Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2760
Peer-review started: January 31, 2019
First decision: May 31, 2019
Revised: July 4, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 26, 2019
Prior studies indicate that doing breathing exercises improves physical performance and quality of life (QoL) in heart failure patients. However, these effects remain unclear and contradictory.
To determine the effects of machine-assisted and non-machine-assisted respiratory training on physical performance and QoL in heart failure patients.
This was a systematic review and network meta-analysis study. A literature search of electronic databases was conducted for randomized controlled trials (RCTs) on heart failure. Respiratory training interventions were grouped as seven categories: IMT_Pn (inspiratory muscle training without pressure or < 10% maximal inspiratory pressure, MIP), IMT_Pl (inspiratory muscle training with low pressure, 10%-15% MIP), IMT_Pm (inspiratory muscle training with medium pressure, 30%-40% MIP), IMT_Ph (inspiratory muscle training with high pressure, 60% MIP or MIP plus aerobics), Aerobics (aerobic exercise or weight training), Qi_Ex (tai chi, yoga, and breathing exercise), and none. The four outcomes were heart rate, peak oxygen uptake (VO2 peak), 6-min walking distance test (6MWT), and Minnesota Living with Heart Failure QoL. The random-effects model, side-splitting model, and the surface under the cumulative ranking curve (SUCRA) were used to test and analyze the data.
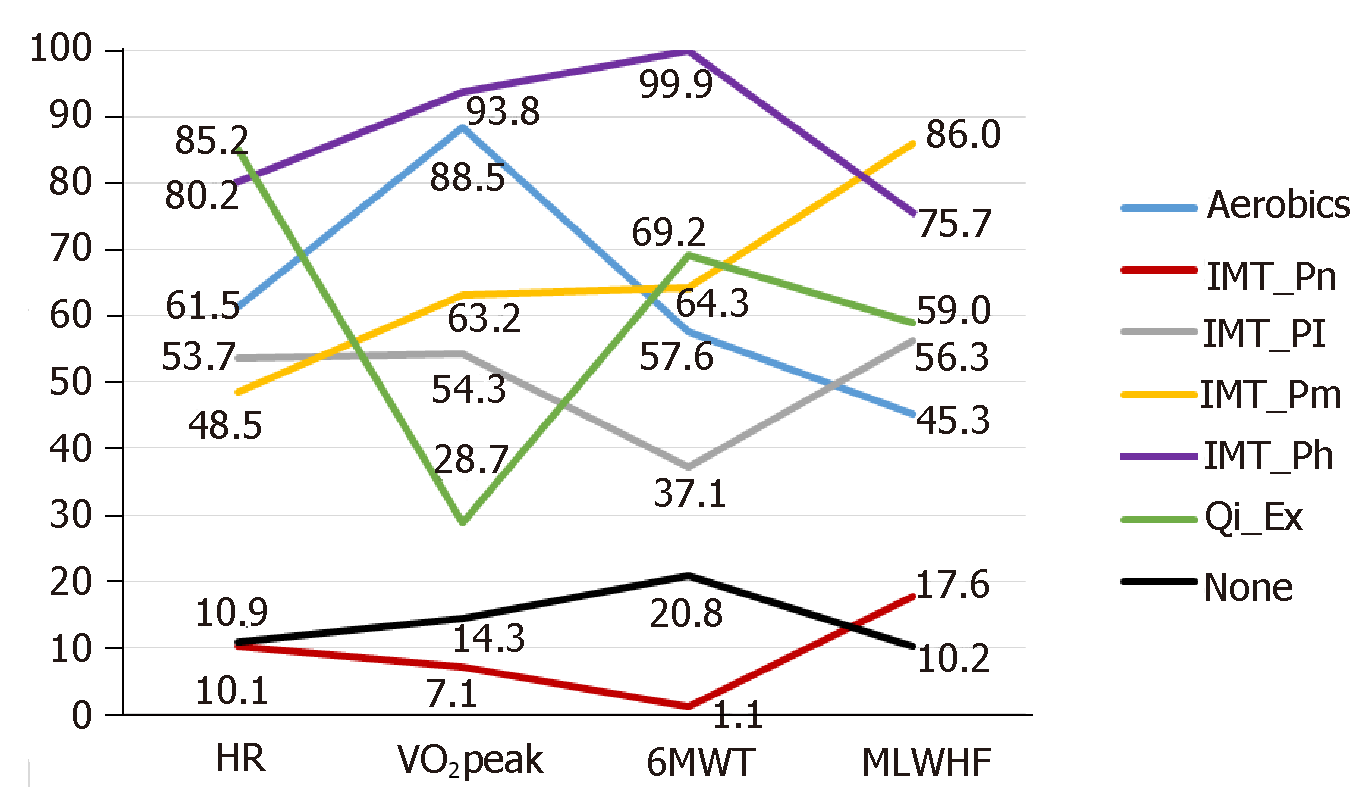
A total of 1499 subjects from 31 RCT studies were included. IMT_Ph had the highest effect sizes for VO2 peak and 6MWT, IMT_Pm highest for QoL, and Qi_Ex highest for heart rate. Aerobics had the second highest for VO2 peak, Qi_Ex second highest for 6MWT, and IMT_Ph second highest for heart rate and QoL.
This study supports that high- and medium-intensity machine-assisted training improves exercise capacity and QoL in hospital-based heart failure patients. After hospital discharge, non-machine-assisted training continuously improves cardiac function.
Core tip: Breathing training interventions, including inspiratory muscle training, tai chi, yoga, and breathing exercises, are effective strategies for improving cardiac function, exercise capacity, and quality of life in heart failure patients. Machine-assisted respiratory training in hospital settings should be prioritized over respiratory training provided in non-hospital settings. Inspiratory muscle training with high pressure effectively improves cardiac function, and inspiratory muscle training with moderate pressure effectively improves quality of life in heart failure patients. In home settings, non-machine-assisted respiratory training such as tai chi, yoga, and breathing exercise effectively reduces (improves) heart rate in heart failure patients.
- Citation: Wang MH, Yeh ML. Respiratory training interventions improve health status of heart failure patients: A systematic review and network meta-analysis of randomized controlled trials. World J Clin Cases 2019; 7(18): 2760-2775
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2760.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2760
As societies age, the incidence of heart failure is estimated to increase to around 12%[1]. Furthermore, it is currently expected that around 8 million adults will be diagnosed with heart failure by 2030[2]. The estimated all-cause mortality rate for heart failure is 8% and 25% for 30-d and 1-year periods, respectively[3]. Moreover, elderly heart failure patients face high rates of comorbidities and hospital readmissions[4]. The annualized lifetime costs associated with heart failure have been estimated at $868-25532 per patient[5]. In light of the above, the diverse care needs of heart failure patients and the high societal costs associated with caring for this growing patient population are issues that will become increasingly important and that, eventually, must be addressed effectively.
Heart failure describes the condition in which a heart is no longer able to pump blood in quantities that are sufficient for the needs of the body. Heart rate is a measure used to assess the effect of heart failure treatments[6], because elevated resting heart rate is associated with reduced left ventricular ejection fraction (LVEF)[6] and increased relative risk of heart failure[7]. As reduced LVEF is known to cause symptoms of dyspnea and reduced exercise tolerance, both of which affect the normal physical performance of heart failure patients, care regimens for heart failure patients currently focus on improving symptoms, maintaining cardiac function, and reducing mortality and morbidity[8]. Furthermore, an additional area of concern is the negative impact on quality of life (QoL) experienced by heart failure patients due to reduced regular activity[9,10].
Current clinical guidelines recommend condition-appropriate exercises as a complementary therapy for heart failure patients in addition to regular pharmacological treatment[8,11]. For example, respiratory muscle training has been shown to effectively improve dyspnea-related low-exercise tolerance in heart failure patients[12]. Respiratory muscle training interventions include machine-assisted respiratory training such as inspiratory muscle training (IMT) and non-machine-assisted respiratory training such as breathing exercises[13]. In hospital settings, machine-assisted respiratory training helps heart failure patients adjust their maximal inspiratory pressure (MIP), which is an important factor in improving inspiratory muscle strength, walking distance, and dyspnea[14]. A prior systematic literature review found IMT to effectively improve exercise capacity in heart failure patients, as measured using the 6-minute walking distance test (6MWT)[15]. Moreover, when performed at higher intensities, IMT not only improved 6MWT scores but also improved peak oxygen uptake (VO2 peak) in these patients[16]. However, as IMT requires using facilities and equipment that are nearly exclusively available in hospitals, continuing to perform IMT after hospital discharge is difficult for most heart failure patients.
Breathing exercises, representing the largest group of non-machine-assisted respiratory training, include tai chi, yoga, and other similar practices. These breathing exercises, which are suited to either hospital or non-hospital settings, have been shown to reduce the risk factors of cardiovascular disease using breathing modification and relaxation techniques[17,18]. Prior studies of heart failure patients have found that practicing tai chi improved heart rate, exercise capacity, and QoL and that practicing mind-body interventions (tai chi, yoga, and meditation) had small-to-moderate, positive effects on exercise capacity and QoL[17,19]. However, the change in effect of performing these exercises at different levels of intensity remains to be fully considered and scientifically demonstrated. One meta-analysis found no significant improvement in VO2 peak or QoL in individuals performing high-intensity interval training in comparison to their peers who were performing moderate-intensity continuous exercise training[20]. However, another meta-analysis found that high-intensity interval training improved the VO2 peak[21] of heart failure patients and that this improvement was effective only when training was maintained for at least 12 wk[21].
Heart rate[6] and LVEF[8,11] are important indicators of cardiac function. Cardiac function is affected by exercise capacity, which is generally assessed using 6MWT[22] and VO2 peak[23] scores. While VO2 peak must be measured in hospital facilities, rough measurements of 6MWT may be taken in non-hospital settings and used to represent exercise capacity[24]. In addition, the relationship between QoL and cardiac event-free survival is affected by status of functional performance[25]. The Minnesota Living With Heart Failure questionnaire (MLWHFQ), which is used widely in clinical settings to assess QoL in heart failure patients[26], is an important indicator of survival after discharge[27].
Evidence-based support for the efficacy of supplemental therapies for heart failure is currently limited and conflicting. Most research analysis to date has focused on pairwise comparisons of exercise effects, such as IMT vs aerobic exercises and IMT vs breathing exercises, and the respective effects of IMT regimens at different levels of intensity. Thus, clinical data on supplemental therapies for heart failure patients is inadequate. Network meta-analysis allows for indirect inference of comparisons that have never been made in individual studies, and allows the ranking of interventions based on their effects[28]. Therefore, this systematic review and network meta-analysis study aimed to determine the effect of respiratory training interventions on physical performance and QoL in patients with heart failure. The comparative effects of machine-assisted respiratory training and non-machine-assisted respiratory training were analyzed in terms of heart rate, LVEF, VO2 peak, 6MWT, and QoL.
Ten online databases were searched for this study, including Medline, PudMed, EBSCO (Academic Search Complete and CINAHL), SPORTDiscus with full text, EMBASE, Cochrane Library, Airiti Library, National Digital Library of Theses and Dissertations in Taiwan (NDLTD), China National Knowledge Infrastructure, China Journal Full-text Database, and China Doctoral Dissertations and Master's Theses Full-text Database. Text words and medical subject headings (MeSH) terms were used to search all studies published up to April 2018. The Boolean operator was used to search related terms, including “heart failure”, “respiratory training”, and “randomized”. In addition, unpublished articles (gray literature) were searched manually.
Criteria for inclusion were original research articles that: (1) Used a randomized controlled trial (RCT) approach; (2) Used adult patients with heart failure as the sample population; (3) Implemented one or more respiratory training interventions (e.g., inspiratory muscle training, tai chi, yoga, breathing exercise, and aerobic exercise); and (4) Examined outcomes, including cardiac function (heart rate and LVEF), exercise capacity (VO2 peak and 6MWT), and QoL (O). Only papers written in English or Chinese were considered for inclusion.
The Cochrane risk of bias assessment tool was used to appraise the selected articles. Two expert reviewers (CL and MH) with at least 15 years of clinical nursing experience and with experience in empirical research evaluated the selected articles independently. Any difference in appraisal recommendation between the two reviewers was resolved by a third reviewer (ML).
Heart rate and LVEF were used to assess cardiac function, VO2 peak and 6MWT were used to assess physical capacity, and the MLWHFQ was used to measure QoL.
Review Manager Software (RevMan 5.3; Cochrane Collaboration, Oxford, United Kingdom) and STATA (Stata corporation, Texas) were used to analyze the pooled data. Standard mean difference (SMD) and 95% confidence interval (CI) were used to represent the intervention effect. A random-effects model was used to pool each treatment effect due to the clinically diverse nature of the 31 included RCT studies. Moreover, a forest plot was used to summarize the intervention effects, heterogeneity was examined using the χ2 test with the Cochrane’s Q and I2 statistics[28,29], and publication bias was assessed using funnel plot and Egger’s test. Furthermore, Bayesian meta-analytical techniques were used to perform network meta-analysis in order to synthesize the direct and indirect evidence that was generated by the included studies[28,30]. Finally, the surface under the cumulative ranking curve (SUCRA) provided a numeric presentation of the overall ranking (range: 0%-100%) of each treatment, with a higher SUCRA value indicating a higher likelihood that a treatment is at or near the top rank[28,31].
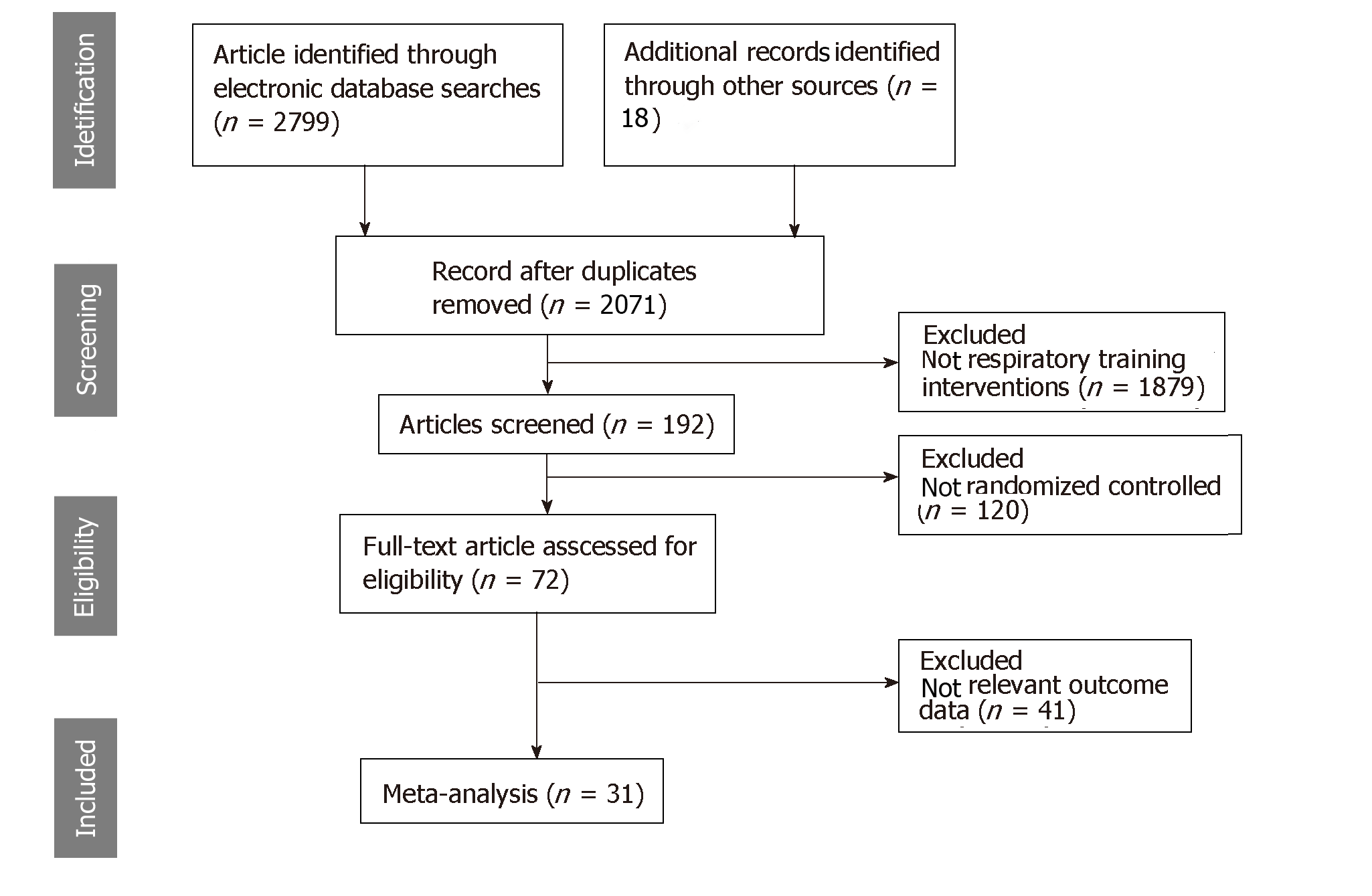
Figure 1 shows the flowchart of the study selection process. A total of 2817 studies met the search criteria. Of these, 746 were eliminated as duplicates and 1879 were eliminated due to poor fit with the topic of this research. Next, after reviewing the title and abstract of the remaining 192 articles, a further 120 were eliminated due to their use of other research designs. The expert reviewers read the entire texts of the remaining articles and employed the inclusion and exclusion criteria to identify a final set of 31 RCT studies.
Table 1 shows the characteristics of the 1499 participants in the 31 RCT studies that were included in the analysis. The 1006 males (67.1%) averaged 60.2 years of age and the 493 females (32.9%) averaged 61.3 years of age. In terms of NYHA class, the largest number of studies (11 RCTs; 35.5%)[32-42] targeted NYHA class II-III patients and the second largest number (5 RCTs; 16.1%)[43-47] targeted NYHA class I-III patients. The duration of the respiratory training interventions in the 31 RCT studies ranged between 4 wk and 24 wk, with the largest number (15 RCTs, 48.4%)[18,32,38,40,42,45-54] lasting for 12 wk, followed by 5 RCTs (16.1%) with interventions that lasted for 8 wk[34,43,44,55,56] and 10 wk[35-37,41,57], respectively.
| First author (year) | Group (n), age (mean ± SD) | Male/ female | NYHAclass | Attrition rate, % | Experimental group (E) | Control group (C) | Duration (wk) | Outcomes |
| Adamopoulos 2014 | E: 21, 57.8 ± 11.7 C: 22, 58.3 ± 13.2 | 19/2 17/5 | II-III | 17.3 | IMT computer type, 60% MIP, 30 min/time, 7 d/wk, hospital Aerobic exercise, 20-45 min/d, 3d/wk, home | Sham IMT, 10% MIP Aerobic exercise | 12 | HR, LVEF, VO2 peak, 6MWT, MLWHFQ score |
| Bosnak-Guclu 2011 | E: 16, 69.5 ± 8 C: 14, 65.7 ± 10.5 | 12/4 12/2 | II-III | 16.6 | IMT threshold type, 40% MIP, 30 min/time, 7 d/wk | Sham IMT, 15% MIP | 6 | HR, VO2 peak, 6MWT |
| Caminitu 2011 | E: 30, 74.1 ± 6 C: 30, 73.4 ± 2 | 25/5 26/4 | II | 0 | Tai chi, 10 movements, 30 mim/time, 2 d/wk, home ET with cycling or walking 30 mim/time, 2 d/wk, home | Endurance training with cycling or walking, 30 min/time, 4 d/wk, home | 12 | HR, VO2 peak, 6MWT |
| Chen 2015 | E: 42, 62.1 ± 4.1 C: 42, 62.9 ± 5.0 | 32/10 34/8 | I-IV | 0 | Deep breathing, 20 repeats/3 times/d, inspiratory 2 s, expiratory > 6 s, deep breathing stop 10-28 s | Usual care | 8 | HR, LVEF, 6MWT |
| Chen 2017 | E: 39, 71.44 ± 13.65 C: 41, 69.08 ± 13.48 | 18/21 24/17 | I-II | 21.5 | Baduanjin, 35 min/time, 3 d/wk | Usual care | 12 | MLWHFQ score |
| Dall'Ago 2006 | E: 16, 54 ± 3 C: 16, 58 ± 2 | 10/6 11/5 | NA | 27.3 | IMT threshold type, 30% MIP, 30 min/time, 7 d/wk | Sham IMT, 0% MIP | 12 | VO2 peak, 6MWT, MLWHFQ score |
| Ekman 2011 | E: 30, 73 ± 11 C: 35, 73 ± 10 | 22/8 24/11 | II-IV | 9.7 | Device-guided paced breathing, 20 min/time, 2 times/d | CD player with earphones, 20 min/time, 2 times/d | 4 | HR |
| Hägglund 2017 | E: 20, 64.1 ± 9.4 C: 20, 65.7 ± 8.5 | 15/5 11/9 | I-III | 25 | Yoga, 60 min/time, 2 times/wk, hospital | Hydrotherapy, 45 min/time, 2 times/wk, hospital | 12 | HR, 6MWT |
| Kawauchi 2017 | E1: 13, 56 ± 7 E2: 13, 54 ± 10 C: 9, 56 ± 7 | 8/5 6/7 5/4 | II-III | 33.9 | E1: IMT computer type, 30% MIP, peripheral muscle training, 7 d/wk. E2: IMT computer type, 15% MIP, 7 d/wk, hospital | Usual care | 8 | 6MWT, MLWHFQ score |
| Krishna 2014 | E: 44, 49.34 ± 5.70 C: 48, 50.14 ± 4.54 | 32/12 32/16 | I-II | 29 | Yoga, asanas and pranayama style, 60 min/time, 3 d/wk | Drug therapy | 12 | HR, LVEF, 6MWT, MLWHFQ score |
| Laoutaris 2004 | E: 20, 57.6 ± 2.3 C: 15, 60.0 ± 2.6 | 18/2 13/2 | II-III | 5.7 | IMT computer type, 60% MIP, 3 d/wk, hospital | Sham IMT, 15% MIP | 10 | HR, LVEF, VO2 peak, 6MWT, MLWHFQ score |
| Laoutaris 2007 | E: 15, 53.0 ± 2.0 C: 23, 59.0 ± 2.0 | 12/3 20/3 | II-III | 0 | IMT computer type, 60% MIP, 3 d/wk, hospital | Sham IMT, 15% MIP | 10 | HR, VO2 peak, 6MWT |
| Laoutaris 2008 | E: 14, 53.4 ± 2.1 C: 9, 57.3 ± 4.0 | 11/3 9/0 | II-III | 0 | IMT computer type, 60% MIP, 3 d/wk, hospital | Sham IMT, 15% MIP | 10 | HR, VO2 peak |
| Laoutaris 2011 | E: 10, 37.2 ± 17.7 C: 5, 41.8 ± 14.6 | 10/0 4/1 | Not reported | 28.5 | IMT computer type, 60% MIP, 2-3 d/wk, hospital Resisted training 45 min/time, 3-5 times/wk, home Aerobic bike or treadmill walk, 30-45 min/d, home | Walk, 30-45 min/d | 10 | VO2 peak, 6MWT, MLWHFQ score |
| Laoutaris 2013 | E: 13, 57.1 ± 11 C: 14, 58.6 ± 8 | 10/3 12/2 | II-III | 3.6 | IMT computer type, 60% MIP, 20 min/time, 3 d/wk, hospital Aerobic bike, 20-30 min/d, home Resisted training 1 RM 15min | Aerobic exercise bike 45-55 min/time, 3 d/wk, hospital | 12 | HR, VO2 peak, 6MWT, MLWHFQ score |
| Lin 2011 | E: 40, 56.8 ± 16.2 C: 40, 57.5 ± 16.2 | 26/14 24/16 | II-IV | 16.3 | Deep breathing, 20 repeats/3 times/d, inspiratory 2 s, expiratory 10 s, deep breathing stop 2-10 s, hospital | Drug therapy, diet counseling | Discharge | HR, 6MWT |
| Martinez 2001 | E: 11, 60 ± 14 C: 9, 57 ± 13 | 16/4 | II-III | Not reported | IMT threshold type, 30% MIP, 15 mins/time, 6 d/wk | Sham IMT, 10% MIP | 6 | VO2 peak, 6MWT |
| Mello 2012 | E: 15, 54.3 ± 2 C: 12, 53.3 ± 2 | 9/6 5/7 | II | 5.4 | IMT threshold type, 30% MIP, 10 min/time, 3 times/d, 7 d/wk | No intervention | 12 | VO2 peak, MLWHFQ score |
| Palau 2014 | E: 14, 68 ± 4.62 C: 12, 74 ± 1.19 | 7/7 6/6 | III-IV | 3.7 | IMT threshold type, 30% MIP, 20 min /time, 2 times/d | Usual care | 12 | VO2 peak, 6MWT, MLWHFQ score |
| Pan 2017 | E: 42, 65.2 ± 5.9 C: 42, 67.2 ± 6.4 | 28/14 29/13 | II-III | 0 | Fast inhalation (0.8-1 s) and slow exhalation (4 s), 10 min/time, 6 times/d (hospital), 3 times/d (home) | Usual care | 12 | HR, 6MWT |
| Parati 2008 | E: 12, 64 ± 9 C: 12, 62.8 ± 10 | 9/3 9/3 | II-III | 0 | Device-guided paced breathing, 18 min/time, 2 times/d | Conventional treatment | 10 | LVEF, VO2 peak, MLWHFQ score |
| Pullen 2008 | E: 9, 52.1 ± 3.3 C: 10, 50.5 ± 12.8 | 2/7 7/3 | I-III | 0 | Yoga, hatha style, 70 min/time, 3d/wk | Drug therapy Education | 8 | VO2 peak, MLWHFQ score |
| Pullen 2010 | E: 21, 55.8 ± 7.6 C: 19, 52.5 ± 12.7 | 10/11 13/6 | I-III | 15 | Yoga, hatha style, 60 min/time, 3 d/wk | Drug therapy Education | 8 | VO2 peak, MLWHFQ score |
| Seo 2016 | E: 18, 55.8 ± 7.6 C: 18, 55.8 ± 7.6 | 25/11 | II-IV | 19.4 | CD-guided diaphragmatic breathing retraining, 15 min/time, 2 times/d, 5 d/wk, home | Education | 8 | 6MWT |
| Winkelmann 2009 | E: 12, 54 ± 12 C: 12, 59 ± 9 | 7/5 4/8 | Not reported | 36.8 | IMT threshold type, 30% MIP, 30 min/time, 7d/wk Aerobic braked cycle ergometer, 20-45 min/time, 3 d/wk | Aerobic braked cycle ergometer, 45 min/time, 3 d/wk | 12 | VO2 peak, 6MWT, MLWHFQ score |
| Yao 2010 | E: 80, 52.4 ± 6.32 C: 70, 51.7 ± 7.26 | 47/33 42/28 | II | 0 | Tai chi, 42 movements, ≥30 min/time, 5 d/wk | Drug therapy, diet and lifestyle counseling | 24 | LVEF, 6MWT, MLWHFQ score |
| Yeh 2004 | E: 15, 66 ± 12 C: 15, 61 ± 14 | 10/5 9/6 | I-IV | 10 | Tai chi, 5 movements, 60 min/time, 3 d/wk | Drug therapy, diet counseling, exercise advice | 12 | VO2 peak, 6MWT, MLWHFQ score |
| Yeh 2011 | E: 50, 68.1 ± 11.9 C: 50, 66.6 ± 12.1 | 28/22 36/14 | I-III | 9 | Tai chi, 5 movements, 60 min /time, 3 d/wk | Drug therapy, exercise advice Education 1 time/2 wk | 12 | VO2 peak, 6MWT, MLWHFQ score |
| Yeh 2013 | E: 8, 68 ± 11 C: 8, 63 ± 11 | 4/4 4/4 | I-III | 0 | Tai chi, 5 movements, 60 min/time, 3 d/wk | Aerobic exercise 60 min/time, 3 d/wk | 12 | HR, VO2 peak, 6MWT, MLWHFQ score |
| Zheng 2017 | E1: 9, 59.45 ± 7.20 E2: 8, 58.90 ± 8.60 C: 7, 59.10 ± 9.10 | 6/3 6/2 5/2 | II-III | 13.9 | E1. Qigong, 30-40 min/time/d E2. Walking, 30-40 min/time/d | Usual care | 12 | LVEF, 6MWT, MLWHFQ score |
| Zhong 2016 | E: 50, 63.5 C: 50, 66.2 | 31/19 28/22 | II-IV | 14 | Abdominal breathing (inspiratory: expiratory =1:1-2, 4 repeats/time), and leg exercise (5-8 min/time), 2 times/d | Usual care | Discharge | HR, 6MWT |
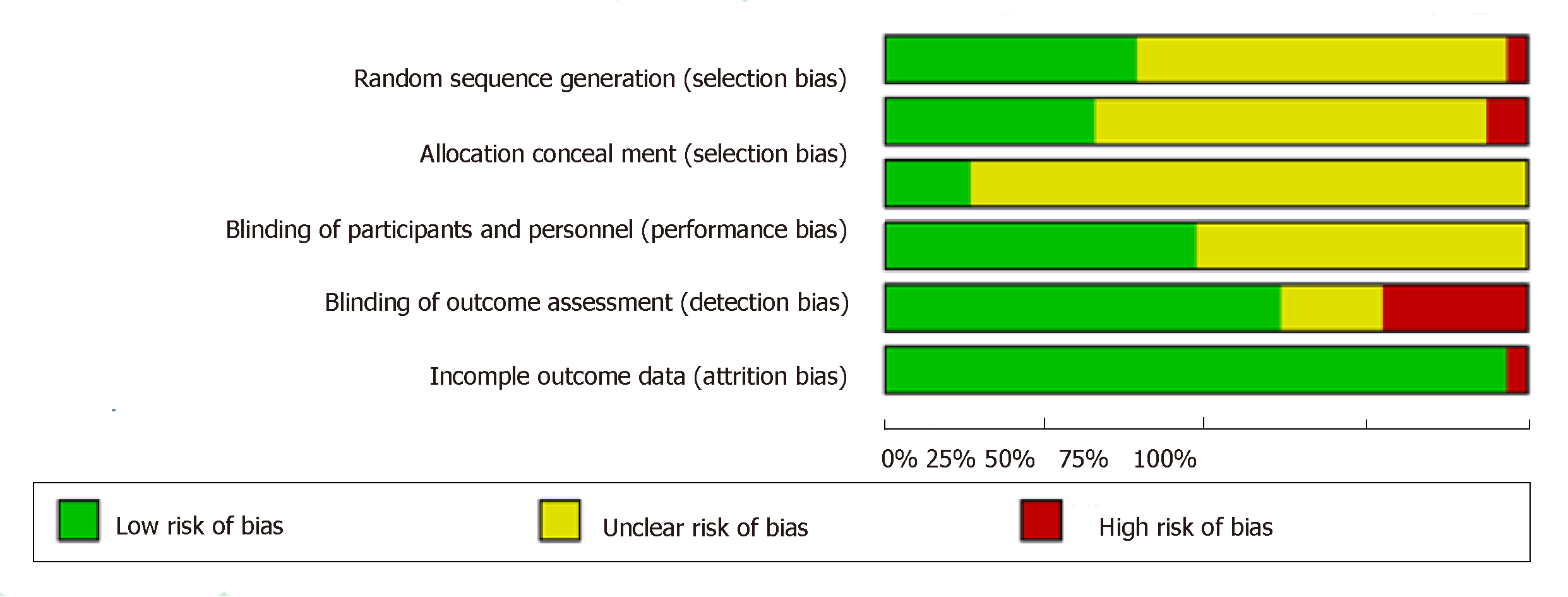
Figure 2 shows the result of the assessment of risk of bias. A total of 13 RCTs (41.9%)[18,33,34,42,45-47,49,54-58] described random sequence generation and 9 (29.0%)[18,33,38,39,47,49,51,54,57] described allocation concealment. With the regard to blinding, 4 RCTs (12.9%)[33,45,47,54] blinded the participants and 14 (45.2%)[18,33,36,37,41,43-45,50-54,57] blinded the data collectors. The average dropout rate of participants was 12%, with 7 RCTs reporting a rate in excess of 20%[18,34,47,49,50,53,57]. Finally, absence of publication bias was further assured by funnel plot and Egger’s test results for heart rate (P = 0.06), VO2 peak (P = 0.16), 6MWT (P = 0.20), and MLWHFQ score (P = 0.37), respectively.
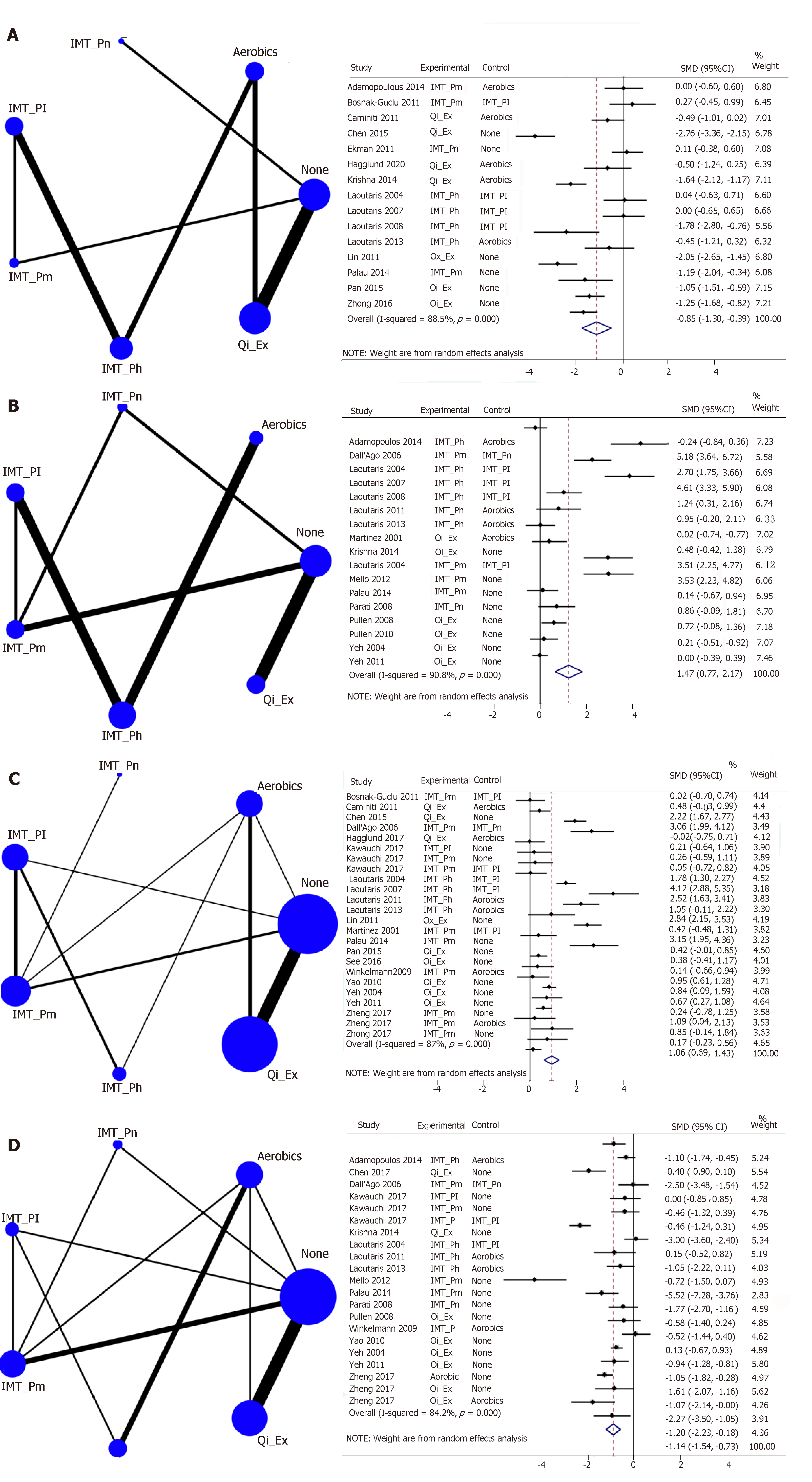
Figure 3 shows forest plots of respiratory training interventions on measure outcomes. The interventions from the included studies were grouped into seven categories, including IMT_Pn (inspiratory muscle training without pressure or < 10% MIP), IMT_Pl (inspiratory muscle training with low pressure, 10%-15% MIP), IMT_Pm (inspiratory muscle training with medium pressure, 30%-40% MIP), IMT_Ph (inspiratory muscle training with high pressure, 60% MIP or MIP plus aerobics), Qi_Ex (tai chi, yoga, or breathing exercise), Aerobics (aerobic exercise or weight training), and none (usual care, standard treatment, or education). A significant difference was found in overall intervention effect among these groups in terms of heart rate [SMD = -0.85, 95%CI: -1.30-(-0.39)], VO2 peak (SMD = 1.47, 95%CI: 0.77-2.17), 6MWT (SMD = 1.06, 95%CI: 0.69-1.43), and MLWHFQ score [SMD = -1.14, 95%CI: -1.54-(-0.73)]. After excluding one study (#29), the inconsistency did not exist in the design by treatment interaction models (heart rate, P = 0.71; VO2 peak, P = 0.22; 6MWT, P = 0.22; MLWHFQ, P = 0.27), and loop inconsistency (heart rate, P = 0.71; VO2 peak, P = 0.22; 6MWT, P = 0.51; MLWHFQ, P = 0.71). All of the results for the side-splitting model were insignificant (P > 0.05) with the exception of IMT_Pl vs IMT_Pm on 6MWT (P = 0.04). Although the direct and indirect effects of these two interventions differed (0.15 ± 0.49 and 3.28 ± 1.22, respectively), these differences were in the same direction. In addition, as tests for discordancy in the overall effect of LVEF (SMD = 0.28, 95%CI: -0.30-0.86) achieved statistical significance (P < 0.05), network analysis was not performed.
Figure 4 shows the SUCRA-based rankings of the respiratory training interventions. For heart rate, Qi_Ex had the highest likelihood of being ranked highest, followed by IMT_Ph and Aerobics. For VO2 peak, IMT_Ph had the highest likelihood of being ranked highest, followed by Aerobics and IMT_Pm. For 6MWT, IMT_Ph had the highest likelihood of being ranked highest, followed by Qi_Ex and IMT_Pm. Finally, for MLWHFQ score, IMT_Pm had the highest likelihood of being ranked highest, followed by IMT_Ph and Qi_Ex.
Table 2 shows the detailed intervention effect of the respiratory training interventions. In terms of heart rate, significant differences from usual care were found for Qi_Ex [SMD = -1.74, 95%CI: -2.26-(-1.23)], IMT_Ph [SMD = -1.58, 95%CI: -2.71-(-0.46)], and Aerobics [SMD = -1.31, 95%CI: -2.23-(-0.39)], respectively. Further, a significant difference in heart rate was found between Qi_Ex and IMT_Pn (SMD = 1.85, 95%CI: 0.58-3.13). In terms of VO2 peak, significant differences from usual care were found for IMT_Ph (SMD = 6.07, 95%CI: 3.80-8.35), Aerobics (SMD = 5.90, 95%CI: 3.43-8.36), IMT_Pm (SMD = 3.87, 95%CI: 2.68-5.07), and IMT_Pl (SMD = 3.37, 95%CI: 1.32-5.41), respectively. Further, the VO2 peak of IMT_Ph differed significantly from that of IMT_Pm [SMD = -2.20, 95%CI: -4.15-(-0.26)], IMT_Pl [SMD = -2.71, 95%CI: -3.72-(-1.69)], and IMT_Pn [SMD = -6.48, 95%CI: -8.93-(-4.03)]. In terms of 6MWT, significant differences from usual care were found for IMT_Ph (SMD = 3.19, 95%CI: 1.69-4.68), Qi_Ex (SMD = 1.17, 95%CI: 0.64-1.71), and Aerobics (SMD = 0.97, 95%CI: 0.03-1.92), respectively. Further, the 6MWT of IMT_Ph differed significantly from that of IMT_Pm [SMD = -2.10, 95%CI: -3.51-(-0.69)], IMT_Pl [SMD = -2.69, 95%CI: -3.89-(-1.49)], and IMT_Pn [SMD = -5.15, 95%CI: -7.56-(-2.75)]. In terms of MLWHFQ scores, significant differences from usual care were found for IMT_Pm [SMD = -2.10, 95%CI: -3.29-(-0.92)], IMT_Ph [SMD -1.79, 95%CI: -3.53-(-0.05)], and Qi_Ex [SMD = -1.42, 95%CI: -2.25-(-0.59)], respectively. Furthermore, a significant difference in MLWHFQ score was found between IMT_Pm and IMT_Pn [SMD = -2.00, 95%CI: -3.72-(-0.28)].
| None | Aerobics | IMT_Pn | IMT_Pl | IMT_Pm | IMT_Ph | Qi_Ex | ||
| Outcome of heart rate | ||||||||
| The outcomes of VO2 peak | None | - | -1.31 | 0.11 | -1.17 | -1.04 | -1.58 | -1.74 |
| (-2.23, -0.39) | (-1.06, 1.28) | (-2.36, 0.02) | (-2.16, 0.09) | (-2.71, -0.46) | (-2.26, -1.23) | |||
| Aerobics | -5.9 | - | 1.42 | 0.14 | 0.27 | -0.27 | -0.43 | |
| (-8.36, -3.43) | (-0.07, 2.91) | (-0.89, 1.16) | (-0.94, 1.49) | (-1.10, 0.56) | (-1.25, 0.38) | |||
| IMT_Pn | 0.41 | 6.31 | - | -1.28 | -1.15 | -1.69 | -1.85 | |
| (-0.96, 1.77) | (3.69, 8.93) | (-2.95, 0.39) | (-2.77, 0.47) | (-3.31, -0.07) | (-3.13, -0.58) | |||
| IMT_Pl | -3.37 | 2.53 | -3.78 | - | 0.13 | -0.41 | -0.57 | |
| (-5.41, -1.32) | (1.15, 3.91) | (-6.00, -1.55) | (-0.95, 1.22) | (-1.13, 0.31) | (-1.74, 0.59) | |||
| IMT_Pm | -3.87 | 2.03 | -4.28 | -0.5 | - | -0.54 | -0.71 | |
| (-5.07, -2.68) | (-0.13, 4.19) | (-5.77, -2.79) | (-2.17, 1.16) | (-1.72, 0.63) | (-1.87, 0.46) | |||
| IMT_Ph | -6.07 | -0.18 | -6.48 | -2.71 | -2.2 | - | -0.16 | |
| (-8.35, -3.80) | (-1.12, 0.77) | (-8.93, -4.03) | (-3.72, -1.69) | (-4.15, -0.26) | (-1.23, 0.91) | |||
| Qi_Ex | -0.42 | 5.48 | -0.83 | 2.95 | 3.46 | 5.66 | - | |
| (-1.20, 0.36) | (2.90, 8.07) | (-2.40, 0.75) | (0.76, 5.14) | (2.03, 4.88) | (3.25, 8.07) | |||
| Outcome of 6-min walking distance test | ||||||||
| The outcome of Minnesota Living with Heart Failure Questionnaire (MLWHF) | None | - | 0.97 | -1.97 | 0.5 | 1.09 | 3.19 | 1.17 |
| (0.03, 1.92) | (-4.19, 0.26) | (-0.72, 1.72) | (0.01, 2.17) | (1.69, 4.68) | (0.64, 1.71) | |||
| Aerobics | 1.06 | - | -2.94 | -0.48 | 0.12 | 2.22 | 0.2 | |
| (-0.42, 2.53) | (-5.20, -0.68) | (-1.74, 0.79) | (-1.02, 1.26) | (0.79, 3.64) | (-0.70, 1.10) | |||
| IMT_Pn | 0.1 | -0.95 | - | 2.46 | 3.06 | 5.15 | 3.14 | |
| (-1.60, 1.81) | (-3.06, 1.16) | (0.29, 4.64) | (1.11, 5.00) | (2.75, 7.56) | (0.89, 5.39) | |||
| IMT_Pl | 1.32 | 0.26 | 1.21 | - | 0.59 | 2.69 | 0.68 | |
| (-0.41, 3.04) | (-1.51, 2.04) | (-1.07, 3.50) | (-0.38, 1.56) | (1.49, 3.89) | (-0.59, 1.95) | |||
| IMT_Pm | 2.1 | 1.04 | 2 | 0.78 | - | 2.1 | 0.08 | |
| (0.92, 3.29) | (-0.46, 2.55) | (0.28, 3.72) | (-0.95, 2.52) | (0.69, 3.51) | (-1.05, 1.22) | |||
| IMT_Ph | 1.79 | 0.73 | 1.68 | 0.47 | -0.31 | - | -2.01 | |
| (0.05, 3.53) | (-0.49, 1.95) | (-0.62, 3.99) | (-1.26, 2.20) | (-2.08, 1.45) | (-3.53, -0.50) | |||
| Qi_Ex | 1.42 | 0.37 | 1.32 | 0.1 | -0.68 | -0.37 | - | |
| (0.59, 2.25) | (-1.21, 1.94) | (-0.57, 3.20) | (-1.77, 1.97) | (-2.09, 0.73) | (-2.21, 1.48) | |||
This systematic review and network meta-analysis study was conducted to determine the respective effects of machine-assisted respiratory training and non-machine-assisted respiratory training on physical performance and QoL in heart failure patients. In terms of machine-assisted respiratory training, the findings support IMT_Ph as the most effective intervention in improving exercise capacity (VO2 peak and 6MWT) and IMT_Pm as the most effective approach in improving QoL. In terms of non-machine-assisted respiratory training, the findings support Qi_Ex as the most effective intervention in improving cardiac function (heart rate). These findings are similar to previous studies, which found that hospital-based machine-assisted respiratory training (IMT 40%-60%) improved both exercise tolerance and QoL[15] and that non-machine-assisted respiratory training (tai chi and yoga) reduced heart rate[19]. This study provides additional, effective care options that clinical staff may adopt and implement with their heart failure patients based on setting (hospital, community, home) and equipment availability as well as patient needs and preferences in order to improve symptoms.
This study identified Qi_Ex, which may be practiced in non-hospital settings, as the best intervention for lowering heart rate in heart failure patients. Qi_Ex includes single and mixed types. Performing the single type of Qi_Ex involves deep breathing, abdominal breathing, fast inhalation-slow exhalation, and yoga. Deep breathing should be practiced three times daily during hospitalization, with 20 deep inhalations per time[58]; the abdominal breathing regimen must be continued for a total of 8 wk[55]; and fast inhalation-slow exhalation should be performed six times daily during hospitalization and three times daily after discharge for a total of 12 wk[40]. Finally, performing yoga concurrently three times weekly further enhances the heart rate lowering effect[18]. The mixed type of Qi_Ex is further divided into two subcategories, the first of which involves a hospital-based abdominal breathing and leg exercise regimen[59] and the second of which involves a home-based tai chi and aerobic exercise regimen[48]. There were 16 RCTs studying on non-machine-assisted respiratory training, of which five had subjects aged over 65 years. Heart failure patients who are old-aged may be somehow limited for non-machine-assisted respiratory training. Reduced heart rate may be achieved through improved sympathetic nervous system functioning caused by adjustments in involuntary respiration activity[54]. Moreover, this study found Qi_Ex to be better than IMT_h in terms of both heart-rate-lowering efficacy and being easy to perform in both hospital and home settings.
The result of the network meta-analysis in this study did not meet requirements for the test for discordancy in the treatment effect of LVEF. The reason for this may be the differences in NYHA class among the various research samples. The baseline LVEF values of the intervention groups in three of the RCTs[35,38,52] were lower than those of their comparison control groups and remained lower after completion of the intervention. Laoutaris et al[36] and Laoutaris et al[38] conducted 12-wk IMT_h interventions on NYHA class II-III individuals; Palau et al[52] conducted a 12-wk IMT_m intervention on NYHA class III-IV individuals and unexpectedly resulted in a reduction in LVEF values[52], while other studies conducted 12-wk IMT_Ph interventions on NYHA class II-III individuals and found no improvement of LVEF. Conversely, all of the RCTs that were reviewed in this study and conducted Qi_Ex interventions on NYHA class I-II patients achieved improvements in LVEF values[18,60]. Similarly, a previous meta-analysis found a high, 98% heterogeneity among LVEF results[17].
This study recommends IMT_Ph as the best approach to improving exercise capacity in heart failure patients, as IMT_Ph was found to have a six-times greater effect than IMT_Pn and over twice that of Qi_Ex in terms of improving both VO2 peak and 6MWT. Moreover, the IMT_Ph intervention that was conducted three times per week for a continuous period of 10 wk attained the largest increase in VO2 peak of any of the included RCT studies[36]. This finding is similar to a previous study that recommended implementing IMT programs at 40%-60% of maximal effort for 3 d weekly for a 6-12-wk period as the optimal approach to increasing VO2 peak[36]. This study recommends Qi_Ex as the best approach to raising exercise capacity (6MWT). Doing Qi_Ex (tai chi) for 2 d weekly for 12 wk[48] and for 24 wk[60] were both found to effectively increase 6MWT distance. This finding is similar to another study on the effects of tai chi[17].
In terms of improving QoL in heart failure patients, this study identified machine-assisted IMT_Pm as the best choice. In the included studies, IMT_Pm was implemented 7 d weekly for a continuous period of 8-12 wk for NYHA class II-III patients[34,50,51,53]. In addition, NYHA class III-IV patients that performed fast inhalation-slow exhalation training six times daily in the hospital and three times daily (10 min per time) for 12 wk after discharge obtained similar optimal results[40]. IMT_Ph was identified as the second best option for NYHA class II-III patients, with both seven[32] and three[35] sessions per week found to improve QoL. The network meta-analysis in this study found that medium resistance was sufficiently effective in improving QoL. Based on the physical abilities of heart failure patients, two weekly sessions at moderate resistance was found to be sufficient for NYHA class III-IV patients, while NYHA class II-III patients may increase their training frequency to seven times per week.
This study is affected by several limitations. First, the meta-analysis was limited to using the data provided in the included RCT studies. Thus, it was only possible to conduct a network meta-analysis of post-intervention data. No comparison of pre-posttest data was possible for each study group. Second, this study was performed exclusively on articles published in either English or Chinese, therefore a linguistic bias might ensue. Third, the average dropout rate of participants was 12% in this study, but seven of the included studies had attrition rates in excess of 20%, with machine-assisted IMT studies accounting for four of these. The findings of this study may thus overestimate the intervention effect. However, 65.3% of the participant loss in these four machine-assisted IMT studies were due to their heart failure prognosis.
This systematic review and network meta-analysis study supports that respiratory training interventions generally improve cardiac function, exercise capacity, and QoL in adult heart failure patients. Specifically, hospital-based, machine-assisted respiratory training significantly improves the physical performance and QoL of these patients. Non-machine-assisted respiratory training such as tai chi, qigong, yoga, and physical exercise, all of which may be done outside of hospital settings and without the use of specialized equipment, was shown to effectively reduce the heart rate of heart failure patients. The findings of this study offer clinical staff both practical insights and practical, settings-based therapeutic strategies for improving the condition of their heart failure patients.
For heart failure, the estimated all-cause mortality rate is 8% and 25% for 30-d and 1-year periods, respectively. It is currently expected that 8 million adults will be diagnosed with heart failure by 2030. The annualized lifetime costs associated with heart failure have been estimated at $868~25532 per patient. Therefore, the care needs of heart failure patients and the high societal costs associated with caring for this growing patient population are issues that will become increasingly important and that, eventually, must be addressed effectively.
Clinical guidelines recommend condition-appropriate exercises as a complementary therapy for heart failure patients in addition to regular pharmacological treatment. Machine-assisted respiratory training such as inspiratory muscle training (IMT) and non-machine-assisted respiratory training such as breathing exercises may improve dyspnea-related physical performance and quality of life (QoL) in heart failure patients. Heart rate and left ventricular ejection fraction (LVEF) are important indicators of cardiac function which is affected by exercise capacity and assessed using the 6-minute walking distance test (6MWT) and peak oxygen uptake (VO2 peak). Currently, most research analysis to date has focused on pairwise comparisons of exercise effects, such as IMT vs aerobic exercises and IMT vs breathing exercises, and the respective effects of IMT regimens at different levels of intensity. Thus, clinical data on supplemental therapies for heart failure patients is inadequate.
To determine the effect of respiratory training interventions on physical performance and quality of life in patients with heart failure.
This was a systematic review and network meta-analysis study. A literature search of 11 electronic databases was conducted for randomized controlled trials on heart failure. Respiratory training interventions were grouped as seven categories and four outcomes. The random-effects model, side-splitting model, and the surface under the cumulative ranking curve were used to test and analyze data.
The interventions from the included studies were grouped as IMT_Pn (inspiratory muscle training without pressure or < 10% MIP), IMT_Pl (inspiratory muscle training with low pressure, 10%-15% MIP), IMT_Pm (inspiratory muscle training with medium pressure, 30%-40% MIP), IMT_Ph (inspiratory muscle training with high pressure, 60% MIP or MIP plus aerobics), Qi_Ex (tai chi, yoga, or breathing exercise), Aerobics (aerobic exercise or weight training), and none (usual care, standard treatment, or education). A significant difference among these groups was found in overall intervention effect on heart rate [95%CI: -1.30-(-0.39)], VO2 peak (95%CI: 0.77-2.17), 6MWT (95%CI: 0.69-1.43), and QoL [95%CI: -1.54 –(-0.73)]. Further, a significant difference was found in heart rate between Qi_Ex and IMT_Pn (95%CI: 0.58-3.13), and in QoL between IMT_Pm and IMT_Pn [95%CI: -3.72-(-0.28)]. The 6MWT of IMT_Ph differed significantly from that of IMT_Pm [95%CI: -3.51-(-0.69)], IMT_Pl [95%CI: -3.89-(-1.49)], and IMT_Pn [95%CI: -7.56-(-2.75)].
This systematic review and network meta-analysis study supports that respiratory training interventions, including IMT, tai chi, yoga, and breathing exercises, are effective strategies for improving cardiac function, exercise capacity, and QoL for adult heart failure patients. Machine-assisted respiratory training in hospital settings should be prioritized over respiratory training provided in non-hospital settings. Specifically, IMT with high pressure effectively improves cardiac function, whereas IMT with moderate pressure effectively improves QoL. In home settings, non-machine-assisted respiratory training such as tai chi, yoga, and breathing exercise effectively improves heart rate.
This study offers clinical staff both practical insights and practical, setting-based therapeutic strategies for improving the condition of their heart failure patients. Respiratory training interventions generally improve cardiac function, exercise capacity, and QoL in adult heart failure patients. However, the result of the network meta-analysis did not meet requirements for the test for discordancy in the treatment effect of LVEF. The reason for this may be the differences in the severity of heart failure among the various research samples. In addition, seven of the included studies had attrition rates in excess of 20%, with IMT studies accounting for four of these. Approximately 65.3% of the participant loss in these IMT studies were due to their heart failure prognosis.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barik R, Deng B, Rostagno C S-Editor: Ma YJ L-Editor: Wang TQ E-Editor: Zhou BX
| 1. | Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, Allison M, Hemingway H, Cleland JG, McMurray JJV, Rahimi K. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. 2018;391:572-580. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 605] [Cited by in F6Publishing: 692] [Article Influence: 115.3] [Reference Citation Analysis (0)] |
| 2. | Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67-e492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4163] [Cited by in F6Publishing: 4382] [Article Influence: 730.3] [Reference Citation Analysis (0)] |
| 3. | Al-Omary MS, Davies AJ, Evans TJ, Bastian B, Fletcher PJ, Attia J, Boyle AJ. Mortality and Readmission Following Hospitalisation for Heart Failure in Australia: A Systematic Review and Meta-Analysis. Heart Lung Circ. 2018;27:917-927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Metra M, Cotter G, El-Khorazaty J, Davison BA, Milo O, Carubelli V, Bourge RC, Cleland JG, Jondeau G, Krum H, O'Connor CM, Parker JD, Torre-Amione G, van Veldhuisen DJ, Rainisio M, Kobrin I, McMurray JJ, Teerlink JR. Acute heart failure in the elderly: differences in clinical characteristics, outcomes, and prognostic factors in the VERITAS Study. J Card Fail. 2015;21:179-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Lesyuk W, Kriza C, Kolominsky-Rabas P. Cost-of-illness studies in heart failure: a systematic review 2004-2016. BMC Cardiovasc Disord. 2018;18:74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 184] [Cited by in F6Publishing: 248] [Article Influence: 41.3] [Reference Citation Analysis (0)] |
| 6. | Prasun MA, Albert NM. The Importance of Heart Rate in Heart Failure and Reduced Ejection Fraction. J Cardiovasc Nurs. 2018;33:453-459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Shi Y, Zhou W, Liu X, Ping Z, Li YQ, Wang C, Lu J, Mao ZX, Zhao J, Yin L, Zhang D, Li L. Resting heart rate and the risk of hypertension and heart failure: a dose-response meta-analysis of prospective studies. J Hypertens. 2018;36:995-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8928] [Cited by in F6Publishing: 8735] [Article Influence: 1091.9] [Reference Citation Analysis (3)] |
| 9. | Blinderman CD, Homel P, Billings JA, Portenoy RK, Tennstedt SL. Symptom distress and quality of life in patients with advanced congestive heart failure. J Pain Symptom Manage. 2008;35:594-603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 212] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 10. | Corrà U, Agostoni PG, Anker SD, Coats AJS, Crespo Leiro MG, de Boer RA, Harjola VP, Hill L, Lainscak M, Lund LH, Metra M, Ponikowski P, Riley J, Seferović PM, Piepoli MF. Role of cardiopulmonary exercise testing in clinical stratification in heart failure. A position paper from the Committee on Exercise Physiology and Training of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20:3-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 107] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 11. | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810-1852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2367] [Cited by in F6Publishing: 2317] [Article Influence: 210.6] [Reference Citation Analysis (0)] |
| 12. | Cahalin LP, Arena R, Guazzi M, Myers J, Cipriano G, Chiappa G, Lavie CJ, Forman DE. Inspiratory muscle training in heart disease and heart failure: a review of the literature with a focus on method of training and outcomes. Expert Rev Cardiovasc Ther. 2013;11:161-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Cahalin LP, Arena RA. Breathing exercises and inspiratory muscle training in heart failure. Heart Fail Clin. 2015;11:149-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Sadek Z, Salami A, Joumaa WH, Awada C, Ahmaidi S, Ramadan W. Best mode of inspiratory muscle training in heart failure patients: a systematic review and meta-analysis. Eur J Prev Cardiol. 2018;25:1691-1701. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Wu J, Kuang L, Fu L. Effects of inspiratory muscle training in chronic heart failure patients: A systematic review and meta-analysis. Congenit Heart Dis. 2018;13:194-202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Gomes Neto M, Ferrari F, Helal L, Lopes AA, Carvalho VO, Stein R. The impact of high-intensity inspiratory muscle training on exercise capacity and inspiratory muscle strength in heart failure with reduced ejection fraction: a systematic review and meta-analysis. Clin Rehabil. 2018;32:1482-1492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 17. | Ren X, Li Y, Yang X, Li J, Li H, Yuan Z, Sun Y, Shang H, Xing Y, Gao Y. The Effects of Tai Chi Training in Patients with Heart Failure: A Systematic Review and Meta-Analysis. Front Physiol. 2017;8:989. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Krishna BH, Pal P, Pal GK, Balachander J, Jayasettiaseelon E, Sreekanth Y, Sridhar MG, Gaur GS. Yoga improves quality of life and functional capacity in heart failure patients. Biomedical Research. 2014;25:178-182. [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 19. | Gok Metin Z, Ejem D, Dionne-Odom JN, Turkman Y, Salvador C, Pamboukian S, Bakitas M. Mind-Body Interventions for Individuals With Heart Failure: A Systematic Review of Randomized Trials. J Card Fail. 2018;24:186-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Gomes Neto M, Durães AR, Conceição LSR, Saquetto MB, Ellingsen Ø, Carvalho VO. High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with heart failure with reduced ejection fraction: A systematic review and meta-analysis. Int J Cardiol. 2018;261:134-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 21. | Ballesta García I, Rubio Arias JÁ, Ramos Campo DJ, Martínez González-Moro I, Carrasco Poyatos M. High-intensity Interval Training Dosage for Heart Failure and Coronary Artery Disease Cardiac Rehabilitation. A Systematic Review and Meta-analysis. Rev Esp Cardiol (Engl Ed). 2019;72:233-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Maldonado-Martín S, Brubaker PH, Eggebeen J, Stewart KP, Kitzman DW. Association Between 6-Minute Walk Test Distance and Objective Variables of Functional Capacity After Exercise Training in Elderly Heart Failure Patients With Preserved Ejection Fraction: A Randomized Exercise Trial. Arch Phys Med Rehabil. 2017;98:600-603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Aspenes ST, Nilsen TI, Skaug EA, Bertheussen GF, Ellingsen Ø, Vatten L, Wisløff U. Peak oxygen uptake and cardiovascular risk factors in 4631 healthy women and men. Med Sci Sports Exerc. 2011;43:1465-1473. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 183] [Cited by in F6Publishing: 194] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 24. | Mazzoni G, Sassone B, Pasanisi G, Myers J, Mandini S, Volpato S, Conconi F, Chiaranda G, Grazzi G. A moderate 500-m treadmill walk for estimating peak oxygen uptake in men with NYHA class I-II heart failure and reduced left ventricular ejection fraction. BMC Cardiovasc Disord. 2018;18:67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Wu JR, Lennie TA, Frazier SK, Moser DK. Health-Related Quality of Life, Functional Status, and Cardiac Event-Free Survival in Patients With Heart Failure. J Cardiovasc Nurs. 2016;31:236-244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 26. | Ostman C, Jewiss D, Smart NA. The Effect of Exercise Training Intensity on Quality of Life in Heart Failure Patients: A Systematic Review and Meta-Analysis. Cardiology. 2017;136:79-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Moser DK, Lee KS, Wu JR, Mudd-Martin G, Jaarsma T, Huang TY, Fan XZ, Strömberg A, Lennie TA, Riegel B. Identification of symptom clusters among patients with heart failure: an international observational study. Int J Nurs Stud. 2014;51:1366-1372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 28. | Chaimani A, Caldwell D, Li T, Higgins J, Salanti G. Chapter 11: Undertaking network meta-analyses. Draft version (16 September 2018) for inclusion in: Higgins JPT, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, Welch V (editors). Cochrane Handbook for Systematic Reviews of Interventions. London: Cochrane 2018; . [Cited in This Article: ] |
| 29. | Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions 5.2.0.2017. Available from: https://training.cochrane.org/handbook. [Cited in This Article: ] |
| 30. | Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331:897-900. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1142] [Cited by in F6Publishing: 1179] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 31. | Mbuagbaw L, Rochwerg B, Jaeschke R, Heels-Andsell D, Alhazzani W, Thabane L, Guyatt GH. Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev. 2017;6:79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 253] [Cited by in F6Publishing: 319] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 32. | Adamopoulos S, Schmid JP, Dendale P, Poerschke D, Hansen D, Dritsas A, Kouloubinis A, Alders T, Gkouziouta A, Reyckers I, Vartela V, Plessas N, Doulaptsis C, Saner H, Laoutaris ID. Combined aerobic/inspiratory muscle training vs. aerobic training in patients with chronic heart failure: The Vent-HeFT trial: a European prospective multicentre randomized trial. Eur J Heart Fail. 2014;16:574-582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 33. | Bosnak-Guclu M, Arikan H, Savci S, Inal-Ince D, Tulumen E, Aytemir K, Tokgözoglu L. Effects of inspiratory muscle training in patients with heart failure. Respir Med. 2011;105:1671-1681. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 34. | Kawauchi TS, Umeda IIK, Braga LM, Mansur AP, Rossi-Neto JM, Guerra de Moraes Rego Sousa A, Hirata MH, Cahalin LP, Nakagawa NK. Is there any benefit using low-intensity inspiratory and peripheral muscle training in heart failure? A randomized clinical trial. Clin Res Cardiol. 2017;106:676-685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Weinsier RL, Schutz Y, Bracco D. Reexamination of the relationship of resting metabolic rate to fat-free mass and to the metabolically active components of fat-free mass in humans. Am J Clin Nutr. 1992;55:790-794. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Laoutaris ID, Dritsas A, Brown MD, Manginas A, Kallistratos MS, Degiannis D, Chaidaroglou A, Panagiotakos DB, Alivizatos PA, Cokkinos DV. Immune response to inspiratory muscle training in patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2007;14:679-685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 37. | Laoutaris ID, Dritsas A, Brown MD, Manginas A, Kallistratos MS, Chaidaroglou A, Degiannis D, Alivizatos PA, Cokkinos DV. Effects of inspiratory muscle training on autonomic activity, endothelial vasodilator function, and N-terminal pro-brain natriuretic peptide levels in chronic heart failure. J Cardiopulm Rehabil Prev. 2008;28:99-106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Laoutaris ID, Adamopoulos S, Manginas A, Panagiotakos DB, Kallistratos MS, Doulaptsis C, Kouloubinis A, Voudris V, Pavlides G, Cokkinos DV, Dritsas A. Benefits of combined aerobic/resistance/inspiratory training in patients with chronic heart failure. A complete exercise model? A prospective randomised study. Int J Cardiol. 2013;167:1967-1972. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 39. | Martínez A, Lisboa C, Jalil J, Muñoz V, Díaz O, Casanegra P, Corbalán R, Vásquez AM, Leiva A. [Selective training of respiratory muscles in patients with chronic heart failure]. Rev Med Chil. 2001;129:133-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Pan QQ. Effect of fast inhalation-slow exhalation rehabilitation training on exercise tolerance in patients with chronic heart failure. China Med Engineering. 2017;25:48-52. [DOI] [Cited in This Article: ] |
| 41. | Parati G, Malfatto G, Boarin S, Branzi G, Caldara G, Giglio A, Bilo G, Ongaro G, Alter A, Gavish B, Mancia G. Device-guided paced breathing in the home setting: effects on exercise capacity, pulmonary and ventricular function in patients with chronic heart failure: a pilot study. Circ Heart Fail. 2008;1:178-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 42. | Zheng L, Zhang C, Wu Xk, Gao A, Li HM, Wang X. Influence of healthcare qigong-6-character formulas (Liuzijue) on heart function in patients with chronic heart failure. Chin J Evid Based Cardiovasc Med. 2017;9:659-662. [Cited in This Article: ] |
| 43. | Pullen PR, Nagamia SH, Mehta PK, Thompson WR, Benardot D, Hammoud R, Parrott JM, Sola S, Khan BV. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. J Card Fail. 2008;14:407-413. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 44. | Pullen PR, Thompson WR, Benardot D, Brandon LJ, Mehta PK, Rifai L, Vadnais DS, Parrott JM, Khan BV. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. 2010;42:651-657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 45. | Yeh GY, McCarthy EP, Wayne PM, Stevenson LW, Wood MJ, Forman D, Davis RB, Phillips RS. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171:750-757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 153] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 46. | Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, Phillips RS, Forman DE. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013;19:77-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 47. | Hägglund E, Hagerman I, Dencker K, Strömberg A. Effects of yoga versus hydrotherapy training on health-related quality of life and exercise capacity in patients with heart failure: A randomized controlled study. Eur J Cardiovasc Nurs. 2017;16:381-389. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 48. | Caminiti G, Volterrani M, Marazzi G, Cerrito A, Massaro R, Arisi A, Franchini A, Sposato B, Rosano G. Tai chi enhances the effects of endurance training in the rehabilitation of elderly patients with chronic heart failure. Rehabil Res Pract. 2011;2011:761958. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | Chen DM, Yu WC, Hung HF, Tsai JC, Wu HY, Chiou AF. The effects of Baduanjin exercise on fatigue and quality of life in patients with heart failure: A randomized controlled trial. Eur J Cardiovasc Nurs. 2018;17:456-466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 50. | Dall'Ago P, Chiappa GR, Guths H, Stein R, Ribeiro JP. Inspiratory muscle training in patients with heart failure and inspiratory muscle weakness: a randomized trial. J Am Coll Cardiol. 2006;47:757-763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 250] [Cited by in F6Publishing: 251] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 51. | Mello PR, Guerra GM, Borile S, Rondon MU, Alves MJ, Negrão CE, Dal Lago P, Mostarda C, Irigoyen MC, Consolim-Colombo FM. Inspiratory muscle training reduces sympathetic nervous activity and improves inspiratory muscle weakness and quality of life in patients with chronic heart failure: a clinical trial. J Cardiopulm Rehabil Prev. 2012;32:255-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 52. | Palau P, Domínguez E, Núñez E, Schmid JP, Vergara P, Ramón JM, Mascarell B, Sanchis J, Chorro FJ, Núñez J. Effects of inspiratory muscle training in patients with heart failure with preserved ejection fraction. Eur J Prev Cardiol. 2014;21:1465-1473. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 53. | Winkelmann ER, Chiappa GR, Lima CO, Viecili PR, Stein R, Ribeiro JP. Addition of inspiratory muscle training to aerobic training improves cardiorespiratory responses to exercise in patients with heart failure and inspiratory muscle weakness. Am Heart J. 2009;158:768.e1-768.e7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 54. | Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, Goldberger AL, Davis RB, Phillips RS. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117:541-548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 189] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 55. | Chen ZF, Chen SZ, Wang XQ, Li QL. Application of active respiratory rehabilitation training in improving exercise tolerance of elderly patients with heart failure. Modern Hospital. 2015;15:75-77. [Cited in This Article: ] |
| 56. | Seo Y, Yates B, LaFramboise L, Pozehl B, Norman JF, Hertzog M. A Home-Based Diaphragmatic Breathing Retraining in Rural Patients With Heart Failure. West J Nurs Res. 2016;38:270-291. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 57. | Laoutaris ID, Dritsas A, Adamopoulos S, Manginas A, Gouziouta A, Kallistratos MS, Koulopoulou M, Voudris V, Cokkinos DV, Sfirakis P. Benefits of physical training on exercise capacity, inspiratory muscle function, and quality of life in patients with ventricular assist devices long-term postimplantation. Eur J Cardiovasc Prev Rehabil. 2011;18:33-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 58. | Lin N, Wang XF. Effects of breathing exercises on exercise tolerance in patients with chronic heart failure. Chin J Nurs. 2011;46:1082-1084. [Cited in This Article: ] |
| 59. | Zhong J, Zhong SM, Ge PY. Effect of Abdominal Breathing Combined with Ankle Pump Exercise on the Exercise Tolerance of Chronic Heart Failure Patients. Today Nurse. 2016;50-51. [Cited in This Article: ] |
| 60. | Yao CD, Li F, Ma YB. Effects of Shadow boxing on rehabilitation in patients with chronic heart failur. Chin J Cardiopulm Rehabil Med. 2010;19:364-367. [Cited in This Article: ] |