Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2815
Peer-review started: March 23, 2019
First decision: May 31, 2019
Revised: June 25, 2019
Accepted: July 20, 2019
Article in press: July 20, 2019
Published online: September 26, 2019
Glomus tumor is an uncommon benign tumor usually presenting with a small mass occurring in the dermis or soft tissue of an extremity, especially subungual region. However, intraneural glomus tumor is sporadic. While most of the glomus tumors are benign, atypical glomus tumors with unusual features can be occasionally found, leading to distinctive malignant potential required different therapeutic approaches. Glomus tumor of uncertain malignant potential is one type of atypical glomus tumor with limited criteria for malignancy and without metastasis.
Herein, we report a case of a 48-year-old Thai male with a large painful mass in his axilla for one year without apparent neurological deficit. Magnetic resonance imaging showed a large heterogeneous mass encasing entire posterior cord of left brachial plexus and axillary artery. The tumor tissue from core needle biopsy histologically demonstrated the sheets and cords of relatively uniform tumor cells with foamy cytoplasm and round to oval hyperchromatic nuclei without atypia. The mitotic count was 0 per 50 high power field. A final diagnosis of glomus tumor of uncertain malignant potential was rendered. Complete surgical resection was performed, followed by adjuvant radiation due to positive margin. Neither local recurrence nor distant metastasis was observed at 2-year follow up. Unfortunately, postoperative incomplete brachial plexopathy without signs of re-innervation by electromyography was persisted. Later nerve grafting reconstruction was performed, followed by ongoing neurological rehabilitation.
Glomus tumor of uncertain malignant potential is exceedingly rare, especially around brachial plexus. Although the prognosis is good, careful histological diagnosis and treatment are needed to achieve an optimal outcome with lower morbidity.
Core tip: Atypical glomus tumors are a group of sporadic glomus tumors exhibit unusual characteristics of malignancy. The glomus tumor of uncertain malignant potential is defined as atypical glomus tumor with at least one, but not all, malignant feature. Moreover, atypical glomus tumor around the nerve region is exceedingly rare and mimic various types of sarcoma, leading to inaccurate diagnosis and inappropriate treatment. Careful histologic diagnosis and a multidisciplinary approach are essential for better clinical outcome with less morbidity. In this report, we present a patient with an extensive glomus tumor of uncertain malignant potential in brachial plexus.
- Citation: Thanindratarn P, Chobpenthai T, Phorkhar T, Nelson SD. Glomus tumor of uncertain malignant potential of the brachial plexus: A case report. World J Clin Cases 2019; 7(18): 2815-2822
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2815.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2815
Glomus tumors are mesenchymal neoplasms arising from the cells of glomus bodies - the arteriovenous anastomoses functioning to regulate the temperature by controlling the peripheral blood flow[1,2]. Glomus tumors are rare, with an estimated incidence of 1%-2% of soft tissue tumors of the extremities[1,2]. Glomus tumors are typically found within the dermis or soft tissue of the extremity, especially the subungual region, but may also be found at other sites including nerves[1-3]. The majority of these tumors are benign; however, some may show unusual clinical characteristics with more aggressive histological features[4]. According to World Health Organization (WHO), atypical glomus tumors were categorized as malignant glomus tumor, symplastic glomus tumor, and glomus tumor of uncertain malignant potential (GT-UMP)[2]. We present a case of the 48-year-old patient with large GT-UMP involving the posterior cord of his left brachial plexus.
A 48-year-old right-handed Thai male patient presented to our hospital with a large solid, painful lump in his left axillary region.
The mass was noticed by the patient himself one year ago, with rapidly progressed in sized during the six months prior to presentation. The pain gradually increased in intensity despite the treatment with painkillers, without cold hypersensitivity or neurological deficit around this area.
The patient had no previous underlying disease.
A personal or family history of benign or malignant tumors did not exist.
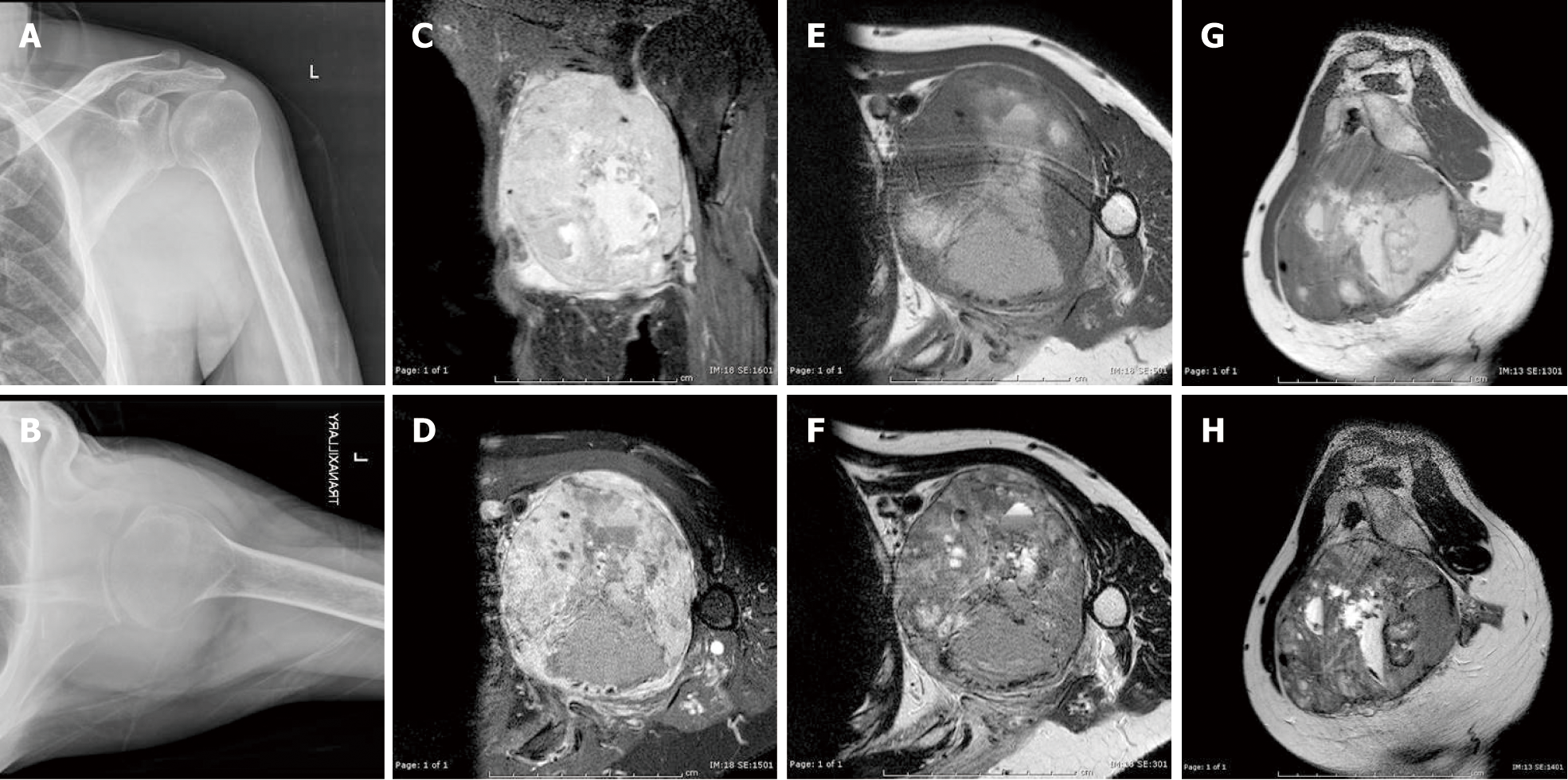
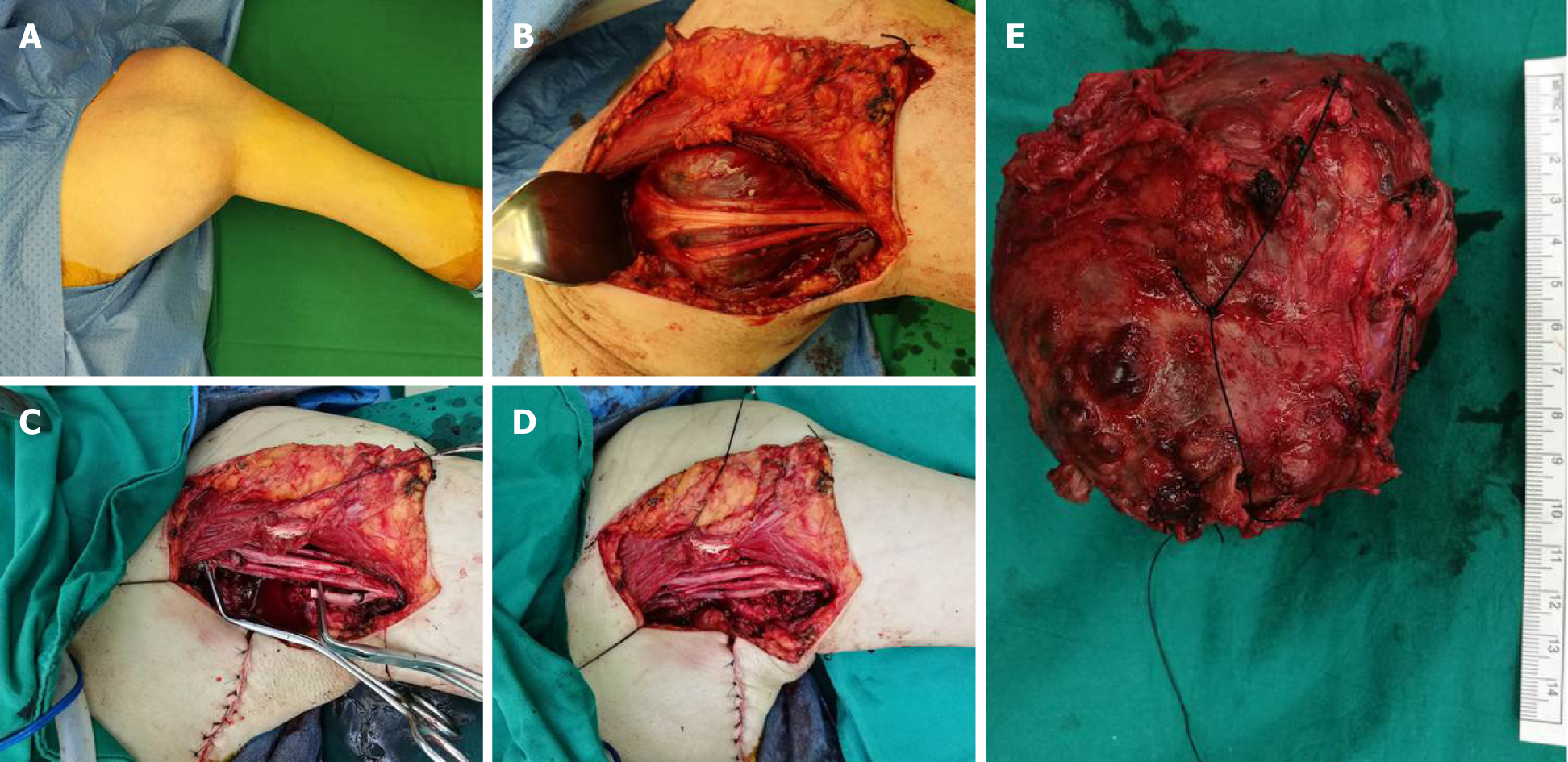
On the physical examination, a large solid, soft tissue mass in his left axillary region was observed (Figure 1). The mass elicited mild tenderness by palpation test without pulsatile sensation. Tinel’s sign was negative. No neurological deficit was observed; however, the patient had limited range of motion of his left shoulder due to pain.
Laboratory examination showed a white blood cell count of 7280/μL, with 62% of neutrophils, hemoglobin of 14.1 g/dL, platelets of 247300/mm3, erythrocyte sedimentation rate 15 mm/h, lactic dehydrogenase 150 U/L, and normal range of electrolyte profile. Besides, the human immunodeficiency virus antibody test was negative.
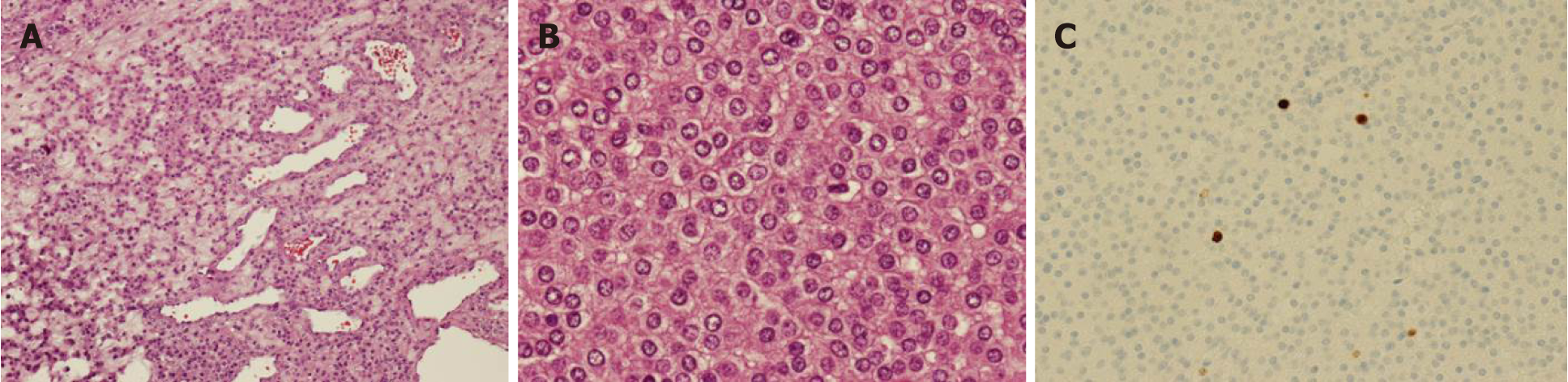
A core needle biopsy was performed. Histologically, the tumor was composed of sheets and cords of relatively uniform tumor cells with moderate amounts of foamy, lightly eosinophilic cytoplasm and round to oval mildly hyperchromatic nuclei without atypia (Figure 2). Immunohistochemical studies revealed the tumor cells to be positive for smooth muscle actin, vimentin and collagen type IV, and negative for S100, AE1/AE3, CD34, GCDFP-15, chromogranin, and synaptophysin. The overall features were felt to be consistent with glomus tumor.
Plain radiography revealed soft tissue shadow around his left axillar. Magnetic resonance imaging (MRI) demonstrated a 9.6 cm × 11.2 cm × 9.8 cm heterogeneous contrast-enhancing mass bulging from the posterior cord of the brachial plexus and encasing the axillary artery and vein associated with vascular invasion, compatible with a malignant soft tissue tumor with a differential diagnosis including undifferentiated pleomorphic sarcoma, malignant peripheral nerve sheath tumor, or lymphoma (Figure 3). Furthermore, the pre-operative chest computerized tomography displayed a 3-mm nodule at the posterior basal segment of the right lower lung.
Hence, because of the size of the tumor without atypia or mitotic activity, the patient was diagnosed with atypical glomus tumor, consistent with GT-UMP.
Management of this patient was discussed at Chulabhorn hospital multidisciplinary tumor board. Complete resection of the tumor, along with an abutted segment of axillary artery, and reconstruction with saphenous vein graft was subsequently performed (Figure 4).
Histologic examination and immunohistochemical analysis of the resected specimen demonstrated the same results seen in the core needle biopsy. The mitotic count was 0 per 50 high power field (HPF), and Ki-67 expression by tumor cells was less than 0%-5%. Possible vascular tumor emboli were present. The final diagnosis was GT-UMP. Because of positive surgical margins and aggressive behavior of the tumor, adjuvant 50-Gray radiation, 25 fractions, was administered to the site. Neither local recurrence nor distant metastasis was observed at 2-year follow up.
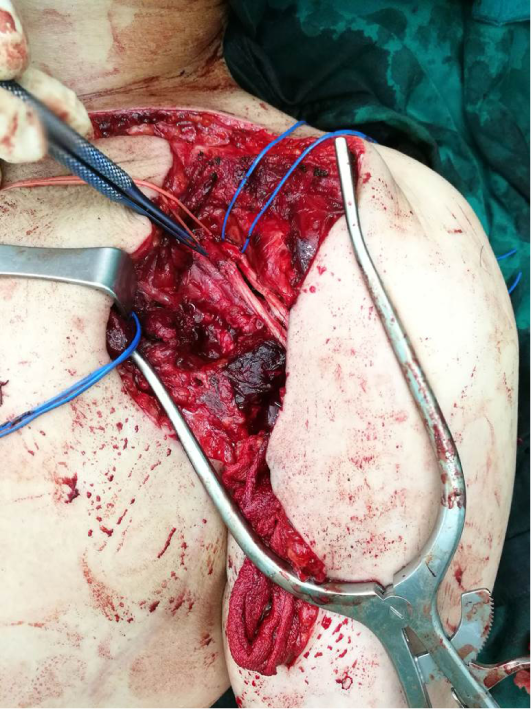
Unfortunately, postoperative incomplete total-arm-type brachial plexopathy persisted. The shoulder range of motion was 70o forward flexion, 70o abduction, 15o internal rotation, and 15o external rotation. Motor power was observed 1+ around the shoulder, 1+ of elbow extension but 3+ of elbow flexion. Left wrist and finger flexion were grade 2+ with no active extension. The sensory decreased to grade 1 from triceps area down to dorsum of fingers. Deep tendon reflexes of the whole affected arm decreased to 1+. There was no sign of re-innervation by electromyographic studies at 3- and 6-mo follow up. Second stage sural nerve grafting to the radial and axillary nerve was performed, along with neurologic rehabilitation to regain triceps tone and function (Figure 5).
Glomus tumors are mesenchymal neoplasms composed of modified perivascular cells that resemble the normal glomus bodies, which regulate temperature by controlling peripheral blood flow[1,2]. The classical presentation of a glomus tumor is characterized by a triad of symptoms including pain, pinpoint tenderness with blunt palpation, and cold hypersensitivity[1,2]. Glomus tumors mostly occur in middle age patients, especially in the fourth decades of life[1,2]; however, they have been described in all age groups. Although no clear sex predilection has been reported for glomus tumors in general, subungual glomus tumors appear to be more common in women[1,2]. While the majority of glomus tumors occur in the subungual region of the finger, they can occur anywhere in the body. Extra-digital cases account for 34%-61% of all glomus tumors, including the wrist, forearm, and foot[3,5]. Unusual sites such as tendons, bone, nerve, gastrointestinal tract, kidney, bladder, lung, and mediastinum have also been reported[3,6-12]. Congenital, familial, and multiple lesions are sporadic[1,2,13].
Most glomus tumors are small, benign neoplasms that occur in the dermis or subcutis of the extremities. However, occasional glomus tumors may show unusual clinical features, such as large size, deep soft tissue or visceral location, infiltrative growth pattern, or multicentricity. Folpe et al[4] studied a large number of glomus tumors having one or more atypical features. Combining the features of large size (more than 2 cm), deep location, necrosis, mitotic activity of more than 5 mitoses/50 HPF, and the combination of high nuclear grade and high mitotic activity, they proposed an empirically useful classification of glomus tumors with atypical features. Currently, more evidence has shown that most of the large and deeply located glomus tumors behave in a clinically benign fashion; hence, the first diagnostic criterion was modified, comparatively shown in Table 1[1,2]. The differential diagnosis of atypical glomus tumor is broad, and to some extent site dependent, as shown in Table 2[4]. Immunohistochemical studies are therefore essential in differentiating between possible diagnostic entities[4]. In our case, the tumor measured 11 cm in maximal diameter but displayed neither mitotic activity nor nuclear atypia.
| Atypical glomus tumors | WHO 4th edition (2013) | Enzinger and Weiss’s Soft Tissue Tumors. 6th edition (2014) |
| Malignant glomus tumor | (1) Marked nuclear atypia and any level of mitotic activity; or (2) Atypical mitotic figures | (1) Marked atypia + mitotic activity (> 5/50 HPF); or (2) Atypical mitotic figures |
| Glomus tumors of uncertain malignant potential | Not fulfilling criteria for malignancy, but having at least one atypical feature other than nuclear pleomorphism | (1) Superficial location + mitotic activity (> 5/50 HPF); or (2) Large size (> 2 cm) and/or deep location |
| Symplastic glomus tumor | Striking nuclear atypia in the absence of any other features indicative of negative outcome (e.g., large size, deep location, mitotic activity, necrosis) | Lack criteria for malignant glomus tumor and marked nuclear atypia only |
| Superficial lesion | Deep lesion |
| Merkel cell carcinoma | Hemangiopericytoma |
| Eccrine spiradenoma | Leiomyosarcoma with epithelioid change |
| Melanoma | Rhabdomyosarcoma |
| Ewing sarcoma/PNET | Ewing sarcoma/PNET |
| Neuroblastoma |
Glomus tumor of the peripheral nerves is uncommon, and GT-UMP of the nerve is extremely rare. Until now, only one case of intraneural GT-UMP in the median nerve has been reported[8]. Complete resection of the tumor is the treatment of choice, although this may be associated with high morbidity. Chemotherapy and radiation are generally not indicated. However, a case of a patient with malignant glomus tumor with BRAF mutation treated with dabrafenib, the oral RAF inhibitor has been reported[9]. The patient experienced no pain, and extremity function was preserved with minimal toxicity. Moreover, MRI demonstrated a decrease in tumor size at 2-wk, 3- and 6-mo follow up after initiating treatment[9]. In our case, the clinical presentation, radiographic features, and intra-operative findings were indicative of aggressiveness. Extensive resection, followed by postoperative radiation, was therefore chosen to achieve an oncologic outcome. To date, the prognosis of GT-UMP has been excellent, with no reports of metastases. However, the number of cases is small and the follow-up time is short.
We report a sporadic case of glomus tumor of uncertain malignant potential of the brachial plexus, which should be considered in the differential diagnosis of atypical glomus tumors. Careful histological examination and immunohistochemical studies to confirm the diagnosis are necessary. A multidisciplinary approach is needed to achieve a clinical outcome with minimal morbidity. Although the prognosis of glomus tumor of uncertain malignant potential is good with surgical resection, the optimal treatment remains unclear.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Senol MG S-Editor: Dou Y L-Editor: A E-Editor: Liu JH
| 1. | Goldblum JR, Folpe AL, Weiss SW. Perivascular tumors. Enzinger and Weiss's Soft Tissue Tumors. Elsevier: Philadelphia, USA 2014; 749-765. [Cited in This Article: ] |
| 2. | Folpe AL, Brems H, Legius E. Glomus tumours. In: Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, editors. World Health Organization Classification of Tumours WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. IARC; Lyon, France 2013; 116-117. [Cited in This Article: ] |
| 3. | Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81:1337-1344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 154] [Cited by in F6Publishing: 163] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 4. | Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25:1-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 405] [Cited by in F6Publishing: 368] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 5. | Chou T, Pan SC, Shieh SJ, Lee JW, Chiu HY, Ho CL. Glomus Tumor: Twenty-Year Experience and Literature Review. Ann Plast Surg. 2016;76 Suppl 1:S35-S40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Sachdev R, Mohapatra I, Goel S, Gajendra S. Intra-Articular Glomus Tumor- A Rare Presentation. Turk Patoloji Derg. 2017;33:175-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Gombos Z, Fogt F, Zhang PJ. Intraosseous glomus tumor of the great toe: a case report with review of the literature. J Foot Ankle Surg. 2008;47:299-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Dahlin LB, Scherman P, Besjakov J, Lindberg E, Solomon DA, Horvai AE, Perry A. Intraneural glomus tumor of "uncertain malignant potential" and with BRAF mutation in the median nerve - an unusual case. Clin Neuropathol. 2017;36:164-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Cuviello A, Goyal A, Zick A, Ahlawat S, Rodriguez FJ, Belzberg AJ, Pratilas CA. Sporadic Malignant Glomus Tumor of the Brachial Plexus With Response to Targeted Therapy Directed Against Oncogenic BRAF. JCO Precis Oncol. 2018;2018. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Gill J, Van Vliet C. Infiltrating glomus tumor of uncertain malignant potential arising in the kidney. Hum Pathol. 2010;41:145-149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Oide T, Yasufuku K, Shibuya K, Yoshino I, Nakatani Y, Hiroshima K. Primary pulmonary glomus tumor of uncertain malignant potential: A case report with literature review focusing on current concepts of malignancy grade estimation. Respir Med Case Rep. 2016;19:143-149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Miettinen M, Paal E, Lasota J, Sobin LH. Gastrointestinal glomus tumors: a clinicopathologic, immunohistochemical, and molecular genetic study of 32 cases. Am J Surg Pathol. 2002;26:301-311. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 229] [Cited by in F6Publishing: 196] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 13. | Chatterjee JS, Youssef AH, Brown RM, Nishikawa H. Congenital nodular multiple glomangioma: a case report. J Clin Pathol. 2005;58:102-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |