Published online Aug 14, 2012. doi: 10.3748/wjg.v18.i30.3992
Revised: October 24, 2011
Accepted: June 8, 2012
Published online: August 14, 2012
AIM: To report our experience using a recently introduced anchoring balloon for diagnostic and therapeutic direct peroral cholangioscopy (DPOC).
METHODS: Consecutive patients referred for diagnostic or therapeutic peroral cholangioscopy were evaluated in a prospective cohort study. The patients underwent DPOC using an intraductal anchoring balloon, which was recently introduced to allow consistent access to the biliary tree with an ultraslim upper endoscope. The device was later voluntarily withdrawn from the market by the manufacturer.
RESULTS: Fourteen patients underwent DPOC using the anchoring balloon. Biliary access with an ultraslim upper endoscope was accomplished in all 14 patients. In 12 (86%) patients, ductal access required sphincteroplasty with a 10-mm dilating balloon. Intraductal placement of the ultraslim upper endoscope allowed satisfactory visualization of the biliary mucosa to the level of the confluence of the right and left hepatic ducts in 13 of 14 patients (93%). Therapeutic interventions by DPOC were successfully completed in all five attempted cases (intraductal biopsy in one and DPOC guided laser lithotripsy in four). Adverse events occurred in a patient on immunosuppressive therapy who developed an intrahepatic biloma at the site of the anchoring balloon. This required hospitalization and antibiotics. Repeat endoscopic retrograde cholangiopancreatography 8 wk after the index procedure showed resolution of the biloma.
CONCLUSION: Use of this anchoring balloon allowed consistent access to the biliary tree for performance of diagnostic and therapeutic DPOC distal to the biliary bifurcation.
- Citation: Parsi MA, Stevens T, Vargo JJ. Diagnostic and therapeutic direct peroral cholangioscopy using an intraductal anchoring balloon. World J Gastroenterol 2012; 18(30): 3992-3996
- URL: https://www.wjgnet.com/1007-9327/full/v18/i30/3992.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i30.3992
The value of cholangioscopy for diagnosis and treatment of biliary disorders has been well established[1]. Diagnostic and therapeutic direct peroral cholangioscopy (DPOC) using an ultraslim upper endoscope offers significant advantages over ductoscopy using dedicated cholangioscopes[2]. The ultraslim endoscope uses a single-operator platform, provides high-definition digital image quality, allows simultaneous irrigation and therapy, is not fragile, and has a larger working channel enabling enhanced diagnostic sampling and therapeutic interventions. However, DPOC in its current state has significant limitations. Initial free biliary cannulation is cumbersome, time consuming, and associated with a significant failure rate. Even when access is obtained, intraductal maneuverability and stability may be compromised by looping of the endoscope in the stomach or duodenum. To address these technical challenges, a prototype biliary anchoring balloon has been designed. Feasibility of this system in an animal model has been assessed but human reports are lacking[2].
We performed a study in 14 patients to assess utility of this device for diagnosis and treatment of various biliary disorders prior to voluntary device withdrawal by the manufacturer. We report our experience using this device for ductal access in all 14 patients.
This was a prospective cohort study of consecutive patients referred to our tertiary care center for endoscopic retrograde cholangiopancreatography (ERCP) and peroral cholangioscopy. The primary aim of the study was to assess the ability to gain access to the bile duct with an ultraslim upper endoscope and visualize the extrahepatic biliary mucosa to the level of the confluence of the left and right hepatic ducts. The secondary aim was to examine the feasibility of performing therapeutic procedures through the endoscope while maintaining intraductal access. This study was approved by The Cleveland Clinic Institutional Review Board. The inclusion criteria were presence of biliary pathology and ability of the patients to give informed consent. The exclusion criteria were coagulopathy, suspicion for acute ascending cholangitis, latex allergy, and biliary ductal diameter < 6 mm.
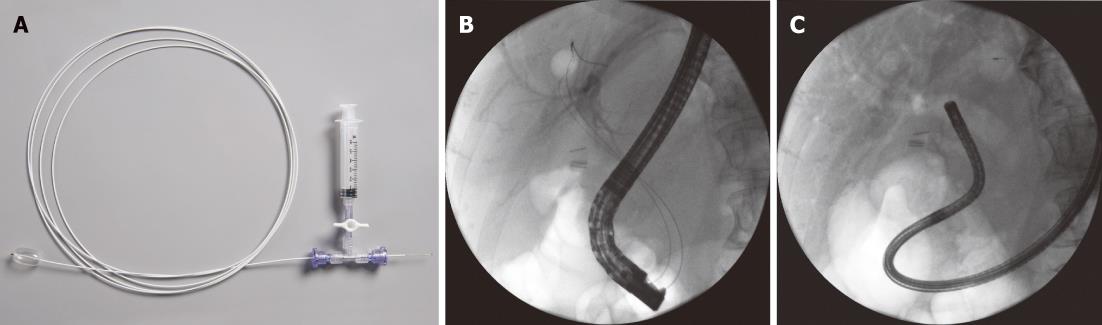
The anchoring balloon used in this study (Cook Medical, Winston-Salem, NC, United States) had five components. A short stylet located at the most proximal end of the device was used to occlude the air channel after the balloon was inflated. This prevented deflation of the balloon after removal of the handle. Immediately distal to the stylet, there was a handle, which could be detached and removed to allow backloading of the device into an ultraslim upper endoscope while maintaining balloon inflation. The device had a 300-cm long, 4-French catheter with a nitinol stiffening core. At the distal end of the catheter, there was a latex balloon that could be inflated to 15 mm and used as an intraductal anchoring point. A radiopaque loop tip was located at the most distal end of the device and allowed positioning of the balloon in the desired duct under fluoroscopic guidance over a guidewire (Figure 1A).
All procedures were performed by an experienced endoscopist, under monitored anesthesia care sedation with the patients in the prone position. Endoscopic sphincterotomy was or had been performed previously prior to direct peroral cholangioscopy in all patients. Balloon sphincteroplasty to 10 mm was performed as needed. After completion of ERCP, a 0.889-mm guidewire was placed in one of the intrahepatic ducts. The anchoring balloon was then directed into that intrahepatic duct by placing the loop end of the device over the guidewire. Location of the guidewire and the anchoring balloon was verified by fluoroscopy (Figure 1B). The balloon was then inflated with air to anchor it within the duct. A gentle pull on the balloon catheter confirmed ductal anchoring. If the pull on the catheter led to dislodgment of the balloon, it was deflated and the procedure was repeated to reposition the balloon in another intrahepatic duct followed by inflation of the balloon and pulling to confirm anchoring. Once anchoring of the balloon was confirmed, the air channel of the device was covered with the stylet to keep the balloon inflated. The proximal handle was then detached from the catheter and removed. This was followed by removal of the duodenoscope and the guidewire, leaving the inflated balloon and its catheter behind. An ultraslim upper endoscope was backloaded over the catheter and advanced into the bile duct to the level of the confluence of the right and left hepatic ducts (Figure 1C). The anchoring balloon was then removed in most cases. The bile duct was irrigated through the accessory channel of the ultraslim endoscope with sterile saline solution, followed by slow withdrawal of the endoscope, allowing systematic inspection of the biliary tree. Air insufflation was not used, to avoid potential complications. Routine antibiotic prophylaxis was not administered. The ultraslim endoscopes used in this study included GIF-XP160 (outer diameter 5.9 mm), GIF-XP180 (outer diameter 5.5 mm), and GIF-N180 (outer diameter 4.9 mm) (Olympus Corporation, Center Valley, PA United States). All endoscopes had an instrument channel with an inner diameter of 2 mm.
Values are presented as mean (range) or frequency (percentage). R version 2.4.1 software (The R Foundation for Statistical Computing, Vienna, Austria) was used to perform all the analyses.
Fourteen consecutive patients underwent DPOC using the new anchoring balloon. The mean age of the patients was 65 years (range: 30-92 years). Nine (64%) patients were female. The indications for the procedure, DPOC findings and final diagnosis are presented in Table 1.
| Indication | DPOC diagnosis | Final diagnosis | Performance of sphincteroplasty | Largest bile duct diameter (mm) |
| Obstructive jaundice | Extrinsic stricture | Pancreatic cancer | Yes | 18 |
| Obstructive jaundice | Extrinsic stricture | Chronic pancreatitis | No | 12 |
| Suspicion for missed stones by ERCP | Stone in the main bile duct | Missed stone by ERCP | Yes | 17 |
| Difficult-to-remove bile duct stone | Large CBD stone | DPOC-guided laser lithotripsy followed by stone removal | Yes | 11 |
| Biliary stricture in a patient with PSC | Benign stricture | Benign PSC stricture | Yes | 10 |
| Biliary filling defect on MRI | Intraductal tumor | Intrahepatic cholangiocarcinoma with intraductal extension | Yes | 10 |
| Suspicion for missed stone(s) by ERCP | No stones found | Yes | 8 | |
| Abnormal LFTs in a post liver transplantation patient | Missed stones during ERCP | Missed stones during ERCP | No | 11 |
| Surveillance after biliary polypectomy | Complete removal of the polyp | Yes | 9 | |
| Difficult-to-remove bile duct stones | Four stones in the main bile duct | DPOC-guided laser lithotripsy followed by stone removal | Yes | 13 |
| Suspected polyp in CBD | Stone in CBD | CBD stone | Yes | 20 |
| Suspicion for missed stones by ERCP | No stones found | Yes | 15 | |
| Difficult-to-remove bile duct stone | Large CBD stones | DPOC-guided laser lithotripsy followed by stone removal | Yes | 22 |
| Difficult-to-remove bile duct stone | Large stone above anastomotic stricture | DPOC-guided laser lithotripsy followed by stone removal | Yes | 16 |
Biliary access with an ultraslim upper endoscope was accomplished in all patients. In 12 of 14 (86%) patients, biliary access required sphincteroplasty with a 10-mm dilating balloon over a guidewire. In 13 of 14 (93%) patients, the bile duct mucosa from the bifurcation to the ampulla could be well visualized. In one patient, the common hepatic duct could not be examined due to a sigmoid-shaped main bile duct that prevented passage of the endoscope proximal to the common bile duct. In this patient, only the mucosa of the common bile duct was inspected.
Therapeutic measures were attempted in five patients. Four patients underwent removal of difficult-to-remove bile duct stones and one patient had intraductal biopsy.
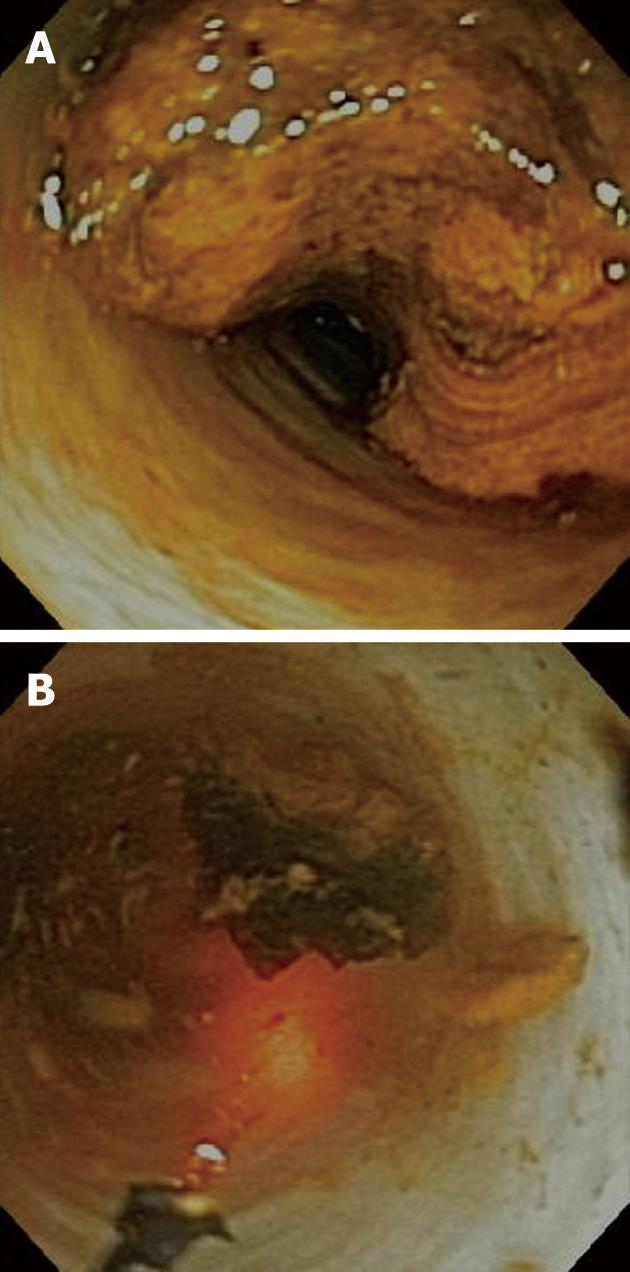
The four patients with difficult-to-remove stones had at least one prior unsuccessful attempt at stone extraction by ERCP with sphincterotomy, sphincteroplasty, and mechanical lithotripsy. In all cases, laser lithotripsy through the ultraslim upper endoscope successfully fragmented the stones, with subsequent removal of the fragments (Figure 2). In one of these cases, however, instability of the ultraslim upper endoscope after removal of the anchoring balloon, required passage of the laser probe (SlimLine GI, Lumenis, Santa Clara, CA, United States) into the bile duct alongside the anchoring balloon, while keeping the balloon inflated in one of the intrahepatic ducts to maintain access. Nonetheless, the procedure was successful with excellent views of the biliary mucosa and performance of laser lithotripsy under direct vision with fragmentation and subsequent removal of the stone fragments.
In one patient, DPOC was performed to evaluate an ill-defined filling defect at the biliary confluence with intrahepatic ductal dilatation seen on magnetic resonance imaging. DPOC successfully visualized the filling defect and showed it to be a tumor projecting into the bile duct lumen (Figure 3). Biopsies of the tumor were obtained through the ultraslim upper endoscope using a regular pediatric forceps (EndoJaw FB-221K; Olympus Corporation, Tokyo, Japan) and showed necrotic tissue. Follow-up imaging studies showed growing intraductal tumor suggesting cholangiocarcinoma.
One patient who had undergone orthotopic liver transplantation 2 years prior to the procedure, and was on immunosuppressive therapy, developed intrahepatic biloma at the site where the balloon was anchored within the duct (Figure 4). She underwent biliary stenting to assure ductal drainage. She also was given an intravenous dose of antibiotics during the procedure and discharged home on oral antibiotics and outpatient follow-up. However, 2 d after discharge she developed fever. She was admitted to the hospital and treated with intravenous antibiotics followed by 2 wk of oral antibiotics after discharge. Repeat ERCP 8 wk after the index procedure showed resolution of the biloma.
Despite its many advantages, DPOC is rarely performed in nonacademic settings. The biggest disadvantage of DPOC has been the difficult and time-consuming task of bile duct cannulation with an upper endoscope, often ending in failure. There are several published reports in the endoscopic literature with innovative suggestions on how to achieve this task. Introduction of the endoscope over a guidewire, through a regular overtube, or with the help of a double-balloon overtube are some of the suggestions[3-6]. However, despite use of these accessories, failure rate remains high[7].
Different variations of inflatable balloons used as an anchor within the biliary tree have therefore been introduced for easier access[2,8]. Using such a device, we were able to gain access to the bile duct with an ultraslim upper endoscope in all cases and obtain high-quality images of the biliary mucosa. We were also able to perform necessary interventions such as shock wave lithotripsy or targeted biopsy in all cases in which therapy was attempted. In one of the therapeutic cases, however, the instability of the ultraslim endoscope upon removal of the balloon could only be remedied by keeping the anchoring balloon in position.
Although this device performed well for allowing access to the bile duct for performance of DPOC and assessment and therapy of disorders of the distal biliary system, we found it difficult to maneuver the endoscope and gain access to the ducts proximal to the bifurcation after deflation and removal of the anchoring balloon. This was mainly due to looping of the endoscope in the stomach or duodenum after removal of the balloon.
The anchoring balloon used in this study was voluntarily withdrawn from the market by the manufacturing company, reportedly because of possible increased risk of air embolism[9]. The possible increased risk of air embolism is probably due to the ability of the ultraslim upper endoscopes to insufflate the biliary tree with air, while at the same time blocking the escape rout of the insufflated air. In this study, we used irrigation with saline rather than air to distend the bile duct and visualize the mucosa of the biliary tree.
One of the patients developed a biloma at the anchoring site of the balloon. Although she had a full recovery with antibiotic therapy, ductal damage at the anchoring site may be another potential adverse event associated with use of anchoring balloons.
One of the main limitations of this study was the small number of patients. However, the primary objective of this study was to assess performance of this device in a limited number of patients. Another limitation was performance of the procedures in a tertiary care referral setting by an endoscopist proficient in all forms of peroral and percutaneous cholangioscopy. This may limit extrapolation of the results to other settings.
In conclusion, our experience suggests that anchoring balloons are effective for consistent access to the bile duct with an ultraslim upper endoscope for performance of diagnostic and therapeutic DPOC distal to the confluence of the right and left hepatic ducts. However, we urge caution with widespread use of anchoring balloons until more information on potential adverse effects is available.
Direct peroral cholangioscopy (DPOC) in its current state has significant limitations. Initial free biliary cannulation is cumbersome, time consuming, and associated with a significant failure rate. Even when access is obtained, intraductal maneuverability and stability may be compromised by looping of the endoscope in the stomach or duodenum.
To address the technical challenges associated with DPOC, a prototype biliary anchoring balloon has been designed. Feasibility of this system in an animal model has been assessed but human reports are lacking. This is the first study assessing utility of this prototype anchoring balloon for diagnosis and treatment of various biliary disorders.
Despite its many advantages, DPOC is rarely performed in nonacademic settings. The biggest disadvantage of DPOC has been the difficult and time-consuming task of bile duct cannulation with an upper endoscope, often ending in failure. There are several published reports in the endoscopic literature with innovative suggestions on how to achieve this task. Introduction of the endoscope over a guidewire, through a regular overtube, or with the help of a double-balloon overtube are some of the suggestions. However, despite use of these accessories, the failure rate remains high. Using an anchoring balloon, the authors were able to gain access to the bile duct with an ultraslim upper endoscope in all cases and obtain high-quality images of the biliary mucosa. They were also able to perform necessary interventions such as shock wave lithotripsy or targeted biopsy in all cases in which therapy was attempted.
This study suggests that anchoring balloons are effective for consistent access to the bile duct with an ultraslim upper endoscope for performance of diagnostic and therapeutic DPOC distal to the confluence of the right and left hepatic ducts.
The authors report clinical experiences of DPOC by using a novel balloon catheter as an assisting accessory. This is a well-written article. However, it is necessary that the authors offer more detailed descriptions and revise several major and minor points.
Peer reviewer: Jong H Moon, MD, PhD, Professor of Medicine, Digestive Disease Center, Bucheon Hospital, Soon Chun Hyang University, No. 1174 Jung-Dong, Wonmi-Ku, Bucheon 420-767, South Korea
S- Editor Cheng JX L- Editor Kerr C E- Editor Xiong L
| 1. | Parsi MA. Peroral cholangioscopy in the new millennium. World J Gastroenterol. 2011;17:1-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 52] [Cited by in F6Publishing: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Waxman I, Dillon T, Chmura K, Wardrip C, Chennat J, Konda V. Feasibility of a novel system for intraductal balloon-anchored direct peroral cholangioscopy and endotherapy with an ultraslim endoscope (with videos). Gastrointest Endosc. 2010;72:1052-1056. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853-857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 122] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 4. | Bohle W. A simple and rapid technique of direct cholangioscopy. Gastrointest Endosc. 2007;65:559. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Choi HJ, Moon JH, Ko BM, Hong SJ, Koo HC, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos). Gastrointest Endosc. 2009;69:935-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Moon JH, Ko BM, Choi HJ, Koo HC, Hong SJ, Cheon YK, Cho YD, Lee MS, Shim CS. Direct peroral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol. 2009;104:2729-2733. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Terheggen G, Neuhaus H. New options of cholangioscopy. Gastroenterol Clin North Am. 2010;39:827-844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Moon JH, Ko BM, Choi HJ, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos). Gastrointest Endosc. 2009;70:297-302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 122] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Efthymiou M, Raftopoulos S, Antonio Chirinos J, May GR. Air embolism complicated by left hemiparesis after direct cholangioscopy with an intraductal balloon anchoring system. Gastrointest Endosc. 2012;75:221-223. [PubMed] [Cited in This Article: ] |