Published online Sep 28, 2007. doi: 10.3748/wjg.v13.i36.4909
Revised: June 1, 2007
Accepted: June 9, 2007
Published online: September 28, 2007
Diffuse large B-cell lymphoma is the most common type of non-Hodgkin's lymphoma. More than 50% of patients have some site of extra-nodal involvement at diagnosis, including the gastrointestinal tract and bone marrow. However, a diffuse large B-cell lymphoma presenting as acute pancreatitis is rare. A 57-year-old female presented with abdominal pain and matted lymph nodes in her axilla. She was admitted with a diagnosis of acute pancreatitis. Abdominal computed tomography (CT) scan showed diffusely enlarged pancreas due to infiltrative neoplasm and peripancreatic lymphadenopathy. Biopsy of the axillary mass revealed a large B-cell lymphoma. The patient was classified as stage IV, based on the Ann Arbor Classification, and as having a high-risk lymphoma, based on the International Prognostic Index. She was started on chemotherapy with CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone). Within a week after chemotherapy, the patient’s abdominal pain resolved. Follow-up CT scan of the abdomen revealed a marked decrease in the size of the pancreas and peripancreatic lymphadenopathy. A literature search revealed only seven cases of primary involvement of the pancreas in B-cell lymphoma presenting as acute pancreatitis. However, only one case of secondary pancreatic involvement by B-cell lymphoma presenting as acute pancreatitis has been published. Our case appears to be the second report of such a manifestation. Both cases responded well to chemotherapy.
- Citation: Saif MW, Khubchandani S, Walczak M. Secondary pancreatic involvement by a diffuse large B-cell lymphoma presenting as acute pancreatitis. World J Gastroenterol 2007; 13(36): 4909-4911
- URL: https://www.wjgnet.com/1007-9327/full/v13/i36/4909.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i36.4909
Non Hodgkin’s lymphoma (NHL) frequently arises in extra-nodal sites, with about 50% of patients having extra-nodal involvement[1]. The gastrointestinal tract is the most frequent site of involvement, with the stomach and intestines being involved in most cases[2]. Involvement of the pancreas by NHL has been infrequently reported[3,4]. Only about 0.2%-2% of patients with NHL have pancreatic involvement at the time of presentation[1,4,5] The present report describes a unique case of NHL with secondary pancreatic involvement presenting as acute pancreatitis. A literature search has revealed seven cases of primary involvement of the pancreas by B-cell lymphoma presenting as acute pancreatitis[6,7]. However, only one case of secondary pancreatic involvement by B-cell lymphoma presenting as acute pancreatitis has been reported[8].
A 57-year-old Caucasian female presented to her primary medical doctor with complaints of abdominal pain. Pain was located in the epigastrium, was dull in character, constant, and grade 3-4/10 in severity. On examination, the patient was also found to have a painful right axillary mass, which appeared to be matted lymph nodes. A biopsy of the matted lymph nodes was undertaken.
However, 4 d later, the patient presented to our emergency department because of worsening abdominal pain. Pain had increased to a severity of 9-10/10 and was associated with nausea and bilious vomiting. On physical examination, she was found to have extreme epigastric tenderness. Laboratory investigations showed an elevated serum amylase level of 623 U/L (normal range 30-110 U/L) and a serum lipase level of 4963 U/L (normal range 23-300 U/L). The patient was initially diagnosed with acute pancreatitis and admitted to the hospital. Past medical history was negative for alcohol consumption or medication use. Abdominal ultrasound done at the time of admission did not reveal any gallstones. Electrolytes and lipid panel were completely normal.
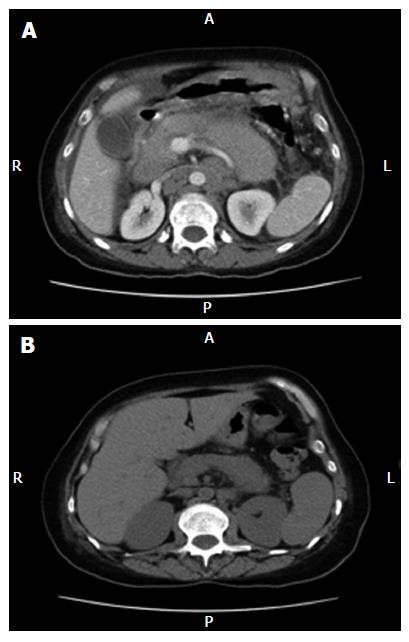
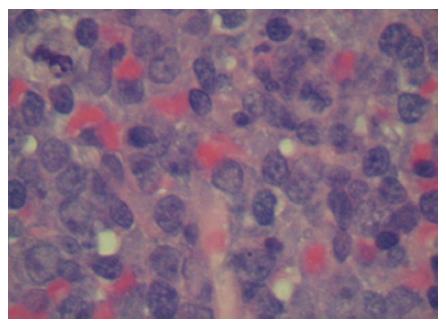
A subsequent abdominal computed tomography (CT) scan showed a diffusely enlarged pancreas due to an infiltrative neoplasm, along with bulky retroperitoneal lymphadenopathy, bulky peripancreatic, mesenteric adenopathy, ascites and peritoneal carcinomatosis (Figure 1A). A report of the biopsy of the axillary mass was available the day after admission, and showed fragments of mononuclear cells with features consistent with lymphocytes, predominantly large in size, with frequent mitotic figures and focal necrosis (Figure 2). Immunohistochemical analysis showed features consistent with a large B-cell lymphoma. Eleven immunohistochemical stains were performed, including CD20, which was positive. Serum lactic dehydrogenase level was elevated to 1227 IU/L (normal range 300-600 U/L) at the time of admission.
Bone marrow biopsy showed evidence of bone marrow involvement by the diffuse large B-cell lymphoma. The patient was classified as stage IV A, based on the Ann Arbor classification designed for Hodgkin's and non-Hodgkin's lymphoma. She was classified as high risk on the International Prognostic Index for diffuse large B-cell lymphoma.
The patient received one cycle of chemotherapy with cyclophosphamide (750 mg/m2 Intravenous), doxorubicin (50 mg/m2 intravenous), vincristine (1.4 mg/m2 intravenous) and prednisone (100 mg/m2 orally daily for 5 consecutive days) (CHOP regimen). Within a week after chemotherapy, the patient’s abdominal pain had resolved and nausea and vomiting had significantly decreased. Her serum amylase and lipase levels returned to normal (Table 1). A follow-up CT scan of the abdomen revealed a marked decrease in the size of the pancreas and retroperitoneal lymph nodes (Figure 1B).
| Serum amylaselevel (U/L) | Serumlipase (U/L) | |
| Before chemotherapy | 623 | 4963 |
| Two days after chemotherapy | 72 | 122 |
| Four days after chemotherapy | 45 | 97 |
Malignant lymphoma infrequently involves the pancreas. The estimated frequency of primary NHL of the pancreas is about 2.2%[4]. Secondary involvement of the pancreas by NHL is rare. Approximately 0.2%-2% of patients with NHL have pancreatic involvement at presentation[1,4,5]. An autopsy series of 1269 cases of NHL found pancreatic involvement in 28.9% of the cases[8]. A literature search of the PubMed database has revealed seven cases of primary involvement of the pancreas by B-cell lymphoma, presenting as acute pancreatitis[6]. However, only one case of secondary involvement of the pancreas by B-cell lymphoma presenting as acute pancreatitis has been described[6]. As in our case of secondary pancreatic involvement, that previous patient also presented with acute abdominal pain radiating to the back. He was found to have elevated serum amylase and serum lipase. A CT scan showed diffuse swelling of the pancreas with two masses, one in the corpus and one in the tail. There was also lymphadenopathy near the pancreas. CT of the thorax showed a large lymph node in the mid mediastinum. This lymph node was biopsied and revealed a large B-cell lymphoma. This case of secondary pancreatic involvement also responded well to chemotherapy. A standard regimen of chemotherapy led to normalization of serum lipase and amylase levels, as well as a decrease in the size of the pancreas and the peripancreatic and retroperitoneal lymph nodes.
Diffuse large B-cell lymphoma is the most common NHL, and makes up 30% of newly diagnosed cases. The lymphoma can present with enlarged lymph nodes at either the primary or extra-nodal sites. More than 50% of patients have some extra-nodal involvement at diagnosis[1]. The most common sites are the gastrointestinal tract and bone marrow, each being involved in 15%-20% of cases.
The presenting symptoms of pancreatic lymphoma are usually non-specific and include abdominal pain (83%), abdominal mass (58%), weight loss (50%), jaundice (37%), acute pancreatitis (12%), small bowel obstruction (12%) and diarrhea (12%). These symptoms help distinguish pancreatic lymphoma from pancreatic carcinoma[2]. Imaging plays an important role in the diagnosis and staging of pancreatic masses[5,9,12]. This is particularly true for pancreatic lymphoma, as treatment and prognosis are significantly different from those for pancreatic adenocarcinoma[9]. A CT scan is the modality commonly used for the detection of pancreatic lymphoma. Two types of morphological presentation have been reported on CT; one is a tumor-like, localized, well-circumscribed mass presenting as a hypoechogenic mass, and the second is a diffuse enlargement infiltrating the pancreas[9,10]. The well-circumscribed tumoral form is distinguished from pancreatic adenocarcinoma by the absence of pancreatic duct involvement and the presence of surrounding lymphadenopathy[9,10]. The imaging findings in the second type are similar to those in acute pancreatitis. Ultrasound- or CT-guided fine needle biopsy of the pancreatic mass can also help distinguish pancreatic lymphoma from pancreatic adenocarcinoma[4]. In the present case, pancreas biopsy was not necessary to diagnose the lymphoma because sufficient tissue was obtained from the axillary mass.
Anthracycline-based chemotherapy is the standard treatment for NHL, and includes six to eight cycles of R-CHOP for patients of all ages[11]. High-grade pancreatic lymphoma generally responds well to standard chemotherapy[11].
Our patient presented with acute abdominal pain and was in the high-risk category of the International Prognostic Index, and was therefore treated as an emergency with high-dose inductive chemotherapy. She responded very well to the chemotherapy and following the first cycle, there was a decrease in the size of the pancreas, as well as the peripancreatic and retroperitoneal lymph nodes. The patient’s abdominal pain resolved and her serum amylase and lipase levels normalized.
Secondary involvement of the pancreas by B-cell lymphoma is a rare occurrence. It is important to include such secondary involvement in the differential diagnosis of patients that present with acute pancreatitis. Pathologic diagnosis is important in distinguishing pancreatic lymphoma from pancreatic carcinoma. Most cases of pancreatic lymphoma respond very well to chemotherapy.
We thank Haswell James E, MD and Soldano Lucille, MD for helping us prepare the manuscript and for their input. A special thanks to the American Cancer Society for their support.
S- Editor Zhu LH L- Editor Kerr C E- Editor Yin DH
| 1. | Kiresi DA, Kivrak AS, Ecirli S, Toy H. Secondary breast, pancreatic, and renal involvement with non-Hodgkin's lymphoma: Imaging findings. Breast. 2006;15:106-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29:252-260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 11] [Reference Citation Analysis (0)] |
| 4. | Webb TH, Lillemoe KD, Pitt HA, Jones RJ, Cameron JL. Pancreatic lymphoma. Is surgery mandatory for diagnosis or treatment? Ann Surg. 1989;209:25-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 77] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Baylor SM, Berg JW. Cross-classification and survival characteristics of 5,000 cases of cancer of the pancreas. J Surg Oncol. 1973;5:335-358. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 174] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Bernardeau M, Auroux J, Cavicchi M, Haioun C, Tsakiris L, Delchier JC. Secondary pancreatic involvement by diffuse large B-cell lymphoma presenting as acute pancreatitis: treatment and outcome. Pancreatology. 2002;2:427-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Mofredj A, Cadranel JF, Darchy B, Barbare JC, Cazier A, Pras V, Biour M. Hepatotoxicity caused by therapeutic doses of paracetamol in alcoholics. Report of 2 cases of fatal hepatitis in cirrhosis. Ann Med Interne (Paris). 1999;150:507-511. [PubMed] [Cited in This Article: ] |
| 8. | Rosenberg SA, Diamond HD, Craver LF. Lymphosarcoma: the effects of therapy and survival in 1,269 patients in a review of 30 years' experience. Ann Intern Med. 1960;53:877-897. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Merkle EM, Bender GN, Brambs HJ. Imaging findings in pancreatic lymphoma: differential aspects. AJR Am J Roentgenol. 2000;174:671-675. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 157] [Cited by in F6Publishing: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Van Beers B, Lalonde L, Soyer P, Grandin C, Trigaux JP, De Ronde T, Dive C, Pringot J. Dynamic CT in pancreatic lymphoma. J Comput Assist Tomogr. 1993;17:94-97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 51] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Practice guidelines in Oncology-v.2. 2006: National Comprehensive Cancer Network; Non Hodgkin's lymphoma. Available from: http: //www.nccn.org/professionals/physician_gls/PDF/nhl.pdf. [Cited in This Article: ] |
| 12. | Bender GN, Case B, Tsuchida A, Timmons JH, Williard W, Lyons MF, Makuch R. Using sector endoluminal ultrasound to identify the normal pancreas when axial computed tomography is falsely positive. Invest Radiol. 1999;34:71-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |