Published online Apr 28, 2012. doi: 10.3748/wjg.v18.i16.1987
Revised: December 7, 2011
Accepted: March 10, 2012
Published online: April 28, 2012
We report a case of acute chylous ascites formation presenting as peritonitis (acute chylous peritonitis) in a patient suffering from acute pancreatitis due to hypertriglyceridemia and alcohol abuse. The development of chylous ascites is usually a chronic process mostly involving malignancy, trauma or surgery, and symptoms arise as a result of progressive abdominal distention. However, when accumulation of “chyle” occurs rapidly, the patient may present with signs of peritonitis. Preoperative diagnosis is difficult since the clinical picture usually suggests hollow organ perforation, appendicitis or visceral ischemia. Less than 100 cases of acute chylous peritonitis have been reported. Pancreatitis is a rare cause of chyloperitoneum and in almost all of the cases chylous ascites is discovered some days (or even weeks) after the onset of symptoms of pancreatitis. This is the second case in the literature where the patient presented with acute chylous peritonitis due to acute pancreatitis, and the presence of chyle within the abdominal cavity was discovered simultaneously with the establishment of the diagnosis of pancreatitis. The patient underwent an exploratory laparotomy for suspected perforated duodenal ulcer, since, due to hypertriglyceridemia, serum amylase values appeared within the normal range. Moreover, abdominal computed tomography imaging was not diagnostic for pancreatitis. Following abdominal lavage and drainage, the patient was successfully treated with total parenteral nutrition and octreotide.
- Citation: Georgiou GK, Harissis H, Mitsis M, Batsis H, Fatouros M. Acute chylous peritonitis due to acute pancreatitis. World J Gastroenterol 2012; 18(16): 1987-1990
- URL: https://www.wjgnet.com/1007-9327/full/v18/i16/1987.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i16.1987
Accumulation of lymph within the peritoneal cavity is a rare pathological entity described as chylous ascites. Most cases occur progressively and the patient suffers from abdominal distention, nausea, vomiting, fatigue or low grade fever. A small number of cases have reported an acute development which may present as a surgical urgency mimicking appendicitis, hollow organ perforation and generalized peritonitis (acute chylous peritonitis). We hereby document a rare case of acute chylous peritonitis in a 46-year-old man with a history of alcoholism presenting with hypertriglyceridemia and acute pancreatitis.
A 46-year-old man presented to the emergency department with an 8-h history of abdominal pain localized to the right abdomen. The pain was of acute onset and was primarily felt at the epigastrium. The patient also mentioned nausea and one episode of vomiting but no fever or diarrhea. Apart from a history of ankylosing spondylitis he also admitted systematical alcohol consumption over a period of several years (> 120 mg/d).
The patient’s overall health condition was not gravely affected, showing a temperature of 37.2 °C, heart rate at 100 bpm and arterial pressure of 125/75 mmHg. On examination, no bowel sounds could be heard and right upper and lower abdominal quadrants appeared tender at palpation with rebound tenderness. Rectal digital examination did not reveal blood or tenderness.
Laboratory investigation showed no elevation of white blood cell count (7.740/mL with 57% polymorphonuclear leukocytes) while C-reactive protein values were only slightly affected (14 mg/L). The patient’s biochemistry showed a mild elevation of hepatic enzymes (aspartate aminotransferase: 107 IU/L, alanine aminotransferase: 45 IU/L, alkaline phosphatase: 165 IU/L and total bilirubin: 1.6 mg/dL). Amylase values were normal both in blood (55 IU/L) and urine samples (404 IU/L). The laboratory notes mentioned that the blood sample of the patient was not totally appropriate for analysis because of a high concentration of lipids. Plain chest and abdominal X-rays(supine and elevated position) revealed no significant pathology such as free air or ileus. The computed tomography (CT) scan showed the presence of free fluid in the abdominal cavity, mainly at the subhepatic space and the right paracolic space, with mild inflammatory changes around the pancreatic head (Figure 1). No atrophy of the pancreas or calcification of the main pancreatic duct was demonstrated.
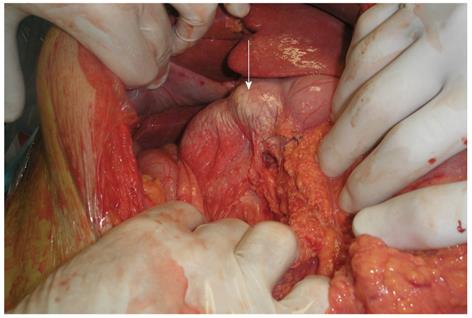
The patient was subsequently taken to the operating room for an exploratory laparotomy. In the peritoneal cavity a great amount of “milky” peritoneal fluid was discovered. Specimens were taken for biochemistry and microbiology. Careful examination of the abdomen revealed a bulky and rigid pancreatic head. Moreover, the surface of the distal stomach, duodenum and upper segment of posterior peritoneum had a white, milky-like appearance (Figure 2). A laceration in the peritoneum (at the root of the transverse mesocolon) was discovered, through which the milky fluid, apparently of retroperitoneal origin, entered the peritoneal cavity. Attempts to obtain a biopsy specimen from the pancreas (with a biopsy needle) were unsuccessful because of hemorrhage after the first attempt due to the pancreatic edema. After a thorough peritoneal lavage and the insertion of 3 drain tubes the midline incision was closed.
During the initial postoperative days, serum samples from the patient appeared to be of high lipidemic concentration, with normal serum amylase values. Only after serial dilutions with the assay buffer were we able to obtain a proper sample for analysis, showing serum amylase values of 870 IU/L. Total cholesterol reached as high as 618 IU/L (normal values up to 200) and triglycerides had a concentration greater than 1.000 mg/dL (normal values up to 175). No elevation of white blood cell count was documented at any time. Analysis of samples from free peritoneal fluid that was collected intraoperatively showed 337 mg/dL cholesterol and 2800 mg/dL triglyceride thus establishing the diagnosis of chylous ascites. Laboratory investigation of the fluid from the drain tubes showed values of amylase to be as high as 60 000 IU/L, decreasing to normal at postoperative day 7, at which time all of the tubes had been removed. Cancer markers α-fetoprotein, carcinoembryonic antigen and carbonic anhydrase 19-9 were within normal values.
The patient received nothing po for 10 d and then was restored gradually to a full (fat-free) diet. Total fat-free parenteral nutrition was given intravenously from postoperative day 4 and for the subsequent 2 wk. Broad spectrum antibiotics were administered for 1 wk postoperatively and were not stopped because the patient suffered outbursts of fever during the end of the first week. Twenty five days after the first operation a second procedure was undertaken, this time due to persisting ileus. The laparotomy revealed adhesions in the peritoneal cavity. Octreotide (0.1 mg) was administered every 8 h from the day of the first surgery until the time of discharge, which came to be after 33 d of hospitalization.
Under normal circumstances, lymph from the lower parts of the body as well as from the viscera is circulated through lymphatic vessels that follow a retroperitoneal course before emptying in the cisterna chyli and finally the thoracic duct and the venous system. This fluid consists of converted long-chain triglycerides at high concentrations that originate from the gut during ingestion. In cases wherea disruption to this normal flow occurs, the peritoneal cavity may be filled with a high-density, milky-like fluid that is called “chyle”. Although there are no unequivocal diagnostic criteria, it is generally agreed that a high concentration of lipids is indicative[1]. A sample of ascites fluid (either acquired by paracentesis or during laparotomy) showing values of triglycerides 2 to 8 times that of plasma is characterized as chyle and the situation “chylous ascites” or “chyloperitoneum”. Some authors have set absolute indicators such as a peritoneal lipid content greater than 200 mg/dL[2]. Other characteristics of chyle are a protein concentration ratio > 0.5 compared to that of plasma, a low cholesterol level (lower than plasma) and elevated amylase values in case of pancreatitis[3].
The formation of chylous ascites is usually a chronic procedure, and the patient typically mentions symptoms of progressive and painless distention of the abdomen for some time before the diagnosis is established. Multiple causes for this relatively rare pathological entity have been described. Aalami et al[1] present a detailed classification of them in a comprehensive review published in 2000. Whereas congenital abnormalities in the formation of the lymphatic vessels (lymphatic hypoplasia or lymphangiectasia) are a frequent cause in infants, surgery and malignancy (especially lymphoma) are among the most common causes in adults[4]. In particular, surgery involving the thoracic cavity or the aorta and the retroperitoneal space has often been associated with the pathogenesis of chylous ascites by means of interrupting the normal lymphatic drainage[5]. Chyloperitoneum may also be the result of trauma to the intestines or mesentery. Idiopathic retroperitoneal fibrosis, sarcoidosis and abdominal or pelvic radiation therapy have also been mentioned in the literature. Infectious diseases are another possible cause, such as filariasis in tropical countries, and tuberculosis mostly in countries with low social and economical level[1].
However, in rare cases the accumulation of chyle within the peritoneal cavity may occur rapidly and the patient may present with symptoms and signs of acute abdomen[6]. Vettoretto et al[6] found less than a 100 cases of acute chylous peritonitis in their review of 2008. The pain appears to be diffuse, possibly due to peritoneal distention and irritation of the root of the mesentery as the retroperitoneal space expands, since the fluid itself is not irritating to the peritoneum. During clinical examination, rebound tenderness and guarding may be documented, which is often localized at the right iliac fossa and this can possibly be explained by pooling of chyle at the right paracolic gutter. Thus the clinical picture may be misleading, with appendicitis, hollow organ perforation and visceral ischemia being the most commonly suspected diagnosis preoperatively[3,7-9]. Chyloperitoneum is usually discovered during exploratory laparotomy, and in some cases this is the only intraoperative finding. Negative laparotomies have been reported[3,6,10,11], in which the underlying cause was never discovered[11].
Pancreatitis is a rare cause of chylous ascites formation[12]. It is believed that either lymph may actually leak through destroyed lymphatics due to pancreatic enzyme erosion or that chylous accumulation is the result of exudation of chyle, caused by the obstruction of lymphatic channel flow secondary to severe inflammatory changes that take place in the retroperitoneal space surrounding the pancreas[1]. Most cases involve chronic pancreatitis[13], though acute pancreatitis has also been recognized as the causative reason, with the first such report dating back to 1984[12]. Since then, only a few cases of chylous ascites secondary to acute pancreatitis have been documented[8,13-15]. In almost all of them, the presence of chyle into the peritoneal cavity was discovered at some time after the episode of pancreatitis, usually days or weeks[13-15]. However, Khan et al[16]reported a case of acute hyperlipidemic pancreatitis-with normal serum amylase as in our case-that presented with acute chylous peritonitis and was treated conservatively. Smith et al[3] operated on a patient with relapsing pancreatitis and acute chylous ascites formation, due to a clinical resemblance with appendicitis.
Therapeutic choices may vary in accordance with the underlying pathology. Thorough lavage of the abdomen and adequate drainage has proven to be an excellent treatment modality for acute chylous peritonitis, since resolution of chylous ascites usually occurs within the next few days. However, successful conservative treatment has also been reported[13,16-18]. This requires proper preoperative diagnosis, which is often difficult due to the exceptional rarity of this pathological condition and its resemblance to other surgical urgencies that call for immediate laparotomy. Long-term fasting supported by total parenteral nutrition offers resolution in many cases. Alternatively, a highprotein and low fat diet has proven to be efficacious in reducing the amount of chyle produced. Administration of octreotide remains controversial[1,13].
In our case, the localization of the pain at the epigastrium and its later course mimicking peritonitis, together with the mild inflammatory changes of the pancreatic head demonstrated on CT imaging, as well as normal amylase values, drew the attention towards a possible duodenal perforation, thus leading the patient to the operating room. Only in the subsequent day and after serial dilutions of the serum samples with the assay buffer were we able to detect an abnormally high level of serum amylase. The interference of excessive serum triglyceride concentrations in the measurement of serum amylase is a known reason for false-negative results and this was also the case with our patient[16]. Moreover, routine serum lipase measurement is not available in our hospital, which could otherwise serve as an adjunct in the diagnosis of acute pancreatitis. However, it should be noted that serum lipase levels too can appear normal in patients with triglyceride-rich serum[16]. In our patient, peritoneal lavage and adequate drainage offered sufficient treatment, while the patient was gradually restored to a full fat-free diet in order to deal with the pancreatitis. Finally, the patient was encouraged to cease alcohol use.
In conclusion, acute abdominal pain due to sudden accumulation of chyle in the peritoneal cavity is a rare situation that the clinician should be aware of in cases of acute abdomen.
Peer reviewers: Antonio Basoli, Professor, General Surgery “Paride Stefanini”, Università di Roma-Sapienza, Viale del Policlinico 155, 00161 Roma, Italy; Naoaki Sakata, MD, PhD, Division of Hepato-Biliary Pancreatic Surgery, Tohoku University Graduate School of Medicine, 1-1 Seiryo-machi, Aoba-ku, Sendai, Miyagi 980-8574, Japan
S- Editor Shi ZF L- Editor Cant MR E- Editor Zhang DN
| 1. | Aalami OO, Allen DB, Organ CH. Chylous ascites: a collective review. Surgery. 2000;128:761-778. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 302] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 2. | Cárdenas A, Chopra S. Chylous ascites. Am J Gastroenterol. 2002;97:1896-1900. [PubMed] [Cited in This Article: ] |
| 3. | Smith EK, Ek E, Croagh D, Spain LA, Farrell S. Acute chylous ascites mimicking acute appendicitis in a patient with pancreatitis. World J Gastroenterol. 2009;15:4849-4852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Browse NL, Wilson NM, Russo F, al-Hassan H, Allen DR. Aetiology and treatment of chylous ascites. Br J Surg. 1992;79:1145-1150. [PubMed] [Cited in This Article: ] |
| 5. | Garrett HE, Richardson JW, Howard HS, Garrett HE. Retroperitoneal lymphocele after abdominal aortic surgery. J Vasc Surg. 1989;10:245-253. [PubMed] [Cited in This Article: ] |
| 6. | Vettoretto N, Odeh M, Romessis M, Pettinato G, Taglietti L, Giovanetti M. Acute abdomen from chylous peritonitis: a surgical diagnosis. Case report and literature review. Eur Surg Res. 2008;41:54-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Lamblin A, Mulliez E, Lemaitre L, Pattou F, Proye C. [Acute peritonitis: a rare presentation of chylous ascites]. Ann Chir. 2003;128:49-52. [PubMed] [Cited in This Article: ] |
| 8. | Michel P, Pagliano G. [Acute chyloperitoneum]. J Chir (Paris). 1992;129:544-549. [PubMed] [Cited in This Article: ] |
| 9. | Fang FC, Hsu SD, Chen CW, Chen TW. Spontaneous chylous peritonitis mimicking acute appendicitis: a case report and review of literature. World J Gastroenterol. 2006;12:154-156. [PubMed] [Cited in This Article: ] |
| 10. | Madding GF, Mclaughlin RF, Mclaughlin RF. Acute chylous peritonitis. Ann Surg. 1958;147:419-422. [PubMed] [Cited in This Article: ] |
| 11. | Weichert RF, Jamieson CW. Acute chylous peritonitis. A case report. Br J Surg. 1970;57:230-232. [PubMed] [Cited in This Article: ] |
| 12. | Goldfarb JP. Chylous effusions secondary to pancreatitis: case report and review of the literature. Am J Gastroenterol. 1984;79:133-135. [PubMed] [Cited in This Article: ] |
| 13. | Al-Ghamdi MY, Bedi A, Reddy SB, Tanton RT, Peltekian KM. Chylous ascites secondary to pancreatitis: management of an uncommon entity using parenteral nutrition and octreotide. Dig Dis Sci. 2007;52:2261-2264. [PubMed] [Cited in This Article: ] |
| 14. | Ben-Ami H, Nagachandran P, Assalia A, Edoute Y. Acute transient chylous ascites associated with acute biliary pancreatitis. Am J Med Sci. 1999;318:122-123. [PubMed] [Cited in This Article: ] |
| 15. | Zhang ZY, Howard JM. Chylous ascites. A late complication of massive peripancreatic necrosis. Int J Pancreatol. 1997;21:259-261. [PubMed] [Cited in This Article: ] |
| 16. | Khan FY, Matar I. Chylous ascites secondary to hyperlipidemic pancreatitis with normal serum amylase and lipase. World J Gastroenterol. 2007;13:480-482. [PubMed] [Cited in This Article: ] |
| 17. | Krizek TJ, Davis JH. Acute chylous peritonitis. Arch Surg. 1965;91:253-262. [Cited in This Article: ] |
| 18. | Thompson PA, Halpern NB, Aldrete JS. Acute chylous peritonitis. J Clin Gastroenterol. 1981;3 Suppl 1:51-55. [PubMed] [Cited in This Article: ] |