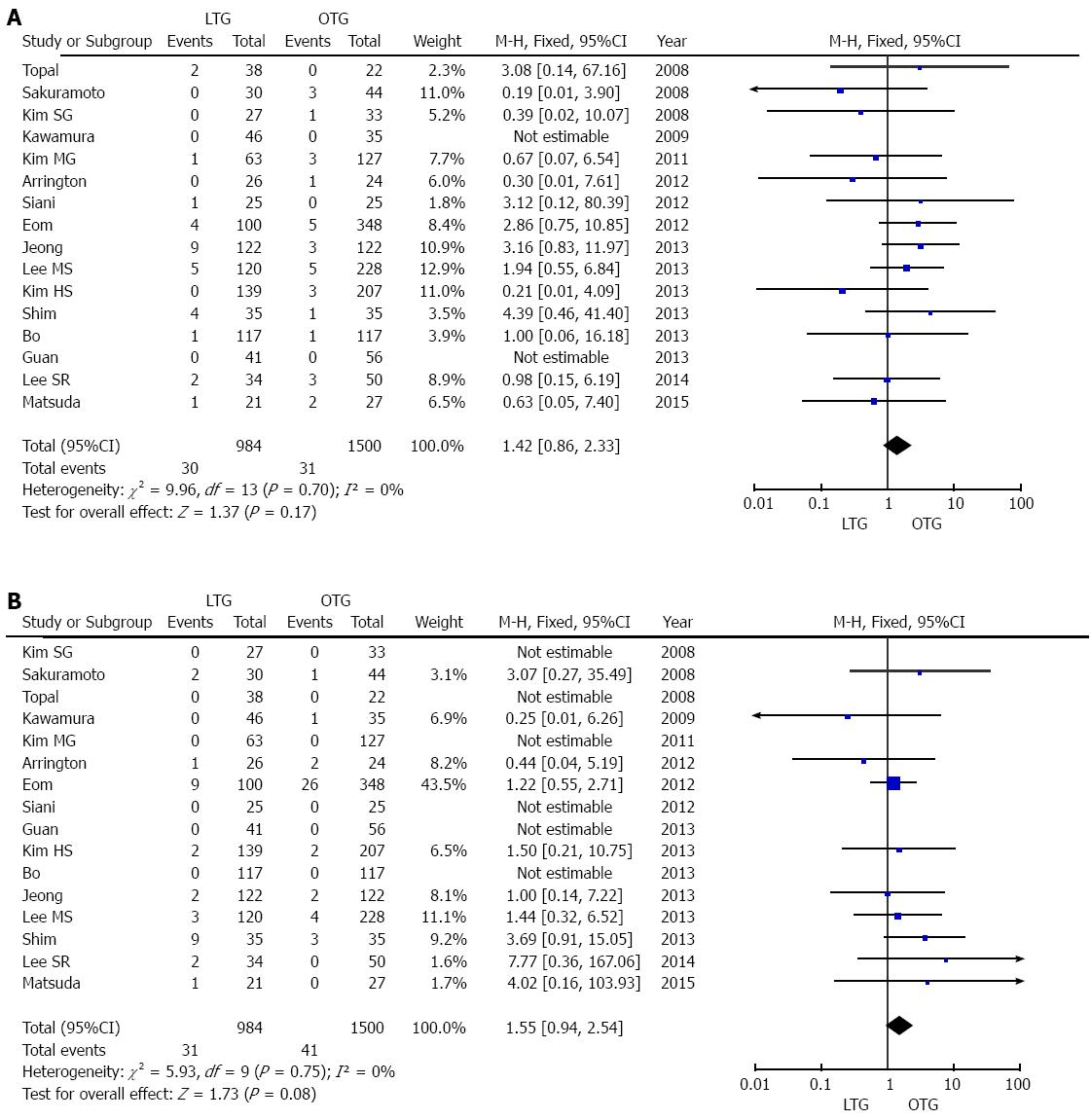
RESULTS: The overall incidence of anastomotic leakage associated with EJS was 3.0% (30 of 984 patients) among LTG procedures and 2.1% (31 of 1500 patients) among OTG procedures in the 16 non-RCTs. The incidence of anastomotic leakage did not differ significantly between LTG and OTG (odds OR = 1.42, 95%CI: 0.86-2.33, P = 0.17, I2 = 0%). Anastomotic stenosis related to EJS was reported in 72 (2.9%) of 2484 patients, and the incidence was 3.2% among LTG procedures and 2.7% among OTG procedures. The incidence of anastomotic stenosis related to EJS was slightly, but not significantly, higher in LTG than in OTG (OR = 1.55, 95%CI: 0.94-2.54, P = 0.08, I2 = 0%). The various procedures for LTG were classified into six categories in the review of case studies of LTG. The incidence of EJS leakage was similar (1.1% to 3.2%), although the incidence of EJS stenosis was relatively high when the OrVilTM device was used (8.8%) compared with other procedures (1.0% to 3.6%).
CONCLUSION: The incidence of anastomotic complications associated with EJS was not different between LTG and OTG. Anastomotic stenosis was relatively common when the OrVilTM device was used.
Core tip: In this updated meta-analysis of non-randomized controlled trials comparing laparoscopic total gastrectomy (LTG) and open total gastrectomy, the incidence of anastomotic leakage was similar, and that of anastomotic stenosis was slightly, but not significantly, higher when LTG was performed. The incidence of anastomotic stenosis was relatively high for new procedures that utilize a trans-orally inserted anvil (OrVilTM) in reported case series of LTG.
- Citation: Inokuchi M, Otsuki S, Fujimori Y, Sato Y, Nakagawa M, Kojima K. Systematic review of anastomotic complications of esophagojejunostomy after laparoscopic total gastrectomy. World J Gastroenterol 2015; 21(32): 9656-9665
- URL: https://www.wjgnet.com/1007-9327/full/v21/i32/9656.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i32.9656
Laparoscopic distal gastrectomy (LDG) is an established minimally invasive procedure for the treatment of gastric cancer, particularly early-stage disease. Several meta-analyses of randomized controlled trials (RCTs) comparing LDG with conventional open distal gastrectomy (ODG) have reported the short-term advantages of LDG, such as less pain, less operative bleeding, and earlier recovery[1-5]. Moreover, LDG was associated with fewer minor postoperative complications, such as wound infection and medical complications, compared with ODG in several meta-analyses, including non-RCTs[6,7]. In contrast, no RCTs comparing laparoscopic total gastrectomy (LTG) with open total gastrectomy (OTG) have been reported, although one RCT compared laparoscopy-assisted gastrectomy including both distal and total gastrectomy with open gastrectomy[8]. Esophagojejunostomy (EJS) after LTG is a complicated procedure requiring extensive experience and a skilled technique, which is a major reason why LTG is not as commonly performed as LDG. However, several meta-analyses of non-RCTs that included patients with mismatched clinical factors have been reported. First, in 2012, Haverkamp et al[9] published a meta-analysis of 8 non-RCTs, showing that LTG was associated with a longer operative time, less blood loss, and a shorter hospital stay than OTG. Postoperative complications did not differ between LTG and OTG in their meta-analysis. Shen et al[10] demonstrated that LTG was associated with a slightly, but not significantly, lower incidence of postoperative complications than OTG. Regarding individual complications, there were slightly lower risks of wound infection and pneumonia with LTG. Chen et al[11] showed that postoperative medical complications were significantly less frequent with LTG than with OTG, but surgical complications were not. In two meta-analyses published in 2014, LTG was shown to result in a longer operative time, less blood loss, lower analgesic use, earlier passage of flatus, quicker resumption of oral intake, earlier hospital discharge, and fewer postoperative complications[12,13]. Regarding individual complications, LTG was associated with fewer wound-related problems than OTG[12].
This review focused on anastomotic complications of EJS after LTG. We conducted a meta-analysis of postoperative anastomotic complications of EJS, such as anastomotic leakage and stenosis, by analyzing the results of non-RCTs that compared LTG with OTG. In addition, we analyzed case series of EJS in conjunction with LTG and evaluated the different procedures used to perform EJS.
First, to conduct this meta-analysis comparing anastomotic complications of EJS between LTG and OTG, a literature search was performed in PubMed for studies published from January 1, 1994 through January 31, 2015. The search terms included “laparoscopic,”“total gastrectomy,” and “gastric cancer.” Reports in languages other than English, reviews, and meta-analyses were excluded. Twenty non-RCTs, but no RCTs, were found. To minimize bias in this meta-analysis of anastomotic complications, we excluded studies that included hand-assisted or robotic approaches, other diseases, and mismatched reconstruction procedures. Four studies were excluded from this meta-analysis for the following reasons. The text of a study by Du et al[14] was not available online; a study by Usui et al[15] included hand-assisted procedures; a study by Kwon et al[16] included robotic surgery; and a study by Mochiki et al[17] included jejunal pouch interposition reconstruction in OTG. The 16 selected non-RCTs are summarized in Table 1. LTG and OTG were compared with regard to anastomotic leakage or stenosis of the EJS.
| Author | Year | Nation | n | Extent of LND1 | Matched factors |
| Kim et al[27] | 2008 | South Korea | 60 | D1 + 8a, 9 | 1, 2, 3, 5, 6, 7 |
| Topal et al[28] | 2008 | Belgium | 60 | D2 | 1, 2, 3, 4, 5, 6, 7 |
| Kawamura et al[29] | 2009 | Japan | 81 | D2-No.10 | 1, 2, 3, 4, 6, 7 |
| Sakuramoto et al[30] | 2009 | Japan | 74 | D1 + 8a, 9/D2-No.10 | 1, 2, 3, 4, 6, 7 |
| Kim et al[31] | 2011 | South Korea | 190 | D2-No.10 | 1, 2, 3, 4, 5, 6, 7 |
| Arrington et al[32] | 2012 | United States | 50 | D0/D1/D2-No.10 | 1, 2, 5, 6, 7 |
| Eom et al[33] | 2012 | South Korea | 448 | D2-No.10 | 4, 6, 7 |
| Siani et al[34] | 2012 | Italy | 50 | D2-No.10 | 1, 2, 5, 6, 7 |
| Bo et al[35] | 2013 | China | 234 | D2-No.10 | 1, 2, 3, 5, 6, 7 |
| Guan et al[36] | 2013 | China | 97 | D2 | 2, 5, 6, 7 |
| Jeong et al[37] | 2013 | South Korea | 244 | D1 + No.8a, 9/D2 | 1, 2, 3, 4, 5, 7 |
| Kim et al[38] | 2013 | South Korea | 346 | D2-No.10 | 1, 2, 3, 4, 5, 6, 7 |
| Lee et al[39] | 2013 | South Korea | 348 | D2 | 1, 2, 4, 6, 7 |
| Shim et al[40] | 2013 | South Korea | 70 | D1 + 8a, 9, 11p/D2 | 1, 2, 5, 6, 7 |
| Lee et al[41] | 2014 | South Korea | 84 | D1 + No.8a, 9, 11p | 1, 2, 5, 6, 7 |
| Matsuda et al[42] | 2015 | Japan | 48 | D1 + No.8a, 9, 11p | 2, 3, 4, 5, 6, 7 |
The Newcastle-Ottawa scoring system (NOS) was used to assess the quality of the non-RCTs[18]. With the NOS, the maximum scores are four points for selection, two for comparability (reconstruction method and the extent of lymphadenectomy), and three for outcome assessment. The studies included in this meta-analysis were of sufficient quality according to the NOS (Table 2).
| Selection | Comparability1 | Exposure | ||||||
| Author | Is the case definition adequate? | Representativeness of the cases | Selection of controls | Definition of controls | of cases and controls on the basis of the design or analysis | Ascertainment of exposure | Same method of ascertainment for cases and controls | Non-responserate |
| Kim et al[27] | * | * | ** | * | * | * | ||
| Topal et al[28] | * | * | ** | * | * | * | ||
| Kawamura et al[29] | * | * | ** | * | * | * | ||
| Sakuramoto et al[30] | * | * | ** | * | * | * | ||
| Kim et al[31] | * | * | ** | * | * | * | ||
| Arrington et al[32] | * | * | ** | * | * | * | ||
| Eom et al[33] | * | * | ** | * | * | * | ||
| Siani et al[34] | * | * | ** | * | * | * | ||
| Bo et al[35] | * | * | ** | * | * | * | ||
| Guan et al[36] | * | * | ** | * | * | * | ||
| Jeong et al[37] | * | * | * | * | * | * | ||
| Kim et al[38] | * | * | ** | * | * | * | ||
| Lee et al[39] | * | * | ** | * | * | * | ||
| Shim et al[40] | * | * | ** | * | * | * | ||
| Lee et al[41] | * | * | ** | * | * | * | ||
| Matsuda et al[42] | * | * | ** | * | * | * |
Second, to review case series reporting anastomotic complications of EJS in LTG, a search of PubMed, performed as described above, yielded 53 case series reports (including more than 10 patients) of LTG that included reconstruction procedures and a results of postoperative anastomotic complications. Several studies partly included comparisons, such as comparisons between LTG and LPG or between different EJS procedures. However, 4 studies were excluded because they also included proximal gastrectomy or other diseases, and 3 studies were excluded because of a suspicion of overlapping data from the same institution. The remaining 46 studies were included in this review (Table 3). We classified anastomotic procedures into the following 6 categories: (1) extracorporeal reconstruction by a single stapling technique using a circular stapler; (2) intracorporeal reconstruction by a single stapling technique using a circular stapler; (3) intracorporeal reconstruction by a double (or hemi-double) stapling technique using a circular stapler with a trans-abdominally inserted anvil (DST/HDST); (4) intracorporeal reconstruction by a double (or hemi-double) stapling technique using a circular stapler with a trans-orally inserted anvil (OrVilTM) (DST/HDST by TOA); (5) intracorporeal reconstruction by side-to-side anastomosis using a linear stapler; and (6) intracorporeal reconstruction by functional end-to-end anastomosis using linear staplers.
| Author | Year | Country | n | EJS leakage | EJS stenosis |
| Extracorporeal SST | |||||
| Hur et al[43] | 2008 | South Korea | 18 | 0 (0) | 0 (0) |
| Lee et al[44] | 2009 | South Korea | 67 | 1 (1.5) | 6 (9.0) |
| Kunisaki et al[45] | 2011 | Japan | 15 | 1 (6.7) | 0 (0) |
| Yoon et al[46] | 2012 | South Korea | 65 | 3 (4.6) | 3 (4.6) |
| Mou et al[47] | 2013 | China | 12 | 0 (0) | 0 (0) |
| Jung et al[48] | 2013 | South Korea | 47 | 2 (4.3) | 2 (4.3) |
| Li et al[49] | 2014 | China | 108 | 1 (0.9) | 0 (0) |
| Sahoo et al[50] | 2014 | India | 47 | 0 (0) | 0 (0) |
| Total | 379 | 8 (2.1) | 11 (2.9) | ||
| Intracorporeal SST with trans-abdominally inserted anvil | |||||
| Usui et al[51] | 2008 | Japan | 15 | 0 (0) | 0 (0) |
| Kinoshita et al[52] | 2010 | Japan | 10 | 0 (0) | 0 (0) |
| Lee et al[53] | 2012 | South Korea | 88 | 3 (3.4) | 0 (0) |
| Shim et al[54] | 2013 | South Korea | 12 | 2 (17) | 5 (42) |
| Kim et al[55] | 2013 | South Korea | 36 | 0 (0) | 0 (0) |
| Yoshikawa et al[56] | 2013 | Japan | 20 | 0 (0) | 0 (0) |
| Du et al[57] | 2013 | China | 52 | 0 (0) | 0 (0) |
| Total | 233 | 5 (2.1) | 5 (2.1) | ||
| Intracorporeal HDST/DST with trans-abdominally inserted anvil | |||||
| Omori et al[58] | 2009 | Japan | 10 | 0 (0) | 0 (0) |
| Nunobe et al[59] | 2011 | Japan | 41 | 2 (4.9) | 3 (7.3) |
| Shim et al[54] | 2013 | South Korea | 14 | 1 (7.1) | 1 (7.1) |
| Lafemina et al[60] | 2013 | United States | 17 | 1 (5.9) | 1 (5.9) |
| Muguruma et al[61] | 2014 | Japan | 32 | 0 (0) | 0 (0) |
| Zhao et al[62] | 2014 | China | 26 | 0 (0) | 0 (0) |
| Total | 140 | 4 (2.9) | 5 (3.6) | ||
| Intracorporeal HDST/DST with trans-orally inserted anvil | |||||
| Jeong et al[63] | 2009 | South Korea | 16 | 0 (0) | 0 (0) |
| Kachikwu et al[64] | 2011 | United States | 16 | 0 (0) | 3 (19) |
| Kunisaki et al[45] | 2011 | Japan | 30 | 1 (3.3) | 0 (0) |
| Marangoni et al[65] | 2012 | United Kingdom | 13 | 0 (0) | 0 (0) |
| Liao et al[66] | 2013 | China | 27 | 1 (3.7) | 1 (3.7) |
| Shim et al[54] | 2013 | South Korea | 12 | 2 (17) | 4 (33) |
| Xie et al[67] | 2013 | China | 28 | 0 (0) | 0 (0) |
| Zuiki et al[25] | 2013 | Japan | 52 | 1 (1.9) | 11 (21) |
| Hiyoshi et al[68] | 2014 | Japan | 21 | 2 (9.5) | 0 (0) |
| Total | 215 | 7 (3.2) | 19 (8.8) | ||
| Intracorporeal STSA | |||||
| Huscher et al[69] | 2007 | Italy | 11 | 0 (0) | 0 (0) |
| Inaba et al[70] | 2010 | Japan | 53 | 2 (3.8) | 0 (0) |
| Bracale et al[71] | 2010 | Italy | 67 | 4 (6.0) | 2 (3.0) |
| Tsujimoto et al[72] | 2012 | Japan | 15 | 0 (0) | 0 (0) |
| Nagai et al[73] | 2013 | Japan | 94 | 2 (2.1) | 0 (0) |
| Petersen et al[74] | 2013 | Denmark | 30 | 3 (10) | 0 (0) |
| Shim et al[54] | 2013 | South Korea | 10 | 0 (0) | 1 (10) |
| Morimoto et al[75] | 2014 | Japan | 77 | 0 (0) | 1 (1.3) |
| Yamamoto et al[76] | 2014 | Japan | 52 | 1 (1.9) | 0 (0) |
| Total | 409 | 12 (2.9) | 4 (1.0) | ||
| Intracorporeal FETEA | |||||
| Ziqiang et al[77] | 2008 | China | 14 | 0 (0) | 0 (0) |
| Kim et al[78] | 2012 | South Korea | 124 | 3 (2.4) | 6 (4.8) |
| Kim et al[79] | 2013 | South Korea | 139 | 1 (0.7) | 1 (0.7) |
| Ebihara et al[80] | 2013 | Japan | 65 | 0 (0) | 3 (4.6) |
| Hiyoshi et al[68] | 2014 | Japan | 24 | 0 (0) | 0 (0) |
| Tsunoda et al[81] | 2014 | Japan | 97 | 1 (1.0) | 0 (0) |
| Total | 463 | 5 (1.1) | 10 (2.2) | ||
Review Manager software, version 5.2 (Cochrane Collaboration, Oxford, United Kingdom), was used to perform this meta-analysis. For discontinuous variables, each postoperative complication was extracted from the trial report; odds ratios (ORs) were calculated from the total number of patients and the observed numbers of events of interest in all groups using a random-effects model. In the tables of our results, squares indicate point estimates of ORs, with 95% confidential intervals (CIs) indicated by horizontal bars. The diamonds represent the summary ORs with 95%CIs from the included studies. P values < 0.05 were considered to indicate statistical significance.
The I2 statistic was used to quantitatively assess heterogeneity. Graphical exploration with funnel plots was used to evaluate publication bias. Publication bias was assessed on the basis of the funnel plot of the included studies.
This meta-analysis included a total of 2484 patients, 984 of whom underwent LTG and 1500 of whom underwent OTG. Anastomotic leakage of EJS was reported in 61 (2.5%) of 2484 patients in the 16 studies. The overall incidence of anastomotic leakage of EJS was 3.0% (30 of 984 patients) with LTG and 2.1% (31 of 1500 patients) with OTG in the 16 studies. The incidence of anastomotic leakage did not differ significantly between LTG and OTG (Figure 1A). Anastomotic stenosis of EJS was reported in 72 (2.9%) of the 2484 patients, and the incidence was 3.2% with LTG and 2.7% with OTG. The incidence of anastomotic stenosis of EJS was slightly, but not significantly, higher in LTG than in OTG (Figure 1B). Publication bias was assessed for each complication using the funnel plot of the included studies. No complications were associated with publication bias, and a symmetric distribution was maintained with all of the studies lying within the 95%CI (data not shown).
In the review of the case series, the overall incidence of anastomotic leakage of EJS in the 46 studies was 2.2% (41 of 1839). The incidences of EJS leakage according to the anastomotic procedure are also shown in Table 3. The overall incidence of anastomotic stenosis of EJS was 2.9% (54 of 1839). The incidences of anastomotic stenosis according to the anastomotic procedure are also shown in Table 3. It was relatively common with the DST/HDST by TOA procedure.
In this updated meta-analysis, the incidence of anastomotic leakage of EJS did not differ significantly between LTG and OTG. This outcome was consistent with the findings of previous meta-analyses by Wang et al[12,19]. The incidence of anastomotic leakage of EJS after TG in our review was not higher than that in other studies of OTG, which have reported incidences of 1.0% to 2.1%[20-22]. The Japanese National Clinical Database (NCD) of digestive surgery reported that the incidence of anastomotic leakage after total gastrectomy was 4.4% (881 of 20011) in 2011[23]. Detailed information, specifically on LTG or OTG, was unavailable. Most of the leaks must have occurred at the EJS in that study. Diverse anastomotic procedures have been reported in studies of LTG. In our review, the incidence of anastomotic leakage of EJS was similar between the various procedures.
In our study, the incidence of anastomotic stenosis of EJS was slightly, but not significantly, higher with LTG than with OTG. One problem was that EJS stenosis was not clearly defined in many of the studies included in our analysis. EJS stenosis was not graded based on a standardized assessment, such as the Clavien-Dindo classification. Therefore, it was unclear whether endoscopic dilation or reoperation was performed in all of the patients diagnosed with EJS stenosis. Another problem was that EJS stenosis often occurred several weeks or months after LTG. Therefore, an accurate incidence of anastomotic stenosis was not shown among the short-term outcomes of LTG, and anastomotic stenosis was not mentioned in the NCD report. In our review of case-series studies, the incidence of anastomotic stenosis was higher among the procedures performed using the OrVilTM device. In a review by Umemura et al[24] comparing procedures used to perform EJS after LTG, the use of circular staplers was significantly associated with higher incidences of both anastomotic leakage (4.7%) and stenosis (8.3%) compared with the use of linear staplers (1.1% and 1.8%, respectively). Even in our analysis, linear stapler methods apparently reduced the risk of stenosis. An anastomotic site formed by a linear stapler could probably secure a wider diameter than one formed by a circular stapler[24]. As another investigator insisted, the high incidence of anastomotic stenosis after DST/HDST may be explained by the following causes: excessive tension at the anastomotic site and focal ischemia at the site where the two staple lines overlap[25]. In the study of the OrvilTM device, which was associated with the highest incidence of anastomotic stenosis, the use of a circular stapler with a smaller size (21 mm) significantly increased the rate of EJS anastomosis compared with the use of a normal-sized stapler (25 mm)[25]. To pass the anvil head of OrvilTM easily through the esophageal entrance, the smaller anvil was probably used in some cases in that study. In OTG, the use of a circular stapler with a small diameter (21 mm) was a significant risk factor for EJS stenosis[26]. Both the DST/HDST procedure and the use of a smaller circular stapler could increase the stenosis in the EJS when the OrvilTM device is used. However, several studies on the use of OrvilTM have shown favorable results. Anastomotic complications may be closely associated with learning curves of surgeons[25]. Therefore, they will probably decrease in any procedures as surgeons acquire more experience and improve their technical skills in performing EJS.
In addition, the value of meta-analyses of non-RCTs remains controversial, as non-RCTs often include groups of patients who are mismatched with respect to background characteristics. Our meta-analysis also had limitations despite the inclusion of studies in which the patients were matched as closely as possible. To draw definitive conclusions, prospective studies are needed to clarify the usefulness of LTG. A prospective phase II study of LTG or laparoscopic proximal gastrectomy has begun in Japan, with anastomotic leakage as the primary endpoint. The problems currently associated with EJS after LTG are an important concern. However, the postoperative outcomes of EJS are expected to improve in the future with increased experience and enhanced surgical skills.
In conclusion, the incidences of anastomotic complications of EJS were similar in this meta-analysis comparing LTG and OTG. In case studies of LTG, the incidence of anastomotic leakage of EJS was not different between various anastomotic procedures, although anastomotic stenosis was relatively common in the DST/HDST by TOA procedure.
Esophagojejunostomy (EJS) after laparoscopic total gastrectomy (LTG) is a complicated procedure requiring extensive experience and a skilled technique, which is a major reason why LTG is not as commonly performed as laparoscopic distal gastrectomy. No randomized controlled trials (RCTs) comparing LTG with open total gastrectomy (OTG) has been reported yet. Several meta-analyses of non-RCTs, including patients with mismatched clinical factors, have been reported.
Anastomotic complication was a major issue in LTG. Various anastomotic procedures of EJS have been attempted for EJS in LTG. Anastomotic methods were roughly categorized into two groups; circular stapler method had been usually performed in OTG, and linear stapler method developed in LTG.
This meta-analysis of non-RCT of LTG vs OTG was updated, and several non-RCTs were excluded due to including hand-assisted or robotic approaches, other diseases, and mismatched reconstruction procedures. Furthermore, we reviewed case series of LTG, and categorized various anastomotic methods of EJS into the following six procedures: (1) extracorporeal reconstruction by single stapling technique using a circular stapler; (2) intracorporeal reconstruction by single stapling technique using a circular stapler; (3) intracorporeal reconstruction by double (or hemi-double) stapling technique using a circular stapler with a trans-abdominally inserted anvil (DST/HDST); (4) intracorporeal reconstruction by double (or hemi-double) stapling technique using a circular stapler with a trans-orally inserted anvil (OrVilTM) (DST/HDST by TOA); (5) intracorporeal reconstruction by side-to-side anastomosis using a linear stapler; and (6) intracorporeal reconstruction by functional end-to-end anastomosis using linear staplers.
The incidence of anastomotic leakage of EJS was similar between LTG and OTG, although that of anastomotic stenosis was slightly, but not significantly, higher with LTG than with OTG. In case series of LTG, the incidence of anastomotic leakage of EJS was not different in various anastomotic procedures, although anastomotic stenosis was slightly higher in the procedure of DST/HDST by TOA.
Single stapling technique of EJS is the following procedure. The purse-string suture is placed in distal esophageal stump. The anvil head of a circular stapler is inserted into the esophageal lumen. The circular stapler is inserted into the distal limb of the jejunum. The circular stapler is combined with the anvil head, and EJS is performed. In double or hemi-double stapling technique, abdominal esophagus is cut by a linear stapler, and EJS is performed by a circular stapler. The anvil head is inserted trans-abdominally before esophageal transection. However, OrVilTM is a device including a trans-orally inserted anvil. The anvil head of OrVilTM connected with gastric tube is inserted through pharynx and esophageal entrance intraoperatively. Side-to-side anastomosis is performed peristaltically by a linear stapler. Functional end-to-end anastomosis is performed anti-peristaltically, and the entry hall is closed by a linear stapler.
This paper is an interesting article. Perhaps the only drawback is that there is not any RCT study, but it has been correctly referred.
P- Reviewer: Kawabata Y, Lara FJP S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Memon MA, Khan S, Yunus RM, Barr R, Memon B. Meta-analysis of laparoscopic and open distal gastrectomy for gastric carcinoma. Surg Endosc. 2008;22:1781-1789. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Chen XZ, Hu JK, Yang K, Wang L, Lu QC. Short-term evaluation of laparoscopy-assisted distal gastrectomy for predictive early gastric cancer: a meta-analysis of randomized controlled trials. Surg Laparosc Endosc Percutan Tech. 2009;19:277-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Ohtani H, Tamamori Y, Noguchi K, Azuma T, Fujimoto S, Oba H, Aoki T, Minami M, Hirakawa K. A meta-analysis of randomized controlled trials that compared laparoscopy-assisted and open distal gastrectomy for early gastric cancer. J Gastrointest Surg. 2010;14:958-964. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 4. | Kodera Y, Fujiwara M, Ohashi N, Nakayama G, Koike M, Morita S, Nakao A. Laparoscopic surgery for gastric cancer: a collective review with meta-analysis of randomized trials. J Am Coll Surg. 2010;211:677-686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Liang Y, Li G, Chen P, Yu J, Zhang C. Laparoscopic versus open gastrectomy for early distal gastric cancer: a meta-analysis. ANZ J Surg. 2011;81:673-680. [PubMed] [Cited in This Article: ] |
| 6. | Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012;255:446-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 277] [Cited by in F6Publishing: 297] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 7. | Inokuchi M, Sugita H, Otsuki S, Sato Y, Nakagawa M, Kojima K. Laparoscopic distal gastrectomy reduced surgical site infection as compared with open distal gastrectomy for gastric cancer in a meta-analysis of both randomized controlled and case-controlled studies. Int J Surg. 2015;15:61-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Cai J, Wei D, Gao CF, Zhang CS, Zhang H, Zhao T. A prospective randomized study comparing open versus laparoscopy-assisted D2 radical gastrectomy in advanced gastric cancer. Dig Surg. 2011;28:331-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Haverkamp L, Weijs TJ, van der Sluis PC, van der Tweel I, Ruurda JP, van Hillegersberg R. Laparoscopic total gastrectomy versus open total gastrectomy for cancer: a systematic review and meta-analysis. Surg Endosc. 2013;27:1509-1520. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 138] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 10. | Shen H, Shan C, Liu S, Qiu M. Laparoscopy-assisted versus open total gastrectomy for gastric cancer: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2013;23:832-840. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Chen K, Xu XW, Zhang RC, Pan Y, Wu D, Mou YP. Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer. World J Gastroenterol. 2013;19:5365-5376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 59] [Cited by in F6Publishing: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Xiong JJ, Nunes QM, Huang W, Tan CL, Ke NW, Xie SM, Ran X, Zhang H, Chen YH, Liu XB. Laparoscopic vs open total gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19:8114-8132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 53] [Cited by in F6Publishing: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 13. | Wang W, Zhang X, Shen C, Zhi X, Wang B, Xu Z. Laparoscopic versus open total gastrectomy for gastric cancer: an updated meta-analysis. PLoS One. 2014;9:e88753. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Du J, Zheng J, Li Y, Li J, Ji G, Dong G, Yang Z, Wang W, Gao Z. Laparoscopy-assisted total gastrectomy with extended lymph node resection for advanced gastric cancer--reports of 82 cases. Hepatogastroenterology. 2010;57:1589-1594. [PubMed] [Cited in This Article: ] |
| 15. | Usui S, Yoshida T, Ito K, Hiranuma S, Kudo SE, Iwai T. Laparoscopy-assisted total gastrectomy for early gastric cancer: comparison with conventional open total gastrectomy. Surg Laparosc Endosc Percutan Tech. 2005;15:309-314. [PubMed] [Cited in This Article: ] |
| 16. | Kwon Y, Cho SI, Kwon YJ, Yang KS, Jang YJ, Kim JH, Park SH, Mok YJ, Park S. Safety of transorally-inserted anvil for esophagojejunostomy in laparoscopic total gastrectomy. Eur J Surg Oncol. 2014;40:330-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Mochiki E, Kamimura H, Haga N, Asao T, Kuwano H. The technique of laparoscopically assisted total gastrectomy with jejunal interposition for early gastric cancer. Surg Endosc. 2002;16:540-544. [PubMed] [Cited in This Article: ] |
| 18. | Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Cited in This Article: ] |
| 19. | Wang W, Li Z, Tang J, Wang M, Wang B, Xu Z. Laparoscopic versus open total gastrectomy with D2 dissection for gastric cancer: a meta-analysis. J Cancer Res Clin Oncol. 2013;139:1721-1734. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Deguchi Y, Fukagawa T, Morita S, Ohashi M, Saka M, Katai H. Identification of risk factors for esophagojejunal anastomotic leakage after gastric surgery. World J Surg. 2012;36:1617-1622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 21. | Nomura S, Sasako M, Katai H, Sano T, Maruyama K. Decreasing complication rates with stapled esophagojejunostomy following a learning curve. Gastric Cancer. 2000;3:97-101. [PubMed] [Cited in This Article: ] |
| 22. | Hyodo M, Hosoya Y, Hirashima Y, Haruta H, Kurashina K, Saito S, Yokoyama T, Arai W, Zuiki T, Yasuda Y. Minimum leakage rate (0.5%) of stapled esophagojejunostomy with sacrifice of a small part of the jejunum after total gastrectomy in 390 consecutive patients. Dig Surg. 2007;24:169-172. [PubMed] [Cited in This Article: ] |
| 23. | Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, Nakagoe T, Shimada M, Kitagawa Y, Sugihara K. Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet-based database. Ann Surg. 2014;260:1034-1039. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 140] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 24. | Umemura A, Koeda K, Sasaki A, Fujiwara H, Kimura Y, Iwaya T, Akiyama Y, Wakabayashi G. Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg. 2015;38:102-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | Zuiki T, Hosoya Y, Kaneda Y, Kurashina K, Saito S, Ui T, Haruta H, Hyodo M, Sata N, Lefor AT. Stenosis after use of the double-stapling technique for reconstruction after laparoscopy-assisted total gastrectomy. Surg Endosc. 2013;27:3683-3689. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 26. | Fukagawa T, Gotoda T, Oda I, Deguchi Y, Saka M, Morita S, Katai H. Stenosis of esophago-jejuno anastomosis after gastric surgery. World J Surg. 2010;34:1859-1863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Kim SG, Lee YJ, Ha WS, Jung EJ, Ju YT, Jeong CY, Hong SC, Choi SK, Park ST, Bae K. LATG with extracorporeal esophagojejunostomy: is this minimal invasive surgery for gastric cancer? J Laparoendosc Adv Surg Tech A. 2008;18:572-578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Topal B, Leys E, Ectors N, Aerts R, Penninckx F. Determinants of complications and adequacy of surgical resection in laparoscopic versus open total gastrectomy for adenocarcinoma. Surg Endosc. 2008;22:980-984. [PubMed] [Cited in This Article: ] |
| 29. | Kawamura H, Yokota R, Homma S, Kondo Y. Comparison of invasiveness between laparoscopy-assisted total gastrectomy and open total gastrectomy. World J Surg. 2009;33:2389-2395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Sakuramoto S, Kikuchi S, Futawatari N, Katada N, Moriya H, Hirai K, Yamashita K, Watanabe M. Laparoscopy-assisted pancreas- and spleen-preserving total gastrectomy for gastric cancer as compared with open total gastrectomy. Surg Endosc. 2009;23:2416-2423. [PubMed] [Cited in This Article: ] |
| 31. | Kim MG, Kim BS, Kim TH, Kim KC, Yook JH, Kim BS. The effects of laparoscopic assisted total gastrectomy on surgical outcomes in the treatment of gastric cancer. J Korean Surg Soc. 2011;80:245-250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Arrington AK, Nelson R, Chen SL, Ellenhorn JD, Garcia-Aguilar J, Kim J. The evolution of surgical technique for total gastrectomy over a 12-year period: a single institution’s experience. Am Surg. 2012;78:1054-1058. [PubMed] [Cited in This Article: ] |
| 33. | Eom BW, Kim YW, Lee SE, Ryu KW, Lee JH, Yoon HM, Cho SJ, Kook MC, Kim SJ. Survival and surgical outcomes after laparoscopy-assisted total gastrectomy for gastric cancer: case-control study. Surg Endosc. 2012;26:3273-3281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Siani LM, Ferranti F, De Carlo A, Quintiliani A. Completely laparoscopic versus open total gastrectomy in stage I-III/C gastric cancer: safety, efficacy and five-year oncologic outcome. Minerva Chir. 2012;67:319-326. [PubMed] [Cited in This Article: ] |
| 35. | Bo T, Peiwu Y, Feng Q, Yongliang Z, Yan S, Yingxue H, Huaxing L. Laparoscopy-assisted vs. open total gastrectomy for advanced gastric cancer: long-term outcomes and technical aspects of a case-control study. J Gastrointest Surg. 2013;17:1202-1208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 36. | Guan G, Jiang W, Chen Z, Liu X, Lu H, Zhang X. Early results of a modified splenic hilar lymphadenectomy in laparoscopy-assisted total gastrectomy for gastric cancer with stage cT1-2: a case-control study. Surg Endosc. 2013;27:1923-1931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Jeong O, Jung MR, Kim GY, Kim HS, Ryu SY, Park YK. Comparison of short-term surgical outcomes between laparoscopic and open total gastrectomy for gastric carcinoma: case-control study using propensity score matching method. J Am Coll Surg. 2013;216:184-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 38. | Kim HS, Kim BS, Lee IS, Lee S, Yook JH, Kim BS. Comparison of totally laparoscopic total gastrectomy and open total gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A. 2013;23:323-331. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 39. | Lee MS, Lee JH, Park do J, Lee HJ, Kim HH, Yang HK. Comparison of short- and long-term outcomes of laparoscopic-assisted total gastrectomy and open total gastrectomy in gastric cancer patients. Surg Endosc. 2013;27:2598-2605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 40. | Shim JH, Oh SI, Yoo HM, Jeon HM, Park CH, Song KY. Short-term outcomes of laparoscopic versus open total gastrectomy: a matched-cohort study. Am J Surg. 2013;206:346-351. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 41. | Lee SR, Kim HO, Son BH, Shin JH, Yoo CH. Laparoscopic-assisted total gastrectomy versus open total gastrectomy for upper and middle gastric cancer in short-term and long-term outcomes. Surg Laparosc Endosc Percutan Tech. 2014;24:277-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 42. | Matsuda T, Iwasaki T, Mitsutsuji M, Hirata K, Maekawa Y, Tsugawa D, Sugita Y, Shimada E, Kakeji Y. Surgical outcomes of intracorporeal circular-stapled esophagojejunostomy using modified over-and-over suture technique in laparoscopic total gastrectomy. Surg Endosc. 2015;Epub ahead of print. [PubMed] [Cited in This Article: ] |
| 43. | Hur H, Jeon HM, Kim W. Laparoscopic pancreas- and spleen-preserving D2 lymph node dissection in advanced (cT2) upper-third gastric cancer. J Surg Oncol. 2008;97:169-172. [PubMed] [Cited in This Article: ] |
| 44. | Lee SE, Ryu KW, Nam BH, Lee JH, Kim YW, Yu JS, Cho SJ, Lee JY, Kim CG, Choi IJ. Technical feasibility and safety of laparoscopy-assisted total gastrectomy in gastric cancer: a comparative study with laparoscopy-assisted distal gastrectomy. J Surg Oncol. 2009;100:392-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 45. | Kunisaki C, Makino H, Oshima T, Fujii S, Kimura J, Takagawa R, Kosaka T, Akiyama H, Morita S, Endo I. Application of the transorally inserted anvil (OrVil) after laparoscopy-assisted total gastrectomy. Surg Endosc. 2011;25:1300-1305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 46. | Yoon HM, Kim YW, Lee JH, Ryu KW, Eom BW, Park JY, Choi IJ, Kim CG, Lee JY, Cho SJ. Robot-assisted total gastrectomy is comparable with laparoscopically assisted total gastrectomy for early gastric cancer. Surg Endosc. 2012;26:1377-1381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 47. | Mou TY, Hu YF, Yu J, Liu H, Wang YN, Li GX. Laparoscopic splenic hilum lymph node dissection for advanced proximal gastric cancer: a modified approach for pancreas- and spleen-preserving total gastrectomy. World J Gastroenterol. 2013;19:4992-4999. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 15] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 48. | Jung YJ, Kim DJ, Lee JH, Kim W. Safety of intracorporeal circular stapling esophagojejunostomy using trans-orally inserted anvil (OrVil) following laparoscopic total or proximal gastrectomy - comparison with extracorporeal anastomosis. World J Surg Oncol. 2013;11:209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 49. | Li P, Huang CM, Zheng CH, Xie JW, Wang JB, Lin JX, Lu J, Wang Y, Chen QY. Laparoscopic spleen-preserving splenic hilar lymphadenectomy in 108 consecutive patients with upper gastric cancer. World J Gastroenterol. 2014;20:11376-11383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 50. | Sahoo MR, Gowda MS, Kumar AT. Early rehabilitation after surgery program versus conventional care during perioperative period in patients undergoing laparoscopic assisted total gastrectomy. J Minim Access Surg. 2014;10:132-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 51. | Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K. Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer. 2008;11:233-237. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 52. | Kinoshita T, Oshiro T, Ito K, Shibasaki H, Okazumi S, Katoh R. Intracorporeal circular-stapled esophagojejunostomy using hand-sewn purse-string suture after laparoscopic total gastrectomy. Surg Endosc. 2010;24:2908-2912. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 53. | Lee JH, Ahn SH, Park do J, Kim HH, Lee HJ, Yang HK. Laparoscopic total gastrectomy with D2 lymphadenectomy for advanced gastric cancer. World J Surg. 2012;36:2394-2399. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 54. | Shim JH, Yoo HM, Oh SI, Nam MJ, Jeon HM, Park CH, Song KY. Various types of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer. Gastric Cancer. 2013;16:420-427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 55. | Kim HI, Cho I, Jang DS, Hyung WJ. Intracorporeal esophagojejunostomy using a circular stapler with a new purse-string suture technique during laparoscopic total gastrectomy. J Am Coll Surg. 2013;216:e11-e16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 56. | Yoshikawa T, Hayashi T, Aoyama T, Cho H, Fujikawa H, Shirai J, Hasegawa S, Yamada T, Oshima T, Yukawa N. Laparoscopic esophagojejunostomy using the EndoStitch and a circular stapler under a direct view created by the ENDOCAMELEON. Gastric Cancer. 2013;16:609-614. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 57. | Du J, Shuang J, Li J, Li J, Hua J. Intracorporeal circular-stapled esophagojejunostomy after laparoscopic total gastrectomy: a novel self-pulling and holding purse-string suture technique. J Am Coll Surg. 2014;218:e67-e72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 58. | Omori T, Oyama T, Mizutani S, Tori M, Nakajima K, Akamatsu H, Nakahara M, Nishida T. A simple and safe technique for esophagojejunostomy using the hemidouble stapling technique in laparoscopy-assisted total gastrectomy. Am J Surg. 2009;197:e13-e17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 59. | Nunobe S, Hiki N, Tanimura S, Kubota T, Kumagai K, Sano T, Yamaguchi T. Three-step esophagojejunal anastomosis with atraumatic anvil insertion technique after laparoscopic total gastrectomy. J Gastrointest Surg. 2011;15:1520-1525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 60. | LaFemina J, Viñuela EF, Schattner MA, Gerdes H, Strong VE. Esophagojejunal reconstruction after total gastrectomy for gastric cancer using a transorally inserted anvil delivery system. Ann Surg Oncol. 2013;20:2975-2983. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 61. | Muguruma K, Tanaka H, Sakurai K, Toyokawa T, Kubo N, Yamashita Y, Sawada T, Ohira M, Hirakawa K. Laparoscopy-assisted total gastrectomy: a simplified approach. Int Surg. 2014;99:79-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 62. | Zhao YL, Su CY, Li TF, Qian F, Luo HX, Yu PW. Novel method for esophagojejunal anastomosis after laparoscopic total gastrectomy: semi-end-to-end anastomosis. World J Gastroenterol. 2014;20:13556-13562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 63. | Jeong GA, Cho GS, Kim HH, Lee HJ, Ryu SW, Song KY. Laparoscopy-assisted total gastrectomy for gastric cancer: a multicenter retrospective analysis. Surgery. 2009;146:469-474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 64. | Kachikwu EL, Trisal V, Kim J, Pigazzi A, Ellenhorn JD. Minimally invasive total gastrectomy for gastric cancer: a pilot series. J Gastrointest Surg. 2011;15:81-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 65. | Marangoni G, Villa F, Shamil E, Botha AJ. OrVil™-assisted anastomosis in laparoscopic upper gastrointestinal surgery: friend of the laparoscopic surgeon. Surg Endosc. 2012;26:811-817. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 66. | Liao GQ, Ou XW, Liu SQ, Zhang SR, Huang W. Laparoscopy-assisted total gastrectomy with trans-orally inserted anvil (OrVil™): a single institution experience. World J Gastroenterol. 2013;19:755-760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 26] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 67. | Xie JW, Huang CM, Zheng CH, Li P, Wang JB, Lin JX, Jun L. A safe anastomotic technique of using the transorally inserted anvil (OrVil) in Roux-en-Y reconstruction after laparoscopy-assisted total gastrectomy for proximal malignant tumors of the stomach. World J Surg Oncol. 2013;11:256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 68. | Hiyoshi Y, Oki E, Ando K, Ito S, Saeki H, Morita M, Baba H, Maehara Y. Outcome of esophagojejunostomy during totally laparoscopic total gastrectomy: a single-center retrospective study. Anticancer Res. 2014;34:7227-7232. [PubMed] [Cited in This Article: ] |
| 69. | Huscher CG, Mingoli A, Sgarzini G, Brachini G, Binda B, Di Paola M, Ponzano C. Totally laparoscopic total and subtotal gastrectomy with extended lymph node dissection for early and advanced gastric cancer: early and long-term results of a 100-patient series. Am J Surg. 2007;194:839-44; discussion 844. [PubMed] [Cited in This Article: ] |
| 70. | Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, Uyama I. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg. 2010;211:e25-e29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 167] [Cited by in F6Publishing: 178] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 71. | Bracale U, Marzano E, Nastro P, Barone M, Cuccurullo D, Cutini G, Corcione F, Pignata G. Side-to-side esophagojejunostomy during totally laparoscopic total gastrectomy for malignant disease: a multicenter study. Surg Endosc. 2010;24:2475-2479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 72. | Tsujimoto H, Uyama I, Yaguchi Y, Kumano I, Takahata R, Matsumoto Y, Yoshida K, Horiguchi H, Aosasa S, Ono S. Outcome of overlap anastomosis using a linear stapler after laparoscopic total and proximal gastrectomy. Langenbecks Arch Surg. 2012;397:833-840. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 73. | Nagai E, Ohuchida K, Nakata K, Miyasaka Y, Maeyama R, Toma H, Shimizu S, Tanaka M. Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery. 2013;153:732-738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 74. | Petersen TI, Pahle E, Sommer T, Zilling T. Laparoscopic minimally invasive total gastrectomy with linear stapled oesophagojejunostomy--experience from the first thirty procedures. Anticancer Res. 2013;33:3269-3273. [PubMed] [Cited in This Article: ] |
| 75. | Morimoto M, Kitagami H, Hayakawa T, Tanaka M, Matsuo Y, Takeyama H. The overlap method is a safe and feasible for esophagojejunostomy after laparoscopic-assisted total gastrectomy. World J Surg Oncol. 2014;12:392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 76. | Yamamoto M, Zaima M, Yamamoto H, Harada H, Kawamura J, Yamaguchi T. A modified overlap method using a linear stapler for intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. Hepatogastroenterology. 2014;61:543-548. [PubMed] [Cited in This Article: ] |
| 77. | Ziqiang W, ZhiMin C, Jun C, Xiao L, Huaxing L, PeiWu Y. A modified method of laparoscopic side-to-side esophagojejunal anastomosis: report of 14 cases. Surg Endosc. 2008;22:2091-2094. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 78. | Kim HS, Kim MG, Kim BS, Lee IS, Lee S, Yook JH, Kim BS. Comparison of totally laparoscopic total gastrectomy and laparoscopic-assisted total gastrectomy methods for the surgical treatment of early gastric cancer near the gastroesophageal junction. J Laparoendosc Adv Surg Tech A. 2013;23:204-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 79. | Kim HS, Kim BS, Lee S, Lee IS, Yook JH, Kim BS. Reconstruction of esophagojejunostomies using endoscopic linear staplers in totally laparoscopic total gastrectomy: report of 139 cases in a large-volume center. Surg Laparosc Endosc Percutan Tech. 2013;23:e209-e216. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 80. | Ebihara Y, Okushiba S, Kawarada Y, Kitashiro S, Katoh H. Outcome of functional end-to-end esophagojejunostomy in totally laparoscopic total gastrectomy. Langenbecks Arch Surg. 2013;398:475-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 81. | Tsunoda S, Okabe H, Obama K, Tanaka E, Hisamori S, Kinjo Y, Sakai Y. Short-term outcomes of totally laparoscopic total gastrectomy: experience with the first consecutive 112 cases. World J Surg. 2014;38:2662-2667. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |