Published online Mar 21, 2006. doi: 10.3748/wjg.v12.i11.1795
Revised: July 25, 2005
Accepted: October 26, 2005
Published online: March 21, 2006
Paraduodenal hernia is the most common internal hernia. The clinical symptoms of paraduodenal hernia may be intermittent and nonspecific. Therefore, it is difficult to diagnose preoperatively. Abdominal computed tomography (CT) scan currently plays an important role in the evaluation and management of paraduodenal hernia before surgical operation. We report one unique case of preoperatively diagnosed left paraduodenal hernia complicated by advanced ascending colon cancer and reviews of Japanese literature.
- Citation: Kurachi K, Nakamura T, Hayashi T, Asai Y, Kashiwabara T, Nakajima A, Suzuki S, Konno H. Left paraduodenal hernia in an adult complicated by ascending colon cancer: A case report. World J Gastroenterol 2006; 12(11): 1795-1797
- URL: https://www.wjgnet.com/1007-9327/full/v12/i11/1795.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i11.1795
Paraduonenal hernia is an uncommon cause of small bowel obstruction. It has been reported that the most common type of internal hernia, reported in more than 50% of internal hernia cases. We report a case of left paraduodenal hernia complicated by ascending colon cancer, which was diagnosed correctly with abdominal CT. This case was confirmed at surgical operation and the clinical and imaging findings of these hernias were reviewed in Japanese literature.
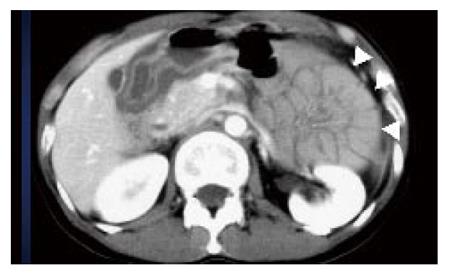
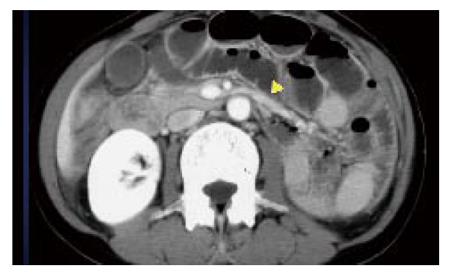
A 47-year-old woman was admitted with right lower quadrant pain and nausea. An elastic hard mass was palpable in the right lower quadrant abdomen. The body temperature was 36.8°C. Arterial blood pressure and cardiac rate were 96/80 mmHg and 70/min respectively. Laboratory tests detected only an anemia. Plain abdominal X-ray showed air-fluid levels of the small intestine loop in the upper abdomen (Figure 1). Abdominal CT scans with intravenous administration of contrast medium showed ascending colon with enhanced mass and ileum dilatation (Figure 2). Abdominal CT scan also showed an encapsulated small bowel loop with no dilatation in the left upper abdomen and the inferior mesenteric vein (IMV) was located in the anterior of the encapsulated small bowel loop formation (Figure 3). Colonoscopy revealed advanced ascending colon cancer with obstruction. We preoperatively diagnosed as ascending colon cancer with left paraduonenal hernia.
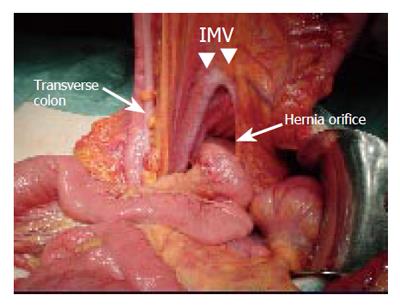
Laparotomy revealed the hernia orifice and hernia sac was located in left mesocolon (Figure 4). IMV was located in the upward of the anterior portion of the hernia sac. Approximately 40 cm of jejunum was within a hernial sac. There were no volvulus or ischemic changes of the jejunum. The patient underwent right hemicolectomy with an end-to-end ileocolonic anastomosis. Anterior hernial sac incision was also performed. The postoperative course was uneventful.
Paraduonenal hernia has been reported that the most common type of internal hernia, reported in more than 50% of internal hernia cases[1,2]. The clinical symptoms of paraduodenal hernia may be intermittent and nonspecific. It is difficult to diagnose preoperatively. Therefore, paraduodenal hernia was found incidentally at laparotomy, autopsy or during radiological investigation for unrelated disease[2-5].
Based on the published cases of paraduodenal hernia in Japan, approximately 68% (82/120 cases) were left sided, and 32% (38/120 cases) were right sided. 70% of these cases were man, and 30% cases were woman[6,7]. The mean age of the onset was 39.5 years. These frequencies of paraduonenal hernia were almost similar to the incidence in English literature.
Internal hernia complicated by colorectal cancer was reported only 3 cases. In our patient case, the origin of the bowel obstruction was not caused by left paraduonenal hernia but obstructed by advanced ascending colon cancer. Clinical findings of paraduodenal hernias are variable, ranging from mild digestive complaints to acute or chronic symptoms of obstruction, sometime asymptomatic.
Many of the paraduodenal hernia can be diagnosed incidentally at laparotomy, autopsy or during radiological investigation for an unrelated disease. Therefore, diagnosis of asymptomatic paraduodenal hernia has been difficult. On the other hand, recently reported cases of symptomatic paraduodenal hernia, 80% (8/10 cases) were diagnosed before operation[6,7]. Especially, abdominal CT currently plays an important role in the evaluation and management of internal hernias[2,3,8,9].
Enhanced CT is helpful in establishing a preoperative diagnosis of the presence of paraduonenal hernia. The specific findings of paraduonenal hernia by CT scan show clustering of small bowel loops, well-circumscribed edge that corresponds to the hernia sac, stretched and engorged mesenteric vessels. In the case of left paraduodenal hernia, IMV were usually located in the upward and anterior displacement of the hernia sac. Abnormalities in the mesenteric vessels including engorgement, crowding and stretching, and displacement of the main mesenteric trunks to the left are important clues to this diagnosis[1,10].
Paraduodenal hernias are believed to occur due to a congenital defect in the descending mesocolon. The small bowel may occur to invaginate into this space, the fossa of Landzert, which lies to the left of the fourth portion of the duodenum. The herniated small-bowel loops may become trapped within this mesenteric sac.
Treatment for the duodenal hernia is based on reduction of the hernia sac and closure of the defect or incision of the hernia sac[11,12]. Paraduodenal hernia induces an over 50% lifetime threat of incarceration, leading to bowel obstruction and strangulations. Therefore, surgical operation should be performed to avoid these complications. Indeed, 20% cases of internal herinas needed for small intestinal resection caused by bowel necrosis[6,7]. In general, postoperative course was uneventful, recurrence case was rare. Recently, laparoscopic surgery for left paraduodenal hernia without bowel necrosis may be useful surgical method because of its minimal invasiveness and aesthetic advantage[13,14]. In our case, we performed anterior hernia sac incision following the right hemicolectomy. Surgeons should pay attention to the mesenteric vessels located near the hernia sac orifice. The displacement of the main mesenteric trunks may cause vessel injury during surgical treatment.
S- Editor Wang J L- Editor Zhang JZ E- Editor Ma WH
| 1. | Tong RS, Sengupta S, Tjandra JJ. Left paraduodenal hernia: case report and review of the literature. ANZ J Surg. 2002;72:69-71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Blachar A, Federle MP, Brancatelli G, Peterson MS, Oliver JH 3rd, Li W. Radiologist performance in the diagnosis of internal hernia by using specific CT findings with emphasis on transmesenteric hernia. Radiology. 2001;221:422-428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 103] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Blachar A, Federle MP, Dodson SF. Internal hernia: clinical and imaging findings in 17 patients with emphasis on CT criteria. Radiology. 2001;218:68-74. [PubMed] [Cited in This Article: ] |
| 4. | Miller PA, Mezwa DG, Feczko PJ, Jafri ZH, Madrazo BL. Imaging of abdominal hernias. Radiographics. 1995;15:333-347. [PubMed] [Cited in This Article: ] |
| 5. | Donnelly LF, Rencken IO, deLorimier AA, Gooding CA. Left paraduodenal hernia leading to ileal obstruction. Pediatr Radiol. 1996;26:534-536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Hirasaki S, Koide N, Shima Y, Nakagawa K, Sato A, Mizuo J, Ogawa H, Ujike K, Tsuji T. Unusual variant of left paraduodenal hernia herniated into the mesocolic fossa leading to jejunal strangulation. J Gastroenterol. 1998;33:734-738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Nishida T, Mizushima T, Kitagawa T, Ito T, Sugiura T, Matsuda H. Unusual type of left paraduodenal hernia caused by a separated peritoneal membrane. J Gastroenterol. 2002;37:742-744. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Warshauer DM, Mauro MA. CT diagnosis of paraduodenal hernia. Gastrointest Radiol. 1992;17:13-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 38] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Osadchy A, Weisenberg N, Wiener Y, Shapiro-Feinberg M, Zissin R. Small bowel obstruction related to left-side paraduodenal hernia: CT findings. Abdom Imaging. 2005;30:53-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Khan MA, Lo AY, Vande Maele DM. Paraduodenal hernia. Am Surg. 1998;64:1218-1222. [PubMed] [Cited in This Article: ] |
| 11. | Campanale , Cavanagh . Left paraduodenal hernia. Am J Surg. 1956;91:436-440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Davis R. Surgery of left paraduodenal hernia. Am J Surg. 1975;129:570-573. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Antedomenico E, Singh NN, Zagorski SM, Dwyer K, Chung MH. Laparoscopic repair of a right paraduodenal hernia. Surg Endosc. 2004;18:165-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Fukunaga M, Kidokoro A, Iba T, Sugiyama K, Fukunaga T, Nagakari K, Suda M, Yosikawa S. Laparoscopic surgery for left paraduodenal hernia. J Laparoendosc Adv Surg Tech A. 2004;14:111-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |