Published online Apr 7, 2012. doi: 10.3748/wjg.v18.i13.1508
Revised: January 6, 2012
Accepted: January 18, 2012
Published online: April 7, 2012
AIM: To clarify the efficiency of the criterion of metabolic syndrome to detecting non-alcoholic fatty liver disease (NAFLD).
METHODS: Authors performed a cross-sectional study involving participants of a medical health checkup program including abdominal ultrasonography. This study involved 11 714 apparently healthy Japanese men and women, 18 to 83 years of age. NAFLD was defined by abdominal ultrasonography without an alcohol intake of more than 20 g/d, known liver disease, or current use of medication. The revised criteria of the National Cholesterol Education Program Adult Treatment Panel III were used to characterize the metabolic syndrome.
RESULTS: NAFLD was detected in 32.2% (95% CI: 31.0%-33.5%) of men (n = 1874 of 5811) and in 8.7% (95% CI: 8.0%-9.5%) of women (n = 514 of 5903). Among obese people, the prevalence of NAFLD was as high as 67.3% (95% CI: 64.8%-69.7%) in men and 45.8% (95% CI: 41.7%-50.0%) in women. Although NAFLD was thought of as being the liver phenotype of metabolic syndrome, the prevalence of the metabolic syndrome among subjects with NAFLD was low both in men and women. 66.8% of men and 70.4% of women with NAFLD were not diagnosed with the metabolic syndrome. 48.2% of men with NAFLD and 49.8% of women with NAFLD weren’t overweight [body mass index (BMI) ≥ 25 kg/m2]. In the same way, 68.6% of men with NAFLD and 37.9% of women with NAFLD weren’t satisfied with abdominal classification (≥ 90 cm for men and ≥ 80 cm for women). Next, authors defined it as positive at screening for NAFLD when participants satisfied at least one criterion of metabolic syndrome. The sensitivity of the definition “at least 1 criterion” was as good as 84.8% in men and 86.6% in women. Separating subjects by BMI, the sensitivity was higher in obese men and women than in non-obese men and women (92.3% vs 76.8% in men, 96.1% vs 77.0% in women, respectively).
CONCLUSION: Authors could determine NAFLD effectively in epidemiological study by modifying the usage of the criteria for metabolic syndrome.
- Citation: Hamaguchi M, Takeda N, Kojima T, Ohbora A, Kato T, Sarui H, Fukui M, Nagata C, Takeda J. Identification of individuals with non-alcoholic fatty liver disease by the diagnostic criteria for the metabolic syndrome. World J Gastroenterol 2012; 18(13): 1508-1516
- URL: https://www.wjgnet.com/1007-9327/full/v18/i13/1508.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i13.1508
Nonalcoholic fatty liver disease (NAFLD) is a common clinical condition with histological features that resemble those of alcohol-induced liver injury, but occurs in patients who do not drink an excessive amount of alcohol (ethanol > 20 g/d)[1,2]. This disease is often associated with obesity[3], type 2 diabetes mellitus[4,5], dyslipidemia[6], and hypertension[7]. Each of these abnormalities carries a cardiovascular disease risk, and together they are often categorized as the insulin resistance syndrome or the metabolic syndrome[8-15].
NAFLD is now considered to be the hepatic representation of the metabolic syndrome[10-15].
Conventional radiology studies used in the diagnosis of fatty liver include ultrasound (US), computed tomography, and magnetic resonance (MR) imaging. Other than these radiological studies, we have no sensitive and low invasive screening method for NAFLD. Alanine aminotransferase (ALT) > 30 IU/L was usually used as the cut off level of screening NAFLD[16,17]. This threshold had a sensitivity of 0.92 for detecting the fatty-fibrotic pattern proven by ultrasound among obese children[18]. However, ALT was within normal levels in 69% of those who had increased liver fat[19]. Similarly, in the Dallas Heart Study, 79% of the subjects with a fatty liver (liver fat content > 5.6%) had normal serum ALT[20]. This implies that a normal ALT does not exclude steatosis. Aspartate aminotransferase (AST) and gamma glutamyltransferase (GGT) also correlate with liver fat content independent of obesity[21], but are even less sensitive than serum ALT.
It was well known that NAFLD was associated with the metabolic syndrome and patients with NAFLD tend to be accompanied with the abnormal component of the metabolic syndrome. However, the efficiency of the criterion of metabolic syndrome for detecting NAFLD has not yet been clarified. We aimed to clarify the efficiency and perform a cross sectional study among apparent healthy Japanese.
We performed a cross-sectional study involving participants of a medical health checkup program including abdominal ultrasonography. The program was conducted in the Medical Health Checkup Center at Murakami Memorial Hospital, Gifu, Japan. The purpose of the medical health checkup program is to promote public health through early detection of chronic diseases and the evaluation of their underlying risk factors. Known as a “human dock”, medical services of this kind are very popular in Japan.
All the subjects participating in such health checkup programs at Murakami Memorial Hospital between January 2004 and December 2008 were invited to join this study. The study was approved by the ethics committee of Murakami Memorial Hospital.
Data collection and exclusion criteria were described previously[8]. In short, we collected the data from urinalysis, blood cell counts, blood chemistry and abdominal ultrasonography. The medical history and lifestyle factors were collected by using a self-administered questionnaire. Exclusion criteria were an alcohol intake of more than 20 g/d, known liver disease, or current use of medication which could influence the metabolic syndrome such as anti-diabetic drugs, anti-hypertensive drugs, anti-dyslipidemic drugs, anti-gout drugs, and/or anti-obesity drugs[8,10].
According to the revised National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATPIII)[22] or the new International Diabetes Federation (IDF) definition[23], subjects who had three or more of the following criteria were diagnosed as having the metabolic syndrome. Fatty liver was defined on the basis of ultrasonographic findings[24]. Of 4 known criteria (hepatorenal echo contrast, liver brightness, deep attenuation, and vascular blurring), the participants were required to have hepatorenal contrast and liver brightness to be given a diagnosis of fatty liver[24].
During study period, we invited 20 012 participants in the health checkup program to enroll in the study. Of those, a total of 17 262 Japanese participants (10 329 men and 6933 women) were enrolled after giving informed consent to be included in the study. We excluded 621 participants (420 men and 201 women) who had known liver disease. In addition, 3330 participants (3042 men and 288 women) who consumed more than 20 g of ethanol per day and 1579 participants (1056 men and 541 women) who were currently receiving medication were excluded. As a result, this study ultimately consisted of 11 714 participants (5811 men and 5903 women). The mean ± SD age was 45.5 ± 9.4 years (range: 18 years to 83 years) for men and 44.3 ± 9.3 years (range: 18 years to 79 years) for women, respectively. The mean body mass index (BMI) was 23.2 ± 3.1 kg/m2 (range: 14.3 to 41.0 kg/m2) in men and 21.1 ± 3.0 kg/m2 (range: 14.0 to 58.3 kg/m2) in women, respectively. The mean abdominal circumference was 81.2 ± 8.1 cm (range: 57.3 cm to 127.5 cm) in men and 71.4 ± 8.2 cm (range: 49.0 cm to 145.0 cm) in women, respectively.
The R version 2.9.0 (available from http://www.r-project.org/) was used for statistical analyses. Two groups of subjects were compared by using the unpaired t-test and the chi-square test, and a P < 0.05 was accepted as a significant level.
The metabolic syndrome defined by revised NCEP-ATPIII definition was detected in 15.0% (95% CI: 14.1%-16.0%) of men (n = 873 of 5811) and in 5.1% (95% CI: 4.5%-5.7%) of women (n = 300 of 5903). The metabolic syndrome defined by IDF definition was detected in 8.2% (95% CI: 7.5%-9.0%) of men (n = 479 of 5811) and in 4.3% (95% CI: 3.8%-4.8%) of women (n = 254 of 5903) (Table 1).
| Men | Total n (%) | Obese n (%) | Non-obese n (%) |
| Number | 5811 | 1441 | 4370 |
| NAFLD | 1874 (32.2) | 970 (67.3) | 904 (20.7%) |
| 5 criteria of the metabolic syndrome | |||
| Increased abdominal circumference | 791 (13.6) | 703 (48.8) | 88 (2) |
| Elevated fasting glucose level | 1967 (33.8) | 704 (48.9) | 1263 (28.9) |
| Elevated blood pressure | 1294 (22.3) | 575 (39.9) | 719 (16.5) |
| Decreased HDL cholesterol level | 1736 (29.9) | 654 (45.4) | 1082 (24.8) |
| Elevated triglyceride level | 1063 (18.3) | 484 (33.6) | 579 (13.2) |
| ALT > 30 | 1269 (21.8) | 670 (46.5) | 599 (13.7) |
| MS defined by rNCEP-ATP III | 873 (15) | 578 (40.1) | 295 (6.8) |
| MS defined by IDF | 479 (8.2) | 443 (30.7) | 36 (0.8) |
| At least 1 criterion | 3680 (63.3) | 1291 (89.6) | 2389 (54.7) |
| At least 2 criteria | 1955 (33.6) | 957 (66.4) | 998 (22.8) |
| At least 1 criterion or ALT > 30 IU/L | 3885 (66.9) | 1337 (92.8) | 2548 (58.3) |
| Women | |||
| Number | 5903 | 563 | 5340 |
| NAFLD | 514 (8.7) | 258 (45.8) | 256 (4.8) |
| 5 criteria of the metabolic syndrome | |||
| Increased abdominal circumference | 878 (14.9) | 430 (76.4) | 448 (8.4) |
| Elevated fasting glucose level | 679 (11.5) | 176 (31.3) | 503 (9.4) |
| Elevated blood pressure | 578 (9.8) | 185 (32.9) | 393 (7.4) |
| Decreased HDL cholesterol level | 1320 (22.4) | 265 (47.1) | 1055 (19.8) |
| Elevated triglyceride level | 195 (3.3) | 73 (13) | 122 (2.3) |
| Elevated ALT (ALT > 30 IU/L) | 200 (3.4) | 78 (13.9) | 122 (2.3) |
| MS defined by rNCEP-ATP III | 300 (5.1) | 174 (30.9) | 126 (2.4) |
| MS defined by IDF | 254 (4.3) | 162 (28.8) | 92 (1.7) |
| At least 1 criterion | 2374 (40.2) | 511 (90.8) | 1863 (34.9) |
| At least 2 criteria | 853 (14.5) | 355 (63.1) | 498 (9.3) |
| At least 1 criterion or elevated ALT | 2430 (41.2) | 515 (91.5) | 1915 (35.9) |
Among obese people, the metabolic syndrome defined by revised NCEP-ATPIII definition was detected in 40.1% (95% CI: 37.6%-42.7%) of men and in 30.9% (95% CI: 27.1%-34.9%) of women, and the metabolic syndrome defined by IDF definition was detected in 30.7% (95% CI: 28.4%-33.2%) of men and in 28.8% (95% CI: 25.1%-32.7%) of women, respectively (Table 1).
NAFLD was detected in 32.2% (95% CI: 31.0%-33.5%) of men (n = 1874 of 5811) and in 8.7% (95% CI: 8.0%-9.5%) of women (n = 514 of 5903). The prevalence of NAFLD in men was four times higher than those in women (Table 1). Among obese people, the prevalence of NAFLD was as high as 67.3% (95% CI: 64.8%-69.7%) in men and 45.8% (95% CI: 41.7%-50.0%) in women (Table 1). NAFLD was associated with body fat accumulation strongly both in men and women.
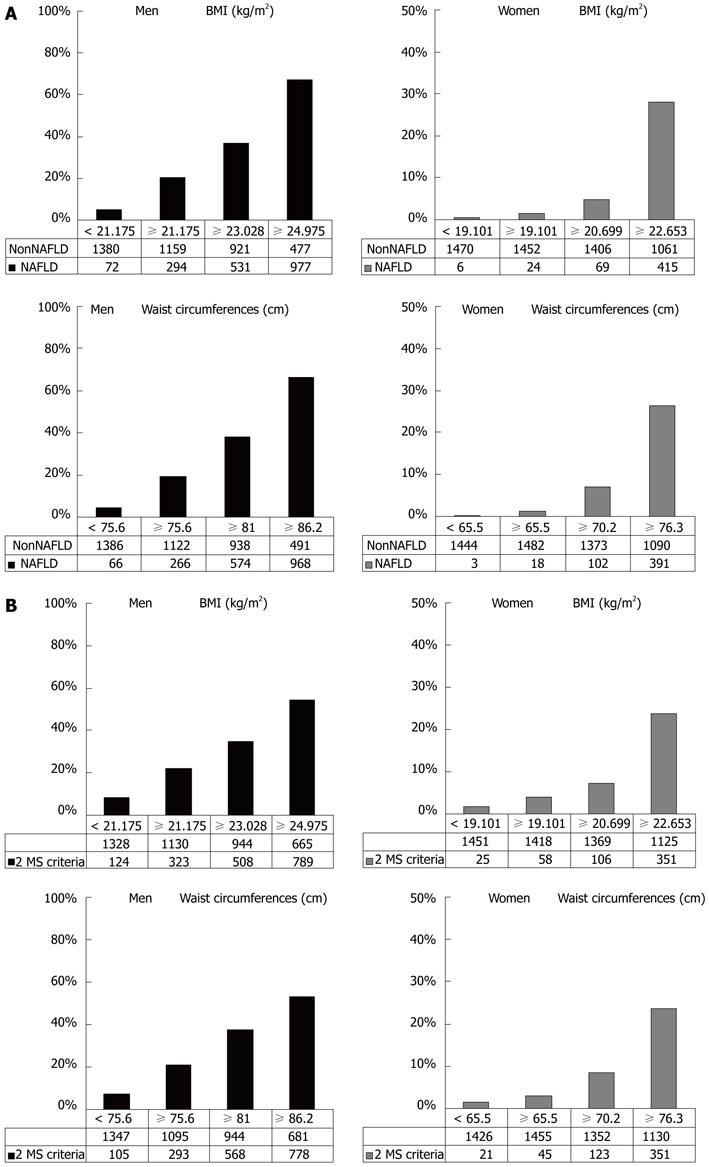
When we separated by quartile the subjects according to their BMI or abdominal circumference, half of NAFLD men and three quarters of NAFLD women were classified in the superior quartile. The prevalence of NAFLD was increased according to the increase of BMI or abdominal circumference (Figure 1A). The role of BMI for NAFLD was equal to that of abdominal circumference both in men and women. The ratio of NAFLD in the superior quartile/total NAFLD was higher in women than in men. The prevalence of individuals who met two or more of the MS criteria other than waist circumference was increased according to the increase of BMI or abdominal circumference (Figure 1B).
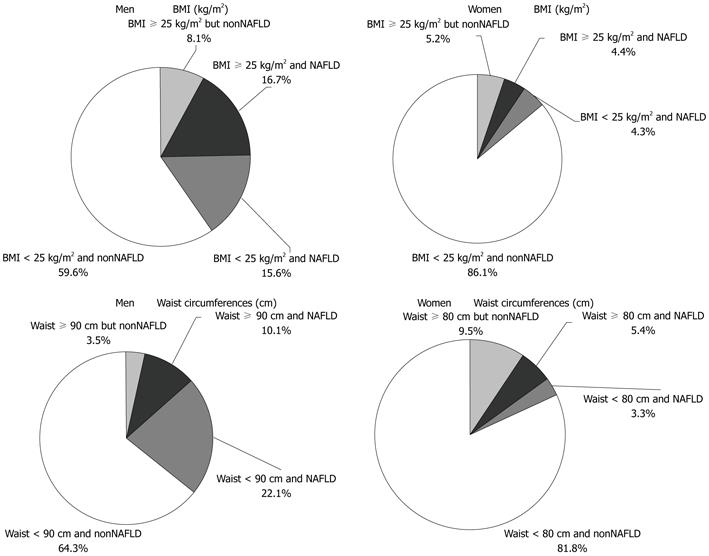
Although NAFLD was associated with obesity or body fat accumulation strongly, the population that was neither overweight (BMI ≥ 25 kg/m2) nor had elevated abdominal circumference was not small (Figure 2). Actually, 48.2% of men with NAFLD and 49.8% of women with NAFLD were not overweight (BMI ≥ 25 kg/m2). Similarly, 68.6% of men with NAFLD and 37.9% of women with NAFLD did not satisfy increased abdominal circumference classification. Half of the NAFLD group was classified as non-obese, but the prevalence of NAFLD among the non-obese population was lower. These facts means an effective method is needed to detect NAFLD among the non-obese population. Then, we separated the subjects into two groups, obese group or non-obese group, and investigated the efficacy of the criteria of metabolic syndrome for detecting NAFLD in each group.
Among the criteria for metabolic syndrome, the criterion of abdominal circumferences (≥ 80 cm) had high sensitivity (87.6%) for detecting NAFLD in women who were overweight (BMI ≥ 25 kg/m2) (Table 2). In other words, abdominal circumference was effective for detecting NAFLD in obese women. However, the criterion of abdominal circumference had low sensitivity (36.3%) in non-obese women. The sensitivity of abdominal circumference (≥ 90 cm) was very low (5.8%) in non-obese men. Even in obese men the sensitivity was not high (55.3%). Other criteria for metabolic syndrome had higher sensitivity in obese men and women than in the non-obese population but sensitivity never exceeded 60%.
| Men | Women | |||||||
| Sensitivity 5 criteria of the metabolic syndrome | Total % | Obese % | Non-obese % | P value | Total % | Obese % | Non-obese % | P value |
| Increased abdominal circumference | 31.40 | 55.30 | 5.80 | < 0.001 | 62.10 | 87.60 | 36.30 | < 0.001 |
| Elevated fasting glucose level | 49.10 | 52.10 | 45.90 | 0.008 | 36.80 | 42.20 | 31.30 | 0.013 |
| Elevated blood pressure | 34.70 | 44.10 | 24.60 | < 0.001 | 31.90 | 41.50 | 22.30 | < 0.001 |
| Decreased HDL cholesterol level | 44.10 | 49.10 | 38.80 | < 0.001 | 50.40 | 56.60 | 44.10 | 0.006 |
| Elevated triglyceride level | 35.20 | 41.00 | 28.90 | < 0.001 | 17.90 | 20.50 | 15.20 | 0.15 |
| Elevated ALT (ALT > 30 IU/L) | 47.90 | 59.20 | 35.80 | < 0.001 | 17.70 | 24.00 | 11.30 | < 0.001 |
| MS defined by rNCEP-ATP III | 33.20 | 48.60 | 16.80 | < 0.001 | 32.50 | 45.00 | 19.90 | < 0.001 |
| MS defined by IDF | 21.00 | 38.10 | 2.70 | < 0.001 | 29.60 | 43.40 | 15.60 | < 0.001 |
| At least 1 criterion | 84.80 | 92.30 | 76.80 | < 0.001 | 86.60 | 96.10 | 77.00 | < 0.001 |
| At least 2 criteria | 61.00 | 74.20 | 46.90 | < 0.001 | 61.10 | 77.50 | 44.50 | < 0.001 |
| At least 1 criterion or elevated ALT | 90.40 | 96.20 | 84.20 | < 0.001 | 87.40 | 96.90 | 79.70 | < 0.001 |
| Specificity | ||||||||
| 5 criteria of the metabolic syndrome | ||||||||
| Increased abdominal circumference | 94.80 | 64.50 | 99.00 | < 0.001 | 89.60 | 33.10 | 93.00 | < 0.001 |
| Elevated fasting glucose level | 73.40 | 57.70 | 75.50 | < 0.001 | 90.90 | 78.00 | 91.70 | < 0.001 |
| Elevated blood pressure | 83.60 | 68.80 | 85.70 | < 0.001 | 92.30 | 74.40 | 93.40 | < 0.001 |
| Decreased HDL cholesterol level | 76.90 | 62.20 | 78.90 | < 0.001 | 80.30 | 61.00 | 81.50 | < 0.001 |
| Elevated triglyceride level | 89.70 | 81.70 | 90.80 | < 0.001 | 98.10 | 93.40 | 98.40 | < 0.001 |
| Elevated ALT (ALT > 30 IU/L) | 90.60 | 79.60 | 92.10 | < 0.001 | 98.00 | 94.80 | 98.20 | < 0.001 |
| MS defined by rNCEP-ATP III | 93.60 | 77.30 | 95.90 | < 0.001 | 97.50 | 81.00 | 98.50 | < 0.001 |
| MS defined by IDF | 97.80 | 84.50 | 99.70 | < 0.001 | 98.10 | 83.60 | 99.00 | < 0.001 |
| At least 1 criterion | 46.90 | 15.90 | 51.10 | < 0.001 | 64.20 | 13.80 | 67.20 | < 0.001 |
| At least 2 criteria | 79.40 | 49.70 | 83.40 | < 0.001 | 90.00 | 49.20 | 92.40 | < 0.001 |
| At least 1 criterion or elevated ALT | 44.30 | 14.20 | 48.40 | < 0.001 | 63.20 | 13.10 | 65.40 | < 0.001 |
As a screening tool for NAFLD, the sensitivity of elevated ALT (ALT > 30 IU/L) was 49.7% in men, which exceeded the sensitivity of the criteria of metabolic syndrome, but it was 17.7% in women, which was lower than all metabolic syndrome criteria were. On the other hand, the specificity of elevated ALT was as high as 90.6% in men and 98.0% in women, but the criteria of metabolic syndrome had equally high specificity.
Next, we defined it as positive at screening for NAFLD when participants satisfied at least one or two components of metabolic syndrome. The sensitivity of the definition “at least 1 criterion” was 84.8% in men and 86.6% in women. Separating subjects with BMI, the sensitivity was higher in obese men and women than in non-obese men and women (92.3% vs 76.8% in men, 96.1% vs 77.0% in women, respectively).
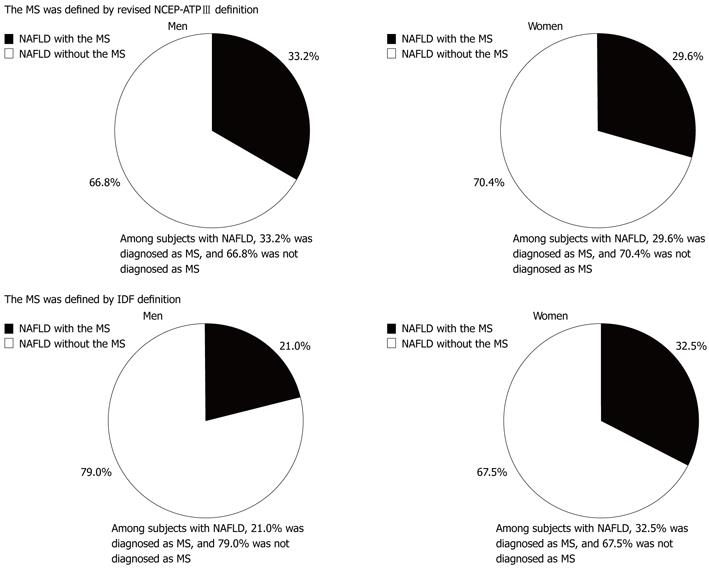
The prevalence of subjects with NAFLD who also had the metabolic syndrome is indicated in Figure 3. Although NAFLD was thought of as being the liver phenotype of metabolic syndrome, the prevalence of the metabolic syndrome among subjects with NAFLD was low both in men and women. Among men with NAFLD, 66.8% were not diagnosed with the metabolic syndrome defined by revised NCEP-ATPIII definition, and 79.0% were not diagnosed with the metabolic syndrome as defined by revised IDF definition. Even in women, 70.4% and 67.5%, respectively, were not diagnosed withmetabolic syndrome by revised NCEP-ATPIII definition and revised IDF definition. These results mean that a large number of participants diagnosed with the metabolic syndrome have NAFLD, but a large number of participants with NAFLD were not diagnosed with the metabolic syndrome, whether we used revised NECP-ATPIII criteria or IDF criteria.
In this study, we clarified the impact of the criteria of the metabolic syndrome for diagnosing NAFLD in a healthy population. The metabolic syndrome was associated with abdominal obesity and its criteria include waist circumference[22,23,25,26], and NAFLD was reported to be associated with abdominal obesity. However, our results indicated there was no significant difference between BMI and waist circumferences as the strength of association with NAFLD or the accumulation of metabolic syndrome criteria.
The presence of multiple metabolic disorders such as diabetes mellitus, obesity, dyslipidaemia and hypertension is associated with a potentially progressive, severe liver disease[15,27]. Previous reports demonstrated that prevalence of NAFLD increased to 10%-80% in individuals with obesity, 35%-90% in individuals with type 2 diabetes mellitus, 30%-56% in individuals with hypertension, and 26%-58% in individuals with dyslipidemia[9,28-30]. Another study in a Japanese population showed that prevalence of NAFLD increased to 43% in individuals with impaired fasting glucose and 62% in individuals with type 2 diabetes mellitus[28]. Some studies estimate the prevalence of NAFLD be up to 15%-30% of the general population[8,31,32], and the prevalence of metabolic syndrome was estimated to be up to 25% of the general population[33]. In those patients with the metabolic syndrome, liver fat content is significantly increased up to 4-fold higher than those without the metabolic syndrome[34], and the incidence of NAFLD has been shown to be increased 4-fold in men and 11-fold in women with the metabolic syndrome[8].
Our data clearly indicated that 21% to 33% of subjects with NAFLD, depending on gender and the criteria used, were diagnosed with the metabolic syndrome. Several previous studies reported how many subjects with NAFLD were diagnosed with the metabolic syndrome, but almost all previous studies were hospital studies. Three population based studies mentioned the prevalence of subjects with NAFLD who were diagnosed with the metabolic syndrome among the general population[8,35,36]. In these studies, the prevalence of the metabolic syndrome among subjects with NAFLD was 17% to 36% depending on gender and the criteria used. The reported prevalence was similar to ours.
There has been no report regarding the sensitivity and specificity of the metabolic syndrome for detecting NAFLD. Among the criteria for metabolic syndrome, the criterion of abdominal circumference had high sensitivity in obese women. However, it had low sensitivity (36.3%) in non-obese women and was very low (5.8%) in non-obese men and low (55.3% in obese men. Other than the criterion of abdominal circumference, none of the sensitivities exceeded 60%. In our study, the specificity of elevated ALT (ALT > 30 IU/L) was 90.6% in men and 98.0% in women. However, the sensitivity was as low as 47.9% in men and 17.7% in women. The specificity of elevated ALT was significantly higher among obese subjects than among non-obese subjects, and sensitivity was higher among obese subjects than among non-obese subjects.
When we investigated the predictability of each component of metabolic syndrome such as abdominal circumference, fasting blood sugar, serum lipid, and blood pressure, each component had high specificity but low sensitivity, similar to elevated ALT. Therefore, we defined it as screening positive for NAFLD, when subjects satisfied at least one criterion of metabolic syndrome; the sensitivity was 84.8% in men and 86.6% in women. Additionally, we defined it as positive when subjects satisfied at least one criterion of metabolic syndrome or elevated ALT. The sensitivity of “at least 1 criterion or elevated ALT” was 90.4% in men and 87.4% in women. However, the specificity of “at least 1 criterion or elevated ALT” was lower -44%-63%.
The result of our study means that we could identify NAFLD effectively in epidemiological study by modifying the usage of the criteria for metabolic syndrome. It is clinically critical evidence that a large part of patients with NAFLD were not diagnosed with the metabolic syndrome, when we used today’s definition for the metabolic syndrome. However, our subject population consisted only of Japanese, thus, the generalizability of our study to non-Japanese populations is uncertain. It is one of our study limitations that we used abdominal ultrasonography for diagnosing NAFLD, although the validation ultrasonography had a sensitivity of 91.7% and a specificity of 100%[24].
It is well known that non-alcoholic fatty liver disease (NAFLD) is associated with the metabolic syndrome and patients with NAFLD tend to also have the metabolic syndrome.
The impact of overlap between NAFLD and the metabolic syndrome has not been evaluated yet.
It is clinically critical evidence that a large number of patients with NAFLD were not diagnosed with the metabolic syndrome in a healthy Japanese population.
The authors could identify NAFLD effectively by modifying the usage of the criteria for metabolic syndrome.
It is a relatively large population study. The conclusion is consistent with recent observations showing the dissociation between NAFLD and other parameters of metabolic syndrome. The readers of this journal will be interested in the findings of this study.
Peer reviewer: Liqing Yu, Assistant Professor, Pathology-Lipid Sciences, Wake Forest University School of Medicine, Medical Center Boulevard, Winston-Salem 27157-1040, United States
S- Editor Gou SX L- Editor O’Neill M E- Editor Zhang DN
| 1. | Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467-2474. [PubMed] [Cited in This Article: ] |
| 2. | Mulhall BP, Ong JP, Younossi ZM. Non-alcoholic fatty liver disease: an overview. J Gastroenterol Hepatol. 2002;17:1136-1143. [PubMed] [Cited in This Article: ] |
| 3. | Bellentani S, Saccoccio G, Masutti F, Crocè LS, Brandi G, Sasso F, Cristanini G, Tiribelli C. Prevalence of and risk factors for hepatic steatosis in Northern Italy. Ann Intern Med. 2000;132:112-117. [PubMed] [Cited in This Article: ] |
| 4. | Akbar DH, Kawther AH. Nonalcoholic fatty liver disease in Saudi type 2 diabetic subjects attending a medical outpatient clinic: prevalence and general characteristics. Diabetes Care. 2003;26:3351-3352. [PubMed] [Cited in This Article: ] |
| 5. | Gupte P, Amarapurkar D, Agal S, Baijal R, Kulshrestha P, Pramanik S, Patel N, Madan A, Amarapurkar A. Non-alcoholic steatohepatitis in type 2 diabetes mellitus. J Gastroenterol Hepatol. 2004;19:854-858. [PubMed] [Cited in This Article: ] |
| 6. | Assy N, Kaita K, Mymin D, Levy C, Rosser B, Minuk G. Fatty infiltration of liver in hyperlipidemic patients. Dig Dis Sci. 2000;45:1929-1934. [PubMed] [Cited in This Article: ] |
| 7. | Donati G, Stagni B, Piscaglia F, Venturoli N, Morselli-Labate AM, Rasciti L, Bolondi L. Increased prevalence of fatty liver in arterial hypertensive patients with normal liver enzymes: role of insulin resistance. Gut. 2004;53:1020-1023. [PubMed] [Cited in This Article: ] |
| 8. | Hamaguchi M, Kojima T, Takeda N, Nakagawa T, Taniguchi H, Fujii K, Omatsu T, Nakajima T, Sarui H, Shimazaki M. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med. 2005;143:722-728. [PubMed] [Cited in This Article: ] |
| 9. | Radu C, Grigorescu M, Crisan D, Lupsor M, Constantin D, Dina L. Prevalence and associated risk factors of non-alcoholic fatty liver disease in hospitalized patients. J Gastrointestin Liver Dis. 2008;17:255-260. [PubMed] [Cited in This Article: ] |
| 10. | McCullough AJ. The clinical features, diagnosis and natural history of nonalcoholic fatty liver disease. Clin Liver Dis. 2004;8:521-533, viii. [PubMed] [Cited in This Article: ] |
| 11. | Adams LA, Angulo P. Recent concepts in non-alcoholic fatty liver disease. Diabet Med. 2005;22:1129-1133. [PubMed] [Cited in This Article: ] |
| 12. | Marchesini G, Marzocchi R, Agostini F, Bugianesi E. Nonalcoholic fatty liver disease and the metabolic syndrome. Curr Opin Lipidol. 2005;16:421-427. [PubMed] [Cited in This Article: ] |
| 13. | Neuschwander-Tetri BA. Nonalcoholic steatohepatitis and the metabolic syndrome. Am J Med Sci. 2005;330:326-335. [PubMed] [Cited in This Article: ] |
| 14. | Lavine JE, Schwimmer JB. Nonalcoholic fatty liver disease in the pediatric population. Clin Liver Dis. 2004;8:549-558, viii-ix. [PubMed] [Cited in This Article: ] |
| 15. | Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, Natale S, Vanni E, Villanova N, Melchionda N. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917-923. [PubMed] [Cited in This Article: ] |
| 16. | Fraser A, Longnecker MP, Lawlor DA. Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999-2004. Gastroenterology. 2007;133:1814-1820. [PubMed] [Cited in This Article: ] |
| 17. | Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr. 2000;136:727-733. [PubMed] [Cited in This Article: ] |
| 18. | Tazawa Y, Noguchi H, Nishinomiya F, Takada G. Serum alanine aminotransferase activity in obese children. Acta Paediatr. 1997;86:238-241. [PubMed] [Cited in This Article: ] |
| 19. | Szczepaniak LS, Nurenberg P, Leonard D, Browning JD, Reingold JS, Grundy S, Hobbs HH, Dobbins RL. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol Endocrinol Metab. 2005;288:E462-E468. [PubMed] [Cited in This Article: ] |
| 20. | Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387-1395. [PubMed] [Cited in This Article: ] |
| 21. | Thamer C, Tschritter O, Haap M, Shirkavand F, Machann J, Fritsche A, Schick F, Häring H, Stumvoll M. Elevated serum GGT concentrations predict reduced insulin sensitivity and increased intrahepatic lipids. Horm Metab Res. 2005;37:246-251. [PubMed] [Cited in This Article: ] |
| 22. | Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486-2497. [PubMed] [Cited in This Article: ] |
| 23. | Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469-480. [PubMed] [Cited in This Article: ] |
| 24. | Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T, Kato T, Takeda N, Okuda J, Ida K. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102:2708-2715. [PubMed] [Cited in This Article: ] |
| 25. | Stone NJ, Bilek S, Rosenbaum S. Recent National Cholesterol Education Program Adult Treatment Panel III update: adjustments and options. Am J Cardiol. 2005;96:53E-59E. [PubMed] [Cited in This Article: ] |
| 26. | World Health Organization Western Pacific Region, International Association for the Study of Obesity, International Obesity Task Force. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications 2000; . [Cited in This Article: ] |
| 27. | Marchesini G, Marzocchi R. Metabolic syndrome and NASH. Clin Liver Dis. 2007;11:105-117, ix. [PubMed] [Cited in This Article: ] |
| 28. | Jimba S, Nakagami T, Takahashi M, Wakamatsu T, Hirota Y, Iwamoto Y, Wasada T. Prevalence of non-alcoholic fatty liver disease and its association with impaired glucose metabolism in Japanese adults. Diabet Med. 2005;22:1141-1145. [PubMed] [Cited in This Article: ] |
| 29. | Fan JG, Zhu J, Li XJ, Chen L, Lu YS, Li L, Dai F, Li F, Chen SY. Fatty liver and the metabolic syndrome among Shanghai adults. J Gastroenterol Hepatol. 2005;20:1825-1832. [PubMed] [Cited in This Article: ] |
| 30. | Amarapurkar DN, Hashimoto E, Lesmana LA, Sollano JD, Chen PJ, Goh KL. How common is non-alcoholic fatty liver disease in the Asia-Pacific region and are there local differences? J Gastroenterol Hepatol. 2007;22:788-793. [PubMed] [Cited in This Article: ] |
| 31. | Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202-1219. [PubMed] [Cited in This Article: ] |
| 32. | Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005;42:44-52. [PubMed] [Cited in This Article: ] |
| 33. | Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356-359. [PubMed] [Cited in This Article: ] |
| 34. | Kotronen A, Westerbacka J, Bergholm R, Pietiläinen KH, Yki-Järvinen H. Liver fat in the metabolic syndrome. J Clin Endocrinol Metab. 2007;92:3490-3497. [PubMed] [Cited in This Article: ] |
| 35. | Sung KC, Ryan MC, Wilson AM. The severity of nonalcoholic fatty liver disease is associated with increased cardiovascular risk in a large cohort of non-obese Asian subjects. Atherosclerosis. 2009;203:581-586. [PubMed] [Cited in This Article: ] |
| 36. | Karnikowski M, Córdova C, Oliveira RJ, Karnikowski MG, Nóbrega Ode T. Non-alcoholic fatty liver disease and metabolic syndrome in Brazilian middle-aged and older adults. Sao Paulo Med J. 2007;125:333-337. [PubMed] [Cited in This Article: ] |