Published online Dec 7, 2011. doi: 10.3748/wjg.v17.i45.4993
Revised: May 26, 2011
Accepted: June 2, 2011
Published online: December 7, 2011
AIM: Prospective evaluation of repeat endoscopic retrograde cholangiopancreatography (ERCP) for failed Schutz grade 1 biliary cannulation in a high-volume center.
METHODS: Prospective intention-to-treat analysis of patients referred for biliary cannulation following recent unsuccessful ERCP.
RESULTS: Fifty-one patients (35 female; mean age: 62.5 years; age range: 40-87 years) with previous failed biliary cannulation were referred for repeat ERCP. The indication for ERCP was primarily choledocholithiasis (45%) or pancreatic malignancy (18%). Successful biliary cannulation was 100%. The precut needle knife sphincterotomy (NKS) rate was 27.4%. Complications occurred in 3.9% (post-ERCP pancreatitis). An identifiable reason for initial unsuccessful biliary cannulation was present in 55% of cases. Compared to a cohort of 940 naïve papilla patients (female 61%; mean age: 59.9 years; age range: 18-94 years) who required sphincterotomy over the same time period, there was no statistical difference in the cannulation success rate (100% vs 98%) or post-ERCP pancreatitis (3.1% vs 3.9%). Precut NKS use was more frequent (27.4% vs 12.7%) (P = 0.017).
CONCLUSION: Referral to a high-volume center following unsuccessful ERCP is associated with high technical success, with a favorable complication rate, compared to routine ERCP procedures.
- Citation: Swan MP, Bourke MJ, Williams SJ, Alexander S, Moss A, Hope R, Ruppin D. Failed biliary cannulation: Clinical and technical outcomes after tertiary referral endoscopic retrograde cholangiopancreatography. World J Gastroenterol 2011; 17(45): 4993-4998
- URL: https://www.wjgnet.com/1007-9327/full/v17/i45/4993.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i45.4993
Despite technical innovations, structured training programs and improved endoscopic imaging, failed biliary cannulation during endoscopic retrograde cholangiopancreatography (ERCP) occurs in 5%-20% of all cases[1]. Achieving biliary cannulation during ERCP remains an important and transparent determinant of a successful procedure for biliary endoscopists and patients alike. The American Society for Gastrointestinal Endoscopy recommendations suggest a biliary cannulation rate of > 85% should be the goal for all endoscopists engaged in ERCP[2]. Differing rates of successful biliary cannulations have been reported from community and tertiary institutions[1,3,4], with higher rates (up to 98%) achieved in specialized tertiary institutions[5,6,7], which reflects higher workload and experience, greater expertise, and more frequent use of more advanced cannulation techniques.
The therapeutic options following failed biliary cannulation may include: (1) repeat endoscopic attempt; (2) percutaneous cholangiography; (3) endoscopic ultrasound (EUS)-guided bile duct puncture and drainage; and (4) surgical management. This study was undertaken to assess the clinical impact of a tertiary referral ERCP service for prior unsuccessful biliary cannulation.
Over a 34-mo period to September 2009, patients referred for a repeat ERCP following a previous failed biliary cannulation were enrolled prospectively on an intention-to-treat basis. A number of different hospitals and endoscopists referred patients to our center following an unsuccessful unsuccessful biliary cannulation at ERCP. All the referring endoscopists were accredited specialist biliary endoscopists[8]. The indication for ERCP was evaluated and deemed appropriate to require a further attempt at biliary cannulation by both the referring specialist and our center. The referring specialist was asked to provide a reason (if any) as to the possible cause for the failed cannulation.
Procedures were performed under propofol-based sedation provided by an anesthetist. An Olympus Exera TJF-160R duodenoscope (Olympus Optical, Japan, Tokyo) was used.
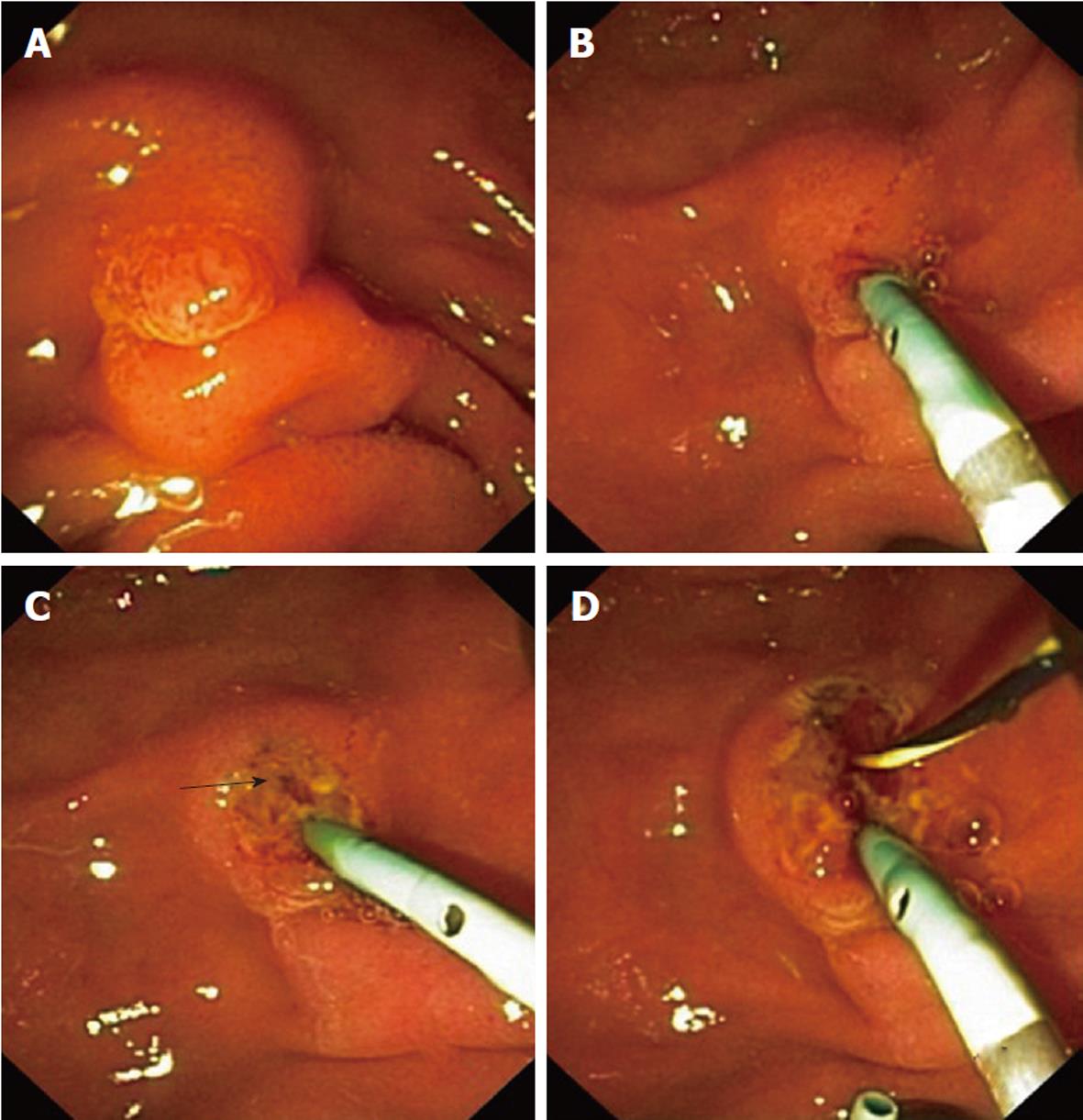
The cannulation technique and algorithm has been previously described in detail elsewhere[7]. A wire-guided technique utilizing a triple-lumen sphincterotome (CleverCut3™; Olympus Medical) and a 400-mm long hydrophilic wire (Jagwire™, Boston Scientific, Spencer, IN, United States) was used initially in all cases. In the event that a precut needle knife sphincterotomy was needed, all procedures used the conventional (freehand papillotomy/deroofing) needle knife sphincterotomy (NKS) method (Figure 1).
As is standard practice at our center[7,9], all cannulation parameters were recorded at the time of the procedure, including time to cannulation, number of attempts on papilla, number of pancreatic cannulations, and cannulation techniques performed. All procedures were performed by or under the direct supervision of two experienced high-volume biliary endoscopists (MJB, SJW). Clinical follow-up was obtained at 24 h and 30 d post-procedure.
Patients referred after prior failed cannulation were compared with a cohort of naïve papilla patients undergoing ERCP for a biliary indication performed at our center during the same time period.
Failed biliary cannulation was defined as the inability to gain deep and free access to the bile duct. Cholangiography alone without deep instrumentation of the bile duct was not recorded as being successful. Complications were defined and recorded according to established consensus criteria[10]. The indication and complexity of the ERCP procedure was graded according to the modified Schutz criteria (Table 1)[11]. Only Schutz grade 1 cases were included in this study. Exclusion criteria were patient age < 18 years old, surgically altered anatomy (Roux-en-Y, Billroth II partial gastrectomy), and duodenal obstruction. As a referral center, Schutz grade 2 and 3 cases were received and managed by our group but were not included in this study.
| Biliary procedures | |
| Grade 1 | Diagnostic cholangiogram |
| Biliary cytology | |
| Standard sphincterotomy ± removal of stones < 10 mm | |
| Stricture dilatation/stent for extra-hepatic stricture | |
| or bile leak | |
| Grade 2 | Diagnostic cholangiogram with |
| Billroth II anatomy | |
| Removal of CBD stones > 10 mm | |
| Stricture dilatation/stent for hilar tumors or benign intrahepatic strictures | |
| Grade 3 | SOD manometry |
| Cholangioscopy | |
| Any therapy with Billroth II anatomy | |
| Removal of intrahepatic stones or any stones with lithotripsy |
Primary endpoints were success of biliary cannulation and post-ERCP complications.
Statistical analysis was performed using StatPlus:mac LE, (AnalystSoft, Vancouver, BC, Canada). Student’s t test was used to detect differences between the two groups. Statistical significance was accepted on the basis of a P value < 0.05.
Fifty-one patients [35 female (69%); mean age: 62.5 years; age range: 40-87 years] with previously unsuccessful biliary cannulation at previous ERCP were referred and prospectively enrolled. The main indications for biliary cannulation and therapeutic intervention (Table 2) in the tertiary referral group were choledocholithiasis (45.1%), pancreatic malignancy (17.7%) and benign biliary disease [i.e., primary sclerosing cholangitis (PSC), chronic pancreatitis related biliary stricture] (12%).
| Indication | Tertiary referral cohort (n = 51) | Naïve papilla cohort (n = 940) | P value |
| Choledocholithiasis | 23 (45.1) | 446 (47.4) | 0.78 |
| Pancreatic malignancy | 9 (17.7) | 194 (20.6) | 0.72 |
| Benign biliary stricture/PSC | 6 (11.8) | 41 (4.4) | 0.03 |
| Bile leak | 5 (9.8) | 59 (6.3) | 0.37 |
| Cholangitis | 4 (7.8) | 57 (6.1) | 0.48 |
| Other (acute pancreatitis, suspected sphincter dysfunction) | 4 (7.8) | 143 (15.2) | 0.22 |
All referred ERCP procedures were assessed as grade 1 difficulty, indicating that they were applicable to be performed by all competent biliary endoscopists. Eleven (21.6%) patients had had a previously attempted precut NKS. Two patients (5%) had post-ERCP pancreatitis (PEP) following their initial unsuccessful biliary cannulation.
Biliary cannulation was successful in all 51 referred patients in a single procedure. A mean of 2.96 attempts (range: 1-8) was required to gain biliary access, with a mean time to successful cannulation of 4.4 min (range: 0.8-13.5 min). Fourteen patients (27.4%) required precut NKS. Eleven patients (21.6%) had had a previous precut NKS attempt before referral, of which 7 seven (64%) required a further NKS to gain biliary access. Two patients (3.9%, both choledocholithiasis indication) developed moderate severity PEP (requiring uncomplicated 5 d and 4 d inpatient stays, respectively). Definitive organic findings (choledocholithiasis, biliary sludge, stricture, malignancy) were identified in 42/51 patients (82%), with the remainder having non-specific features such as biliary duct dilatation only.
The naïve ERCP cohort comprised 940 patients (female 61%; male 39%; mean age: 59.9 years; age range: 18-96 years) and was not significantly different from the referred failed ERCP cohort (Table 3). Indications were similar to those in the referral cohort (Table 2). The majority of procedures were performed for either choledocholithiasis (47.4%) or pancreatic malignancy (20.6%). Cannulation success was 98% (920/940), and 12.7% required NKS to gain access to the bile duct. A mean 3.2 cannulation attempts (range: 1-14) was required to gain biliary access, with a mean time to successful cannulation of 4.2 min (range: 8 s-41 min). The complication rate was 3.8% overall: 3.1% PEP, 0.5% bleeding, and 0.2% perforation. Two patients had perforation following sphincterotomy and both were managed conservatively in hospital for 9 and 11 d, respectively.
| Non-referred naive papilla | Previous failed biliary cannulation | P value | |
| No. | 940 | 51 | |
| Mean age (yr) | 62.5 (40-87) | 59.9 (18-96) | NS |
| Sex (female:male) | 69:31 | 61:39 | NS |
| Cannulation attempts | 3.2 (1-14) | 2.96 (1-8) | NS |
| Time to cannulation | 4.2 min (0.08-41) | 4.4 min (0.8-13.5) | NS |
| Cannulation success | 98% | 100% | 1.00 |
| NKS rate | 12.7% | 27.4% | 0.017 |
| PEP | 3.1% | 3.9% | 1.00 |
| Other ERCP complication | Bleeding 0.5% | Nil | |
| Perforation 0.2% |
No reason for the initial failed biliary cannulation was identified in 23 (45%) patients. The 28 patients (55%) with an identifiable reason had a wide range of possible explanations for initial failure, including long and mobile (floppy) papilla and intraduodenal segment of the common bile duct (n = 8, 29%), unstable position (n = 9, 32%), small papilla (n = 4, 14%) or periampullary diverticulum (n = 7, 25%). In two of the periampullary diverticular cases, the papilla could not be identified at the initial procedure.
Technical rates, rates of successful biliary cannulation and complications were comparable in both groups (Table 3). Only the use of precut NKS in the tertiary referral cohort was significantly different at 27.4% vs 12.7% (P = 0.017). Half of the NKS procedures were performed in patients with a previous NKS attempt. Correcting for this variable, the NKS rate in the referred group was still statistically significantly greater (20%) than in the comparison group (P < 0.05).
Following a failed cannulation attempt, the endoscopist, in consultation with the patient and family, should carefully consider the next management step. The procedural indication and the definitive need for therapeutic intervention should be re-evaluated. Non-invasive imaging including magnetic resonance cholangiography or EUS should be utilized if they are likely to add value before proceeding. This study demonstrates that following an unsuccessful attempt at biliary cannulation, a further attempt in a tertiary referral center achieves a high success rate with minimal complications. We have specifically examined Schutz grade 1 patients; a cohort typical of cases managed by appropriately trained and competent biliary endoscopists in routine practice. The current study’s incidence of complications of 3.9% (which was limited to PEP) is not different from the large and carefully studied comparison group or from other large recently published studies[12,13].
