Published online Sep 7, 2008. doi: 10.3748/wjg.14.5217
Revised: August 18, 2008
Accepted: August 25, 2008
Published online: September 7, 2008
AIM: To determine whether efflux systems contribute to multidrug resistance of H pylori.
METHODS: A chloramphenicol-induced multidrug resistance model of six susceptible H pylori strains (5 isolates and H pylori NCTC11637) was developed. Multidrug-resistant (MDR) strains were selected and the minimal inhibitory concentration (MIC) of erythromycin, metronidazole, penicillin G, tetracycline, and ciprofloxacin in multidrug resistant strains and their parent strains was determined by agar dilution tests. The level of mRNA expression of hefA was assessed by fluorescence real-time quantitative PCR. A H pylori LZ1026 knockout mutant (ΔH pylori LZ1026) for (putative) efflux protein was constructed by inserting the kanamycin resistance cassette from pEGFP-N2 into hefA, and its susceptibility profiles to 10 antibiotics were evaluated.
RESULTS: The MIC of six multidrug-resistant strains (including 5 clinical isolates and H pylori NCTC11637) increased significantly (≥ 4-fold) compared with their parent strains. The expression level of hefA gene was significantly higher in the MDR strains than in their parent strains (P = 0.033). A H pylori LZ1026 mutant was successfully constructed and the ΔH pylori LZ1026 was more susceptible to four of the 10 antibiotics. All the 20 strains displayed transcripts for hefA that confirmed the in vitro expression of these genes.
CONCLUSION: The efflux pump gene hefA plays an important role in multidrug resistance of H pylori.
-
Citation: Liu ZQ, Zheng PY, Yang PC. Efflux pump gene
hefA ofHelicobacter pylori plays an important role in multidrug resistance. World J Gastroenterol 2008; 14(33): 5217-5222 - URL: https://www.wjgnet.com/1007-9327/full/v14/i33/5217.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.5217
| Strains | Exptl condition | Agar dilution test MIC (μg/mL) | ||||
| MTZ | ERY | CIP | TET | PEN | ||
| 03154 | Before induction | 0.125 | 0.125 | 0.25 | 0.25 | 0.125 |
| After induction (fold) | 8× | 4× | 4× | 8× | 16× | |
| 12025 | Before induction | 2 | 0.063 | 0.125 | 0.03 | 0.063 |
| After induction (fold) | 16× | 2× | 8× | 4× | 16× | |
| 12021 | Before induction | 4 | 0.125 | 0.25 | 0.125 | 0.063 |
| After induction (fold) | 16 | 1× | 16× | 8× | 8× | |
| 11032 | Before induction | 1 | 0.063 | 0.063 | 0.063 | 0.25 |
| After induction (fold) | 8× | 4× | 4× | 16× | 16× | |
| 03174 | Before induction | 0.5 | 0.125 | 0.25 | 0.125 | 0.125 |
| After induction (fold) | 8× | 1× | 8× | 4× | 32× | |
| 11637 | Before induction | 0.5 | 0.063 | 0.125 | 0.03 | 0.25 |
| After induction (fold) | 4× | 2× | 4× | 8× | 16× | |
| Strains | PT (hefA/gyrB) | MDR (hefA/gyrB) |
| 03154 | 1.87 | 2.67 |
| 12025 | 0.32 | 2.84 |
| 12021 | 1.22 | 8.94 |
| 11032 | 3.84 | 5.04 |
| 03174 | 4.16 | 6.03 |
| 11637 | 4.41 | 9.56 |
| Total (mean ± SD) | 2.6356 ± 1.7245 | 5.8466 ± 2.9370 |
H pylori is a Gram-negative bacterium that colonizes human gastric mucosa[1] and plays an important role in the pathogenesis of chronic gastritis, peptic ulcer, gastric adenocarcinoma, and gastric mucosa-associated lymphoid tissue lymphoma[2,3]. Successful treatment usually requires two or three kinds of antibiotics in combination with a proton pump inhibitor. In recent years, the eradication rate of H pylori for standard therapies has decreased due to the increasing antimicrobial resistance[4,5]. Possible mechanisms of intrinsic drug resistance involve decreased drug uptake or increased drug efflux[6]. Efflux of compounds is a phenomenon commonly observed in bacteria[7-9]. Through this process, organisms are protected from possible toxic effects of metabolite accumulation or external compounds, and compound efflux results in a decreased susceptibility to a variety of antibiotics. Five families of multidrug efflux transporters have been described[10]. One of them, widespread in Gram-negative bacteria, is the resistance-nodulation-division (RND) family of efflux systems[11-13]. The RND family of efflux systems has three components: inner membrane efflux proteins (IEPs) which act with the other two components, a periplasmic efflux protein (PEP) which facilitates interaction with the other two components, and an outer membrane efflux protein (OEP) which is the TolC (the outer membrane efflux protein in Escherichia coli) or a TolC homolog[14].
Bina JE and coworkers[15] have identified three RND efflux systems, namely hefABC, hefDEF, and hefGHI. Each of them is consisted a translocase, an accessory protein, and a TolC homolog. hefA, hefD, and hefG are the TolC homolog encoding the outer membrane efflux protein. In their study, the hefGHI operon was expressed only in vivo. Nevertheless, they could not establish a role of these efflux systems in antibiotic resistance. An unfortunate choice of compounds and a methodology that may not be sensitive enough to relatively small differences in susceptibilities between the mutant and parental strains may have impacted their study. van Amsterdam et al[16] identified 27 putative translocases in the H pylori 26695 genome, but only four putative H pylori OEPs or TolC homologs. Parallel translocases may function in a limited number of OEPs[17]. Thus, inactivation of a TolC-like protein may affect the functions of multiple translocases. They evaluated the susceptibility profiles of the inactivation of the four TolC homologs after insertion, but could not quantitate the operon expression levels of the efflux systems in multidrug resistant strains of H pylori. In view of the biological difference of the H pylori strains in Asia, Europe and North America[18], the present study was to determine whether efflux systems of H pylori contribute to antimicrobial susceptibility. A chloramphenicol-induced multidrug resistance model of 6 susceptible H pylori strains (5 isolates and H pylori NCTC11637) was developed by detecting the minimal inhibitory concentration (MIC) of the strains to metronidazole, tetracycline, erythromycin, penicillin G, and ciprofloxacin. The levels of mRNA expression of hefA in multidrug-resistance (MDR) strains and their parent strains were assessed by fluorescence real-time quantitative PCR. To further evaluate the role of hefA in multidrug resistance of H pylori, a clinical isolate of H pylori LZ1026 was selected, which represent the Chinese strains. A H pylori LZ1026 knockout mutant was constructed and its susceptibility profiles to 10 kinds of antibiotics were evaluated.
Chemical reagents were purchased from TaKaRa Biotechnology Co. Ltd (Dalian, China). Restriction enzymes, polymerases, T4 DNA ligase, Quant SYBR Green PCR Kits and other molecular biology reagents were purchased from Biosail Biotechnology Co. Ltd (Beijing, China), and used following their manufacturers’ instructions. Amoxicillin, cefotaxime, ceftazidime, polymyxin B, nalidixic acid, clarithromycin, norfloxacin, gentamicin, metronidazole, tetracycline, erythromycin, chloramphenicol, and ciprofloxacin, penicillin G were purchased from the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China). Nucleic acid sequencing and synthesis were performed in SaiBaiSheng Biotechnology Co. Ltd (Beijing, China).
H pylori LZ1026 and 20 other clinical isolates of H pylori were obtained from routine cultures of clinical gastric biopsies from patients with peptic ulcer or chronic active gastritis at the Second Affiliated Hospital of Zhengzhou University (Zhengzhou, China). H pylori NCTC11637 obtained from HeNan Key Laboratory of Molecular Medicine was used as a reference. Isolates were cultured on Brucella agar medium plates containing 7% lysed sheep blood at 37°C under microaerobic conditions (50 mL/L O2, 100 mL/L CO2, 850 mL/L N2) for 48-72 h. Identification of H pylori isolates was based on the results of Gram staining, cell morphology, and positive reaction for catalase, oxidase and urease activity. Putative multidrug efflux knockout mutant of H pylori LZ1026 was grown on sheep blood agar plates containing 25 μg of kanamycin (KAN) per mL and 100 μg of ampicillin (AMP) per mL. The vectors pBluescript II SK (-)and pEGFP-N2 were from HeNan Key Laboratory of Molecular Medicine. E.coli DH5α was used for subcloning the hefA operon. E.coli were grown in Luria broth. For cloning in E.coli, 100 mg/mL AMP was used.
Susceptible strains were isolated from gastric biopsy samples using multiple antibiotic resistance induction tests. Induction of chloramphenicol resistance of susceptible isolates was performed by selecting resistant colonies that arose in the agar plates containing 1/2 × MIC chloramphenicol. The resistant colonies were incubated for 48-72 h under microaerobic conditions to increase the concentration of chloramphenicol by one fold up to 128 × MIC. The strains were further incubated on fresh plates with no chloramphenicol for 4 generations, and then transfered onto plates containing 4 × MIC chloramphenicol[19].
Induced colonies were maintained on plates containing 4 × MIC of erythromycin, metronidazole, tetracycline, penicillin G or ciprofloxacin, respectively. The colonies were incubated for 48-72 h under microaerobic conditions. A four-fold increase in MIC of the multidrug resistant strains was considered significant[20]. Six multidrug resistant strains were selected.
H pylori cells grown for 48 h on sheep blood agar plates were resuspended in phosphate-buffered saline. Suspensions of H pylori were adjusted to an optical density of 0.1 at 625 nm , and 1 μL of these suspensions containing approximately 105 CFU/mL, was spread on horse blood agar plates containing approximately 5 × 104 bacteria within 5 mm[21]. MICs of erythromycin, metronidazole, penicillin G, tetracycline, and ciprofloxacin in multidrug resistant strains and their parent isolates were determined with the conventional two-fold agar dilution tests. MICs of the kinds of 10 antibiotics against the hefA mutant strain of H pylori LZ1026 and its wild strain were also detected[22].
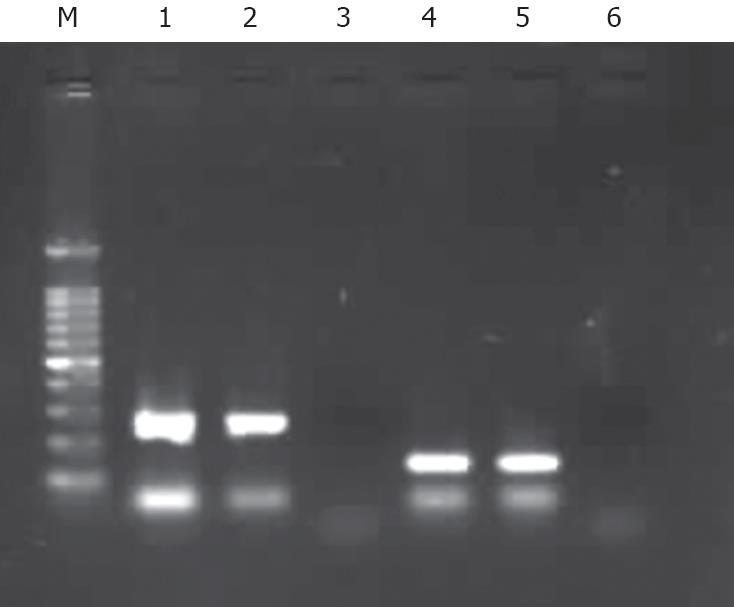
RNA was isolated using the total RNA kit (SBS Genetech Co., Ltd Beijing, China) and reverse transcribed into cDNA. Complete removal of DNA was verified by direct PCR with the RNA as a template (Figure 1). hefA, versus gyrB (a housekeeping gene encoding for gyrase B), was utilized to study the relative expression of the hefA gene in 6 multidrug resistant strains, and their parent strains: H pylori 03154, H pylori 12025, H pylori 12021, H pylori 11032, H pylori 03174, NCTC11637. cDNA of hefA and gyrB was amplified using a 5700 sequence detector real time PCR machine (Perkin Elmer Company) in the presence of Real Master Mix (SYBR Green). The gene-specific primers used were designed based on the sequence alignments of the genes from H pylori 11637 in GenBank. The sequences of hefA (accession No: AF059041) are F: (5’-ACGCCTCGAGTAAAAGCG CAAGGGAATTTG-3’) and R: (5’-ACGCTCTAG ATTCGCTAATTGGCCTAGCAT-3’). The PCR primers were predicted to amplify a 162-bp amplicon. Expression of the housekeeping gene gyrB (accession No: AB084049) was assessed in parallel with the primer pair gyrB: F: (5’-TTACTACGACTTATCCTGGGGCTA GCGCTG-3’) and R: (5’-CCCCATCAATTTCCACAT TCTCCGC-3’). The PCR primers were predicted to amplify a 267-bp amplicon.
To plot standard curves for real-time PCR, cDNAs of the hefA and gyrB genes were cloned into the pMD19-T vector system (TaKaRa Biotechnology). The vector containing cDNAs of the hefA or gyrB genes with known molar concentrations was utilized. Single reactions were prepared for each cDNA along with each serial of dilution using the SYBR Green Master Mix (Stratagene). Each PCR also included a reverse transcription negative control to confirm the absence of genomic DNA, and a non template negative control to check the primer-dimer. Each reaction consisted of 20 μL, containing 2 μL of cDNA and 5 pmol of each primer. The cycling conditions were 1 cycle of denaturation at 95°C for 1 min, followed by 35 three-segment cycles of amplification at 95°C for 30 s, at 55°C for 1 min, and at 68°C for 30 s during which the fluorescence was automatically measured, and one three-segment cycle of product melting at 95°C for 1 min, at 55°C for 30 s, and at 95°C for 30 s. The baseline adjustment method of the Gene Amp 5700 SDS (Perkin-Elmer) software was used to determine Ct (the threshold cycle) in each reaction. A melting curve was plotted for each primer pair to verify the presence of one gene-specific peak, and the absence of primer dimer. All samples were amplified in three independent reactions, and the mean was used for further analysis[23-25].
To assess whether the differences were actually statistically significant, an analysis of paired-samples t - test was utilized to study the degree of statistical significance of hefA gene expression between MDR and parent strains.
All standard DNA techniques, transformation of E.coli, and DNA analysis procedures were performed as previously described[26-28]. Plasmid DNA was isolated using a TIANprep Mini plasmid kit (TianGen Biotech Co. Ltd, Beijing, China). H pylori LZ1026 strain was isolated from a patient with peptic ulcer, and its internal portion (bp 277 to 1 574) of the hefA gene (reference from H pylori 11637 in GenBank accession number AF059041) was amplified. A restriction fragment, approximately 1298 bp, was purified and ligated into XbaI and XhoI-digested vector pBluescript II SK(-). H pylori LZ1026 knockout mutant for (putative) efflux protein was constructed by inserting the KAN resistance cassette from vector pEGFP-N2 into hefA, resulting in an 859 bp deletion. This suicide plasmid was then introduced into H pylori LZ1026 by natural transformation, and transformants were selected by plating them on a selective medium containing 25 mg of kanamycin/mL. Insertion of the KAN resistance cassette at the desired location(s) in the H pylori putative efflux gene was confirmed by PCR. Each clone was sequenced by Biosia Biotechnology Company (Shanghai, China).
To obtain the multidrug-resistant strains, a chloram-phenicol-induced model was developed. Following one-fold concentration increase of chloramphenicol, the MICs of chloramphenicol-induced strains resistant to metronidazole, tetracycline, erythromycin, penicillin G, and ciprofloxacin were detected. The MICs of 6 multidrug-resistant strains (including 5 clinical isolates and H pylori NCTC11637) were significantly increased (≥ 4-fold) compared with their parent strains (Table 1).
The expression of hefA in multidrug resistant strains and their parent isolates was assessed by relative real-time RT-PCR. Each relative expression value was the mean of three replicas. The relative expression of hefA versus gyrB in 5 clinical isolates and H pylori 11637 was significantly higher in MDR (5.8466 ± 2.9370) than in PT (2.6356 ± 1.7245) (Table 2). The results reveal that the relative expression of hefA was higher in the induced multidrug resistant strains than in their wild isolates. The difference in hefA expression was statistically significant (P =0.033) (Figure 2).
To further evaluate the role of efflux pump gene hefA of H pylori in multidrug resistance, a H pylori LZ1026 mutant was successfully constructed, and its disrupted hefA gene was uniquely different from that of the wild strain. A hefA gene fragment (about 1147 bp) of H pylori LZ1026 was sequenced and submitted to the GenBank (accession No. EU271683). Susceptibilities to wild-type strain of H pylori (H pylori LZ1026) and its isogenic mutant with putative RND outer membrane efflux protein were determined. The hefA (H pilori 0605, numbers refer to the loci in H pylori 26695) was genetically inactivated. MICs were determined by agar dilution tests. The H pylori mutant increased its susceptibility. The MIC of four of the 10 tested kinds of antibiotics (amoxicillin, cefotaxime, ceftazidime, polymyxin B, ciprofloxacin, nalidixic acid, clarithromycin, norfloxacin, chloramphenicol, and gentamicin,) was decreased at least 8-fold in the H pylori LZ1026 mutant, 8-fold in clarithromycin, 32-fold in cefotaxime, 16-fold in chloramphenicol, 8-fold in gentamicin. The MICs were decreased after treatment with different antibiotics, which is consistent with the hypothesis that the product of hefA participates in multidrug efflux.
Transcription of the gene hefA encoding a homolog of E.coli TolC outer membrane protein was assessed by RT-PCR with cDNA obtained from 20 different H pylori isolates. All the 20 strains displayed transcripts of hefA that confirmed the in vitro expression of these genes (data not shown).
Treatment of H pylori infection usually requires administration of two or more kinds of antibiotics concurrently. However, it may ultimately not be sufficient due to increased antibiotic resistance. Indeed, bacterial resistance to antibiotics hampers treatment of H pylori infections. Besides chromosomally-encoded drug resistance, intrinsic resistance to toxic compounds through increased export might be of importance in multidrug resistance of H pylori. Efflux systems have been identified in H pylori[15,16], yet the possibility that these systems are implicated in multidrug resistance has not been established previously[15]. In this study, the hefA gene was chosen from three TolC homologs: hefA, hefD and hefG, which encode the outer membrane efflux protein in H pylori. It was demonstrated earlier that the hefD and hefG genes are only poorly expressed in vitro and only RND efflux systems are known to have a wide variety of antibiotic substrates[15,22].
In the present study, because it was laborious to select the multidrug resistant strains from clinical isolates of H pylori, we developed a chloramphenicol-induced multidrug resistant model of H pylori, for the first time to our knowledge. Using this model, six multidrug resistant strains were elicited successfully, and their MICs of metronidazole, tetracycline, erythromycin, penicillin G, and ciprofloxacin were significantly increased (≥ 4-fold) compared with their parent strains, except that the MIC of erythromycin was mildly increased in 4 wild strains, indicating a difference in substrate specificity with other bacteria[29,30]. In contrast, they could only dampen the function of a group of efflux systems by constructing mutant strain. But, they could not quantitate the operon expression levels in the efflux systems[16]. In this study, the relative real-time RT-PCR was introduced to assess the expression level of the hefA gene encoding the outer membrane efflux protein in 5 clinical isolates and H pylori11637, suggesting that the relative expression of hefA is higher in induced multidrug resistant strains than in their wild susceptible isolates. This is consistent with the hypothesis that the expression of RND efflux systems in many bacteria is regulated by environmental stimuli, including the presence of antibiotics and antimicrobial compounds, growth stage, and stress factors[7-9]. By inserting the KAN resistance cassette into hefA, we also constructed a H pylori mutant strain (ΔH pylori LZ1026). By detecting the susceptibility to 10 kinds of antimicrobials with a more sensitive method of two-fold agar dilution tests, we showed that similar to other gram-negative organisms, the H pylori hefA mutant increased its susceptibility to antibiotics, which is consistent with the findings in a previous study[22], confirming that high expression of the hefA plays an important role in MDR of H pylori. Since H pylori contain an active multidrug efflux mechanism, compound efflux needs to be taken into account when determining resistance mechanisms in H pylori.
In recent years, the eradication rates of H pylori for standard therapies have decreased due to increasing antimicrobial resistance. Multidrug resistant H pylori strains have already been discovered. Possible mechanisms underlying multidrug resistant H pylori strains are involved in decreased drug uptake or increased drug efflux. Efflux of compounds is a phenomenon commonly observed in bacteria, and compound efflux decreases the susceptibility of H pylori strains to a variety of antibiotics. The contribution of efflux proteins to antibiotic resistance of H pylori strains is not well established.
With the increasing antimicrobial resistance to H pylori, multidrug resistant H pylori strains have been discovered. Researches on the mechanisms of antibiotic resistance of H pylori have becoming a medical research hotspot. The mechanism underlying multidrug resistance of H pylori is still unclear.
The contribution of efflux proteins to antibiotic resistance of H pylori, strains is not well established. In view of the biological difference of H pylori strains in Asia, Europe and North America, H pylori strains were isolated from Chinese people in the present study. The study was to determine whether efflux systems in H pylori strains contribute to their antimicrobial susceptibility. A chloramphenicol-induced multidrug resistant model of H pylori strains was developed. The level of mRNA expression of hefA in multidrug-resistant (MDR) strains and their parent strains were assessed by fluorescence real-time quantitative PCR. A H pylori LZ1026 knockout mutant was constructed and its susceptibility profiles to 10 kinds of antibiotics were evaluated.
This study confirmed that high expression of the hefA plays an important role in MDR of H pylori. Since H pylori contain an active multidrug efflux mechanism, compound efflux needs to be taken into account when determining resistance mechanisms in H pylori.
Efflux pump is chromosomally located or acquired by bacteria, which can either be activated by environmental signals or by a mutation in a regulatory gene. Two major categories exist: one is energized by proton motive force and the other is dependent on ATP. The pumps may have limited or broad substrates, the so-called multiple drug resistant pumps themselves form a number of related families.
The authors studied the significance of efflux pump gene hefA in multidrug resistance of H pylori. The study is interesting and well designed.
Peer reviewer: Tadashi Shimoyama, MD, Hirosaki University, 5 Zaifu-cho, Hirosaki 036-8562, Japan
S- Editor Li DL L- Editor Wang XL E- Editor Ma WH
| 1. | Moayyedi P, Hunt RH. Helicobacter pylori public health implications. Helicobacter. 2004;9 Suppl 1:67-72. [Cited in This Article: ] |
| 2. | Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1:1311-1315. [Cited in This Article: ] |
| 3. | Crowe SE. Helicobacter infection, chronic inflammation, and the development of malignancy. Curr Opin Gastroenterol. 2005;21:32-38. [Cited in This Article: ] |
| 4. | Egan BJ, Katicic M, O’Connor HJ, O’Morain CA. Treatment of Helicobacter pylori. Helicobacter. 2007;12 Suppl 1:31-37. [Cited in This Article: ] |
| 5. | Malfertheiner P, Megraud F, O’Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ. Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772-781. [Cited in This Article: ] |
| 6. | Nikaido H. Antibiotic resistance caused by gram-negative multidrug efflux pumps. Clin Infect Dis. 1998;27 Suppl 1:S32-S41. [Cited in This Article: ] |
| 7. | Borges-Walmsley MI, Walmsley AR. The structure and function of drug pumps. Trends Microbiol. 2001;9:71-79. [Cited in This Article: ] |
| 8. | Putman M, van Veen HW, Konings WN. Molecular properties of bacterial multidrug transporters. Microbiol Mol Biol Rev. 2000;64:672-693. [Cited in This Article: ] |
| 9. | Dastidar V, Mao W, Lomovskaya O, Zgurskaya HI. Drug-induced conformational changes in multidrug efflux transporter AcrB from Haemophilus influenzae. J Bacteriol. 2007;189:5550-5558. [Cited in This Article: ] |
| 10. | Paulsen IT, Chen J, Nelson KE, Saier MH Jr. Comparative genomics of microbial drug efflux systems. J Mol Microbiol Biotechnol. 2001;3:145-150. [Cited in This Article: ] |
| 11. | Saier MH Jr, Tam R, Reizer A, Reizer J. Two novel families of bacterial membrane proteins concerned with nodulation, cell division and transport. Mol Microbiol. 1994;11:841-847. [Cited in This Article: ] |
| 12. | Liu J, Takiff HE, Nikaido H. Active efflux of fluoroquinolones in Mycobacterium smegmatis mediated by LfrA, a multidrug efflux pump. J Bacteriol. 1996;178:3791-3795. [Cited in This Article: ] |
| 13. | Baucheron S, Imberechts H, Chaslus-Dancla E, Cloeckaert A. The AcrB multidrug transporter plays a major role in high-level fluoroquinolone resistance in Salmonella enterica serovar typhimurium phage type DT204. Microb Drug Resist. 2002;8:281-289. [Cited in This Article: ] |
| 14. | Johnson JM, Church GM. Alignment and structure prediction of divergent protein families: periplasmic and outer membrane proteins of bacterial efflux pumps. J Mol Biol. 1999;287:695-715. [Cited in This Article: ] |
| 15. | Bina JE, Alm RA, Uria-Nickelsen M, Thomas SR, Trust TJ, Hancock RE. Helicobacter pylori uptake and efflux: basis for intrinsic susceptibility to antibiotics in vitro. Antimicrob Agents Chemother. 2000;44:248-254. [Cited in This Article: ] |
| 16. | van Amsterdam K, Bart A, van der Ende A. A Helicobacter pylori TolC efflux pump confers resistance to metronidazole. Antimicrob Agents Chemother. 2005;49:1477-1482. [Cited in This Article: ] |
| 17. | Koronakis V. TolC--the bacterial exit duct for proteins and drugs. FEBS Lett. 2003;555:66-71. [Cited in This Article: ] |
| 18. | Monteiro MA, Zheng P, Ho B, Yokota S, Amano K, Pan Z, Berg DE, Chan KH, MacLean LL, Perry MB. Expression of histo-blood group antigens by lipopolysaccharides of Helicobacter pylori strains from asian hosts: the propensity to express type 1 blood-group antigens. Glycobiology. 2000;10:701-713. [Cited in This Article: ] |
| 19. | Michea-Hamzehpour M, Kahr A, Pechere JC. In vitro stepwise selection of resistance to quinolones, beta-lactams and amikacin in nosocomial gram-negative bacilli. Infection. 1994;22 Suppl 2:S105-S110. [Cited in This Article: ] |
| 20. | Wierzbowski AK, Boyd D, Mulvey M, Hoban DJ, Zhanel GG. Expression of the mef(E) gene encoding the macrolide efflux pump protein increases in Streptococcus pneumoniae with increasing resistance to macrolides. Antimicrob Agents Chemother. 2005;49:4635-4640. [Cited in This Article: ] |
| 21. | Jeannot K, Sobel ML, El Garch F, Poole K, Plesiat P. Induction of the MexXY efflux pump in Pseudomonas aeruginosa is dependent on drug-ribosome interaction. J Bacteriol. 2005;187:5341-5346. [Cited in This Article: ] |
| 22. | Kutschke A, de Jonge BL. Compound efflux in Helicobacter pylori. Antimicrob Agents Chemother. 2005;49:3009-3010. [Cited in This Article: ] |
| 23. | Aellen S, Que YA, Guignard B, Haenni M, Moreillon P. Detection of live and antibiotic-killed bacteria by quantitative real-time PCR of specific fragments of rRNA. Antimicrob Agents Chemother. 2006;50:1913-1920. [Cited in This Article: ] |
| 24. | Nygard AB, Jorgensen CB, Cirera S, Fredholm M. Selection of reference genes for gene expression studies in pig tissues using SYBR green qPCR. BMC Mol Biol. 2007;8:67. [Cited in This Article: ] |
| 25. | Nayak AK, Rose JB. Detection of Helicobacter pylori in sewage and water using a new quantitative PCR method with SYBR green. J Appl Microbiol. 2007;103:1931-1941. [Cited in This Article: ] |
| 26. | Lee DH, Oh DC, Oh YS, Malinverni JC, Kukor JJ, Kahng HY. Cloning and characterization of monofunctional catalase from photosynthetic bacterium Rhodospirillum rubrum S1. J Microbiol Biotechnol. 2007;17:1460-1468. [Cited in This Article: ] |
| 27. | Yuan JP, Li T, Shi XD, Hu BY, Yang GZ, Tong SQ, Guo XK. Deletion of Helicobacter pylori vacuolating cytotoxin gene by introduction of directed mutagenesis. World J Gastroenterol. 2003;9:2251-2257. [Cited in This Article: ] |
| 28. | Jo C, Jo SA. A simple method to construct T-vectors using XcmI cassettes amplified by nonspecific PCR. Plasmid. 2001;45:37-40. [Cited in This Article: ] |
| 29. | Burse A, Weingart H, Ullrich MS. NorM, an Erwinia amylovora multidrug efflux pump involved in in vitro competition with other epiphytic bacteria. Appl Environ Microbiol. 2004;70:693-703. [Cited in This Article: ] |
| 30. | Fehlner-Gardiner CC, Valvano MA. Cloning and characterization of the Burkholderia vietnamiensis norM gene encoding a multi-drug efflux protein. FEMS Microbiol Lett. 2002;215:279-283. [Cited in This Article: ] |