CASE REPORT
A 83-year-old woman was admitted to our hospital because of intermittent abdominal colicky pain and vomiting for 26 h. The pain localized over the periumbilical area with radiation along the medial side of the thigh. The patient had had several episodes of similar syndrome during the past 13 mo, but it relieved spontaneously or by treatment with intravenous fluids and nasogastric suction. A diagnosis of intestinal obstruction was made 7 mo prior to current admission. But the cause of disease was unclear. She had a similar attack 5 mo earlier, was suspected of having incarcerated hernia by ultrasonography. A loop of small bowel at the left groin region was noted (Figure 1). But subsequent investigations and treatment were refused after the relief of pain. She also had a history of chronic constipation, ischemic heart disease and chronic bronchitis. She had no previous abdominal surgery. On her arrival, the body temperature was 36.8°C, blood pressure was 105/75 mmHg, heart rate was 92 beats per minute. Her body mass index was 18 (body weight 39 kg, height 147 cm). Physical examination revealed an emaciated lady with a soft but distended abdomen, visible bowel coils, mild tenderness over the lower abdomen, and hyperactive bowel sounds. No mass or rebound pain of the abdomen was noted. There was no palpable hernia in the groin. No abnormal signs were found on rectal and vaginal examinations. The Howship-Romberg sign, which characterized by pain or paresthesia in the hip with radiation down the medial thigh to the knee on the affected side, was positive. The white blood cell count was 11.2 × 109/L and other serum analyses were within normal limits. The initial plain abdominal radiography showed dilated loops of small bowel (Figure 2). Computed tomography (CT) scan demonstrated an abrupt stenosis at the terminal ileum in addition to the dilation of small bowel (Figure 3A). A low-density mass was also noted between the pectineus and the left external obturator muscles (Figure 3B). Three-dimensional reconstructed CT revealed a loop of small bowel protruding into the left obturator canal. The stenosis of the lumen and distended small bowel loops in the abdomen were well visualized (Figure 4). Incarcerated obturator hernia was diagnosed and emergency laparotomy was arranged immediately. Unfortunately, her family refused surgery because of her worsening condition, general weakness and the high risk involved. The patient was managed conservatively with intravenous fluids and nasogastric suction. On the third evening after admission, her abdominal pain suddenly became worse and constant. Subsequently, she developed restlessness and more unbearable generalized abdominal pain. On examination, the body temperature was 37.7°C, the blood pressure was 75/55 mmHg, and the heart rate was 128 beats per minute. There were obvious signs of peritonism and bowel sounds were absent. The diagnosis of perforation of small bowel and septic shock was made. The patient underwent emergency surgery after explanation to her guardian. Laparotomy revealed a loop of the terminal ileum about 80 cm from the ileocecal valve, herniating into the left obturator canal (Figure 5A). Perforation of small bowel was noted proximal to the port of incarceration (Figure 5B). The peritoneal contamination was severe. In view of the patient’s poor conditions, we resected the perforated ileal segment and performed an end-ileostomy with closure of the distal loop. The defect at the hernia site was 1.5 cm in diameter and was closed with a few interrupted non-absorbable sutures (Figure 5C). The operating time was 75 min. Postoperatively, the patient was complicated with MODS and received subsequent treatment in intensive care unit. She recovered well and discharged 21 d after surgery. The second operation for re-established intestinal continuity was suggested 3 mo after operation. But the patient declined and now she is still uncertain about it. No recurrence of the hernia was noted during the 5 mo follow-up.
Figure 1 Ultrasonographic image of the left groin demonstrating a fluid-filled loop of bowel with the neck of the hernia uncertainly identified (arrow).
Figure 2 Plain abdominal film revealing multiple dilated loops of small bowel in an emaciated woman with scoliosis.
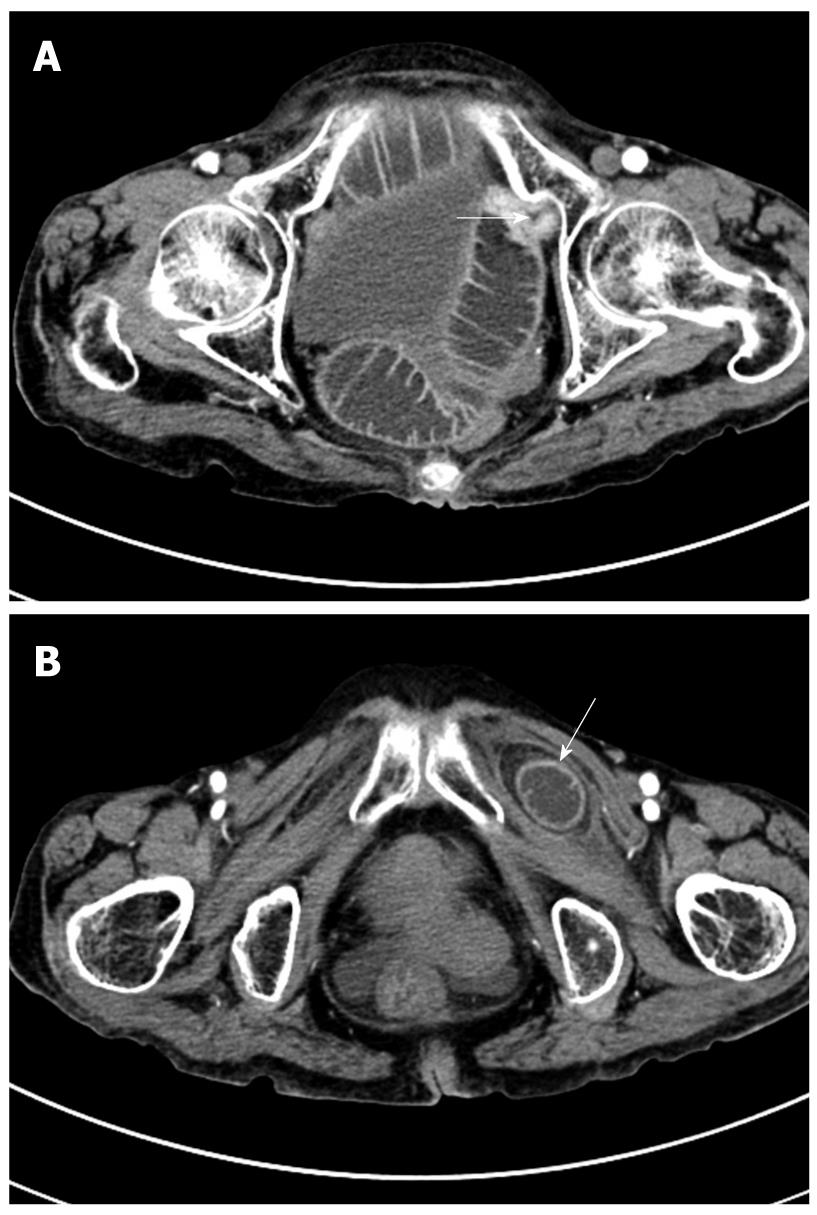
Figure 3 Abdominal axial CT image.
A: Severe dilated small bowel and abrupt stenosis at the terminal ileum in the pelvic cavity (arrow); B: A low-density mass with clear border located between the pectineus and the left external obturator muscles (arrow).
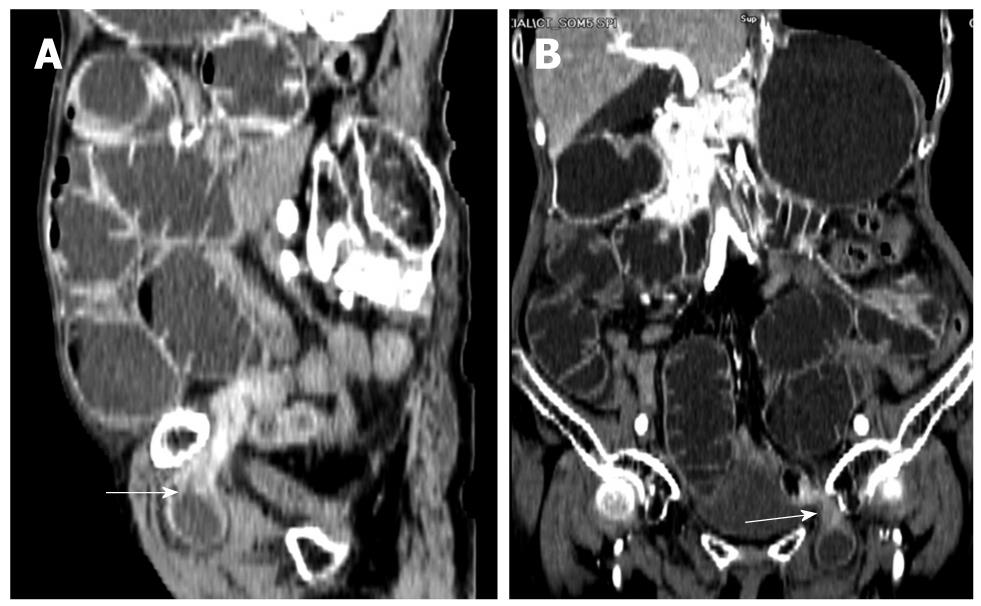
Figure 4 Three-dimensioned reconstructed CT (A: Sagittal section; B: Coronal section) finding extensive dilation of the small bowel loops and a loop of small bowel protruding into the left obturator canal with the transition zone from dilated to collapsed bowel (arrows).
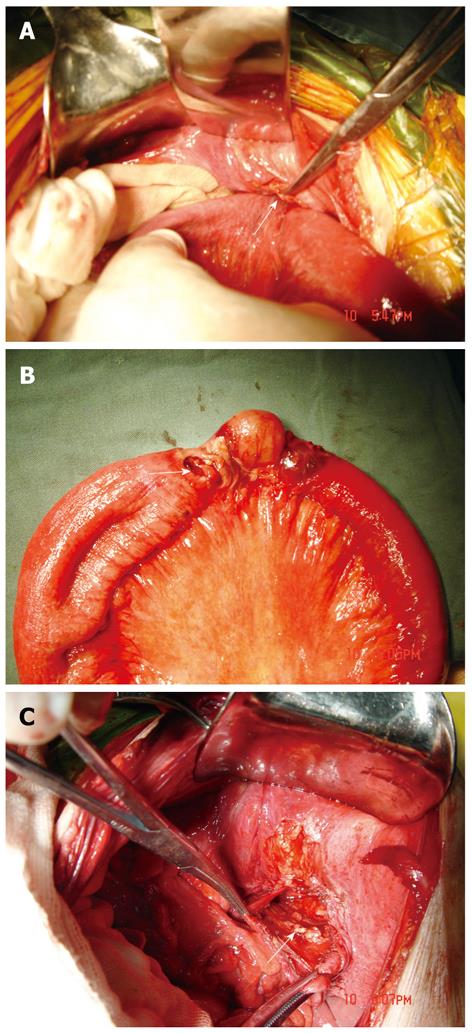
Figure 5 Intraoperative photography illustrating.
A: Incarcerated small bowel at left obturator foramen (arrow); B: Perforation of ileum proximal to the site of incarceration (arrow); C: A defect in the left obturator canal (arrow).
DISCUSSION
An obturator hernia is a herniated viscera through the peritoneal defect that is bounded superiorly by the pubic ramus and inferiorly by the free edge of the obturator membrane[2]. The incidence was approximately nine times higher in women than in men due to the wider pelvis and relatively greater diameter of the obturator foramen in females[3]. Recent published series show nearly exclusive incidence in women[4-7]. It occurs most commonly in emaciated elderly women between 70 and 90 years of age. The loss of protective preperitoneal fat from aging or malnutrition makes a larger space in the obturator canal and facilitates the formation of a hernia[8,9]. Thus, it is not surprising that most of the patients are markedly underweight. The majority of obturator hernias occur on the right side probably because the sigmoid colon may cover the left obturator foramen and prevents herniation[10]. About 6% of cases are bilateral and some may be associated with other types of hernia, such as the indirect inguinal hernia, the direct inguinal hernia, or the femoral hernia[11]. It is uncertain if concomitant conditions that lead to constant and increased intra-abdominal pressure such as constipation, ascites, chronic obstructive pulmonary disease, kyphoscoliosis, or multiparity are risk factors for obturator hernia. Our case presented most of these predisposing factors, including old age, emaciation, constipation and chronic bronchitis.
There are three anatomic stages in the development of obturator hernia[8]. Stage one: preperitoneal connective tissue and fat enter the pelvic orifice of the obturator canal. Stage two begins with a peritoneal dimple through the canal and progresses to the formation of a peritoneal sac. Stage three is characterized by clinically significant symptoms produced by the entrance of an organ, usually the ileum, sometimes the omentum or part of the bladder, into the sac. Rarely, it was reported that ovary or Meckel’s diverticulum can also be incarcerated[12,13]. Our case appeared obviously to be in the third stage of development at the time of admission because of the presence of intestinal obstruction.
The most common presentation of obturator hernia is mechanical small bowel obstruction caused by incarceration of the bowel into the obtutator canal. The symptoms may be acute or intermittent if the hernia content reduces into the peritoneal cavity spontaneously. In some cases, the initial symptoms are mild nausea, vomiting and anorexia, probably due to incomplete herniation or Richter’s type. Obturator neuralgia is also an important complaint that extends from the inguinal crease to the anteromedial aspect of the thigh. The Howship-Romberg sign is reported to be present in nearly 50% of cases which refers to pain along the medial thigh and sometimes in the hip caused by compression of the obturator nerve by the hernia sac[10,12]. Flexion of the thigh usually relieves the pain. Extension, abduction, or medial rotation of the hip may exacerbate the pain. The clinical diagnosis is often difficult to make when this sign is absent. However, the Howship-Romberg sign was generally masked by the severe abdominal symptoms, and it was always neglected before operation. Another possible sign on presentation is the Hannington-Kiff sign[14]. It is characterized by an absent adductor reflex in the thigh, resulting from obturator nerve compression. The obturator canal is easily identified by digital vaginal examination at either 2 o’clock or 10 o’clock position. Palpation of a tender mass in the obturator region is of great value in obtaining the correct diagnosis. However, it is evident in only a few cases because the incarcerated mass is usually small and deeply situated.
Various imaging modalities have been applied to establish accurate preoperative diagnosis of this rare disease, including plain abdominal radiography, herniography, ultrasonography, CT, and gastrointestinal imaging with contrast medium. Plain radiography provides no specific findings apart from a dilated bowel loop, and can not reveal any significant information as to the cause of intestinal obstruction[15]. It is almost unuseful in diagnosing obturator hernia. Herniography can directly demonstrate the hernial sac, but has no place in the emergency diagnosis of obturator hernia and is used only in elective cases. Ultrasonography has been considered as a reliable modality with the presence of a hypoechoic tubular structure or a cystic lesion in the region of obturator canal. However, it is not easily identified due to the deep location within the pelvic musculature and smaller hernia sac[1]. In 1983, CT was first reported to be useful for detecting obturator hernia by Cubillo, and now is regarded as the standard diagnostic modality for obturator hernia with a documented accuracy of 80%[10,16]. CT images may demonstrate an air-filled or fluid-filled bowel loop in the region of the obturator foramen. In a study of a series of patients, Kammori et al[10] reported that 15 of 16 patients who were confirmed to have obturator hernia were diagnosed by CT alone. With the advent of multi-slice helical CT scan and the three-dimensional reconstruction technique, the accurate images are of great help in identifying obturator hernia and understanding the relationship between obturator canal and small bowel, as was seen in our study. In our case, the history taking, clinical manifestation and Howship-Romberg sign only gave the suspicion of obturator hernia. The definitive diagnosis was made by CT images.
There is a general agreement that obturator hernia must be treated surgically. A variety of operative approaches to obturator hernias have been described including retropubic approach, obturator approach, inguinal extraperitoneal approach, transperitoneal approach and combined approach with either a laparotomy or laparoscopy[3,17-19]. However, because of the rarity of this condition, there is no consensus on the most proper approach. In patients with an established preoperative diagnosis, an extraperitoneal approach is the best surgical procedure. However, a transperitoneal approach will be necessary in those patients with intestinal obstruction of uncertain cause. We prefer transperitoneal approach because it can obtain adequate exposure, avoid vessel damage, facilitate the reduction of the incarcerated bowel, identify and allow resection of the strangulated bowel when necessary, and easy repair of the defect as well. It should be emphasized that careful dissection of the hernia sac is essential to avoid injury of the obturator nerve or vessels, and the contralateral side must be routinely explored because of the chance of underlying hernia[18]. Recently, with the advantage of minimal invasion, laparoscopic technique has been applied in management of obturator hernia. This mini-invasive method may provide some benefits for these high-risk patients, such as less postoperative pain, fewer complications, earlier ambulatory and shorter hospital stay[17]. However, experience with laparoscopy is largely based on isolated case report. The laparoscopic operation for obturator hernia is infeasible in an emergency and is still limited to be performed widely due to the technical problems[20]. As in other hernias, after reduction of the contents, the defect of obturator canal should be repaired. Methods of repair vary from a simple suture or using autogenous adjacent tissue like broad ligament, ovary or uterus to permanent prosthetic mesh[21,22]. But the use of mesh is not advised in the presence of peritonitis or bowel resection because of the potential risk of infection.
Early surgical intervention is essential to the appropriate treatment of obturator hernia. However, surgeons are often reluctant to operate and family members always hesitate in proceeding with clinical management because of the age, the concomitant disease and the general condition of the patient. Conservative medical treatments were attempted in hopes that the obstruction would be reduced, which undoubtedly result in delayed surgical intervention and increased the morbidity and mortality rates. In our study, the duration from onset of symptoms to surgery was 3.7 d. Here we felt deeply regret that the delayed operation led to the gut resection with ileostomy and severe complications. Fortunately, the patient recovered well.
In conclusion, obturator hernia is relatively rare and is a significant cause of intestinal obstruction, particularly in emaciated elderly women without a history of abdominal surgery. It is important that physicians consider obturator hernia in mind when making a diagnosis in patients with small bowel obstruction. For the diagnosis of obturator hernia, the intermittent attacks of intestinal obstruction, a positive Howship-Romberg sign, a palpable tender mass in the groin area by digital vaginal examination are helpful. Abdominal CT is useful for viewing a loop of small bowel herniated into the obturator canal. The point of early surgical intervention is highlighted because it is the only hope to lower the high morbidity and mortality associated with this condition.