Outcomes for a repeat endoscopic attempt following unsuccessful ERCP in heterogeneous groups of patients have been reported > 10 years previously[14-16]. The past decade has seen many changes in ERCP practice, coupled with enhanced awareness of the risk factors for complications, particularly PEP, and greater utilization of non-invasive imaging. The importance of dedicated training and continuous quality audit has also been more widely recognized. The endoscopes, accessories utilized and cannulation techniques used have also evolved. This contemporary study carefully examined a well-characterized group of Schutz grade 1 cases and confirmed that prior failure by a competent and accredited biliary endoscopist is not an absolute indication to seek an alternative strategy to access the biliary tree, nor is a repeat attempt associated with higher complications. In 1999, Ramirez et al[14] reported 47 patients with failed cannulation, of which 24 (51%) underwent repeat ERCP by the same endoscopist. Successful cannulation was achieved in 87.5%, without any complications being noted. Although a significant proportion of cases were Schutz 1 complexity, Billroth II anatomy was present in 17% of cases and minor papillary cannulation was required in 2%. Kumar et al[16] in 1995 and Choudari et al[15] in 2000 documented referral to a tertiary center for a second ERCP attempt in 113 and 562 patients, respectively. Over 50% of cases were Schutz grade 2-3 and represented a high degree of difficulty, including > 20% of cases requiring manometry. Both studies achieved 96% successful cannulation, although complications (mostly pancreatitis) occurred in 10%-11% of patients. Unlike the current study, the higher proportion of more complex cases in these last two retrospective studies reduces the ability to extrapolate the results to more general endoscopic practice. It is quite reasonably argued that Schutz grade 2 and 3 cases should not be attempted outside of high volume, expert tertiary centers. The rate of NKS in the cohort of referred patients (27.4%) was significantly higher than in the naïve papilla group, as well as appreciably higher than the aforementioned studies of repeat ERCP following previously failed cannulation[13-15] and other recent studies[17]. Our unit has recently shown that, in experienced hands, NKS is not a risk for PEP[17]. The use of NKS in a referred group of previous unsuccessful cannulations should be considered a necessary and vital part of the armamentarium of an experienced ERCP endoscopist.
Increasingly compelling data are emerging to confirm that, when the clinical entity or its treatment is complex or attended by high morbidity, then referral to experienced high-volume centers results in superior procedural and patient outcomes and reduced costs[18,19]. Similarly, ERCP procedures in high-volume centers have confirmed benefits including improved cannulation rates, lower complication rates and better patient outcomes[20,21]. Patients who have failed one attempt at cannulation in competent hands self select themselves as a group of “difficult cannulation” patients and are therefore best managed in an experienced tertiary center.
In the event of failed ERCP cannulation, studies indicate that 50%-60% of patients have further therapeutic procedures-radiological, surgical or repeat endoscopic management[22,23]. Percutaneous trans-hepatic cholangiography drainage and stenting is a common interventional radiological procedure utilized in the management of malignant obstructive jaundice, as well as in the treatment of operative bile leaks and benign biliary strictures[24,25].The technical and clinical success of a radiological approach has been reported to be > 90%, however, complications occur in 20%-30%, including cholangitis, bile leak, hemorrhage, post-procedural pain and stent/tube malfunction[26]. Protracted inpatient management is also usually necessary. The use of surgical management is of limited utility in non-malignant indications due to high morbidity (17%-37%) and high mortality (2%-5%)[27-29]. Recently, EUS-guided biliary drainage, either via rendezvous approach or direct puncture and stenting, has emerged as a viable therapeutic alternative[30,31]. This technique is used mainly in malignant obstructions, with technical and clinical success rates above 90% and 5%-15% complication rates. However, experience is currently limited to enthusiastic proponents of this technique and its durability is not well established.
The technical reasons for unsuccessful Schutz grade 1 biliary cannulation have not been previously documented. Although this study does not have an explanation for unsuccessful biliary cannulation in all cases (only 55% had an identifiable etiology), it does detail situations that intuitively may lead to more difficult cannulation, such as a long and mobile intraduodenal portion of the bile duct, periampullary diverticulum, an unstable position or a small papilla. Peripapillary diverticulum was cited as the cause of 14% of the unsuccessful biliary cannulations, despite two recent studies indicating no effect on cannulation rates[32,33].
The current study is limited by lack of randomization to an alternative therapeutic modality or a comparator group. Selection bias may also have been present because the referred patients were likely to have been considered more appropriate for a repeat ERCP attempt by the referrers than those not referred.
In conclusion, referral to an experienced high-volume center following an initial unsuccessful Schutz grade 1 biliary cannulation attempt is associated with high technical success and a favorable complication profile, compared to other routine naïve papilla ERCP procedures. We believe that a second ERCP procedure in a tertiary referral center should be the next management step following an unsuccessful biliary cannulation in this patient group. This type of clinical pathway should be part of the range of management options available to biliary endoscopists working outside high-volume tertiary centers.
Endoscopic retrograde cholangiopancreatography (ERCP) is an invaluable endoscopic technique in the management of gallstones and bile duct pathology. The technique is not always successful and it is unclear what the next management step should be following a failed attempt.
Knowledge in endoscopy continues to evolve on many fronts with an ever-expanding repertoire of indications and techniques. Evidence based justification is addressed with each new advance however more common dilemmas (such as what to do following a failed ERCP procedure) lack clear evidence. Repeat ERCP attempt has been evaluated in three previous studies, but all have involved a higher complexity than that what is seen in routine, everyday practice. Recent publications have addressed alternative therapeutic modalities but either lack widespread availability or inferior safety profiles.
This study demonstrated that in the setting of a low risk, uncomplicated patient a failed ERCP procedure can be successfully and safely managed by a repeat ERCP procedure via referral to a specialized, high volume endoscopy unit.
This type of clinical pathway following a failed ERCP attempt should be part of the range of management options available to biliary endoscopists working outside of high volume tertiary centres.
ERCP is an advanced endoscopic technique that is used to access and visualize the bile ducts and pancreas, as well as to perform therapeutic management in the setting of gallstones, malignancy and post surgical complications.
This paper deals with a clinical pathway in failed biliary cannulation. Results showed clear data about the high success rate of biliary cannulation in tertiary referral centre. Overall, the study clearly demonstrated a clinical pathway in failed biliary cannulation.
Peer reviewer: Kyu Taek Lee, MD, PhD, Professor, Department of Medicine Samsung Medical Center, Sungkyunkwan, University School of Medicine, No. 50, Irwon-dong, Gangnam-gu, Seoul 135-710, South Korea
S- Editor Sun H L- Editor Kerr C E- Editor Zhang DN
| 1. | Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson M, Williamson PJ. Are we meeting the standards set for endoscopy? Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007;56:821-829. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 177] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Petrini JL, Safdi MA. Quality indicators for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc. 2006;63:S29-S34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Schlup MM, Williams SM, Barbezat GO. ERCP: a review of technical competency and workload in a small unit. Gastrointest Endosc. 1997;46:48-52. [PubMed] [Cited in This Article: ] |
| 4. | Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1-10. [PubMed] [Cited in This Article: ] |
| 5. | Kaffes AJ, Bourke MJ, Ding S, Alrubaie A, Kwan V, Williams SJ. A prospective, randomized, placebo-controlled trial of transdermal glyceryl trinitrate in ERCP: effects on technical success and post-ERCP pancreatitis. Gastrointest Endosc. 2006;64:351-357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Laasch HU, Tringali A, Wilbraham L, Marriott A, England RE, Mutignani M, Perri V, Costamagna G, Martin DF. Comparison of standard and steerable catheters for bile duct cannulation in ERCP. Endoscopy. 2003;35:669-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 164] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Available from: http: //www.conjoint.org.au/information.html (accessed 3 February 2010). [Cited in This Article: ] |
| 9. | Swan MP, Bourke MJ, Alexander S, Williams SJ, Bailey AA, Hope R, Ruppin DC. A sequential cannulation protocol including early pancreatic stent placement and needle knife sphincterotomy: Interim analysis of a randomized trial. Gastrointest Endosc. 2009;69:AB139-AB140. [Cited in This Article: ] |
| 10. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] [Cited in This Article: ] |
| 11. | Johanson JF, Cooper G, Eisen GM, Freeman M, Goldstein JL, Jensen DM, Sahai A, Schmitt CM, Schoenfeld P. Quality assessment of ERCP. Endoscopic retrograde cholangiopacreatography. Gastrointest Endosc. 2002;56:165-169. [PubMed] [Cited in This Article: ] |
| 12. | Cheon YK, Cho KB, Watkins JL, McHenry L, Fogel EL, Sherman S, Lehman GA. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest Endosc. 2007;65:385-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 449] [Cited by in F6Publishing: 426] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 14. | Ramirez FC, Dennert B, Sanowski RA. Success of repeat ERCP by the same endoscopist. Gastrointest Endosc. 1999;49:58-61. [PubMed] [Cited in This Article: ] |
| 15. | Choudari CP, Sherman S, Fogel EL, Phillips S, Kochell A, Flueckiger J, Lehman GA. Success of ERCP at a referral center after a previously unsuccessful attempt. Gastrointest Endosc. 2000;52:478-483. [PubMed] [Cited in This Article: ] |
| 16. | Kumar S, Sherman S, Hawes RH, Lehman GA. Success and yield of second attempt ERCP. Gastrointest Endosc. 1995;41:445-447. [PubMed] [Cited in This Article: ] |
| 17. | Bailey AA, Bourke MJ, Kaffes AJ, Byth K, Lee EY, Williams SJ. Needle-knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis (with video). Gastrointest Endosc. 2010;71:266-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 18. | Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117-2127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2383] [Cited by in F6Publishing: 2367] [Article Influence: 112.7] [Reference Citation Analysis (0)] |
| 19. | Swan MP, Bourke MJ, Alexander S, Moss A, Williams SJ. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc. 2009;70:1128-1136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 155] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 20. | Varadarajulu S, Kilgore ML, Wilcox CM, Eloubeidi MA. Relationship among hospital ERCP volume, length of stay, and technical outcomes. Gastrointest Endosc. 2006;64:338-347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 118] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Aronson N, Flamm CR, Bohn RL, Mark DH, Speroff T. Evidence-based assessment: patient, procedure, or operator factors associated with ERCP complications. Gastrointest Endosc. 2002;56:S294-S302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Perdue DG, Freeman ML, ERCOST study group. Failed biliary ERCP: A prospective multicenter study of risk factors, complications and resource utilization. Gastrointest Endosc. 2004;59:T1479. [Cited in This Article: ] |
| 23. | Kevans D, Zeb F, Donnellan F, Courtney G, Aftab AR. Failed biliary access following needle knife fistulotomy: is repeat interval ERCP worthwhile? Scand J Gastroenterol. 2010;45:1238-1241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Born P, Rösch T, Triptrap A, Frimberger E, Allescher HD, Ott R, Weigert N, Lorenz R, Classen M. Long-term results of percutaneous transhepatic biliary drainage for benign and malignant bile duct strictures. Scand J Gastroenterol. 1998;33:544-549. [PubMed] [Cited in This Article: ] |
| 25. | Kim ES, Lee BJ, Won JY, Choi JY, Lee DK. Percutaneous transhepatic biliary drainage may serve as a successful rescue procedure in failed cases of endoscopic therapy for a post-living donor liver transplantation biliary stricture. Gastrointest Endosc. 2009;69:38-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 26. | van Delden OM, Laméris JS. Percutaneous drainage and stenting for palliation of malignant bile duct obstruction. Eur Radiol. 2008;18:448-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 128] [Cited by in F6Publishing: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 27. | Shimizu Y, Kimura F, Shimizu H, Yoshidome H, Ohtsuka M, Miyazaki M. The morbidity, mortality, and prognostic factors for ampullary carcinoma and distal cholangiocarcinoma. Hepatogastroenterology. 2008;55:699-703. [PubMed] [Cited in This Article: ] |
| 28. | Michelassi F, Erroi F, Dawson PJ, Pietrabissa A, Noda S, Handcock M, Block GE. Experience with 647 consecutive tumors of the duodenum, ampulla, head of the pancreas, and distal common bile duct. Ann Surg. 1989;210:544-554; discussion 554-556. [PubMed] [Cited in This Article: ] |
| 29. | van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van der Harst E, Kubben FJ, Gerritsen JJ, Greve JW, Gerhards MF, de Hingh IH. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med. 2010;362:129-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 717] [Cited by in F6Publishing: 638] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 30. | Kahaleh M, Hernandez AJ, Tokar J, Adams RB, Shami VM, Yeaton P. Interventional EUS-guided cholangiography: evaluation of a technique in evolution. Gastrointest Endosc. 2006;64:52-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 193] [Cited by in F6Publishing: 216] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 31. | Yamao K. EUS-guided choledochoduodenostomy. Gastrointest Endosc. 2009;69:S194-S199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Panteris V, Vezakis A, Filippou G, Filippou D, Karamanolis D, Rizos S. Influence of juxtapapillary diverticula on the success or difficulty of cannulation and complication rate. Gastrointest Endosc. 2008;68:903-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Tyagi P, Sharma P, Sharma BC, Puri AS. Periampullary diverticula and technical success of endoscopic retrograde cholangiopancreatography. Surg Endosc. 2009;23:1342-1345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |