CASE REPORT
FS is a 52-year-old newspaper carrier working night shifts, who lives with his wife; they have three children. FS was referred from the pain clinic to the psychiatric clinic (tertiary centre, Medical University of Vienna) after 36 years of chronic pain and visiting multiple physicians (general practitioners, neurologists, anaesthetists, and orthopaedists) with the same health problem without any somatic explanation despite a repeated and thorough examination of systems – no therapy had worked. His present complaints are pain throughout the body, especially in the joints, the scalp, (papillary) breast. Furthermore, he complained about gingival paraesthesia, difficulties swallowing, digestive problems, and chronic sleep disturbances. FS is talkative, self-confident, friendly, and outgoing. At the age of 16 years, he met his first love, his admired wife-to-be, and he had his first pain attack, a terrible headache. As a child of divorced parents, he had been separated from his brother and was raised by his mother, grandparents, aunt, and in foster care. In his childhood, FS’s emotional and physical needs were consistently ignored, being beaten, and emotionally neglected in foster care. However, he took advantage of the laissez-faire style of education, truanted from school, and stayed out late in the evening. He did not finish clarinet education and began his work as a newspaper carrier, to finance a house and his family. For about 2 years, he suffered from a new kind of fierce pain attack, in his description evocative of this first attack, only deeper and affecting the whole body like “a flash resulting in a pillar of pain from head to toe”. The attacks appear about three times a month, in his free time. However, the most annoying complaint is recurrent left-sided hemiplegia in the morning, preventing him from starting the day without the help of his wife. Thus, only after his wife helps him out of the bed, he walks with a limp to the bathroom and takes an extensive shower, with the hemiplegia remitting spontaneously. FS has no explanation for his symptoms and behaviour. However, he had sought comfort in explaining them with the lunisolar tide, with changes in the weather pattern, and with tension and disconnection in family relationships. The relationship with his wife had worsened lately, together with his sexual disturbances. Due to the marital conflicts, he now is motivated for a new check-up and appears excited about any possible help[4].
OVERCOMING THE FOURTH NARCISSISTIC OFFENCE – THE CHANCE FOR AN EFFICIENT COOPERATION
Narcissistic personalities show an extreme over-reaction if confronted with a minor offence, because their grandiose views of themselves, built as a defence against any feeling of vulnerability, are threatened. Unlike a person with narcissistic personality disorder, FS acknowledges him needing help but seems prone to idealising his new saviour, which can quickly turn into devaluation when feeling vulnerable or threatened. For the physicians and therapists now confronted with FS’s chronic condition, this means to handle insecurities and to build a therapeutic relationship stable enough to endure expectable alliance ruptures, should the solution to FS’s problem not be straightforward. Due to the complexity of the somatoform/somatic symptom disorder, understanding is challenging and often requires the acceptance of not being able to know every detail but to accept the subjective burden of the patient, without giving up on trying. This implies the acceptance of limitations and a confrontation with the gap between ideal and reality. With this reasonably foreseeable loss of the feeling of omnipotence, a narcissistic wound for patients and doctors might result in the feeling of being hurt with a tendency of withdrawal resulting in a repairable interpersonal rupture. Also, interdisciplinary collaboration, needed in clinical work and research when dealing with such complex diseases, can be challenging as it requires a realistic view of one’s limitations to participate in a dialogue with experts and acknowledge contributions to the research topics from other scientific and clinical fields. Nevertheless, diversified collaboration might shed light on this complexity to reach possible treatment strategies, as well as strategies towards precise understanding and process-outcome research. But a closer differentiated look is necessary.
THEORETIC BACKGROUND: THE SOMATIC DISTRESS DISORDER
“[…] The two foes of human happiness are pain and boredom.” (Schopenhauer A)[5].
The somatoform pain disorder/somatic symptom disorder/bodily distress disorder is characterized by severe, persisting chronic pain, with a marked psychological strain and pronounced reduction of the patient’s quality of life. Furthermore, its origin as well as its overall longitudinal symptom dynamic and severity are linked to emotional conflicts and psychosocial risks and distress. With a prevalence of 9%–20% in the general population, somatoform/somatic symptom disorders’ relevance for the health care services is quite high as patients usually are heavy users of services[6-8].
Pathogenesis
Psychiatry and neurology are both sciences dealing with disorders concerning the brain–mind interface. Exploring the interdependence of psychological and biological phenomena, either in a conscious or in an unconscious way, again, might influence both biological and psychological processes, and their interrelations (e.g., psychoneuroimmunology: depression and different profiles of the immune system[9]).
Neuronal circuits active in psychosocial distress are also associated with physical pain; emotional and physical pain exist on the same continuum[10,11]. In early childhood, somatisation is regarded as a normal and necessary developmental phase, as a reaction to stress and distress, and diminishes with maturation[12]. The same reaction already in older children is regarded as a pathological one, and the need for a classification that does justice to these developmental steps, thus avoiding over-pathologising, has been highlighted[13-15]. Interpersonal and intrapersonal emotional distress is felt as agonising pain and suffering instead. In such patients, adequate ways of communicating distress are not well developed; dysfunctional interpersonal affect regulation between caregiver and child is at the origin of the disorder[12]. On a neuronal level, networks associated with interpersonal distress are also associated with the neuronal circuits responsible for pain[16-18].
Development of affect regulation
However, at the core of the problem are dysfunctional affect regulation abilities and attachment patterns, developed in early interpersonal experiences, thus being transmitted from one generation to the other[12]. Especially in vulnerable persons with genetic predisposition and in unfavourable environmental conditions and contexts such deficits might lead to somatoform disorders[12]. In the above-mentioned case report, the educational style was characterised by emotional neglect and rejection. FS developed rejection sensitivity and a high level of worry[19]. His discomfort with closeness shows up in the relationship with his wife. He is caught in repetition: his pain expression, an expression of his distress and inner tension, leads to his wife having to care for him. Thus, in a way, he is asking for closeness, but at the same time, it seems that he feels uneasy about his wife caring for him.
While in early childhood, especially in the perinatal period, arousal and excitation are experienced and regulated somatically[12], later more sophisticated ways of regulating external and internal stimuli should rise, together with the development of cognition and higher mental functioning.
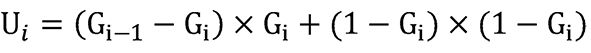
As separation from the caregiver might provoke fear in early childhood, this is one of the challenges to master in this developmental period. Diverse strategies and ways to deal with this and similarly distressing events (e.g., hunger, tiredness, pain or fever) need to be developed, partly depending on the availability of care). In psychodynamic theory this process especially has been investigated in Winnicott’s theory of holding (importance of the external object), Bion’s theory of container/contained, and Klein’s theory with a particular focus on the internal and phantasmatic experience of the child[20]. At first, the child needs soothing and satisfaction of needs by the caregiver in case of distress (compare Figure 1).
Figure 1 The emergence of mentalized affectivity.
Mutual interactions between caregiver and child are shown as a process where the caregiver infers the inner thoughts and affective states through signals expressed by the child (and the contextual information and knowledge available). At first, the child notices a somatic experience and expresses it nonverbally to the caregiver as a signal. Then, the caregiver metabolises this signal (resonance, reflection, reaction) and communicates an expression of this metabolized affect to the child (mirroring display). In the next step, the child internalises this reaction of the caregiver in response to its own experience as a picture/idea of the primal state. In such a way a transformation from a somatic experience to an integration of the child’s inner state is acquired via symbolisation in repeated social interaction.
Additionally, postevent processing of distress varies and is relevant (see[21] for social distress). However, with time, it learns to soothe itself together with an understanding of the situation together with its own and the others’ affective and mental states. Intention mirroring was found to be more frequent in securely attached mothers, based on well-attuned, affect-mirroring communication[22]. Self-compassion has been shown to be lower in patients with somatoform symptoms when confronted with healthy subjects[23]. In perpetuating the somatoform disorder, a learned bias to shift one’s attention on somatic/bodily processes leads to an exaggerated experiencing and perception of somatic signals, increasing the risk of misperception and misinterpretation of such sensations. Furthermore, also a link between attachment patterns and somatisation has been shown for adults (insecure attachment[22,24], fearful and preoccupied attachment[25]). The case history discussed earlier in this paper also shows how “doctor shopping” can be perpetuated by the patient’s insecure attachment pattern and the need for the symptom as a sign and symbol, with high costs for the health care system and a multitude of examinations for the patient.
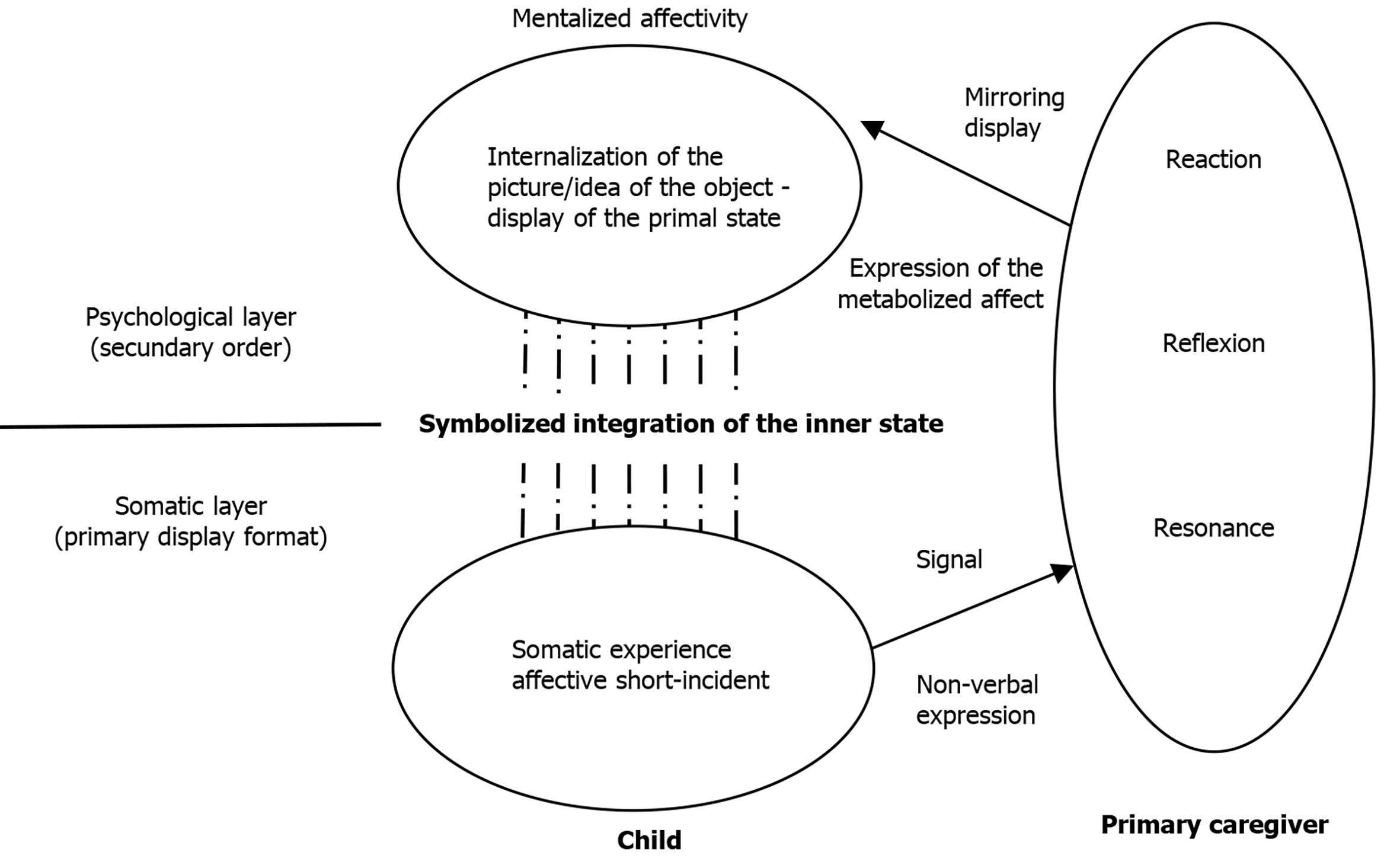
To conclude, affect regulation is linked to the attachment pattern and mediated by social interaction (see also[12], compare Figure 2). An insecure-avoidant attachment pattern is associated with problems to trust someone and the intolerance of closeness[26]. Thus, interventions addressing attachment in therapy have the potential to improve symptoms.
Figure 2 Vulnerability and psychodynamics.
Predisposing factors for somatoform disorders/somatic symptoms/bodily distress disorders
A higher lifetime prevalence of somatoform disorders has been observed for individuals with early trauma[27], lacking parental care[28], negative experiences/ stressful live events[29,30], and child abuse[31]. However, the manifestation of a somatoform disorder also depends on the parenting style[28] (e.g., avoidance/ rejection, conflicts or emotionally unstable parents, lack of discipline and inconsistent discipline, or controlling and overprotective parents)[28]. Continuity of somatic symptoms between adolescence and early adulthood has been shown and points to the high tendency of chronicity in this group of patients. Earlier research has shown that the level of somatic symptoms in a patient’s parents might be associated with the ones in their children [32,33]. In twin studies, a genetic predisposition was suggested[34].
Biological perspectives on somatoform disorders
High subjective distress, in severity not fitting the present objective findings, is one of the main symptoms of somatoform disorders (ICD10)[35]/somatic symptom/bodily distress disorders (ICD11)[2]. Unfortunately, although somatoform disorders encompass a heterogeneous group of diseases, some unrecognised diseases, misclassified as somatoform disorders might be relabelled after a repeated, sufficient examination. Furthermore, some potentially curable diseases still might lack the techniques to study them[36].
As somatoform symptoms are not considered strictly mental/psychological events, biological processes play an important role[36,37]. The underlying physiology of distress has been studied, explaining to some extent the genesis, and the experiencing of symptoms[36]. Especially research on inflammation-associated symptoms has gained promising results lately. The association between subjective health complaints and inflammation has been shown[38,39]. Raison and colleagues[39] have argued that depression is an accessory phenomenon that comes together with adaptive advantages due to genes promoting inflammation. The field of psychoneuroimmunology investigates environmental influences on the development of the immune system. Repeated exposure to danger leads to immune reactions (proinflammatory state) with proinflammatory cytokines and the possibility of immune sensitisation. For somatoform disorders and for sickness behaviour, specific cytokine patterns have been identified[40].
Social exclusion has been shown to be associated with somatic complaints, especially with pain. Social rejection and physical pain both are distressing, and they share a common somatosensory representation[41]. Experiments investigating the pain threshold in children/adolescents with somatic symptoms showed a divergent reaction regarding their sensory threshold after social exclusion when contrasted with controls[42]. While the group with somatisation showed a stable sensory threshold, the controls showed a decreased threshold[42]. Adolescents with functional abdominal pain showed increased parasympatic activation when exposed to induced social exclusion, whereas healthy controls showed no such activation pattern[43].
As mentioned above, the pain network is linked to the neuronal network concerned with the regulation of distress provoked by interpersonal stimuli. Important structures involved in distress regulation (emotional and the affective component of somatic pain) are the medial prefrontal cortex (antinociceptive effects, including biopsychological pain management but also chronification[44]), the dorsal anterior cingulate, and the anterior insula[41]; these regions are also involved in processing social rejection. While the brain regions concerned with the somatic representation of physical pain include the operculo-insular region; these regions are not activated by social rejection[41].
As pain is associated with depression and antidepressants influence pain (e.g., tricyclic antidepressants such as amitriptyline, and selective serotonin reuptake inhibitors such as citalopram), common biochemical mechanisms are likely[45].
The role of oxytocin in social cognition, including the development of attachment and trust as well as in pain has been investigated, but there are still many open questions[46].
Exogenous factors influence human life and health. Evidence suggests that social interactions might have an influence on the expression of genes[47,48], while epigenetic and genetic predispositions modify the response to environmental factors[48,49]. Epigenetic changes have been shown to be influenceable by separation and traumatisation with potentially permanent and profound changes. Mechanisms underlying epigenetic changes include DNA methylation, histone modification, RNA silencing, regulation of genes, etc.[49]. For example, epigenetic changes are one key mechanism of how stressors interact with the genome[50]. Influences on the reaction to stress in patients with depression have been shown to be associated with a changed expression of cortisol receptors in the hypothalamus (methylation and modification of histones), leading to a prolonged and pronounced stress reaction due to higher cortisol levels (changed glucocorticoid signalling). The hypothalamic–pituitary–adrenal axis activation is common in major depressive disorder[51].
Reconsidering the main aspects from the biological, psychological, developmental, and social domains it often remains open, how psychic transformations can be understood properly to provide meaningful treatments, the respective training, and to conduct appropriate process and outcome research.
UNDERSTANDING PSYCHIC TRANSFORMATIONS
One problem in psychotherapy research is finding answers to the questions of how psychotherapy works, and what works for whom, how do psychic transformations happen at all, and how to make them last? Patients requiring psychotherapy are a heterogeneous group (differences in medication, social context, comorbidities, previous therapy, age group, etc.), this makes interpretation of data difficult in investigations with small sample sizes. It is not possible to run the same experiment in the same patient twice under different environmental or social conditions, because each intervention changes the investigated individuum and context. Investigating long-term data is expensive, but long-term results matter as much as process research does. Comparison of new therapeutic approaches with the best known and best available care is particularly problematic in long-term therapies with real patients, because of good enough evidence for existing therapies. Randomisation to new therapeutic approaches and innovative interventions is problematic due to ethical concerns (potentially unknown side effects and unknown long-term outcome, freedom of choice for the paying and informed patient).
SIMULATING THE MIND AND APPLICATION
Modelling and simulation have a long history in science to gain insight into complex phenomena and conduct virtual experiments when real ones are not possible. This approach could be useful here. Artificial intelligence models of the mind–brain interface, rending exploration of machine learning capabilities possible, also could allow for investigations that are ethically or technically not possible in humans. To that end, the simulating the mind and applications (SiMA) model was developed. Far more than a mathematical toy, it supports the exploration of theoretic and abstract concepts so challenging as the connections between psyche and body.
The model of Mealy: bridging the gap
Coupling of the neurological system and the psyche: When searching for a scientific description of a model that considers a coupling of the neurological system and the psyche, one is inevitably confronted with the contradictions in the nomenclature of the different scientific communities. When we use the term “brain”, we often hear the accusation that parts of the nervous system, as well as the associated sensory and actuators systems, are being excluded. The term “mental apparatus” is quickly pushed into the corner of neurological reductionism, and the term “nervous system” is hardly associated with the psyche. Therefore, for the purpose of this article, the term Ψ-organ will be used. The term “organ” indicates that the information system of the human being can be regarded as a unified system like all other organs. The term “Ψ” indicates that mainly psychoanalytical knowledge is used to describe the psyche of the Ψ-organ.
With this foundational understanding, the challenging scientific question of how the physical and the psychological can be described without contradiction in a common and unified model can be posed.
There have been a few approaches to this question in the past; all of which have been unsatisfactory. Two of the most frequently cited are that of Peterfreund and that of Turkle[52,53]. Peterfreund was too focused on the mathematical considerations and barely made the connection to neurology. He did not achieve a complete model based on neurological as well as psychological concepts[52]. Turkle did not find a unified model between neurology and psyche, either, but focused mainly on the collaboration between artificial intelligence and psychoanalysis[53]. A relatively new idea from Solms[54] must be viewed sceptically from an information technology (computer technology) perspective. His attempt to build a bridge between the mental and neurological description is based on the assumption that one can merge the methods and laws of physics with those of information technology in one mathematical equation system, without substantiating this experimentally.
The model concept of SiMA is different. Dietrich uses Mealy’s theory, which is generally applied in computer science, to bridge the gap between the physical and the information technology fields[55,56]. It guarantees an exact merging of the neurological and the mental domains according to strict scientific principles. The experimental simulation results confirm his approach.
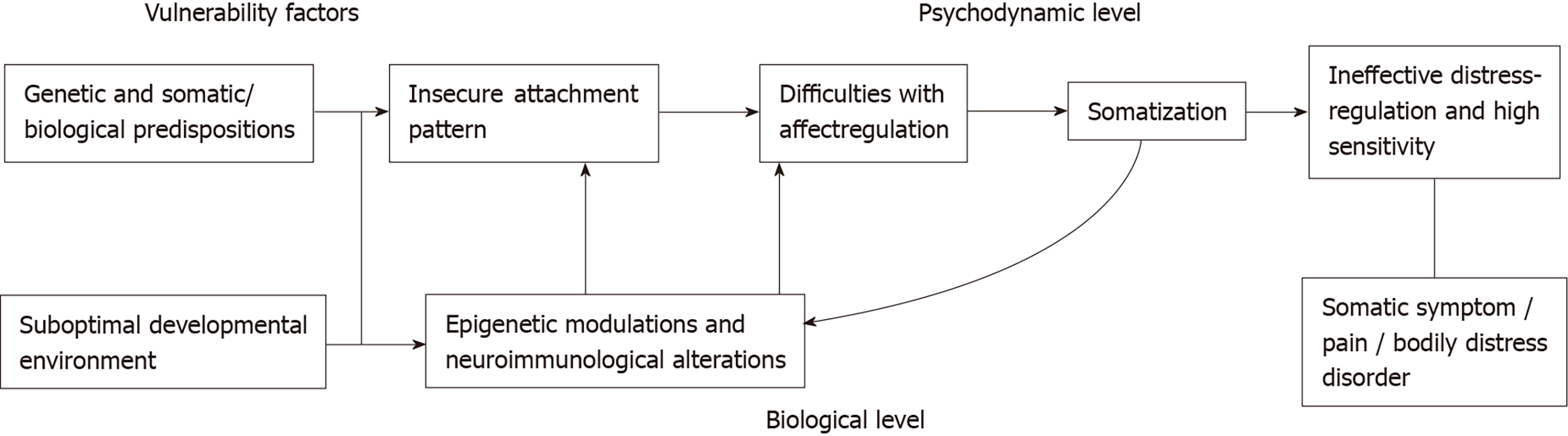
Mealy published his idea in 1955[57]. He succeeded in developing a modelling method named after him for the calculation of electronic digital circuits. The digital circuit is transferred into a two-layer model. The lower layer contains the functions that are described physically, while the upper layer contains the functions that are described in terms of information technology (Figure 3). Both layers are connected via a clearly described interface. The description is a mathematical process. It can only be imagined abstractly. One must be aware that the real circuit is conceptually split into two layers: the physical layer and the information layer (not comprehensible from a physical point of view). The interface between both layers is defined by the information flowing through them. In the lower layer, the information is described physically, and in the upper layer, the same information is described information technologically.
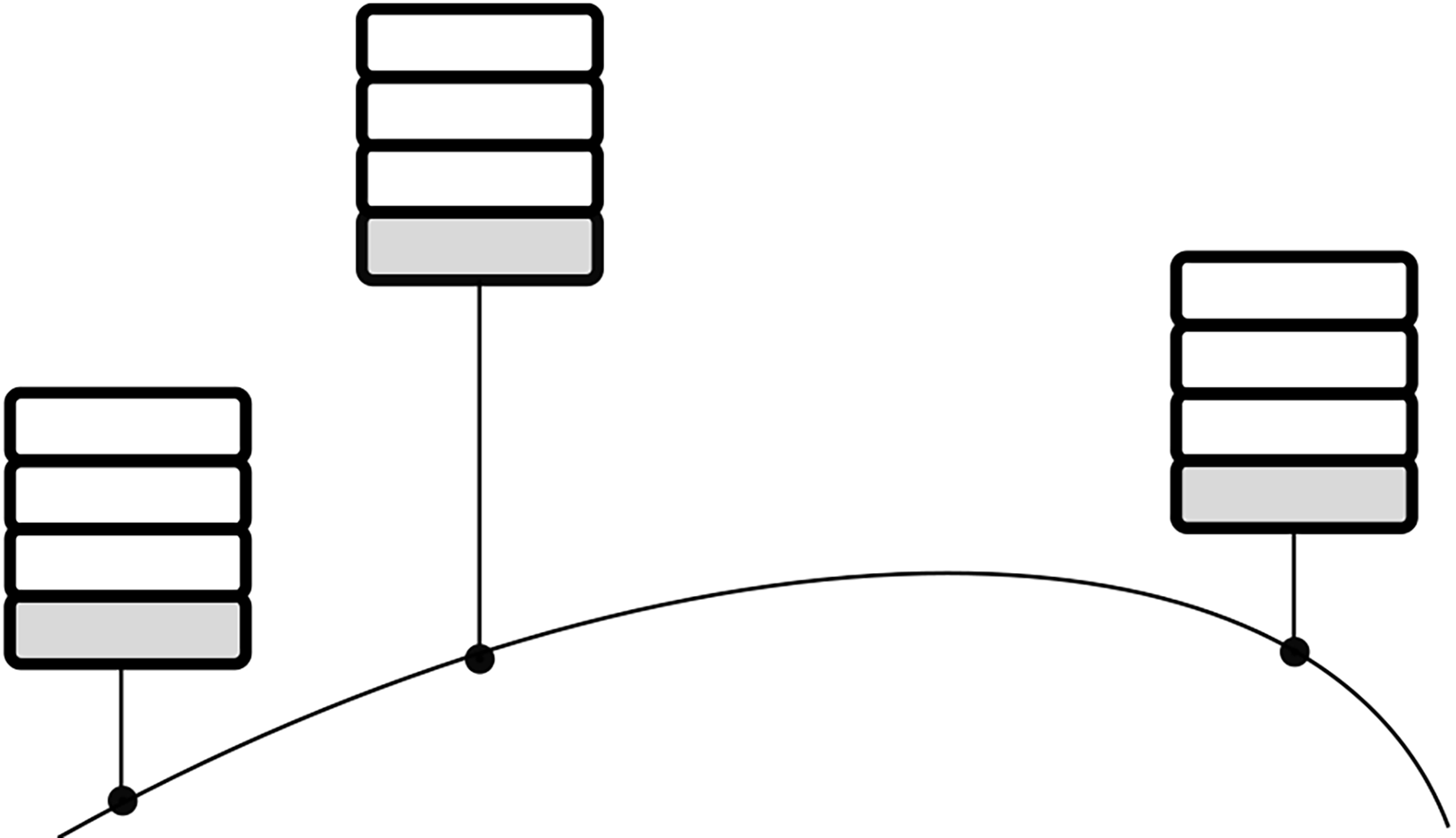
Figure 3 Mealy model.
Current state and current inputs determine the Mealy model’s output values. A mealy machine consists of a finite set of states, inputs and outputs and a transition as well as an output function. The model produces an output (h) while an input (a) is received (in the same simulation step). In this figure the real circuit is conceptually split into two layers: the physical layer (rectangle shaded in grey) and the information layer (rectangle shaded in white). The interface between both layers (dashed line) is defined by the information flowing through them. An abstract concept of the transition between the two layers (information technology and physics) is shown.
The physical layer in Figure 3 can be diverse. In digital electronic circuits, functions can be transistors, resistors, or diodes, and information can be expressed by physical quantities such as voltages or currents. Accordingly, neurons can be described based on such functions. Referring to Figure 3, the information quantities entering the lower layer (information a) are quantities that act on the human sensors and thus must be described physically. The same applies to the output quantities h. The information quantities acting within the lower layer (the information quantities b, c, f and g) are therefore to be described by electrical properties: voltages, currents and temporal behaviour of the neurons. If one changes to the upper layer, i.e., all quantities (the information quantities d and e) become independent of their underlying physics and are described purely in abstract terms. Figuratively speaking, electrical signals turn into bits and bytes. The passage of all information through the functions of the upper layer is also independent of time, it happens instantaneously. If information d in Figure 3 is generated by information c, it is simultaneously present as a quantity at the output of the upper layer and thus as a quantity f at the lower layer.
Mealy and his team were able to prove through experiments that this model – also known as the Mealy machine – was not just a mathematical gimmick. Scientists also developed modified mathematical description methods that went beyond this. Today, every design language for the development of hardware (like computer components), is based on this very abstract principle. Nowadays, no computer is conceivable without Mealy’s theory.
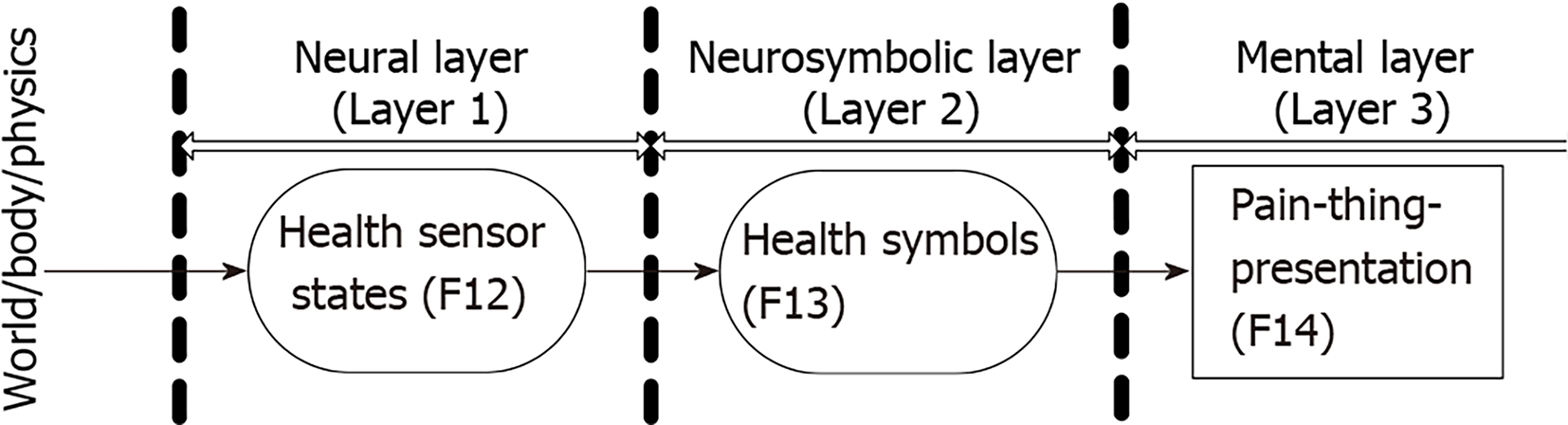
A generalization of the Mealy principle is just as important. Imagine that several computers are to communicate with each other. The first international standardised model of this kind was the International Organization for Standardization (ISO)/open systems interconnection (OSI) model. The layer described in terms of information technology can be subdivided as required and the functions it contains can be allocated within it according to their specific tasks. The layers are arranged hierarchically. Each column in Figure 4 represents such an ISO/OSI model. The lowest layer (layer 1) is always the physically described layer, which defines the (physical) connection to the other computers. The upper layers of Figure 4 are the units described in terms of information technology. This means that the upper layer in the Mealy model is subdivided into several, further layers. The basic principle is identical in both models.
Figure 4 Possible coupling of computers according to ISO/OSI.
Each column in this figure represents such an ISO/OSI model with hierarchically arranged layers. The lowest layer (rectangle shaded in grey) is always the physically described layer, which defines the (physical) connection to the other computers. The upper layers of the columns in this figure are the units described in terms of information technology (rectangles shaded in white: the upper layer in the Mealy model is subdivided into several layers as required, with functions allocated within according to the specific tasks). ISO: International Organization for Standardization; OSI model: Open Systems Interconnection model.
The original Mealy model (Figure 3) was developed for the design of digital circuits, i.e., to obtain a holistic, functional model for the physical and informational description. The generalization of this principle, i.e., the abstraction of physical signals and states into information symbols that can be further aggregated and processed on higher system layers, leads to models such as the ISO/OSI model (Figure 4) or, in SiMA, a holistic, functional model of the Ψ-organ.
To bridge the gap to the Psy-sciences to overcome the fourth narcissistic offense of not being able to understand somatic symptom disorders / bodily distress disorders good enough and provide meaningful treatment options for patients, a precise stepwise collaborative working model must be considered to simulate possible ways of understanding.
SOMATIC PAIN IN SiMA AND ITS POSSIBILITIES FOR BRIDGING THE GAP
In structuring and describing functions of the mind, SiMA builds on psychoanalytic principles and concepts[56]. Functions and their inter-relations are grouped in layers according to their association with physical, unconscious and conscious processing of information. To avoid systematic errors in the development of the technical implementation and to ensure a consistent and holistic model, the concept was developed in an interdisciplinary discourse.
A central point in the model is the feedback from the body of what in SiMA is called an agent. To that end, interfaces for sensory inputs are foreseen[58], and the body of the agent is modelled. The concept of pain, however, was not originally included[59] because in psychoanalysis, pain is only seen as a pseudo drive. “The goal of this pseudo drive is just the cessation of the organic change and the associated unpleasure. Other, direct pleasure cannot be derived from the stopping of the pain. Pain is also imperative…”[60,61]. This served as guideline for including a model of somatic pain. Its implementation was tested via simulations, and the results discussed in an interdisciplinary review.
Originally, the SiMA model did not comprise feedback to the psyche when the agent experienced pain. Consequently, the agent would not show a reaction if its health status worsened. The inclusion of the pain concept necessitated an extension of the existing model structure and the inclusion of interfaces across the layers to allow for representing somatic pain in the psyche. The source of pain are sensory inputs of the body signalling a change. In contrast to drives, pain relief cannot generate pleasure. Therefore, pain cannot be treated in the drive track of the model. Rather, it must be included in the perception track and produce corresponding unpleasure there. This unpleasure is used in turn to create rated memories and emotions.
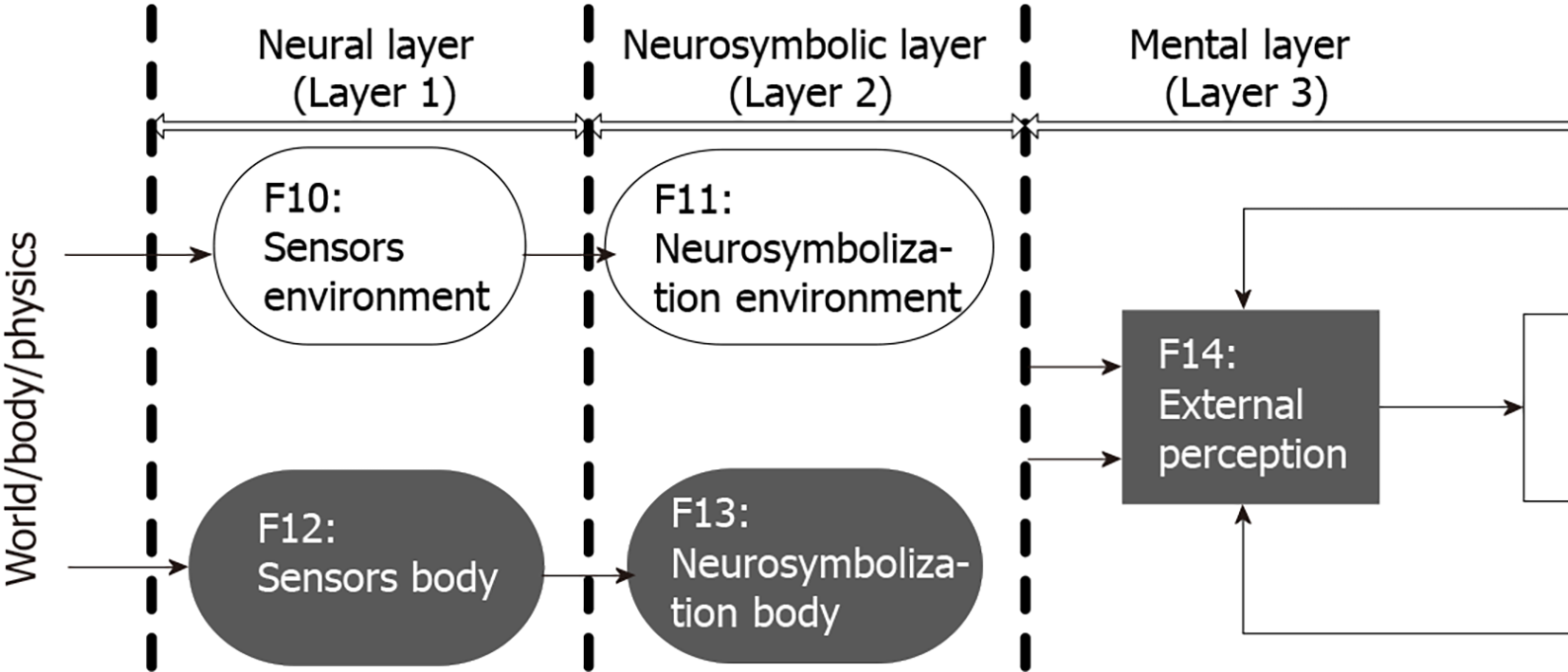
Figure 5 shows the functions added to the model (relevant for the processing of somatic pain[62]). Functions F12 generate the sensory inputs to the body. They register changes, e.g., when the agent is hurt. The sensor value is then transferred to F13 which extracts symbol’s that can subsequently be processed by the psyche. These symbols contain actual values as well as connections to the symbol health status. All this information is provided to the mental layer and further processed in F14 which generates a factual perception related to the representation of pain (Figure 6)[62]. The amount and rate of change of the symbols translate into a level of the somatic pain. Moreover, F14 generates unpleasure correlated to the pain level. This unpleasure is factored into the calculation of the emotion and added to the existing unpleasure stemming from the current drive situation. It is thus available to the functional model for subsequent decision-making and memory creation.
Figure 5 Excerpt from the simulating the mind and applications model.
The functions relevant for the processing of somatic pain are shown (marked in dark grey).
Figure 6 Creation of pain perception from the body sensors of the agent[62] Neural layer (layer 1): functions F12 generate the sensory inputs to the body (health sensor states/registering changes).
Neurosymbolic layer (layer 2): this sensor value is then transferred to F13 which extracts symbols, containing actual values as well as connections to the symbol health status. Mental layer (layer 3): all this information is provided to the mental layer and further processed in F14 which generates a factual perception related to the representation of pain (i.e., unpleasure correlated to the pain level).
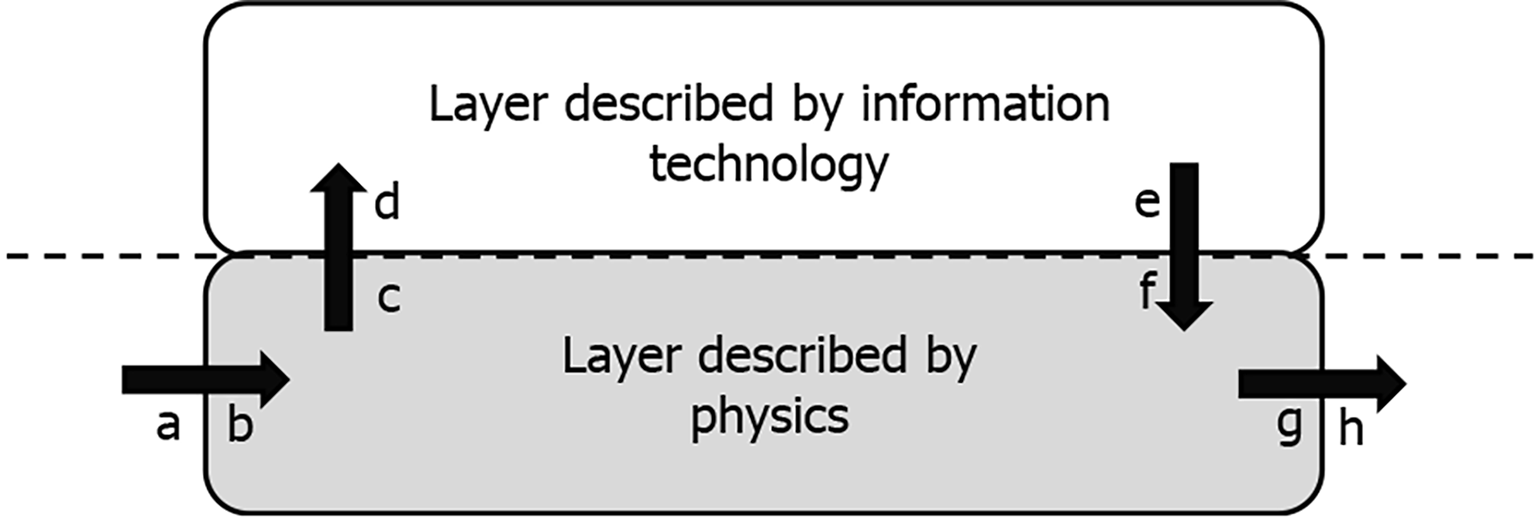
Calculation of the unpleasure in F14 accounts for changes in the health status as well as the difference to the optimal health,
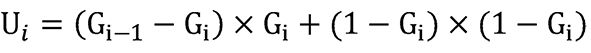
with Ui being the new unpleasure value, Gi the current health status, Gi-1 the health status from the previous simulation cycle, and 1 Gi being the difference between the current and the maximum health. The health value is from the range [0..1], where 1 represents optimal health and 0 represents the death of the agent. The resulting unpleasure is also scaled to [0..1]. The equation is split up into two parts, where the first part is the change of the current health to the previous state and the second part is the difference between current and the maximum health. Both parts are weighted by the current health status (Gi). If the health status is high, the change of health will be weighted more than the difference to the maximum health. These equations were derived in interdisciplinary discussions and proved reasonable in simulation experiments.
Optimal health and its definition are challenging, as it presents an ideal but subjective state, characterized by the absence of disease but furthermore by being at one's optimum and being balanced in all aspects of existence. Thus, a difference (1 Gi) between this ideal and the current health states (Gi) is the normal state, always including a certain but variable amount of unpleasure (Ui). The tricky part is quantifying the amount of the difference.