Published online Apr 28, 2012. doi: 10.3748/wjg.v18.i16.1953
Revised: November 24, 2011
Accepted: December 15, 2011
Published online: April 28, 2012
AIM: To investigate the efficacy of cap-fitted colonoscopy (CFC) with regard to cecal intubation time.
METHODS: Two hundred and ninety-five patients undergoing screening colonoscopy at Gospel Hospital, Kosin University College of Medicine were enrolled in this randomized controlled trial between January and December 2010. Colonoscopies were conducted by a single endoscopist. Patient characteristics including age, sex, body mass index, history of abdominal surgery, quality of preparation, and the presence of diverticulosis were recorded.
RESULTS: One hundred and fifty patients were allocated into a CFC group and 145 into a non-CFC (NCF) group. Cecal intubations were achieved in all patients. Cecal intubation time in the CFC group was significantly shorter than in the NCF group for specific conditions: age ≥ 60 years, prior abdominal surgery, and poor bowel preparation. The number of detected adenomas was higher in the CFC group than in the NCF group (P = 0.040).
CONCLUSION: CFC facilitated shortening of the cecal intubation time in difficult cases, and was more sensitive for detecting adenomas than was NCF.
- Citation: Kim HH, Park SJ, Park MI, Moon W, Kim SE. Transparent-cap-fitted colonoscopy shows higher performance with cecal intubation time in difficult cases. World J Gastroenterol 2012; 18(16): 1953-1958
- URL: https://www.wjgnet.com/1007-9327/full/v18/i16/1953.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i16.1953
Colorectal cancer is a major cause of cancer-related mortality and morbidity, and it is evident that this fatality rate has led to an increase in colonoscopy preventative treatment[1-3]. A multinational and multicenter survey performed in Asia has shown that the overall prevalence of advanced colorectal neoplasm in asymptomatic individuals is comparable with that in the West[4]. Removal of colonic adenomas by screening colonoscopy could reduce colorectal cancer incidence and mortality rate.
Colonoscopy, however, can be a complicated procedure and requires a skillful endoscopist[5-7]. The anatomical factors of difficult cecal intubation can usually be categorized into one of two problems: (1) an angulated and/or narrowed sigmoid colon; and (2) a redundant colon[8]. These anatomical difficulties are commonly observed in specific cases, such as female patients, older age, previous gynecologic surgery, and the presence of diverticulosis[9-17]. Published studies have suggested the use of a narrower instrument shaft or one with both a narrower shaft and a shorter bending section for use in angulated or narrowed sigmoid colons, and a stiffened shaft with simultaneous application of abdominal pressure for overcoming the problems associated with redundant colons[8,18,19]. However, these maneuvers are not always successful and may require the endoscopist to change instruments during the procedure.
Several studies have evaluated the efficacy of transparent cap-fitted colonoscopy (CFC) compared to that of non CFC (NCF), and have found no difference in cecal intubation time between CFC and NCF[20-22]. The one established advantage of CFC is that it is more sensitive to polyp detection than is NCF[20,21]. However, these results are not consistent with our daily experience, in that CFC requires a shorter time for cecal intubation than does NCF.
Short cecal intubation time is important for several reasons: less anesthetic medication is required; colonic inflation results in less discomfort; and sufficient withdrawal time for accurate examination. The purpose of this study was to evaluate whether CFC could result in shorter cecal intubation time compared with NCF. Additionally, we compared the detection rate of colonic adenomas in this study.
From January to December 2010, 300 consecutive patients scheduled for their first ever colonoscopy as a routine health check at Gospel Hospital, Kosin University College of Medicine were included in the study. Exclusion criteria were as follows: age < 18 years; hospitalization due to other diseases undergoing colonoscopy investigation; evidence of acute or chronic renal failure; cardiovascular diseases including recent myocardial infarction, congestive heart failure, unstable angina, and cardiac arrhythmias; ascites; electrolyte imbalance; active inflammatory bowel disease, ileus and/or suspected bowel obstruction; pregnant or breast feeding; or childbearing potential without adequate contraception. Patient medical history, demographic data, and body weight were recorded. For all patients, clinical hemodynamic, hematological, and biochemical measurements, including whole blood count, blood sugar, blood urea nitrogen, creatinine, and serum electrolyte (sodium, potassium, chloride, phosphorus, ionized calcium and magnesium) levels were measured. After initial evaluations, patients who had no exclusion criteria were randomized to receive CFC or NCF by one physician who was blinded to the results of previous colonoscopies. This study was approved by the Institutional Review Board of Kosin University College of Medicine, Busan, South Korea.
After providing informed consent, patients in both groups were encouraged to adhere to a clear liquid diet from 06:00 h to midnight on the day before colonoscopy, and further oral intake was not allowed after midnight. All patients drank 4 L of polyethylene glycol electrolyte lavage solution, starting 7 h before colonoscopy at a rate of 250 mL every 15 min until all of the solution had been consumed, as recommended by the manufacturer (Olympus Optical Corp, Tokyo, Japan). Before colonoscopy, a physical examination and clinical hemodynamic measurements were repeated. The transparent plastic cap (D-14304; Olympus Optical Corp., Toyko, Japan) used for CFC was 14 mm in outer diameter, 10 mm in length, and had a 1 mm wall thickness. This cap can be fitted and fixed to the tip of the colonoscope (CIF H260; Olympus Optical Corp.). To ensure consistency in the evaluations, all colonoscopies were performed by the same attending endoscopist using the standard technique of negotiating the colon with as little air insufflation as possible. The principal examination was carried out during withdrawal. Ileal intubation was attempted when it was relevant.
For evaluating the efficacy of CFC against NCF, the duration time of insertion up to the cecum was compared between the CFC and NCF groups. Additionally, the number of adenomas detected during colonoscopy was calculated. Factors presumed to influence cecal intubation time were sex, age, body mass index, and history of abdominal surgery; all of which were evaluated before colonoscopy. The quality of preparation was classified as follows: grade 0, percentage of visible mucosa > 90%, excellent visibility (small volume of clear liquid requiring minimal suctioning for adequate visualization), and no intestinal bubbles; grade 1, percentage of visible mucosa > 90%, good visibility (large volume of clear liquid or small amount of fecal residue, not preventing a reliable examination), and small number of intestinal bubbles; grade 2, percentage of visible mucosa > 90%, fair visibility (some semi-solid stool that could be suctioned or washed away, preventing a reliable examination), and moderate number of intestinal bubbles; and grade 3, percentage of visible mucosa < 90%, poor visibility (large amount of semi-solid stool that could not be suctioned or washed away, not allowing a complete examination to be done), and large number of intestinal bubbles. The number of adenomas was calculated during colonoscopy. Discomfort of each patient was recorded using a four-point scale (1: easy; 2: tolerable; 3: some pain; 4: severe pain).
Statistical analysis was performed using SPSS version 16.0 (SPSS, Chicago, IL, United States). For normally distributed continuous variables, Student’s t test was used to assess differences between the two groups. For categorical variables, Fisher’s exact test was used. Cox multivariate regression analysis was performed to produce statistically significant variables in the present study. Two-sided P values < 0.05 were considered statistically significant.
Initially, 150 patients volunteered for each group. However, five patients in the conventional endoscopy group withdrew their consent after finishing all examinations; therefore, 150 patients for cap-assisted colonoscopy and 145 patients for conventional colonoscopy were enrolled. There were no significant differences in the backgrounds between the group with CFC and that with NCF (Table 1).
| CFC(n = 150) | NCF(n = 145) | P value | |
| Gender | |||
| Male | 94 (62.7) | 87 (62.6) | 1.000 |
| Female | 56 (37.3) | 58 (37.4) | |
| Age (yr) mean ± SD | 65.4 ± 15.3 | 66.1 ± 14.8 | 0.736 |
| Body mass index (kg/m2), mean ± SD | 26.2 ± 10.6 | 27.4 ± 9.6 | 0.489 |
| History of abdominal surgery | 43 (28.6) | 32 (22.1) | 0.181 |
| Cesarean section | 20 (13.3) | 15 (10.3) | 0.474 |
| Appendectomy | 16 (10.6) | 10 (6.9) | 0.306 |
| Distal gastrectomy due to peptic ulcer | 7 (4.7) | 7 (4.8) | 1.000 |
| Diverticulosis | 51 (34.0) | 42 (30.0) | 0.382 |
| Preparation score 2 or 3 | 30 (20.0) | 31 (21.3) | 0.776 |
Cecal intubation was achieved in all cases regardless of method. The average time for insertion from anus to cecum was shorter in the CFC group than in the NCF group, but the difference was not statistically significant (262 ± 154 s vs 281 ± 138 s, P = 0.057). CFC showed greater adenoma detection than did NCF (2.0 ± 2.5 vs 1.2 ± 1.6; P = 0.040), especially for sessile adenomas (1.8 ± 1.9 vs 1.0 ± 0.9; P = 0.039). There was no significant difference between the two groups regarding patient discomfort scores during colonoscopy (2.3 ± 1.0 vs 2.3 ± 0.8, P = 0.741). These results are shown in Table 2.
| CFC(n = 150) | NCF(n = 145) | P value | |
| Cecal intubation time (s) | 262 ± 154 | 281 ± 138 | 0.057 |
| Number of detected adenomas | 2.0 ± 2.5 | 1.2 ± 1.6 | 0.040 |
| Size of adenoma (cm) | 2.0 ± 3.1 | 2.6 ± 2.9 | 0.061 |
| Sessile type, n | 1.8 ± 1.9 | 1.0 ± 0.9 | 0.039 |
| Pedunculated type, n | 0.4 ± 0.8 | 0.3 ± 0.7 | 0.557 |
| Patient discomfort, scores | 2.3 ± 1.0 | 2.3 ± 0.8 | 0.741 |
Multivariate analyses revealed that cecal intubation time was significantly longer in patients aged > 60 years, with a history of abdominal surgery, and two or three points in quality of bowel preparation as described in Table 3.
| Cecal intubation time | P value | |
| Gender | 0.881 | |
| Male | 254 ± 145 | |
| Female | 257 ± 135 | |
| Age (yr) | 0.012 | |
| < 60 | 244 ± 114 | |
| ≥ 60 | 322 ± 113 | |
| Body mass index (kg/m2) | 0.047 | |
| < 23 | 243 ± 114 | |
| ≥ 23 | 277 ± 125 | |
| History of abdominal surgery | 0.044 | |
| Yes | 387 ± 173 | |
| No | 221 ± 117 | |
| Diverticulosis | 0.747 | |
| Yes | 251 ± 146 | |
| No | 256 ± 142 | |
| Quality of preparation | 0.045 | |
| 0 or 1 | 278 ± 155 | |
| 2 or 3 | 364 ± 183 |
Multivariate analyses revealed that CFC required a significantly shorter cecal intubation time than did NCF in specific patients, including older patients (244 ± 123 s vs 330 ± 213 s; P = 0.009), those with history of abdominal surgery (240 ± 106 s vs 351 ± 219 s; P = 0.012), and those with bowel preparation score 2 or 3 (224 ± 96 s vs 302 ± 176 s; P = 0.006), as shown in Table 4.
| CFC | NCF | P value | |
| Gender | |||
| Male | 234 ± 109 | 257 ± 137 | 0.053 |
| Female | 276 ± 173 | 257 ± 134 | 0.997 |
| Age (yr) | |||
| < 60 | 249 ± 130 | 233 ± 106 | 0.784 |
| ≥ 60 | 244 ± 123 | 330 ± 213 | 0.009 |
| Body mass index (kg/m2) | |||
| < 23 | 246 ± 125 | 240 ± 118 | 0.067 |
| ≥ 23 | 296 ± 170 | 248 ± 148 | 0.674 |
| History of abdominal surgery | 240 ± 106 | 351 ± 219 | 0.012 |
| Diverticulosis | 218 ± 66 | 279 ± 189 | 0.169 |
| Quality of preparation | |||
| 0 or 1 | 255 ± 133 | 251 ± 147 | 0.861 |
| 2 or 3 | 224 ± 96 | 302 ± 176 | 0.006 |
Colonoscopy is a common endoscopic procedure. It is widely used for the investigation of lower gastrointestinal tract disorders and screening for colorectal adenomas[23]. However, failure to reach the cecum occurs in up to 10% of cases[10,24]. A transparent cap was initially designed for mucosectomy and was later used during colonoscopy to enhance colonic polyp detection[22]. CFC is an effective rescue method for patients who fail to achieve cecal intubation[25]. This benefit is more apparent for inexperienced colonoscopists[26]. Moreover, it has been shown that such a device can shorten cecal intubation time among experienced colonoscopists[27]. However, the present study showed that there was no significant difference between CFC and NCF in cecal intubation time, although the average cecal intubation time of CFC was shorter than that for NCF.
Although there was no significant difference in cecal intubation time between the two groups, CFC showed a shorter time than did NCF in several specific situations: age ≥ 60 years, history of abdominal surgery, and poor bowel preparation. In previous studies, predictive factors for incomplete colonoscopy were female sex, older age, previous gynecologic surgery, and the presence of diverticulosis[9-12]. In addition, female sex and older age are well known factors responsible for longer cecal intubation times[13-17]. Consistent with these previous results, CFC in the current study displayed a shorter cecal intubation time in difficult cases, such as in older patients, and those with a history of abdominal surgery, and poor bowel preparation. In our study, a single experienced endoscopist performed all procedures; this might be the reason why there was no difference between the two groups in cecal intubation time.
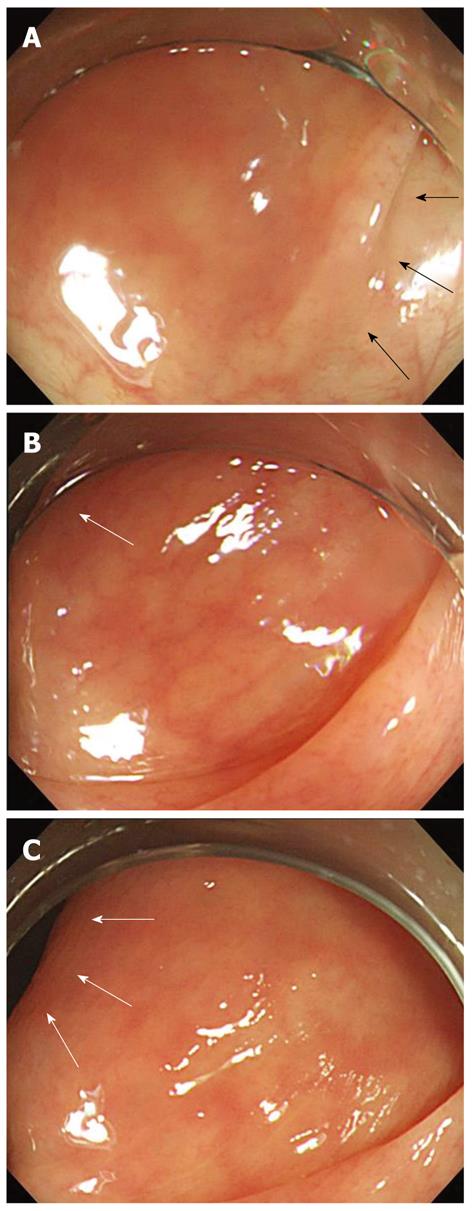
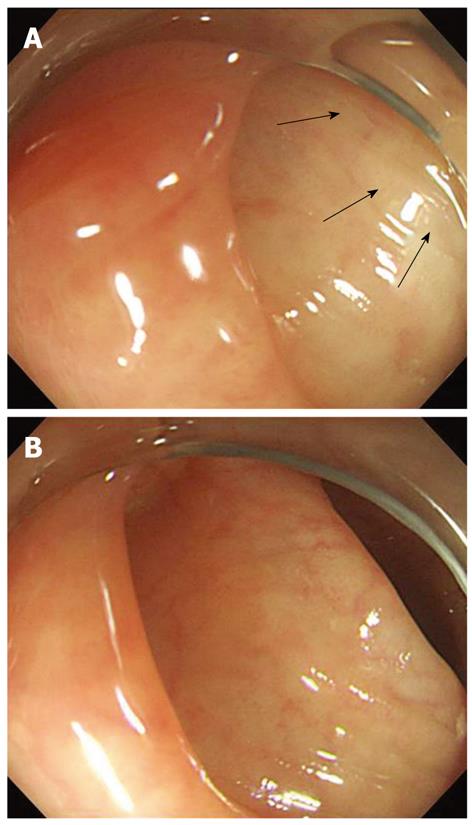
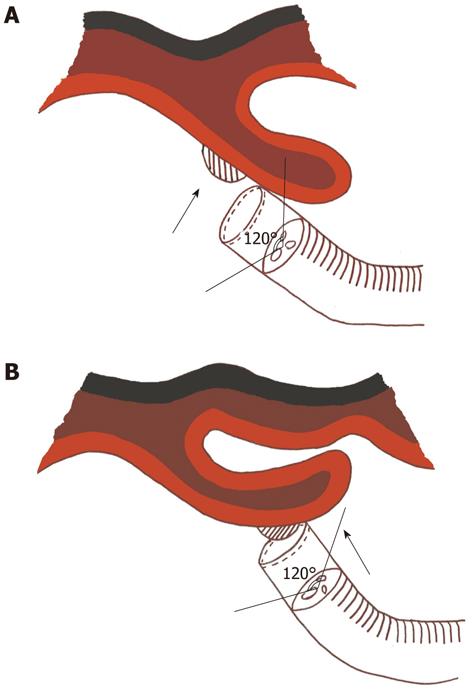
A possible explanation for this difference is less air insufflation during CFC than with NCF. A recent study revealed that the limited use of low-air insufflation in the rectum and sigmoid colon shortened the cecal intubation time and decreased post-procedural abdominal bloating[28]. Low-air insufflation causes less bowel inflation and produces less angulations of the bowel, thus enhancing cecal intubation. The use of CFC requires extremely low air insufflations. Experts in CFC can advance a cap-fitted colonoscope by pushing and pulling using meticulous lever manipulation without air insufflation, especially in the rectum and sigmoid colon. Extremely low air insufflation can be achieved in CFC because the cap prevents the mucosa from touching the lens directly and enables continuous lumen observation (Figure 1)[21]. Another important CFC characteristic is that the lateral side can be observed through the transparent wall of the cap (Figure 2)[21]. In the hepatic and splenic flexures, observing the lateral side through the transparent wall of the cap can help endoscopists determine the next step of the colonoscopy.
Another advantage of CFC in cecal intubation was that more adenomas were observed in the CFC group during withdrawal compared to those in the NCF group. Cap usage greatly facilitates the identification of small adenomas. During insertion and withdrawal of the cap-fitted colonoscope, the lumen of the colon can always be seen clearly because the mucosa never directly touches the lens[21]. The opposite, blind side of the folds can easily be observed and treated with fewer problems in CFC because they can be straightened to improve the view (Figure 3)[20], and the lateral side can be observed through the transparent wall of the cap[21]. Fecal matter may stick to the inside of the cap in cases of poor bowel preparation, thereby impairing the view. Using the water insufflation button or simple flushing through the biopsy channel can lead to ineffective cap clearing. The cap, however, was easily cleaned in CFC by pressing the whole circumference of the cap against the mucosal surface and then flushing the biopsy channel[20]. Moreover, CFC enhanced cecal intubation compared to that of NCF in cases of poor bowel preparation (scores of 2 and 3).
In conclusion, CFC has advantages in overcoming the problems associated with angulated and/or narrowed sigmoid and redundant colon, thereby resulting in significantly higher performance in cecal intubation time in difficult cases such as old age, prior abdominal operation, and poor bowel preparation. Furthermore, CFC displayed a higher sensitivity in detecting colonic adenomas than did NCF.
We acknowledge the contribution of Miss Da Hyun Ahn, first grade student in Kosin University College of Medicine, for creating the figures to explain the efficacy of CFC.
Colorectal cancer is a major cause of cancer-related mortality and morbidity, and it is evident that this fatality rate has led to an increase in colonoscopy preventative treatment. Colonoscopy, however, can be a complicated procedure and requires a skillful endoscopist. The anatomical factors of difficult cecal intubation can usually be categorized into one of two problems: (1) an angulated and/or narrowed sigmoid colon; and (2) a redundant colon. These anatomical difficulties are commonly observed in specific cases, such as female patients, older age, previous gynecological surgery, and the presence of diverticulosis. Published studies have suggested the use of a narrower instrument shaft or one with both a narrower shaft and a shorter bending section for use in angulated or narrowed sigmoid colons, and a stiffened shaft with simultaneous application of abdominal pressure for overcoming the problems associated with redundant colons.
Several studies have evaluated the efficacy of a transparent cap-fitted colonoscopy (CFC) compared to that of non-CFC (NCF) and found that there was no difference in cecal intubation time between CFC and NCF. The one established advantage of CFC is that it is more sensitive to polyp detection than is NCF.
The transparent plastic cap is made by Olympus Optical Corp., Tokyo, Japan. It is 17 mm in outer diameter, with a 2 mm wall thickness and 10 mm in length, and can be fitted and fixed to the tip of the colonoscope. This can cause less air insufflation during CFC than with NCF. Low-air insufflation causes less bowel inflation and produces less angulations of the bowel, thus enhancing cecal intubation. The present study aimed to evaluate whether CFC could result in shorter cecal intubation time compared with NCF. Additionally, the study compared the detection rate of colonic adenomas.
CFC has advantages in overcoming the problems associated with angulated and/or narrowed sigmoid and redundant colon, thereby resulting in significantly higher performance in cecal intubation time in difficult cases, such as elderly patients, and those with prior abdominal operation, and poor bowel preparation. Furthermore, CFC displayed a higher sensitivity in detecting colonic adenomas than did NCF.
Transparent CFC: a colonoscopic procedure with a transparent cap at the front view of the colonoscope.
The present study showed that CFC had shorter cecal intubation time in difficult cases. This is an interesting and good study.
Peer reviewer: Won Ho Kim, MD, Professor, Department of Internal Medicine, Yonsei University College of Medicine, 134 Shinchon-dong Seodaemun-ku, Seoul 120-752, South Korea
S- Editor Cheng JX L- Editor Kerr C E- Editor Zhang DN
| 1. | Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1214] [Cited by in F6Publishing: 1180] [Article Influence: 49.2] [Reference Citation Analysis (0)] |
| 2. | Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med. 2000;343:169-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 708] [Cited by in F6Publishing: 750] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 3. | Rex DK, Johnson DA, Lieberman DA, Burt RW, Sonnenberg A. Colorectal cancer prevention 2000: screening recommendations of the American College of Gastroenterology. American College of Gastroenterology. Am J Gastroenterol. 2000;95:868-877. [PubMed] [Cited in This Article: ] |
| 4. | Byeon JS, Yang SK, Kim TI, Kim WH, Lau JY, Leung WK, Fujita R, Makharia GK, Abdullah M, Hilmi I. Colorectal neoplasm in asymptomatic Asians: a prospective multinational multicenter colonoscopy survey. Gastrointest Endosc. 2007;65:1015-1022. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 107] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, Kirk LM, Litlin S, Lieberman DA, Waye JD. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296-1308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 691] [Cited by in F6Publishing: 700] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 6. | Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Mergener K, Petersen BT. Quality indicators for colonoscopy. Am J Gastroenterol. 2006;101:873-885. [PubMed] [Cited in This Article: ] |
| 7. | Barclay RL, Vicari JJ, Doughty AS, Johanson JF, Greenlaw RL. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med. 2006;355:2533-2541. [PubMed] [Cited in This Article: ] |
| 8. | Rex DK. Achieving cecal intubation in the very difficult colon. Gastrointest Endosc. 2008;67:938-944. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Dafnis G, Granath F, Påhlman L, Ekbom A, Blomqvist P. Patient factors influencing the completion rate in colonoscopy. Dig Liver Dis. 2005;37:113-118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Church JM. Complete colonoscopy: how often? And if not, why not? Am J Gastroenterol. 1994;89:556-560. [PubMed] [Cited in This Article: ] |
| 11. | Anderson JC, Gonzalez JD, Messina CR, Pollack BJ. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000;95:2784-2787. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 148] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 12. | Cirocco WC, Rusin LC. Factors that predict incomplete colonoscopy. Dis Colon Rectum. 1995;38:964-968. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 132] [Cited by in F6Publishing: 140] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Waye JD, Bashkoff E. Total colonoscopy: is it always possible? Gastrointest Endosc. 1991;37:152-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 142] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Bernstein C, Thorn M, Monsees K, Spell R, O'Connor JB. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005;61:72-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 143] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Ristikankare M, Hartikainen J, Heikkinen M, Janatuinen E, Julkunen R. The effects of gender and age on the colonoscopic examination. J Clin Gastroenterol. 2001;32:69-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Anderson JC, Messina CR, Cohn W, Gottfried E, Ingber S, Bernstein G, Coman E, Polito J. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001;54:558-562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 181] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 17. | Kim WH, Cho YJ, Park JY, Min PK, Kang JK, Park IS. Factors affecting insertion time and patient discomfort during colonoscopy. Gastrointest Endosc. 2000;52:600-605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 155] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Rex DK, Chen SC, Overhiser AJ. Colonoscopy technique in consecutive patients referred for prior incomplete colonoscopy. Clin Gastroenterol Hepatol. 2007;5:879-883. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Rex DK, Goodwine BW. Method of colonoscopy in 42 consecutive patients presenting after prior incomplete colonoscopy. Am J Gastroenterol. 2002;97:1148-1151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Dafnis GM. Technical considerations and patient comfort in total colonoscopy with and without a transparent cap: initial experiences from a pilot study. Endoscopy. 2000;32:381-384. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Tada M, Inoue H, Yabata E, Okabe S, Endo M. Feasibility of the transparent cap-fitted colonoscope for screening and mucosal resection. Dis Colon Rectum. 1997;40:618-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 58] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Matsushita M, Hajiro K, Okazaki K, Takakuwa H, Tominaga M. Efficacy of total colonoscopy with a transparent cap in comparison with colonoscopy without the cap. Endoscopy. 1998;30:444-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 124] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977-1981. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Aslinia F, Uradomo L, Steele A, Greenwald BD, Raufman JP. Quality assessment of colonoscopic cecal intubation: an analysis of 6 years of continuous practice at a university hospital. Am J Gastroenterol. 2006;101:721-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 132] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Lee YT, Hui AJ, Wong VW, Hung LC, Sung JJ. Improved colonoscopy success rate with a distally attached mucosectomy cap. Endoscopy. 2006;38:739-742. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 26. | Kondo S, Yamaji Y, Watabe H, Yamada A, Sugimoto T, Ohta M, Ogura K, Okamoto M, Yoshida H, Kawabe T. A randomized controlled trial evaluating the usefulness of a transparent hood attached to the tip of the colonoscope. Am J Gastroenterol. 2007;102:75-81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 119] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 27. | Lee YT, Lai LH, Hui AJ, Wong VW, Ching JY, Wong GL, Wu JC, Chan HL, Leung WK, Lau JY. Efficacy of cap-assisted colonoscopy in comparison with regular colonoscopy: a randomized controlled trial. Am J Gastroenterol. 2009;104:41-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 28. | Hsieh YH, Tseng KC, Lin HJ. Limited low-air insufflation is optimal for colonoscopy. Dig Dis Sci. 2010;55:2035-2042. [PubMed] [Cited in This Article: ] |