Published online Feb 28, 2009. doi: 10.3748/wjg.15.990
Revised: December 25, 2008
Accepted: December 31, 2008
Published online: February 28, 2009
AIM: To clarify whether there is any difference in the symptom relief in patients with reflux esophagitis following the administration of four Proton pump inhibitors (PPIs).
METHODS: Two hundred and seventy-four patients with erosive reflux esophagitis were randomized to receive 8 wk of 20 mg omeprazole (n = 68), 30 mg of lansoprazole (n = 69), 40 mg of pantoprazole (n = 69), 40 mg of esomeprazole (n = 68) once a day in the morning. Daily changes in heartburn and acid reflux symptoms in the first 7 d of administration were assessed using a six-point scale (0: none; 1: mild; 2: mild-moderate; 3: moderate; 4: moderate-severe; 5: severe).
RESULTS: The mean heartburn score in patients treated with esomeprazole more rapidly decreased than those receiving other PPI. Complete resolution of heartburn was also more rapid in patients treated with esomeprazole for 5 d compared with omeprazole (P = 0.0018, P = 0.0098, P = 0.0027, P = 0.0137, P = 0.0069, respectively), lansoprazole (P = 0.0020, P = 0.0046, P = 0.0037, P = 0.0016, P = 0.0076, respectively), and pantoprazole (P = 0.0006, P = 0.0005, P = 0.0009, P = 0.0031, P = 0.0119, respectively). There were no significant differences between the four groups in the rate of endoscopic healing of reflux esophagitis at week 8.
CONCLUSION: Esomeprazole may be more effective than omeprazole, lansoprazole, and pantoprazole for the rapid relief of heartburn symptoms and acid reflux symptoms in patients with reflux esophagitis.
- Citation: Zheng RN. Comparative study of omeprazole, lansoprazole, pantoprazole and esomeprazole for symptom relief in patients with reflux esophagitis. World J Gastroenterol 2009; 15(8): 990-995
- URL: https://www.wjgnet.com/1007-9327/full/v15/i8/990.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.990
Gastroesophageal reflux disease (GERD) is a common disorder with a high incidence rate of 10%-38% in the Western population occurring at least once a week[12]. The prevalence of GERD has been increasing[3].
The severity of GERD is directly correlated with the degree and duration of esophageal acid exposure and is highly pH dependent[4–6]. Chronic exposure is associated with serious complications including esophageal stricture in 4%-20% of patients[4] and Barrett’s esophagus in up to 15% of patients with GERD[4–7].
Healing of reflux esophagitis is directly correlated with the intragastric pH > 4.0[89]. The efficacy of antisecretory drugs in healing reflux esophagitis depends on the strength and duration of acid suppression within a 24 h period, and the duration of the treatment[10]. Proton pump inhibitor (PPI) therapy is effective for acid-related symptoms. A number of investigators have reported that earlier symptom relief and higher endoscopic healing rates have been obtained with PPI in comparison with H2-receptor antagonists (H2-RAs)[1112]. The time period required to obtain maximal inhibition of gastric acid secretion is, however, reported to differ between PPI[13–17]. The time taken for the resolution of symptoms in patients with reflux esophagitis is, therefore, unlikely to be uniform in all PPI. As the quality of life (QOL) of patients with reflux esophagitis is decreased by heartburn symptoms[1819], quick symptom relief is important to normalize their QOL. It has not hitherto been fully determined whether differences in the onset of anti-secretary activity may affect the speed of symptom relief with different PPI. In this study, we investigated the differences in symptom relief in the first 7 d of administration of omeprazole, lansoprazole, pantoprazole, and esomeprazole in patients with reflux esophagitis.
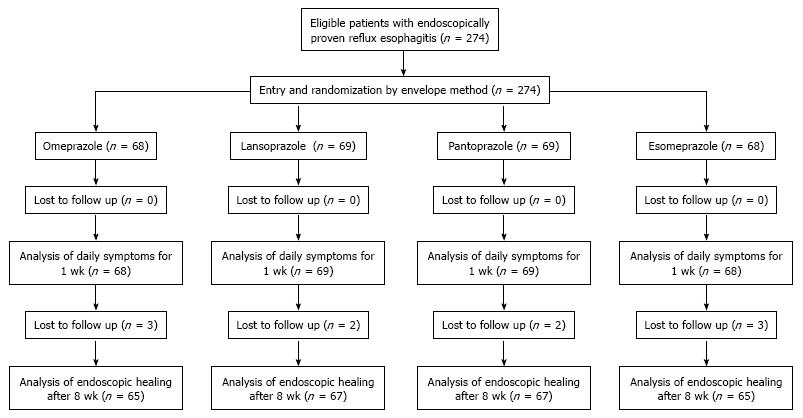
Two hundred and seventy-four patients with endoscopically proven reflux esophagitis in the Affiliated Hospital of Yanbian University from January, 2006 to September, 2007 and the Affiliated Hospital of Hainan Medical College from October, 2007 to November, 2008 were included in the study. Ten of the patients were lost to follow-up, who refused endoscopic examination after administration of PPI. Subjects with active peptic ulcer, upper gastrointestinal cancers, malignant diseases of other organs, severe cardiac, hepatic, or renal diseases, anemia (hemoglobin concentration < 10 g/dL), or who were pregnant and/or lactating, were excluded. After written informed consent for enrollment in this study was obtained, one of four PPI (omeprazole, lansoprazole, pantoprazole, or esomeprazole, which were contained in sealed envelopes) was administrated for 8 wk (Figure 1). The sealed envelopes containing one of four PPI were randomly assigned for administration. Each PPI was administered once in the morning, 20 mg omeprazole, 40 mg pantoprazole, 30 mg lansoprazole, and 40 mg esomeprazole. Subjects were not permitted to take H2-RAs or prokinetic drugs during the study period. There were 135 men and 139 women (mean age 57.8 ± 13.5 years, range 36-85 years).
All endoscopic examinations were performed by one endoscopist, using a high-resolution upper gastrointestinal endoscope (GIF 260 series; Olympus, Tokyo, Japan) before and 8 wk after the administration of PPI. Endoscopic diagnosis and the grading of reflux esophagitis were based on the Los Angeles (LA) classification[20]. Helicobacter pylori (H pylori) infection status was also tested by measuring serum anti-H pylori immunoglobulin IgG antibodies, using an ELISA test (Institute of Immunology, Tokyo, Japan).
All patients were asked to keep a symptom diary, in which they recorded the severity of symptoms (heartburn and acid reflux) prior to and during the first 7 d of PPI administration. The severity of symptoms was graded on a six-point scale (0: none; 1: mild; 2: mild-moderate; 3: moderate; 4: moderate-severe; 5: severe and/or intolerable) and was recorded daily. Mild symptoms were defined as a heartburn/acid reflux that did not disturb the normal daily activity of the patients. Moderate symptoms were defined as those that bothered the daily activity, while the patients continued to work productively. Severe symptoms were defined as high-grade symptoms that stopped the daily productive activity of the patients. The patients were instructed to record the severity of their symptoms as a whole previous day’s score in the following morning. The daily changes in the severity of two symptoms (heartburn and acid reflux) were separately analyzed. The primary endpoint of the present study was to clarify whether rapid symptom relief in the first week of drug administration differed between the four kinds of PPI.
Statistical analysis of inter-group data was performed using the Microsoft Office Excel F-test. The Microsoft Office Excel F-test was also used to compare the complete disappearance of symptoms between the groups. In addition, sex, age, H pylori status and grading of endoscopic esophagitis were analyzed by χ2 test.
There were no significant differences between the groups in sex, age, H pylori status, the grade of reflux esophagitis, and the proportion of cases with heartburn and acid reflux symptoms before the administration of the drugs (Table 1).
| Omeprazole (n = 68) | Lansoprazole (n = 69) | pantoprazole (n = 69) | Esomeprazole (n = 68) | Statistical difference | |
| Sex (male/female) | 33/35 | 35/34 | 34/35 | 33/35 | NS |
| Age (mean ± SD) (yr) | 57.9 ± 14.1 | 58.1 ± 13.0 | 57.8 ± 13.2 | 57.4 ± 12.8 | NS |
| H pylori (positive/negative) Endoscopic esophagitis (Los Angeles classification) | 29/39 | 31/38 | 30/39 | 29/39 | NS |
| A | 20 | 20 | 20 | 20 | NS |
| B | 26 | 26 | 28 | 26 | NS |
| C | 20 | 21 | 20 | 20 | NS |
| D | 2 | 2 | 1 | 2 | NS |
| Symptoms | |||||
| Heartburn (%) | 61 (89.7) | 63 (91.3) | 62 (89.9) | 63 (92.6) | NS |
| Acid reflux (%) | 33 (48.5) | 35 (50.7) | 34 (49.3) | 35 (51.5) | NS |
| No symptom (%) | 8 (11.8) | 5 (7.2) | 8 (11.5) | 5 (7.4) | NS |
No severe side effects related to PPI administration were reported in subjects participating in the present study. None of the patients needed to take antacids for the relief of symptoms after PPI administration.
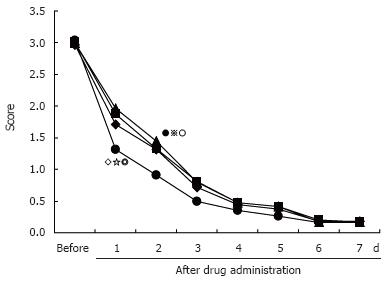
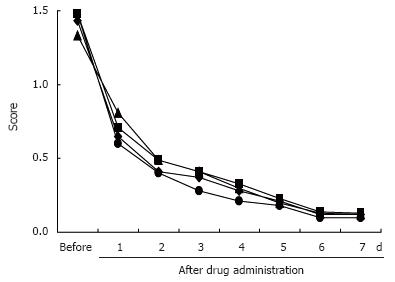
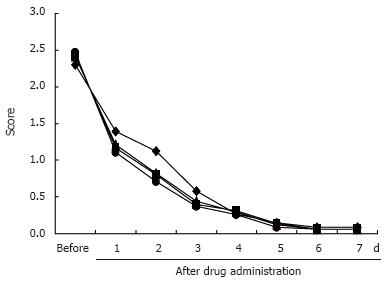
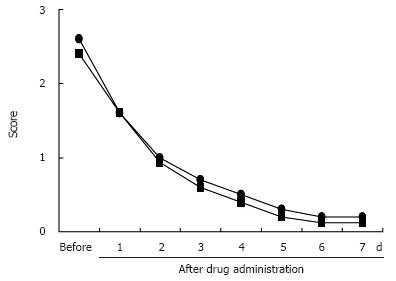
Figure 2 and Figure 3 show the daily changes in the mean symptom scores of heartburn and acid reflux in all patients with each PPI. Although there were no differences between the groups in the heartburn score before PPI administration, the heartburn score was significantly lower in subjects administered esomeprazloe after the first and second days than in those administered omeprazole (P = 0.0031, P = 0.0092), lansoprazole (P = 0.0039, P = 0.0088), and pantoprazole (P = 0.0009, P = 0.0036), respectively. This difference between subjects administered esomeprazole and the other PPI tended to disappear after 5 d of administration of the test drugs. No significant differences in acid reflux scores were seen between the groups (Figure 3).
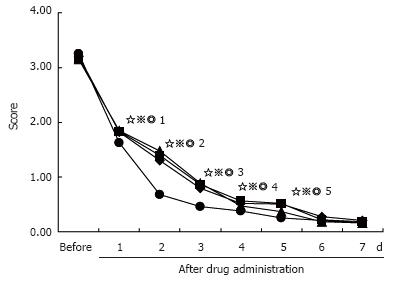
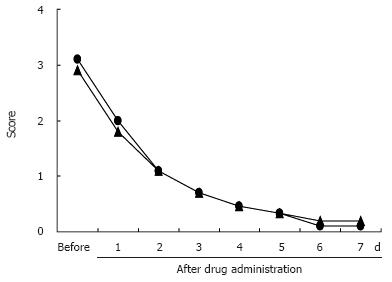
When the analysis was limited to only the patients who initially reported heartburn and acid reflux, the heartburn score of those subjects administered esomeprazole decreased more quickly than those administered omeprazole, lansoprazole, and pantoprazole (Figure 4). This difference also tended to disappear after 5 d of administration of the test drugs. Complete disappearance of heartburn symptoms after administration of the test drugs from 1 d to 5 d occurred more rapidly in subjects administered esomeprazole than in those administered omeprazole (P = 0.0018, P = 0.0098, P = 0.0027, P = 0.0137, P = 0.0069, respectively), pantoprazole (P = 0.0006, P = 0.0005, P = 0.0009, P = 0.0031, P = 0.0119, respectively), and lansoprazole (P = 0.0020, P = 0.0046, P = 0.0037, P = 0.0016, P = 0.0076, respectively). No significant differences in acid reflux scores were seen between the groups (Figure 5).
Ten of the 274 subjects enrolled in the present study refused endoscopic examination after administration of PPI, so upper gastrointestinal endoscopy was performed in 264 patients at week 8 after the commencement of drugs. These patients had taken all of the PPI. The endoscopic healing rates for reflux esophagitis in subjects administered omeprazole, lansoprazole, pantoprazole and esomeprazole were 87.7%, 89.6%, 91.1% and 95.4%, respectively. Although the healing rate in subjects administered esomeprazole tended to be higher than in those administered omeprazole, lansoprazole and pantoprazole, the differences did not reach statistically significant levels.
When the patients were divided into H pylori positive and negative groups, the healing rate for reflux esophagitis at week 8 in H pylori positive patients tended to be higher than that in negative subjects (92.4% vs 85.8%, P > 0.05, χ2 =2.95, by χ2 test).
The daily changes in heartburn score during the first week of administration of the test drugs did not differ between H pylori-positive and H pylori-negative patients by F-test (Figure 6). There was no significant difference in the complete disappearance of heartburn between H pylori-positive and H pylori-negative patients (Figure 7).
The daily changes in the acid reflux score during the first week of administration of the test drugs also did not differ between H pylori-positive and H pylori-negative patients (data not shown).
Gastroesophageal reflux disease (GERD) is caused by acid reflux, which can be treated by suppressing gastric acid secretion[2122]. The efficacy of antisecretory drugs in healing reflux esophagitis depends on the potency of acid suppression[12], and PPIs are considered to be the most effective drugs for reflux esophagitis[23]. The symptoms of reflux esophagitis, such as heartburn, have been demonstrated to markedly impair QOL in these patients[1819]. Complete and rapid relief of symptoms is, therefore, of critical importance in the treatment of patients with reflux disease.
In the present study, we compared with efficacy of omeprazole, pantoprazole, lansoprazole, pantoprazole and esomeprazole for symptom relief in the first 7 d of treatment for reflux esophagitis. The administration of esomeprazole was most effective for symptom relief within 2 d compared with omeprazole, pantoprazole, lansoprazole and pantoprazole administration, this difference disappeared 5 d after commencement of drug administration. The results of present study are consistent with those of the study by Rohss et al[24–26] and Miner P Jr et al[27], who reported that esomeprazole 40 mg daily was more effective than omeprazole 20 mg daily, lansoprazole 30 mg, pantoprazole 40 mg daily in the relief of heartburn symptoms during the first day and the first 5 d after the commencement of administration.
In the present study, we demonstrated that esome-prazole gave faster symptom relief than pantoprazole, pantoprazole, lansoprazole and omeprazole. Because esomeprazole has been shown to have a faster onset of antisecretory activity than omeprazole, lansoprazole and pantoprazole[2427], esomeprazole rapidly increased the detectable intragastric pH > 4 on the first treatment day[26], and the first 5 d after commencement of administration of esomeprazole, and the intragastric pH > 4 maintained for a longer period of time than lansoprazole, pantoprazole and omeprazole[2527].
Although the symptom relief was faster by administration of esomeprazole than by omeprazole, pantoprazole or lansoprazole, the four kinds of PPI investigated in the present study were demonstrated to be effective for symptom relief within 1 wk in patients with endoscopically proven esophagitis. Recently, PPI has been also used for the diagnosis of gastroesophageal reflux, not only in the patients with non-erosive reflux disease (NERD)[2829], but also in patients with atypical gastroesophageal reflux symptoms[3031]. The present study suggests that the four kinds of PPI are effective for the diagnosis of the existence of gastroesophageal acid reflux, and it may be worthwhile investigating whether esomeprazole can shorten the time period necessary for diagnosis.
The healing rate of reflux esophagitis after 8 wk of treatment tended to be higher in patients administered esomeprazole than in those administered omeprazole, lansoprazole or pantoprazole, although these differences did not reach a statistically significant level. However, these differences need to be confirmed by further large comparative studies, which may have been caused by variations in the proportion of H pylori positive patients between the four PPI regimen groups, because H pylori infection has been reported to influence the healing of reflux esophagitis by PPI[32]. The degree of symptom relief was not, however, different during the first week of administration of PPI between H pylori positive and negative patients. The symptomatic response to PPI treatment during the first week administration should not, therefore, be affected by H pylori status.
There were several limitations in the comparison of the speed of symptom relief between the four PPIs in the present study since the study subjects were relatively small in number, and some patients with endoscopically proven reflux esophagitis, but without any reflux symptoms were included in the study.
In conclusion, the present study found that esomeprazole 40 mg daily may be more effective than either omeprazole 20 mg daily, pantoprazole 40 mg daily or lansoprazole 30 mg daily for the rapid relief of heartburn symptoms in patients with endoscopically proven reflux esophagitis. Symptom relief after several days of treatment and reflux esophagitis healing rates after 8 wk of treatment, were not different between patients treated with omeprazole, pantoprazole, lansoprazole, or esomeprazole.
In patients with gastroesophageal reflux disease (GERD), esomeprazole has demonstrated pharmacological and clinical benefits beyond those seen with the other proton pump inhibitors (PPIs ). The efficacy of omeprazole, pantoprazole, lansoprazole, pantoprazole and esomeprazole for symptom relief in the first 7 d of treatment for reflux esophagitis was compared with endoscopic healing rates for reflux esophagitis after 8 wk of treatment.
Although many investigators have reported that esomeprazole can more rapidly increase detectable intragastric pH > 4 on the first treatment day, and the first 5 d than the other PPIs, symptom relief after administration of the lansoprazole, pantoprazole, omeprazole and esomeprazole has not been investigated. This paper showed for the first time that symptom relieved in patients with GERD after administration of the lansoprazole, pantoprazole, omeprazole and esomeprazole. Esomeprazole more rapidly relieved heartburn after administration of the test drugs than the other PPIs.
This is a report designed to analyze a symptom relief for GERD subjects based on presenting symptoms and endoscopic healing rate for reflux esophagitis in China. This clinical study was well designed and the manuscript is well written.
| 1. | Kennedy T, Jones R. The prevalence of gastro-oesophageal reflux symptoms in a UK population and the consultation behaviour of patients with these symptoms. Aliment Pharmacol Ther. 2000;14:1589-1594. [Cited in This Article: ] |
| 2. | Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448-1456. [Cited in This Article: ] |
| 3. | Shaw MJ, Talley NJ, Beebe TJ, Rockwood T, Carlsson R, Adlis S, Fendrick AM, Jones R, Dent J, Bytzer P. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:52-57. [Cited in This Article: ] |
| 4. | Spechler SJ. Epidemiology and natural history of gastro-oesophageal reflux disease. Digestion. 1992;51 Suppl 1:24-29. [Cited in This Article: ] |
| 5. | Orlando RC. The pathogenesis of gastroesophageal reflux disease: the relationship between epithelial defense, dysmotility, and acid exposure. Am J Gastroenterol. 1997;92:3S-5S; discussion 5S-7S. [Cited in This Article: ] |
| 6. | Johnston BT, Collins JS, McFarland RJ, Love AH. Are esophageal symptoms reflux-related? A study of different scoring systems in a cohort of patients with heartburn. Am J Gastroenterol. 1994;89:497-502. [Cited in This Article: ] |
| 7. | Winters C Jr, Spurling TJ, Chobanian SJ, Curtis DJ, Esposito RL, Hacker JF 3rd, Johnson DA, Cruess DF, Cotelingam JD, Gurney MS. Barrett's esophagus. A prevalent, occult complication of gastroesophageal reflux disease. Gastroenterology. 1987;92:118-124. [Cited in This Article: ] |
| 8. | Holloway RH, Dent J, Narielvala F, Mackinnon AM. Relation between oesophageal acid exposure and healing of oesophagitis with omeprazole in patients with severe reflux oesophagitis. Gut. 1996;38:649-654. [Cited in This Article: ] |
| 9. | Johansson KE, Ask P, Boeryd B, Fransson SG, Tibbling L. Oesophagitis, signs of reflux, and gastric acid secretion in patients with symptoms of gastro-oesophageal reflux disease. Scand J Gastroenterol. 1986;21:837-847. [Cited in This Article: ] |
| 10. | Bell NJ, Hunt RH. Role of gastric acid suppression in the treatment of gastro-oesophageal reflux disease. Gut. 1992;33:118-124. [Cited in This Article: ] |
| 11. | Jansen JB, Van Oene JC. Standard-dose lansoprazole is more effective than high-dose ranitidine in achieving endoscopic healing and symptom relief in patients with moderately severe reflux oesophagitis. The Dutch Lansoprazole Study Group. Aliment Pharmacol Ther. 1999;13:1611-1620. [Cited in This Article: ] |
| 12. | Kawano S, Murata H, Tsuji S, Kubo M, Tatsuta M, Iishi H, Kanda T, Sato T, Yoshihara H, Masuda E. Randomized comparative study of omeprazole and famotidine in reflux esophagitis. J Gastroenterol Hepatol. 2002;17:955-959. [Cited in This Article: ] |
| 13. | Besancon M, Simon A, Sachs G, Shin JM. Sites of reaction of the gastric H,K-ATPase with extracytoplasmic thiol reagents. J Biol Chem. 1997;272:22438-22446. [Cited in This Article: ] |
| 14. | Williams MP, Sercombe J, Hamilton MI, Pounder RE. A placebo-controlled trial to assess the effects of 8 days of dosing with rabeprazole versus omeprazole on 24-h intragastric acidity and plasma gastrin concentrations in young healthy male subjects. Aliment Pharmacol Ther. 1998;12:1079-1089. [Cited in This Article: ] |
| 15. | Williams MP, Pounder RE. Review article: the pharmacology of rabeprazole. Aliment Pharmacol Ther. 1999;13 Suppl 3:3-10. [Cited in This Article: ] |
| 16. | Gardner JD, Perdomo C, Sloan S, Hahne WF, Barth JA, Rodriguez-Stanley S, Robinson M. Integrated acidity and rabeprazole pharmacology. Aliment Pharmacol Ther. 2002;16:455-464. [Cited in This Article: ] |
| 17. | Saitoh T, Fukushima Y, Otsuka H, Hirakawa J, Mori H, Asano T, Ishikawa T, Katsube T, Ogawa K, Ohkawa S. Effects of rabeprazole, lansoprazole and omeprazole on intragastric pH in CYP2C19 extensive metabolizers. Aliment Pharmacol Ther. 2002;16:1811-1817. [Cited in This Article: ] |
| 18. | Dimenas E. Methodological aspects of evaluation of Quality of Life in upper gastrointestinal diseases. Scand J Gastroenterol Suppl. 1993;199:18-21. [Cited in This Article: ] |
| 19. | Dimenas E, Carlsson G, Glise H, Israelsson B, Wiklund I. Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl. 1996;221:8-13. [Cited in This Article: ] |
| 20. | Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172-180. [Cited in This Article: ] |
| 21. | Ghillebert G, Demeyere AM, Janssens J, Vantrappen G. How well can quantitative 24-hour intraesophageal pH monitoring distinguish various degrees of reflux disease? Dig Dis Sci. 1995;40:1317-1324. [Cited in This Article: ] |
| 22. | Mittal RK, Holloway RH, Penagini R, Blackshaw LA, Dent J. Transient lower esophageal sphincter relaxation. Gastroenterology. 1995;109:601-610. [Cited in This Article: ] |
| 23. | Sachs G. Proton pump inhibitors and acid-related diseases. Pharmacotherapy. 1997;17:22-37. [Cited in This Article: ] |
| 24. | Rohss K, Lind T, Wilder-Smith C. Esomeprazole 40 mg provides more effective intragastric acid control than lansoprazole 30 mg, omeprazole 20 mg, pantoprazole 40 mg and rabeprazole 20 mg in patients with gastro-oesophageal reflux symptoms. Eur J Clin Pharmacol. 2004;60:531-539. [Cited in This Article: ] |
| 25. | Rohss K, Wilder-Smith C, Naucler E, Jansson L. Esomeprazole 20mg provides more effective intragastric Acid control than maintenance-dose rabeprazole, lansoprazole or pantoprazole in healthy volunteers. Clin Drug Investig. 2004;24:1-7. [Cited in This Article: ] |
| 26. | Rohss K, Hasselgren G, Hedenstrom H. Effect of esomeprazole 40 mg vs omeprazole 40 mg on 24-hour intragastric pH in patients with symptoms of gastro-esophageal reflux disease. Dig Dis Sci. 2002;47:954-958. [Cited in This Article: ] |
| 27. | Miner P Jr, Katz PO, Chen Y, Sostek M. Reanalysis of intragastric pH results based on updated correction factors for Slimline and Zinetics 24 single-use pH catheters. Am J Gastroenterol. 2006;101:404-405; author reply 405-406. [Cited in This Article: ] |
| 28. | Johnsson F, Weywadt L, Solhaug JH, Hernqvist H, Bengtsson L. One-week omeprazole treatment in the diagnosis of gastro-oesophageal reflux disease. Scand J Gastroenterol. 1998;33:15-20. [Cited in This Article: ] |
| 29. | Fass R, Ofman JJ, Sampliner RE, Camargo L, Wendel C, Fennerty MB. The omeprazole test is as sensitive as 24-h oesophageal pH monitoring in diagnosing gastro-oesophageal reflux disease in symptomatic patients with erosive oesophagitis. Aliment Pharmacol Ther. 2000;14:389-396. [Cited in This Article: ] |
| 30. | Meier JH, McNally PR, Punja M, Freeman SR, Sudduth RH, Stocker N, Perry M, Spaulding HS. Does omeprazole (Prilosec) improve respiratory function in asthmatics with gastroesophageal reflux? A double-blind, placebo-controlled crossover study. Dig Dis Sci. 1994;39:2127-2133. [Cited in This Article: ] |
| 31. | Hanson DG, Kamel PL, Kahrilas PJ. Outcomes of antireflux therapy for the treatment of chronic laryngitis. Ann Otol Rhinol Laryngol. 1995;104:550-555. [Cited in This Article: ] |
| 32. | Holtmann G, Cain C, Malfertheiner P. Gastric Helicobacter pylori infection accelerates healing of reflux esophagitis during treatment with the proton pump inhibitor pantoprazole. Gastroenterology. 1999;117:11-16. [Cited in This Article: ] |