Published online Mar 21, 2006. doi: 10.3748/wjg.v12.i11.1780
Revised: October 29, 2005
Accepted: November 18, 2005
Published online: March 21, 2006
Tumors arising from the anal canal are usually of epithelial origin and are mostly squamous cell carcinoma or basal cell carcinoma. We present a case of benign anal adenomas arising from the anus, an extremely rare diagnosis. A 78-year-old white man presented with rectal bleeding of several months duration. Examination revealed a 4 cm friable mass attached to the anus by a stalk. At surgery, the mass was grasped with a Babcock forceps and was resected using electrocautery. Microscopic examination revealed a tubulovillus adenoma with no areas of high grade dysplasia or malignant transformation. The squamocolumnar junction was visible at the edges of the lesion confirming the anal origin of the tumor. We believe the tubulovillus adenoma arose from either an anal gland or its duct that opens into the anus. Although seen rarely, it is important to recognize and treat these tumors at an early stage because of their potential to transform into adenocarcinoma.
- Citation: Anand BS, Verstovsek G, Cole G. Tubulovillous adenoma of anal canal: A case report. World J Gastroenterol 2006; 12(11): 1780-1781
- URL: https://www.wjgnet.com/1007-9327/full/v12/i11/1780.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i11.1780
The anal canal is lined by transitional mucosa in its proximal one-half and by stratified squamous epithelium in the distal portion. Anal glands and ducts arise from this area and are lined by stratified columnar epithelium. The anal glands have secretary functions and help lubricate the anal canal[1]. Tumors of the anal canal are uncommon and are classified according to their tissue of origin. These consist of tumors of epithelial origin (squamous cell carcinoma, basal cell carcinoma, adenosquamous carcinoma), lymphoid tissue (lymphoid polyp, malignant lymphoma), mesenchymal tissue (fibroma, fibrosarcoma, leiomyoma, leiomyosarcoma), neural tissues (neurofibroma, ganglioneuroma), and vascular tissue (hemangioma, angiosarcoma)[2].
The most common tumor of the anal canal is squamous cell carcinoma, which arises from the squamous epithelium of the anal canal. Rarely, adenocarcinoma of the anus has been recognized and is believed to arise from the anal glands or ducts. There is a single report of multiple adenomatous polyps arising in the transitional zone of the anus in a patient with familial adenomatous polyposis (FAP), seven years after colon resection and ileo-anal anastomosis[3].
We describe a patient with a tubulovillus adenoma arising from the anal canal. These tumors are rarely encountered in patients without predisposing risk factors, such as FAP, ulcerative colitis or Crohn’s disease.
The patient was a 78 years old white man who presented with history of rectal bleeding for several months. Bleeding occurred with almost every bowel movement and consisted of passage of fresh blood. The patient was otherwise healthy with no recent change in bowel habit, weight loss or reduced appetite. The patient was referred to the gastrointestinal service for work-up of rectal bleeding. His past history was positive only for hypertension. General physical examination was unremarkable. At the time of colonoscopy, rectal examination revealed a 4 cm friable mass attached to the anus by a definite stalk. The mass was located entirely outside the anal canal, with no extension into the rectum. Colonoscopy showed polyps in transverse (tubular adenoma), descending (tubulovillus adenoma with high grade dysplasia) and sigmoid colon (villous adenoma), which were removed endoscopically by the snare technique. At surgery, the anal polyp was found to be attached to the anus by a stalk. The mass was grasped with a Babcock forceps and was resected using electrocautery.
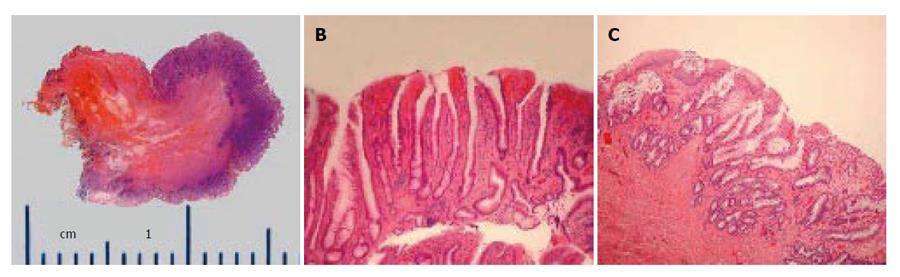
Gross examination of the specimen showed a tan-red, soft tissue mass, measuring 4.0 cm x 1.4 cm x 1.2 cm (Figure 1A). Microscopic examination revealed a tubulovillus adenoma (TVA), with nearly 30% of the surface of the polyp showing villous architecture (Figure 1B). There were no areas of high grade dysplasia or malignant transformation. The squamocolumnar junction was visible at the edges of the lesion and did not show any atypical changes (Figure 1C).
The anal canal is lined by stratified squamous epithelium and the most common tumor arising from this site is squamous cell carcinoma. Rarely, adenocarcinomas have been reported and these are believed to arise form the anal glands or their ducts which open into the anus. The current concept of the etiology of colorectal adenocarcinoma is based on the multistep genetic sequence of events which lead to the transformation of normal mucosa to adenoma and finally carcinoma[4]. That a similar sequence may occur in the development of adenocarcinoma of the anus was shown in a recent study which described the development of an invasive apocrine adenocarcinoma arising from a benign adenoma in the perianal region of a 45 year old women[5]. In our patient, the polyp was attached to the anus by a narrow stalk. Moreover, at histopathology, squamocolumnar junction was visible at the edges of the histological specimen confirming that the polyp arose from the anus and not from the rectum. We believe the site of origin of the tubulovillus adenoma in our patient was from one of the anal glands which are the only adenomatous elements in the anus. It is unclear why such tumors are not diagnosed more frequently. It is possible that because of the submucosal location of the anal glands, such adenomas are not easily visible and only become apparent when malignant transformation takes place. Clinically, it is important to recognize and treat these tumors at an early stage because of their potential to transform into adenocarcinoma.
S- Editor Wang J L- Editor Zhang JZ E- Editor Ma WH
| 1. | Corman M, Allison SI, Kuehne J. Malignant tumors of the anal canal. In Handbook of Colon & Rectal Surgery. Philadelphia: Lippincott Williams &Wilkins 2002; 574-593. [Cited in This Article: ] |
| 2. | Corman M, Allison SI, Kuehne J. Less common tumors and tumorlike lesions of the colon, rectum and anus. In Handbook of Colon & Rectal Surgery. Philadelphia: Lippincott Williams &Wilkins. 2002;594-636. [Cited in This Article: ] |
| 3. | Malassagne B, Penna C, Parc R. Adenomatous polyps in the anal transitional zone after ileal pouch-anal anastomosis for familial adenomatous polyposis: treatment by transanal mucosectomy and ileal pouch advancement. Br J Surg. 1995;82:1634. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, Nakamura Y, White R, Smits AM, Bos JL. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319:525-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4616] [Cited by in F6Publishing: 4368] [Article Influence: 121.3] [Reference Citation Analysis (0)] |
| 5. | MacNeill KN, Riddell RH, Ghazarian D. Perianal apocrine adenocarcinoma arising in a benign apocrine adenoma; first case report and review of the literature. J Clin Pathol. 2005;58:217-219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |