Published online Sep 7, 2014. doi: 10.3748/wjg.v20.i33.11835
Revised: May 19, 2014
Accepted: June 13, 2014
Published online: September 7, 2014
AIM: To evaluate the feasibility of a second parallel transjugular intrahepatic portosystemic shunt (TIPS) to reduce portal venous pressure and control complications of portal hypertension.
METHODS: From January 2011 to December 2012, 10 cirrhotic patients were treated for complications of portal hypertension. The demographic data, operative data, postoperative recovery data, hemodynamic data, and complications were analyzed.
RESULTS: Ten patients underwent a primary and parallel TIPS. Technical success rate was 100% with no technical complications. The mean duration of the first operation was 89.20 ± 29.46 min and the second operation was 57.0 ± 12.99 min. The mean portal system pressure decreased from 54.80 ± 4.16 mmHg to 39.0 ± 3.20 mmHg after the primary TIPS and from 44.40 ± 3.95 mmHg to 26.10 ± 4.07 mmHg after the parallel TIPS creation. The mean portosystemic pressure gradient decreased from 43.80 ± 6.18 mmHg to 31.90 ± 2.85 mmHg after the primary TIPS and from 35.60 ± 2.72 mmHg to 15.30 ± 3.27 mmHg after the parallel TIPS creation. Clinical improvement was seen in all patients after the parallel TIPS creation. One patient suffered from transient grade I hepatic encephalopathy (HE) after the primary TIPS and four patients experienced transient grade I-II after the parallel TIPS procedure. Mean hospital stay after the first and second operations were 15.0 ± 3.71 d and 16.90 ± 5.11 d (P = 0.014), respectively. After a mean 14.0 ± 3.13 mo follow-up, ascites and bleeding were well controlled and no stenosis of the stents was found.
CONCLUSION: Parallel TIPS is an effective approach for controlling portal hypertension complications.
Core tip: We retrospectively reviewed 10 patients treated in our institution who underwent a second parallel transjugular intrahepatic portosystemic shunt (TIPS) to reduce portal venous pressure and portosystemic pressure gradient to an acceptable level and control the complications of portal hypertension. We also present our experience evaluating the feasibility and safety of this technique. Parallel TIPS is an effective approach for controlling portal hypertension complications.
- Citation: He FL, Wang L, Yue ZD, Zhao HW, Liu FQ. Parallel transjugular intrahepatic portosystemic shunt for controlling portal hypertension complications in cirrhotic patients. World J Gastroenterol 2014; 20(33): 11835-11839
- URL: https://www.wjgnet.com/1007-9327/full/v20/i33/11835.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i33.11835
The transjugular intrahepatic portosystemic shunt (TIPS) is an effective way for controlling complications of portal hypertension, including gastrointestinal bleeding and refractory ascites in patients with cirrhosis. TIPS was first described by Rösch et al[1] in 1969, and it is currently considered to be one of the most important improvements in interventional therapy and represents a major contribution to treatment of patients with cirrhosis and portal hypertension syndrome[2]. TIPS can reduce portal vein pressure and portosystemic pressure gradient (PSG; pressure difference between portal vein and the cava) in 90%-95% of cases, while a small number of patients do not benefit from TIPS and portal vein pressure remains high after one shunt due to insufficient PSG reduction[3]. Here, we retrospectively reviewed 10 cases out of 205 treated in our institution who underwent a second parallel TIPS to reduce portal venous pressure and PSG to an acceptable level and control the complications of portal hypertension. We also present our experience evaluating the feasibility and safety of this technique.
Between January 2011 and December 2012, 10 patients with cirrhosis (7 males) with a mean age of 52.30 ± 4.52 years underwent a parallel TIPS in our institution (Table 1). All the patients were infected with hepatitis B virus and had complications from cirrhosis and portal hypertension. The indications for TIPS were refractory ascites (n = 9) and gastrointestinal bleeding (n = 1). A second shunt tract was established due to insufficient relief of symptoms and unsuccessful reduction of portal vein pressure. The patients underwent portosystemic shunt twice within 3-6 mo. The hepatic function status evaluated by Child-Pugh classification was class B in eight cases and class C in two. The follow-up time was 9-18 mo and the mean time was 14.0 ± 3.13 mo.
| Characteristic | |
| Sex (M/F) | 7/3 |
| Age (yr, mean ± SD) | 52.30 ± 4.52 |
| Child-Pugh classification | |
| B | 8 |
| C | 2 |
| Indication for TIPS | |
| Refractory ascites | 9 |
| Gastrointestinal bleeding | 1 |
The first TIPS procedure was performed in the Interventional Radiology Suite under local anesthesia. The Rösch-Uchida Transjugular Liver Access Set (Cook, Bloomington, IN, United States) was used for every patient. Right jugular venous access was established with a 10-F sheath. A 5-F multipurpose catheter was used to engage the right hepatic vein and perform angiography, and a curved cannula was then advanced with the guidewire into the right hepatic vein. A sheathed needle was advanced into the portal vein through the liver parenchyma and the guide wire was placed into the portal vein through the sheath. Portal vein angiography was performed with a 5-F pigtail catheter and portal vein pressure and right atrium pressure were measured. Subsequently, the shunt tract was dilated with an angioplasty balloon ranging from 8 to 10 mm, and a covered stent with a diameter of 8 or 10 mm was utilized. If the distal shunt was not sufficient for the shunt tract, an additional stent was utilized to extend the length. The varicose coronary gastric vein was embolized to prevent future gastrointestinal bleeding and the portal vein angiography and pressure measurements were performed again. The PSG was measured before and after the shunt creation.
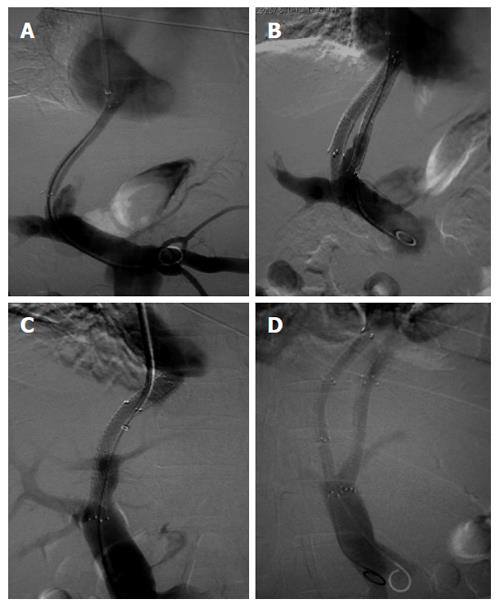
In nine patients, ascites was not relieved and recurrent gastrointestinal bleeding occurred in the other patient, even though ultrasound proved the patency of all the first shunt tracts. Therefore, a second TIPS was established 3 mo after the first procedure. The right jugular venous access was used for the second shunt tract. Through the first shunt tract, portal vein angiography was carried out (Figure 1A) and pressure was measured. The Rösch-Uchida Transjugular Liver Access Set was used and the systemic vein to portal vein parenchymal tract was attempted with the previous technique. With the stents of the first tract as the mark, puncture of the portal vein with the sheathed needle was more targeted and efficient. In four patients, the shunt tract was directly advanced from the vena cava to the portal vein because the right hepatic vein was not available for both tracts. The shunt tract was dilated, the stents were deployed and the varicose coronary gastric vein and other collaterals were embolized as described in this article. Portal vein angiography (Figure 1B) and pressure measurements were once again performed. The PSG was measured as described.
We compared perioperative and postoperative data in all the patients who underwent both TIPS procedures. This study was approved by ethics committee of Shijitan Hospital, Capital Medical University.
All the patients were under close monitoring during the perioperative period. Complications including abdominal cavity hemorrhage, hepatic failure and hepatic encephalopathy (HE) were observed. The patients remained in contact with the doctors who had performed the procedures. Clinical observations included reduction of ascites, gastrointestinal bleeding and HE. They were subjected to ultrasound imaging at 1, 3 and 6 mo after TIPS placement. Evaluations included stent patency, blood flow of the shunt tracts, and presence of ascites.
SPSS for Windows version 17.0 was utilized for data processing and statistical analysis, with paired-sample t test for data measurement. Data are summarized as frequencies and continuous variables as mean ± standard deviation (SD). P < 0.05 was considered statistically significant.
All the patients underwent a primary and parallel TIPS procedure, which were successful in all cases, with no technical complications. In six patients the second shunt tract was advanced from the hepatic vein to the portal vein and in the other four patients, the shunt tract was directly advanced from the vena cava to the portal vein (also named direct intrahepatic portacaval shunt; DIPS) (Figure 1C and D). The second tracts were created 3 mo after the first ones. In nine patients, the varicose coronary gastric vein was embolized. The mean duration of the first operation was 89.20 ± 29.46 min and the second operation was 57.0 ± 12.99 min, with a significant difference (P = 0.001).
TIPS altered the portal pressure in all patients after the second operation (Table 2). The mean portal system pressure prior to TIPS placement was 54.80 ± 4.16 mmHg, which decreased to 39.0 ± 3.20 mmHg after the first shunt tract was established (P < 0.001). The mean portal system pressure prior to the second TIPS was 44.40 ± 3.95 mmHg and decreased to 26.10 ± 4.07 mmHg after the procedures (P < 0.001). The mean PSG prior to the TIPS placement was 43.80 ± 6.18 mmHg, which decreased to 31.90 ± 2.85 mmHg after the first shunt tract was established (P < 0.001). The mean PSG prior to the second TIPS was 35.60 ± 2.72 mmHg and decreased to 15.30 ± 3.27 mmHg after the procedures (P < 0.001).
| Primary TIPS | Parallel TIPS | |||||||||
| Before (mmHg, mean ± SD) | After (mmHg, mean ± SD) | t value | P value | Before (mmHg, mean ± SD) | After (mmHg, mean ± SD) | t value | P value | t value1 | P value1 | |
| Portal venous pressure | 54.80 ± 5.16 | 39.00 ± 3.20 | 21.73 | < 0.001 | 44.40 ± 3.95 | 26.10 ± 4.07 | 11.70 | < 0.001 | 18.35 | < 0.001 |
| PSG | 43.80 ± 6.18 | 31.90 ± 2.85 | 9.38 | < 0.001 | 35.60 ± 2.72 | 15.30 ± 3.27 | 67.67 | < 0.001 | 20.01 | < 0.001 |
Clinical improvement was seen in all patients after the parallel TIPS procedure. Ascites was not relieved sufficiently after the first procedure, but it disappeared completely in seven patients and decreased obviously in two patients within 7-14 d after the second procedure. Recurrent hemorrhage was not seen in the patient with gastrointestinal bleeding.
Complications occurred during the procedures and postoperative complications including hepatic failure and HE were observed after the first and second operations. No surgery-related complications such as abdominal cavity hemorrhage or subcutaneous hematoma were found. One patient suffered from transient grade I encephalopathy after the first operation and four patients experienced transient grade I-II HE after the second procedure, which were relieved after medical treatment. One patient with Child-Pugh class C suffered from hepatic failure after the first operation. He and the other Class C patient and one with Child-Pugh class B had hepatic failure after the second operation, which was cured within 1 wk. Two patients suffered from both HE and hepatic failure. The duration of hospital stay for the parallel TIPS procedure was longer than for the primary TIPS procedure: mean hospital stay after the first and second operations was 15.0 ± 3.71 d and 16.90 ± 5.11 d, respectively (P = 0.014).
The patients were followed for a mean of 14.0 ± 3.13 mo without loss to follow-up. Two patients with Child-Pugh class C were hospitalized several times due to poor liver function and the other eight patients were followed in the outpatient department. Ascites and bleeding were well controlled during follow-up and no stent stenosis was found by ultrasonic examination. The incidence of transient HE was 30% at 3 mo, 40% at 6 mo and 50% at 12 mo. All patients survived during follow-up. No patient underwent liver transplantation.
TIPS is an effective method of treating complications of portal hypertension due to cirrhosis, and has been utilized widely in clinical practice as a safe and minimally invasive procedure[4]. Liver transplantation has not yet been popularized, therefore, TIPS is of major importance worldwide[5]. TIPS has been proven to be effective in 59.4%-91% of cases for secondary prevention of variceal bleeding and in 38%-84% of cases in controlling ascites[6]. The symptoms improved after the parallel TIPS procedure in our study. We believe that uncontrolled ascites and gastrointestinal bleeding after the first TIPS procedure were due to high portal vein pressure and insufficient PSG reduction. In our study, the mean portal vein pressure prior to TIPS was 54.80 ± 4.16 mmHg, which was 10-15 mmHg higher than that in patients who underwent TIPS reported before[6]. The symptoms were controlled after the second procedure when the mean portal vein pressure decreased to 26.10 ± 4.07 mmHg and the mean PSG decreased to 15.30 ± 3.27 mmHg. In 2006, a Brazilian doctor, Néstor[7] reported one case with a second parallel TIPS tract when the first shunt was patent, which reduced the PSG to 9 mmHg and relieved clinical symptoms. Parvinian reported two cases of parallel TIPS for treatment of complications of cirrhotic portal hypertension, with reduction of PSG to 12 and 10 mmHg[8]. The American Association for the Study of Liver Diseases (AASLD) recommends reducing PSG to < 8 mmHg to improve quality of life[9]. Reducing the portal vein pressure and PSG to an acceptable level is the key point of TIPS procedures.
In our study of 10 cases, the technical success rate of a second parallel TIPS tract was 100%. The mean duration of the first procedure was 89.20 ± 29.46 min and the second operation was 57.0 ± 12.99 min, which showed a statistically significant difference. The procedures were all carried out by the same group of doctors, therefore, the reduction in procedure time resulted in more targeted puncture of the portal vein from the vena cava. In TIPS operations, the most critical and time-consuming feature is puncture of the portal vein. In 10%-30% of cases, percutaneous transhepatic portal vein angiography is performed to guide the procedure, and consequently increases the risk of injury to the biliary tract and hepatic vein, and abdominal cavity hemorrhage[10]. In building the parallel tract in this study, with the first tract as the mark, no percutaneous transhepatic portal vein angiography was performed. In four patients, the shunt tract was directly advanced from the vena cava to the portal vein, and the procedures is also named DIPS, due to the absence of the hepatic vein as a shunt outflow. DIPS was first described in 2001 by Petersen et al[11]. The hallmark of the DIPS procedure is the use of the caudate lobe as the parenchymal tract to create a side-to-side portocaval shunt. The advantage of the DIPS procedure is not using the hepatic vein as a shunt outflow[12,13]. In a previous study, DIPS was performed by an intravascular ultrasound probe introduced via a femoral vein approach[14]. However, no intravascular ultrasound was utilized in our study because the stents of the first tract were a marker for the portal vein. DIPS was the first choice for creating a parallel TIPS tract in cases with an insufficient hepatic vein. In 9 patients the varicose coronary gastric veins were embolized because gastrointestinal bleeding was mainly caused directly by rupture of these vessels in patients with portal hypertension.
Covered stent grafts have been routinely applied in TIPS procedures and have increased the patency rates. Yet, utilization of covered stent grafts in TIPS procedures also increases the risk of HE[15,16]. In our study, 4 of 10 patients experienced transient grade HE, which may have resulted in a significant increase in outflow or large PSG reduction. In cases with a parallel TIPS, close attention should be paid to HE, and treatment against encephalopathy should be given before and after the procedure.
In conclusion, the parallel TIPS procedure is an effective approach for controlling complications of portal hypertension in patients with cirrhosis in whom primary TIPS does not reduce portal vein pressure or PSG to an acceptable level. The parallel TIPS procedure takes less time by using the stents of the first tract as a marker for the portal vein. DIPS is an option for avoiding using the hepatic vein as a shunt outflow. HE is the main complication of the procedure and treatment against encephalopathy should be given before and after the parallel TIPS creation.
The transjugular intrahepatic portosystemic shunt (TIPS) has been proven to be an effective way for controlling complications of portal hypertension. TIPS can reduce portal vein pressure in 90%-95% of cases, while a small number of patients can benefit from TIPS, and the portal vein pressure remains high after one shunt procedure.
In 2006, a Brazil doctor, Néstor Hugo Kisilevzky, reported one case with a second parallel TIPS tract when the first shunt was patent, which reduced the portosystemic pressure gradient (PSG) to 9 mmHg and relieved clinical symptoms. Parvinian reported two cases of parallel TIPS for treatment of complications of cirrhotic portal hypertension, reducing the PSG to 12 and 10 mmHg.
This study investigated the demographic data, operative data, postoperative recovery data, hemodynamic data and complications of this new technique in 10 patients.
The authors presented their experience evaluating the feasibility and safety of this technique. However, randomized controlled trials with more patients should be considered.
TIPS is a procedure performed in which a shunt is placed between the portal and hepatic veins.
In this manuscript, the authors retrospectively analyzed 10 patients who underwent a parallel TIPS in order to reduce the portal venous pressure and PSG to an acceptable level and control complications of portal hypertension between January 2011 and December 2012 at their hospital. Although the results of the manuscript can assist in present their experience evaluating the feasibility and safety of parallel TIPS to reduce the portal venous pressure and PSG to an acceptable level, there remain major concerns.
P- Reviewer: Genesca J, Murata S, Sharma V, Shen SQ S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Rösch J, Hanafee WN, Snow H. Transjugular portal venography and radiologic portacaval shunt: an experimental study. Radiology. 1969;92:1112-1114. [PubMed] [Cited in This Article: ] |
| 2. | Wang J. Clinical utility of entecavir for chronic hepatitis B in Chinese patients. Drug Des Devel Ther. 2014;8:13-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Parvinian A, Omene BO, Bui JT, Knuttinen MG, Minocha J, Gaba RC. Angiographic patterns of transjugular intrahepatic portosystemic shunt dysfunction and interventional approaches to shunt revision. J Clin Imaging Sci. 2013;3:19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Parvinian A, Bui JT, Knuttinen MG, Minocha J, Gaba RC. Transjugular intrahepatic portosystemic shunt for the treatment of medically refractory ascites. Diagn Interv Radiol. 2012;20:58-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Li SW, Wang K, Yu YQ, Wang HB, Li YH, Xu JM. Psychometric hepatic encephalopathy score for diagnosis of minimal hepatic encephalopathy in China. World J Gastroenterol. 2013;19:8745-8751. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 52] [Cited by in F6Publishing: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Darcy M. Evaluation and management of transjugular intrahepatic portosystemic shunts. AJR Am J Roentgenol. 2012;199:730-736. [PubMed] [Cited in This Article: ] |
| 7. | Néstor HK. Tips for controlling portal hypertension complications: efficacy, predictors of outcome and technical variations. Radiol Bras. 2006;39:385-395. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Parvinian A, Gaba RC. Parallel TIPS for treatment of refractory ascites and hepatic hydrothorax. Dig Dis Sci. 2013;58:3052-3056. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Harrod-Kim P, Saad WE, Waldman D. Predictors of early mortality after transjugular intrahepatic portosystemic shunt creation for the treatment of refractory ascites. J Vasc Interv Radiol. 2006;17:1605-1610. [PubMed] [Cited in This Article: ] |
| 10. | Eesa M, Clark T. Transjugular intrahepatic portosystemic shunt: state of the art. Semin Roentgenol. 2011;46:125-132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Petersen BD, Clark TW. Direct intrahepatic portocaval shunt. Tech Vasc Interv Radiol. 2008;11:230-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Hoppe H, Wang SL, Petersen BD. Intravascular US-guided direct intrahepatic portocaval shunt with an expanded polytetrafluoroethylene-covered stent-graft. Radiology. 2008;246:306-314. [PubMed] [Cited in This Article: ] |
| 13. | Petersen B, Binkert C. Intravascular ultrasound-guided direct intrahepatic portacaval shunt: midterm follow-up. J Vasc Interv Radiol. 2004;15:927-938. [PubMed] [Cited in This Article: ] |
| 14. | Peynircioglu B, Shorbagi AI, Balli O, Cil B, Balkanci F, Bayraktar Y. Is there an alternative to TIPS? Ultrasound-guided direct intrahepatic portosystemic shunt placement in Budd-Chiari syndrome. Saudi J Gastroenterol. 2010;16:315-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Sajja KC, Dolmatch BL, Rockey DC. Long-term follow-up of TIPS created with expanded poly-tetrafluoroethylene covered stents. Dig Dis Sci. 2013;58:2100-2106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Maleux G, Perez-Gutierrez NA, Evrard S, Mroue A, Le Moine O, Laleman W, Nevens F. Covered stents are better than uncovered stents for transjugular intrahepatic portosystemic shunts in cirrhotic patients with refractory ascites: a retrospective cohort study. Acta Gastroenterol Belg. 2010;73:336-341. [PubMed] [Cited in This Article: ] |