Published online Oct 16, 2015. doi: 10.12998/wjcc.v3.i10.920
Peer-review started: March 28, 2015
First decision: May 18, 2015
Revised: June 11, 2015
Accepted: September 2, 2015
Article in press: September 25, 2015
Published online: October 16, 2015
Gastric varices (GV) are one of the most common complications for patients with portal hypertension. Currently, histoacryl injection is recommended as the initial treatment for bleeding of GV, and this injection has been confirmed to be highly effective for most patients in many studies. However, this treatment might be ineffective for some types of GV, such as splenic vein thrombosis-related localized portal hypertension (also called left-sided, sinistral, or regional portal hypertension). Herein, we report a case of repeated pancreatitis-induced complete splenic vein thrombosis that led to intractable gastric variceal bleeding, which was treated by splenectomy. We present detailed radiological and pathological data and blood rheology analysis (the splenic artery - after a short gastric vein or stomach vein - gastric coronary vein - portal vein). The pathophysiology can be explained by the abnormal direction of blood flow in this patient. To our knowledge, this is the first reported case for which detailed pathology and blood rheology data are available.
Core tip: Here, we report a case in which chronic pancreatitis-induced complete splenic vein thrombosis led to intractable gastric variceal bleeding, which is effectly treated by splenectomy. We have provided details regarding the imaging and pathology data, and we describe the hemodynamic characteristics. Then, we reviewed the disease onset and treatment methods, which may provide a reference for the clinical diagnosis and treatment of similar patients.
- Citation: Tang SH, Zeng WZ, He QW, Qin JP, Wu XL, Wang T, Wang Z, He X, Zhou XL, Fan QS, Jiang MD. Repeated pancreatitis-induced splenic vein thrombosis leads to intractable gastric variceal bleeding: A case report and review. World J Clin Cases 2015; 3(10): 920-925
- URL: https://www.wjgnet.com/2307-8960/full/v3/i10/920.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i10.920
Gastric varices (GV) are among the most common complications affecting patients with portal hypertension, which has a mortality rate that can reach as high as 20% within 6 wk[1]. Currently, histoacryl injection is recommended as the initial treatment for bleeding GV, and this approach has been confirmed to be highly effective for most patients in many studies[2-5]. However, this treatment might be ineffective for some types of GV, such as splenic vein thrombosis-related localized portal hypertension (also called left-sided sinistral or regional portal hypertension). Herein, we report a case of recurrent pancreatitis-induced complete splenic vein thrombosis that led to intractable gastric variceal bleeding, which was treated by splenectomy. We present detailed radiological and pathological data and blood rheology analysis results (splenic artery - after a short gastric vein or stomach vein - gastric coronary vein - portal vein). The pathophysiology can be explained by the abnormal direction of blood flow in this patient. To our knowledge, this is the first reported case for which detailed pathology and blood rheology data are available.
A 58-year-old man was admitted to our hospital due to recurrent melena lasting for over a month and vomiting lasting for two hours. His past history revealed a history of heavy drinking of at least 200 g daily that exceeded 30 years; however, approximately 7 years before, his alcohol consumption had decreased. Over the past 7 years, he had experienced recurrent pancreatitis five times, and all incidences resolved. Approximately one month prior to admission, this patient began to experience melena with no obvious cause. Endoscopy showed that the gastric mucosa was elevated with fundal varices without active bleeding. After conservative treatment, the melena became intermittent. Then, another endoscopic examination revealed severe GV, and the patient received five histoacryl injections. Subsequently, he experienced intermittent melena and vomited approximately 200 mL of blood. Physical examination showed anemia, splenomegaly spanning three ribs across the liver, and active bowel sounds (7/min). Blood examinations revealed the following: Red blood cell, 2.98 × 1012/L; hemoglobin concentration, 67 g/L; and platelet count, 90 × 109/L. Both liver and kidney functions were normal. Abdominal enhanced computed tomography (CT) showed cirrhosis and an enlarged portal vein.
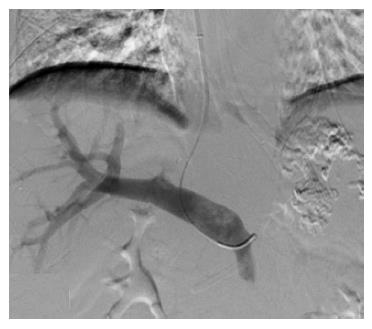
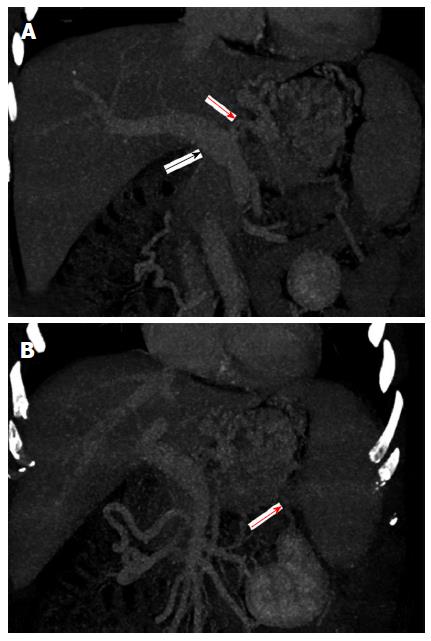
The patient was diagnosed with alcoholic cirrhosis, portal hypertension, splenomegaly and GV. Then, emergency endoscopy revealed bleeding GV, and a second histoacryl injection treatment was performed. However, this patient was also experiencing intermittent vomiting, which had become more frequent because the histoacryl injection did not effectively stop the bleeding from fundus varices. Emergency transjugular intrahepatic portosystemic shunt placement was performed as a hemostatic treatment. Portal vein puncture was successful, and portal vein radiography showed an enlarged portal vein; however, the splenic vein and gastric coronary vein were not imaged (Figure 1). Then, another abdominal enhanced CT and portal systemic vascular reconstruction were performed. The enhanced CT scan revealed an enlarged portal vein from the origin of the gastric coronary vein and an enlarged and circuitous gastric coronary vein (Figure 2A). The splenic vein did not show any flow signals in the portal venous phase (Figure 2B). The portal systemic vascular reconstruction image did not show the splenic vein or spleen signals. These data indicated that the intractable gastric variceal bleeding was not induced by alcoholic cirrhosis or portal hypertension but rather by regional portal hypertension promoted by complete splenic vein thrombosis after recurrent pancreatitis.
Taking into account the poor general condition of the patient, splenic artery embolization could have led to serious complications. Therefore, laparotomy was performed for splenectomy. After opening the abdomen, normal liver size, color and texture were observed. During surgery, we found adhesions of the spleen to organs and tissues, such as the stomach, transverse colon and kidney. Approximately two hours were spent separating the extensive adhesions.
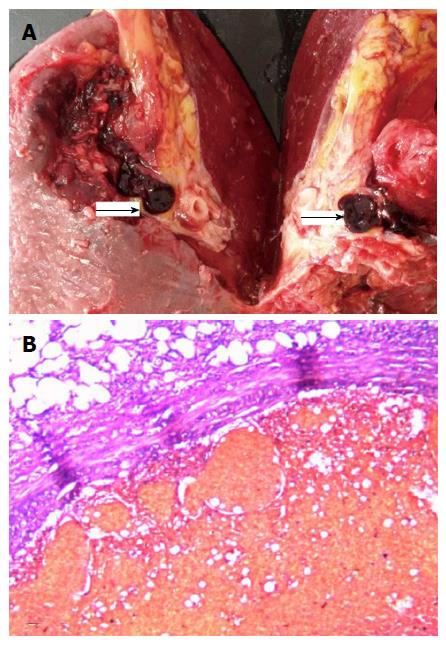
After separation of the surrounding tissues and ligation of the splenic artery and short gastric vessels, we successfully removed the spleen and found that the pancreas was very hard to the touch. After anatomical resection of the spleen, we found that the splenic vein was completely blocked by thrombosis (Figure 3A), and the pathology results further confirmed splenic vein thrombosis (Figure 3B). One month after splenectomy, endoscopic examination revealed that the fundal varices had markedly reduced, and ultrasound examination revealed a normal-sized portal vein.
Gastric variceal bleeding due to regional portal hypertension with splenic vein thrombosis is a severe, life-threatening condition, which is very difficult to control[6]. Patients with splenic vein thrombosis-induced GV, who usually have normal hepatic function, are unlike those with generalized portal hypertension[7], and their mortality risk is higher than that of patients with variceal hemorrhage due to other causes[6,8]. A previous study has shown that as many as 37 different specific etiologies lead to splenic vein thrombosis[9], the most common of which is pancreatitis[10]. The rate of splenic vein thrombosis is 7% to 20% in patients who have previously suffered from pancreatitis[11]. Splenic vein thrombosis induced by pancreatitis was first reported by Hirschfeldt[12]. Other causes of this disease include myeloproliferative neoplasm[13,14], gastrointestinal, pancreatic and hepatobiliary cancers, liver cirrhosis[15], abdominal compression and vibration[16], pancreatic exocrine cancer[17], factors secondary to splenic metastatic cancer[18], minimally invasive distal pancreatectomy[19], and splenic laceration[20].
The splenic vein originates in a large and non-tortuous vessel from the spleen, lies inferior to the splenic artery, and runs behind the pancreatic body and tail. Therefore, the splenic vein endothelium can be damaged by inflammation in the nearby pancreatitis, which can induce splenic vein thrombosis and obstruction. Since the first report of splenic vein thrombosis induced by pancreatitis in 1920[12], five types of pancreatitis have been identified, including chronic, acute, familial, traumatic and autoimmune pancreatitis (Table 1), the most common of which is chronic pancreatitis[11,21-24]. Recently, we have reported a patient with chronic pancreatitis-associated splenic vein thrombosis caused by regional portal hypertension who was treated by partial splenic artery embolization[25]. Acute pancreatitis has been reported to be another common cause of splenic vein thrombosis[23,26,27]. In addition, familial[28], traumatic[29] and autoimmune[30] pancreatitis-induced splenic vein thrombosis and GV have been reported.
| Chronic pancreatitis |
| Longstreth et al[21], 1971 |
| Little et al[22], 1981 |
| Moossa et al[23], 1985 |
| Bernades et al[24], 1992 |
| Heider et al[11], 2004 |
| Tang et al[25], 2015 |
| Acute pancreatitis |
| Moossa et al[23], 1985 |
| Madsen et al[26], 1986 |
| Rogers et al[27], 1989 |
| Familial pancreatitis |
| McElroy et al[28], 1972 |
| Traumatic pancreatitis |
| Salam et al[29], 1973 |
| Autoimmune pancreatitis |
| Ishikawa et al[30], 2012 |
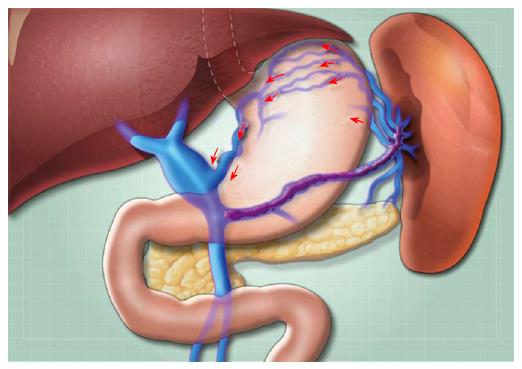
Herein, we report a case of pancreatitis-induced complete splenic vein thrombosis that led to intractable gastric variceal bleeding. This patient was first misdiagnosed with alcoholic cirrhosis-induced portal hypertension. After direct portal venography and portal vein reconstruction, the patient was finally diagnosed with regional portal hypertension induced by complete splenic vein thrombosis after pancreatitis. Normally, blood flows through the splenic artery and short gastric vein from the fundus back to the portal vein. After passing through the spleen, blood flows through the splenic vein[31]. However, when the splenic vein is completely blocked, splenic artery blood cannot flow back through the splenic vein, which causes the spleen to become congested and enlarged. Blood must reflux to the gastric fundus vein through the short gastric vein, which results in a significant increase in gastric fundus pressure, varices, and reflux to the vena cava through the stomach, the renal vein shunt and other branches. When the pressure of the gastric fundus vein is higher than that of the portal vein, the gastric coronary vein will become enlarged, and blood will reflux to the portal vein through the gastric coronary vein, inducing portal vein enlargement (Figure 4). Therefore, these blood rheology findings explain all of the symptoms, signs, laboratory test results and imaging data of the patient.
Antithrombotic therapy has been recommended for venous thromboembolic disease[32-34]. An institutional (Mayo clinic) database search has revealed that a total of 2454 patients were diagnosed with acute pancreatitis from January 1996 to December 2006, with splenic vein thrombosis noted in 45 (1.8%) patients, and the use of oral anticoagulation was considered to be reasonably safe in these patients[35]. However, for chronic pancreatitis, the incidence of splenic vein thrombosis can reach 20% to 40%[36-38]. For complete splenic vein thrombosis patients, antithrombotic therapy may aggravate the risk of bleeding due to fundal varices. Therefore, splenic artery embolization is one of the best treatments for bleeding GV induced by splenic vein thrombosis[14,39-42]. However, “post-embolization syndrome” is a common side effect experienced after splenic artery embolization and includes abdominal pain, fever, vomiting, and purulent infection depending on the arterial embolism size and the patient’s condition. Another study has suggested that transjugular endovascular recanalization of the splenic vein is a safe and effective therapeutic option in patients with regional portal hypertension and is not associated with an increased risk of procedure-related complications[43]. As the condition of the patient in the present report was poor due to massive blood loss, we chose splenectomy via laparotomy, which was successful.
This paper describes a case of chronic pancreatitis-induced complete splenic vein thrombosis, which led to intractable gastric variceal bleeding. We have provided details regarding the imaging and pathology data and have described the hemodynamic characteristics. In addition, we have reviewed the disease onset and treatment methods, which may provide a reference for the clinical diagnosis and treatment of similar patients.
A 58-year-old man with recurrent melena lasting for over a month and vomiting lasting for 2 h.
Chronic pancreatitis-induced complete splenic vein thrombosis led to intractable gastric variceal bleeding.
Red blood cell, 2.98 × 1012/L; hemoglobin concentration, 67 g/L; and platelet count, 90 × 109 /L.
Enhanced computed tomography scan revealed an enlarged portal vein from the origin of the gastric coronary vein and an enlarged and circuitous gastric coronary vein. The splenic vein did not show any flow signals in the portal venous phase.
Laparotomy was performed for splenectomy.
This is the first reported case for which detailed pathology and blood rheology data are available.
A very interesting paper.
P- Reviewer: Del Chiaro M, Yoshida H S- Editor: Yu J L- Editor: Wang TQ E- Editor: Jiao XK
| 1. | Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol. 1989;84:1244-1249. [PubMed] [Cited in This Article: ] |
| 2. | Huang YH, Yeh HZ, Chen GH, Chang CS, Wu CY, Poon SK, Lien HC, Yang SS. Endoscopic treatment of bleeding gastric varices by N-butyl-2-cyanoacrylate (Histoacryl) injection: long-term efficacy and safety. Gastrointest Endosc. 2000;52:160-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 191] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Chang CJ, Hou MC, Lin HC, Lee HS, Liao WC, Su CW, Lee SD. The safety and probable therapeutic effect of routine use of antibiotics and simultaneously treating bleeding gastric varices by using endoscopic cyanoacrylate injection and concomitant esophageal varices with banding ligation: a pilot study. Gastrointest Endosc. 2010;71:1141-1149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Mishra SR, Sharma BC, Kumar A, Sarin SK. Primary prophylaxis of gastric variceal bleeding comparing cyanoacrylate injection and beta-blockers: a randomized controlled trial. J Hepatol. 2011;54:1161-1167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 5. | Sharma BC, Banka AK, Rawat A, Srivastava S. Gastric Varices in Cirrhosis versus Extrahepatic Portal Venous Obstruction and Response to Endoscopic N-Butyl-2-cyanoacrylate Injection. J Clin Exp Hepatol. 2013;3:19-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Sato T, Yamazaki K, Toyota J, Karino Y, Ohmura T, Suga T. Gastric varices with splenic vein occlusion treated by splenic arterial embolization. J Gastroenterol. 2000;35:290-295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc. 1986;32:264-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 246] [Cited by in F6Publishing: 233] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 8. | Köklü S, Coban S, Yüksel O, Arhan M. Left-sided portal hypertension. Dig Dis Sci. 2007;52:1141-1149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Lareo J, Gea F, Abreu C, Barrios A, Garrido A, Albillos C. Isolated splenic vein thrombosis. J Clin Nutr Gastroenterol. 1986;1:221-224. [Cited in This Article: ] |
| 10. | Köklü S, Yüksel O, Arhan M, Coban S, Başar O, Yolcu OF, Uçar E, Ibiş M, Ertugrul I, Sahin B. Report of 24 left-sided portal hypertension cases: a single-center prospective cohort study. Dig Dis Sci. 2005;50:976-982. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Heider TR, Azeem S, Galanko JA, Behrns KE. The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239:876-880; discussion 880-882. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Hirschfeldt H. Die Erkankungen der Milz: Die Hepatolineal Erkankungen. Berlin: Publisher 1920; 384. [DOI] [Cited in This Article: ] |
| 13. | De Stefano V, Martinelli I. Splanchnic vein thrombosis: clinical presentation, risk factors and treatment. Intern. Emerg Med. 2010;5:487-494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 14. | Gianotti R, Charles H, Hymes K, Chandarana H, Sigal S. Treatment of gastric varices with partial splenic embolization in a patient with portal vein thrombosis and a myeloproliferative disorder. World J Gastroenterol. 2014;20:14495-14499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE. Survival and recurrence in patients with splanchnic vein thromboses. Clin Gastroenterol Hepatol. 2010;8:200-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 130] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 16. | Tzur I, Almoznino-Sarafian D, Dotan E, Copel L, Gorelik O, Shteinshnaider M, Cohen N. Splenic vein thrombosis following abdominal compression and vibration: a case report. Angiology. 2008;59:514-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Dedania N, Agrawal N, Winter JM, Koniaris LG, Rosato EL, Sauter PK, Leiby B, Pequignot E, Yeo CJ, Lavu H. Splenic vein thrombosis is associated with an increase in pancreas-specific complications and reduced survival in patients undergoing distal pancreatectomy for pancreatic exocrine cancer. J Gastrointest Surg. 2013;17:1392-1398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Hiraiwa K, Morozumi K, Miyazaki H, Sotome K, Furukawa A, Nakamaru M, Tanaka Y, Iri H. Isolated splenic vein thrombosis secondary to splenic metastasis: a case report. World J Gastroenterol. 2006;12:6561-6563. [PubMed] [Cited in This Article: ] |
| 19. | Kang CM, Chung YE, Jung MJ, Hwang HK, Choi SH, Lee WJ. Splenic vein thrombosis and pancreatic fistula after minimally invasive distal pancreatectomy. Br J Surg. 2014;101:114-119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Nomura T, Keira N, Urakabe Y, Naito D, Enomoto S, Nishikawa S, Matsubara H, Tatsumi T. Fatal splenic laceration in a young woman caused by idiopathic isolated splenic vein thrombosis. Intern Med. 2009;48:907-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Longstreth GF, Newcomer AD, Green PA. Extrahepatic portal hypertension caused by chronic pancreatitis. Ann Intern Med. 1971;75:903-908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 53] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Little AG, Moossa AR. Gastrointestinal hemorrhage from left-sided portal hypertension. An unappreciated complication of pancreatitis. Am J Surg. 1981;141:153-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 86] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Moossa AR, Gadd MA. Isolated splenic vein thrombosis. World J Surg. 1985;9:384-390. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 81] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Bernades P, Baetz A, Lévy P, Belghiti J, Menu Y, Fékété F. Splenic and portal venous obstruction in chronic pancreatitis. A prospective longitudinal study of a medical-surgical series of 266 patients. Dig Dis Sci. 1992;37:340-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 129] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Tang S, He X, Wang Z. Partial splenic artery embolization treatment of chronic pancreatitis associated splenic vein thrombosis caused regional portal hypertension: a case report. Linchuang Gandanbing Zazhi. 2015;31:771-772. [Cited in This Article: ] |
| 26. | Madsen MS, Petersen TH, Sommer H. Segmental portal hypertension. Ann Surg. 1986;204:72-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 105] [Article Influence: 2.8] [Reference Citation Analysis (18)] |
| 27. | Rogers C, Klatt EC. Splenic vein thrombosis in patients with acute pancreatitis. Int J Pancreatol. 1989;5:117-121. [PubMed] [Cited in This Article: ] |
| 28. | McElroy R, Christiansen PA. Hereditary pancreatitis in a kinship associated with portal vein thrombosis. Am J Med. 1972;52:228-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Salam AA, Warren WD, Tyras DH. Splenic vein thrombosis: a diagnosable and curable form of portal hypertension. Surgery. 1973;74:961-972. [PubMed] [Cited in This Article: ] |
| 30. | Ishikawa T, Itoh A, Kawashima H, Ohno E, Itoh Y, Nakamura Y, Hiramatsu T, Miyahara R, Ohmiya N, Haruta J. Peripancreatic vascular involvements of autoimmune pancreatitis. J Gastroenterol Hepatol. 2012;27:1790-1795. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Butler JR, Eckert GJ, Zyromski NJ, Leonardi MJ, Lillemoe KD, Howard TJ. Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review and meta-analysis of its incidence and rate of gastrointestinal bleeding. HPB (Oxford). 2011;13:839-845. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 132] [Article Influence: 10.2] [Reference Citation Analysis (1)] |
| 32. | de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 794] [Cited by in F6Publishing: 710] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 33. | Condat B, Pessione F, Helene Denninger M, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000;32:466-470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 342] [Cited by in F6Publishing: 360] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 34. | Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1466] [Cited by in F6Publishing: 1299] [Article Influence: 81.2] [Reference Citation Analysis (0)] |
| 35. | Harris S, Nadkarni NA, Naina HV, Vege SS. Splanchnic vein thrombosis in acute pancreatitis: a single-center experience. Pancreas. 2013;42:1251-1254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 36. | Sakorafas GH, Sarr MG, Farley DR, Farnell MB. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000;179:129-133. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 101] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 37. | Weber SM, Rikkers LF. Splenic vein thrombosis and gastrointestinal bleeding in chronic pancreatitis. World J Surg. 2003;27:1271-1274. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 38. | Agarwal AK, Raj Kumar K, Agarwal S, Singh S. Significance of splenic vein thrombosis in chronic pancreatitis. Am J Surg. 2008;196:149-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 39. | Stone PA, Phang D, Richmond B, Gill G, Campbell JE. Splenic artery embolization for the treatment of bleeding gastric varices secondary to splenic vein thrombosis. Ann Vasc Surg. 2014;28:737.e7-737.11. [PubMed] [Cited in This Article: ] |
| 40. | Sankararaman S, Velayuthan S, Vea R, Herbst J. Severe gastric variceal bleeding successfully treated by emergency splenic artery embolization. Pediatr Int. 2013;55:e42-e45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Saugel B, Gaa J, Phillip V, Schmid RM, Huber W. Splenic artery embolization in a woman with bleeding gastric varices and splenic vein thrombosis: a case report. J Med Case Rep. 2010;4:247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Paramythiotis D, Papavramidis TS, Giavroglou K, Potsi S, Girtovitis F, Michalopoulos A, Papadopoulos VN, Prousalidis J. Massive variceal bleeding secondary to splenic vein thrombosis successfully treated with splenic artery embolization: a case report. J Med Case Rep. 2010;4:139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Luo X, Nie L, Wang Z, Tsauo J, Tang C, Li X. Transjugular endovascular recanalization of splenic vein in patients with regional portal hypertension complicated by gastrointestinal bleeding. Cardiovasc Intervent Radiol. 2014;37:108-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |