Published online Nov 28, 2012. doi: 10.3748/wjg.v18.i44.6501
Revised: September 3, 2012
Accepted: September 12, 2012
Published online: November 28, 2012
An extrahepatic arterioportal fistula (APF) involving the gastroduodenal artery and superior mesenteric vein is rare and mostly results from iatrogenic injuries. The clinical symptoms associated with APFs may include abdominal pain, gastrointestinal bleeding, ascites, nausea, vomiting, diarrhea, or even congestive heart failure. We present the case of a 70-year-old man who presented with chronic abdominal pain and gastrointestinal bleeding secondary to APF and portal vein thrombosis. The endovascular embolization of APF was accomplished successfully, and symptoms of portal hypertension resolved immediately after intervention. Unfortunately, the patient did not respond well to anticoagulation therapy with warfarin. Therefore, the patient underwent implantation of a transjugular intrahepatic portosystemic shunt, and the complications of portal hypertension resolved. In conclusion, the embolization of APF is technically feasible and effective and can be considered the first-choice therapy in selected patients.
- Citation: Nie L, Luo XF, Li X. Gastrointestinal bleeding caused by extrahepatic arterioportal fistula associated with portal vein thrombosis. World J Gastroenterol 2012; 18(44): 6501-6503
- URL: https://www.wjgnet.com/1007-9327/full/v18/i44/6501.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i44.6501
Upper gastrointestinal bleeding in patients with cirrhosis is usually due to portal hypertension, which is common in this population. Nevertheless, bleeding resulting from extrahepatic arterioportal fistulas (APFs) is extremely rare[1-3]. Extrahepatic APF may cause severe portal hypertension, which leads to upper and lower gastrointestinal bleeding, refractory ascites, diarrhea, and hepatic encephalopathy. We present an unusual case of a 70-year-old man who presented with chronic abdominal pain and gastrointestinal bleeding secondary to APF and portal vein thrombosis.
A 70-year-old man with a history of cirrhosis resulting from hepatitis B virus infection was admitted to our hospital with complaints of chronic abdominal pain and melena. At the time of admission, his pulse rate was 63 beats/min, and his arterial blood pressure was 117/61 mmHg. Laboratory tests disclosed the following values: red blood cells, 2.65 × 1012/L; white blood cells, 5.65 × 109/L; PC, 207 × 109/L; prothrombin time, 15.9 s; total bilirubin, 1.1 mg/dL; albumin, 3.2 g/dL; aspartate aminotransferase, 47 IU/L; alanine aminotransferase, 43 IU/L; and alkaline phosphatase, 450 IU/L. The patient underwent cholecystectomy at the age of 67 because of acute cholecystitis.
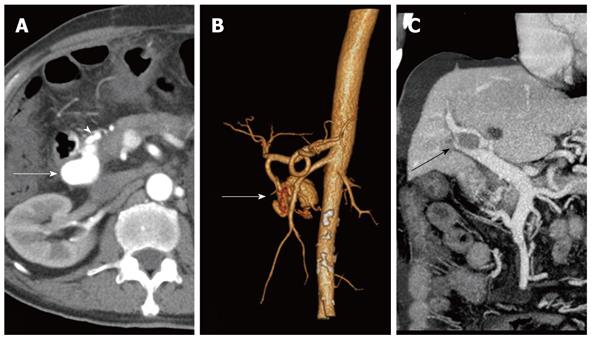
Upper gastrointestinal endoscopy showed multiple severe esophageal and duodenal descendent varices and portal hypertensive gastropathy. Computerized tomography (CT) of the abdomen demonstrated the presence of a large aneurysm next to the head of the pancreas filled by the dilated gastroduodenal artery (GDA), draining into the superior mesenteric vein (SMV) (Figure 1). Other CT findings were cirrhotic liver, the presence of esophageal varices, portal thrombosis, moderate ascites and splenomegaly (Figure 1).
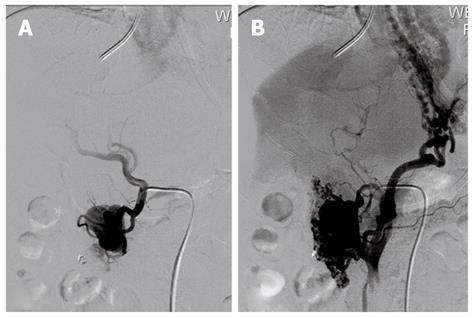
Under local anesthesia, a 5-F Cobra catheter (Teramo Co., Fijinomiya, Japan) was advanced into the GDA via the common femoral artery. Selective digital subtraction angiography showed an APF between the GDA and SMV, and the blood flow from the SMV did not go into the portal vein but into the collateral veins (Figure 2). Embolization of the extrahepatic APF was performed to occlude the fistula and reduce portal pressure using stainless metal coils (Cook Incorporated, Bloomington, United States). A further angiography of the GDA confirmed immediate cessation of the fistula and the abrogation of the hyperkinetic portal flow (Figure 3). After the procedure, the gastrointestinal bleeding stopped, and the patient reported symptomatic improvement, with resolution of the chronic abdominal pain. Four days later, the patient was discharged in good condition. He was also started on anticoagulation therapy with warfarin, and the dose was adjusted to achieve an International Normalized Ratio of 2 to 3.
Three years after intervention, the patient presented to the emergency room with acute upper gastrointestinal bleeding. CT scan demonstrated multiple thromboses in the right and main portal vein and massive ascites, without any sign of APF (Figure 4). Because anticoagulation therapy was not successful, the patient underwent implantation of a transjugular intrahepatic portosystemic shunt (TIPS). Currently, two years after TIPS, despite several episodes of mild hepatic encephalopathy requiring conventional medical treatment, the patient remains clinically well.
Extrahepatic APF involving the GDA and SMV is an uncommon disorder of the mesenteric vasculature characterized by abnormal communication between the arterial and portal circulation. The most common causes of APFs are reported to be congenital vascular malformations, blunt or penetrating traumas and iatrogenic injuries[1,4-6]. Our patient had no history of abdominal traumas or other vascular malformations, suggesting that the APF most likely arose as a result of iatrogenic vascular injury during the previous biliary surgery.
Both CT and magnetic resonance imaging with intravenous contrast material can provide useful information for the diagnosis of APFs, specifically, the exact anatomic location and extent of mesenteric vessel involvement. Doppler ultrasonography is another useful imaging modality for diagnosis, which can not only detect the position of an APF but also evaluate the flow direction. Arteriography should be performed as soon as possible for diagnostic purposes and evaluating APF hemodynamics, delineating the fistula site, and determining the size of the feeding artery. In the present case, CT of the abdomen clearly revealed a large aneurysm, which was supplied by the GDA and had fistulated into the SMV, with radiological evidence of portal hypertension.
APF is an uncommon but treatable cause of portal hypertension. The clinical symptoms associated with APFs may include abdominal pain, gastrointestinal bleeding, ascites, nausea, vomiting, diarrhea, or even congestive heart failure[4,7]. In this case, extrahepatic APF led to secondary portal hypertension, resulting in upper gastrointestinal bleeding and moderate ascites. Portal hypertension disappeared immediately after cessation of the APF.
Generally, the early treatment of APF is mandated, even in asymptomatic patients with a high-flow fistula, to prevent complications. Both open and endovascular management of APFs has been well described[5,8,9]. However, there is an increased use of endovascular techniques as first-choice therapy, including embolization or stent insertion[8,10]. Endovascular techniques provide a less invasive alternative to surgical procedures, can be performed under local anesthesia, and do not impede planned surgery. In our case, a 5-F Cobra catheter was used to extend the peripheral fistula position, and it allowed for the exact placement of the coils in the feeding GDA.
The endovascular embolization of APF was accomplished successfully, and symptoms of portal hypertension resolved immediately after intervention. Unfortunately, the patient did not respond well to anticoagulation therapy with warfarin. We elected to treat the patient with TIPS rather than endoscopic treatment for two reasons. The first reason is that because the patient did not respond well to warfarin, endoscopic therapy plus anticoagulation therapy seemed impossible to recanalize the portal vein. The second reason was that TIPS could not only reduce the portal pressure but also recanalize the portal vein and avoid rethrombosis by restoring portal flow through a low-resistance shunt.
In conclusion, extrahepatic APF is a rare cause of portal hypertension and may cause gastrointestinal bleeding and ascites. The embolization of APF is technically feasible and effective and can be considered the first-choice therapy in selected patients. Moreover, by embolizing the APF, chronic abdominal pain was also controlled.
Peer reviewers: Hyo-Cheol Kim, MD, Clinical Assistant Professor in Vascular Intervention Section, Department of Radiology, Seoul National University Hospital, No. 28 Yongon-dong, Chongno-gu, Seoul 110-744, South Korea; Yu-Yuan Li, Professor, Department of Gastroenterology, First Municipal People’s Hospital of Guangzhou, No. 1 Panfu Road, Guangzhou 510180, Guangdong Province, China
S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Krishan S, McPherson S, Pine J, Hayden J. Current management of mesenteric extrahepatic arterioportal fistulas: report of a case treated with a gastroduodenal artery stent graft and literature review. Vasc Endovascular Surg. 2010;44:139-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Pietri J, Remond A, Reix T, Abet D, Sevestre H, Sevestre MA. Arterioportal fistulas: twelve cases. Ann Vasc Surg. 1990;4:533-539. [PubMed] [Cited in This Article: ] |
| 3. | Denys A, Hammel P, de Baere T, Vilgrain V, Bernades P, Roche A, Menu Y. Arterioportal fistula due to a ruptured pancreatic pseudocyst: diagnosis and endovascular treatment. AJR Am J Roentgenol. 1998;170:1205-1206. [PubMed] [Cited in This Article: ] |
| 4. | Sonnenschein MJ, Anderson SE, Lourens S, Triller J. A rare case of jejunal arterio-venous fistula: treatment with superselective catheter embolization with a tracker-18 catheter and microcoils. Cardiovasc Intervent Radiol. 2004;27:671-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Vauthey JN, Tomczak RJ, Helmberger T, Gertsch P, Forsmark C, Caridi J, Reed A, Langham MR, Lauwers GY, Goffette P. The arterioportal fistula syndrome: clinicopathologic features, diagnosis, and therapy. Gastroenterology. 1997;113:1390-1401. [PubMed] [Cited in This Article: ] |
| 6. | Lu ZY, Ao JY, Jiang TA, Peng ZY, Wang ZK. A large congenital and solitary intrahepatic arterioportal fistula in an old woman. World J Gastroenterol. 2009;15:1656-1659. [PubMed] [Cited in This Article: ] |
| 7. | Wang BW, Wu DH, Lin CK, Huang JS, Mok KT. Superior mesenteric arteriovenous fistula associated with portal obstruction. Zhonghua Yi Xue Zazhi (. Taipei). 2001;64:586-591. [PubMed] [Cited in This Article: ] |
| 8. | Yeo KK, Dawson DL, Brooks JL, Laird JR. Percutaneous treatment of a large superior mesenteric artery pseudoaneurysm and arteriovenous fistula: a case report. J Vasc Surg. 2008;48:730-734. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Marrone G, Caruso S, Miraglia R, Tarantino I, Volpes R, Luca A. Percutaneous transarterial embolization of extrahepatic arteroportal fistula. World J Gastroenterol. 2006;12:5562-5564. [PubMed] [Cited in This Article: ] |
| 10. | Bouziane Z, Ghissassi B, Bouayad M, Sefiani Y, Lekehal B, El Mesnaoui A, Bensaid Y. Successful endovascular management of postoperative arterio portal fistula. Ann Vasc Surg. 2011;25:385.e1-385.e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |