Published online Aug 7, 2013. doi: 10.3748/wjg.v19.i29.4832
Revised: June 13, 2013
Accepted: June 19, 2013
Published online: August 7, 2013
Laparoscopic cholecystectomy is a standard operation for benign gallbladder disease. As experience with laparoscopic cholecystectomy has increased, the procedure has become possible in patients with anesthetic problems. Patients with ankylosing spondylitis or severe kyphosis represent a challenging group to anesthesiologists and laparoscopic surgeons since these diseases are associated with difficult intubation, restrictive ventilatory defects, and cardiac problems. The relatively new approach of awake fiberoptic intubation is considered to be the safest option for patients with anticipated airway difficulties. Laparoscopic cholecystectomy is usually performed under general anesthesia but considerable difficulties in anesthetic management are encountered during laparoscopic surgery; for example, hemodynamic instability may develop in patients with cardiopulmonary dysfunction due to pneumoperitoneum and position changes during the operation. Nonetheless, regional anesthesia can be considered as a valid option for patients with gallbladder disease who are poor candidates for general anesthesia due to cardiopulmonary problems. We report three cases of laparoscopic cholecystectomy successfully performed in patients with anesthetic problems that included cardiopulmonary disease, severe kyphosis, and ankylosing spondylitis.
Core tip: This paper reported three cases of laparoscopic cholecystectomy successfully performed in patients with anesthetic problems that included cardiopulmonary disease, severe kyphosis, and ankylosing spondylitis. This study demonstrates that regional anesthesia can be considered as a valid option for patients with gallbladder disease who are poor candidates for general anesthesia due to cardiopulmonary problems.
- Citation: Kim BS, Joo SH, Joh JH, Yi JW. Laparoscopic cholecystectomy in patients with anesthetic problems. World J Gastroenterol 2013; 19(29): 4832-4835
- URL: https://www.wjgnet.com/1007-9327/full/v19/i29/4832.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i29.4832
Laparoscopic cholecystectomy is a standard procedure for the management of gallbladder disease. As experience with laparoscopic cholecystectomy has increased, laparoscopic cholecystectomy in patients with anesthetic problems has become possible. Ankylosing spondylitis is a challenge to the anesthesiologist and to the laparoscopic surgeon because it is associated with difficult intubation, restrictive ventilatory defects, and cardiac problems. Kyphotic patients may also suffer considerable perioperative morbidity such as cardiac problems and respiratory insufficiency. While laparoscopic cholecystectomy is classically performed under general anesthesia, regional anesthesia must be considered as a valid option for patients with gallbladder disease who are poor candidates for general anesthesia. We report three cases of laparoscopic cholecystectomy successfully performed in patients with anesthetic problems that included cardiopulmonary disease, severe kyphosis, and ankylosing spondylitis. All patients were informed about the operative and anesthetic procedures and provided consent.
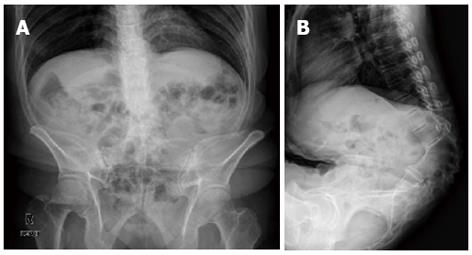
A 71-year-old, American Society of Anesthesiology (ASA) physical status III male patient (168 cm, 56 kg) underwent laparoscopic cholecystectomy due to acute cholecystitis with cholelithiasis. The patient had undergone a right pneumonectomy nine years previous to this procedure (Figure 1). A standard pulmonary function test revealed a moderate obstructive and restrictive pattern. Hypokinesia of the apical anterior and septum segments was observed on echocardiography. Pulmonology consultation reported a moderate postoperative risk that could be fatal if postoperative pneumonia developed. Cardiology consultation reported a postoperative risk of 1%-5% based on modified Goldman cardiac risk criteria[1]. Because severe postoperative complications were anticipated, segmental spinal anesthesia was performed and CO2 inflation to an intra-abdominal pressure of 8 mmHg. Laparoscopic cholecystectomy was performed; the procedure was smooth and uneventful. The patient was discharged 3 d after surgery.
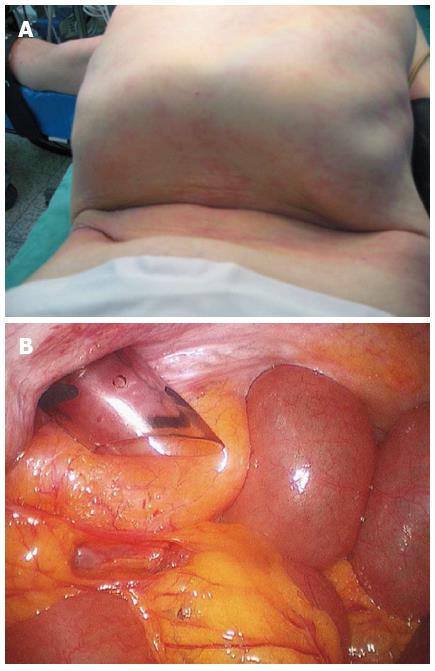
A 42-year-old male patient (173.6 cm, 68.9 kg) suffering from ankylosing spondylitis was admitted to our hospital presenting with right upper quadrant pain. Abdominal ultrasound revealed a 2 cm sized cholelithiasis for which he was scheduled to undergo laparoscopic cholecystectomy. The patient was ASA III and Mallampati grade IV on airway examination. The patient had fixed rigidity of the cervical spine and could not lie supine (Figure 2A) and his mouth opening was restricted. Accordingly, he was placed in a supine position with three pillows under his head. The anesthesiology team decided to perform fiberoptic intubation through the nasotracheal tree while the subject was conscious (Figure 2B). The patient was informed of an anticipated difficult orotracheal intubation. Laparoscopic cholecystectomy was performed without any complication. There were no perioperative complications related to airway management, and the patient was discharged 3 d after surgery.
A 54-year-old female patient (140 cm, 45.6 kg) with ASA physical status III suffering from severe thoracolumbar kyphosis (Figure 3) presented with right upper quadrant pain. The patient was diagnosed with acute cholecystitis on abdominal ultrasound and was scheduled to undergo laparoscopic cholecystectomy. Moderate restrictive pattern was found following a pulmonary function test. The patient could not lie supine and needed thick pillows beneath her head for support. Her thoracic cage was tilted anteriorly resulting in a low-lying costal margin and narrow abdomen. It was difficult to insert trocars because of narrow abdomen (Figure 4). CO2 was used to inflate her intra-abdominal pressure to 8 mmHg. The patient underwent laparoscopic cholecystectomy successfully and discharged from hospital at 5 d after surgery.
Considerable difficulties in anesthetic management are encountered during laparoscopic surgery. Hemodynamic instability in patients with cardiopulmonary dysfunction may develop due to pneumoperitoneum and position changes during the operation. While laparoscopic cholecystectomy is usually performed under general anesthesia, regional anesthesia has been used in special high-risk cases[2]. However, laparoscopic cholecystectomy under general anesthesia has been reported as safe and feasible even in high-risk patients[3]. Here, we show that carbon dioxide pneumoperitoneum with an intra-abdominal pressure of 8-12 mmHg for high-risk patients can be safe if the patients are well monitored and hemodynamic instability is actively treated. However, the patient in case 1 was at risk of post-operative death if pneumonia developed in the remnant lung, and was scheduled for the regional anesthesia. Due to the harmful effects of high intra-abdominal pressure, it is recommended that the lowest pressure possible that allows adequate exposure of the operative field be used[4]. A laparoscopic cholecystectomy was successfully carried out by maintaining CO2 pressure < 8 mmHg during the operation with the active participation of the attending anesthesiologists.
Ankylosing spondylitis is a chronic and progressive inflammatory disease involving articulations of the spine and adjacent tissue. Oral intubation is difficult in ankylosing spondylitis patients with cervical spine rigidity. Recently, awake fiberoptic intubation has been increasingly used, and considered to be the safest option for patients with anticipated airway difficulties[5,6]. To secure the airway, we used awake fiberoptic intubation in case 2 with written informed consent of the patient. In addition to airway management, anesthesiologists need to be concerned with restrictive ventilator defects and airway problems associated with ankylosing spondylitis. Therefore, preoperative examination for cardiovascular and pulmonary function is required[7].
Kyphosis is a deformity of the spine. Anesthesia for kyphosis in common with ankylosing spondylitis is often challenging. There is usually secondary involvement of the respiratory, cardiovascular, and neurologic systems. A detailed pre-anesthetic assessment and optimization of the respiratory and cardiovascular systems should be done[8]. It is desirable to maintain the lowest intra-abdominal pressure to prevent the adverse hemodynamic effect of pneumoperitoneum in restrictive lung disease. Another concern for the laparoscopic surgeon for a patient with kyphosis is positioning of the patient and surgical approach to the abdomen. Increasing numbers of older patients are presenting with benign gallbladder disease with senile kyphosis caused by aging or osteoporosis. Laparoscopic surgery is minimally invasive, and in severely kyphotic patients the procedure may prove difficult in approaching the narrow abdomen. In the third case, we performed this difficult surgery because the chest of the patient was tilted anteriorly and the abdominal cavity was narrowed by low-lying costal margin. Abnormalities of the spine can alter the contour of the pelvic vessels. Kyphosis, scoliosis, and the other skeletal abnormalities can affect vascular anatomy and must be considered during trocar insertion[9]. Severe senile kyphosis is not a contraindication for laparoscopic surgery[10].
Patients with spinal deformity such as ankylosing spondylitis and kyphosis form a challenging group to anesthesiologists and laparoscopic surgeons because of difficulties in intubation, positioning, and abdominal approaches. Careful preoperative anesthetic assessment for respiratory dysfunction, cardiac impairment, difficult airway, and associated specific problems in patients with ankylosing spondylitis or kyphosis is imperative. In patients with severely compromised respiratory function the final surgical plan should be a joint decision between surgeon and anesthesiologist. The patient and family should be warned about the possibility of postoperative ventilation and prolonged respiratory weaning and support.
As newer and more extensive laparoscopic procedures have been implemented, close cooperation between the laparoscopic surgeon and the anesthesiologist is required. We have performed laparoscopic cholecystectomy in seven patients with kyphosis. No perioperative complications occurred. While several studies[11] about obstetrics and gynecology and spine surgery in patients with ankylosing spondylitis and kyphosis have been reported, only one report has addressed laparoscopic cholecystectomy[12,13].
In conclusion, we successfully performed three cases of laparoscopic cholecystectomy in patients with anesthetic problems including cardiopulmonary disease, severe kyphosis, and ankylosing spondylitis.
P- Reviewer Shi HY S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, Burke DS, O’Malley TA, Goroll AH, Caplan CH. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845-850. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1895] [Cited by in F6Publishing: 1467] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 2. | Gramatica L, Brasesco OE, Mercado Luna A, Martinessi V, Panebianco G, Labaque F, Rosin D, Rosenthal RJ, Gramatica L. Laparoscopic cholecystectomy performed under regional anesthesia in patients with chronic obstructive pulmonary disease. Surg Endosc. 2002;16:472-475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Koivusalo AM, Pere P, Valjus M, Scheinin T. Laparoscopic cholecystectomy with carbon dioxide pneumoperitoneum is safe even for high-risk patients. Surg Endosc. 2008;22:61-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, Fuchs KH, Jacobi Ch, Jansen FW, Koivusalo AM. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16:1121-1143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 423] [Cited by in F6Publishing: 360] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 5. | Machata AM, Gonano C, Holzer A, Andel D, Spiss CK, Zimpfer M, Illievich UM. Awake nasotracheal fiberoptic intubation: patient comfort, intubating conditions, and hemodynamic stability during conscious sedation with remifentanil. Anesth Analg. 2003;97:904-908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (1)] |
| 6. | Ahmad N, Channa AB, Mansoor A, Hussain A. Management of difficult intubation in a patient with ankylosing spondylitis--a case report. Middle East J Anesthesiol. 2005;18:379-384. [PubMed] [Cited in This Article: ] |
| 7. | Steib A, Beller JP, Lleu JC, Otteni JC. [Difficult intubation managed by laryngeal mask and fibroscopy]. Ann Fr Anesth Reanim. 1992;11:601-603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Raw DA, Beattie JK, Hunter JM. Anaesthesia for spinal surgery in adults. Br J Anaesth. 2003;91:886-904. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 96] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Gordon LA, Shapiro SJ, Daykhovsky L. Problem-solving in laparoscopic surgery. Surg Endosc. 1993;7:348-355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Sato T, Yamaguchi S, Ozawa S, Ishii T, Tashiro J, Hosonuma T, Koyama I, Gagner M. Is laparoscopic surgery a contraindication in patients with severe senile kyphosis? Hepatogastroenterology. 2010;57:1095-1098. [PubMed] [Cited in This Article: ] |
| 11. | Bansal N, Gupta S. Anaesthetic management of a parturient with severe kyphoscoliosis. Kathmandu Univ Med J (KUMJ). 2008;6:379-382. [PubMed] [Cited in This Article: ] |
| 12. | Pan PH, Moore CH. Doxorubicin-induced cardiomyopathy during pregnancy: three case reports of anesthetic management for cesarean and vaginal delivery in two kyphoscoliotic patients. Anesthesiology. 2002;97:513-515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Chowbey PK, Panse R, Khullar R, Sharma A, Soni V, Baijal M. Laparoscopic cholecystectomy in a patient with ankylosing spondylitis with severe spinal deformity. Surg Laparosc Endosc Percutan Tech. 2005;15:234-237. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |