Published online Mar 19, 2022. doi: 10.5498/wjp.v12.i3.379
Peer-review started: March 29, 2021
First decision: August 19, 2021
Revised: August 22, 2021
Accepted: January 22, 2022
Article in press: January 22, 2022
Published online: March 19, 2022
Mood disorders are the most common mental disorders, affecting approximately 350 million people globally. Recent studies have shown that neuroimmune interaction regulates mood disorders. Brain-derived neurotrophic factor (BDNF) and its precursor pro-BDNF, are involved in the neuroimmune crosstalk during the development of mood disorders. BDNF is implicated in the pathophysiology of psychiatric and neurological disorders especially in antidepressant pharmacotherapy. In this review, we describe the functions of BDNF/pro-BDNF signaling in the central nervous system in the context of mood disorders. In addition, we summarize the developments for BDNF and pro-BDNF functions in mood disorders. This review aims to provide new insights into the impact of neuroimmune interaction on mood disorders and reveal a new basis for further development of diagnostic targets and mood disorders.
Core Tip: The neuroimmune crosstalk plays a crucial role in the regulation of mood disorders. Recent studies have shown that the brain-derived neurotrophic factor (BDNF) and its precursor pro-BDNF are cardinal regulators in the neuroimmune axis. However, the roles and potential mechanisms of BDNF/pro-BDNF signaling in the neuroimmune crosstalk in the context of mood disorders remain unexplored. In this review, we summarize recent studies on the role of BDNF/TrkB signaling and pro-BDNF/p75NTR signaling in the neuroimmune axis and how they influence the development of mood disorders.
- Citation: Zhao XP, Li H, Dai RP. Neuroimmune crosstalk through brain-derived neurotrophic factor and its precursor pro-BDNF: New insights into mood disorders. World J Psychiatry 2022; 12(3): 379-392
- URL: https://www.wjgnet.com/2220-3206/full/v12/i3/379.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i3.379
Mood disorders are complex diseases characterized by mood depression and anhedonia. Depressive episodes, manic episodes, bipolar disorder, as well as persistent mood disorders are the typical symptoms. In addition, mood disorders are among the most common mental disorders in the world and major contributors to the global burden of disease[1,2]. In Europe, for example, the current burden is greater than that from 10 years ago despite the availability of reasonably effective pharmacological and psychological interventions[3]. Moreover, the World Health Organization in 2008 ranked major depression as the third cause of the disease burden worldwide and predicted that the disease will rank first by 2030[4]. Furthermore, various studies have shown the impact of depression, anxiety and stress on different systems including the cardiovascular and immune systems[5]. However, the mechanisms and pathogenesis of the syndrome still remain unclear. Although antidepressants were previously used extensively in the treatment of mood disorders, current forms of treatment are largely suboptimal. It is therefore urgent and necessary to explore novel therapeutic targets for the treatment of mood disorders.
Several theories have been put forward to explain mood disorders, including the neural circuit hypothesis, neurotransmitter hypothesis, hypothalamus-pituitary-adrenal (HPA) axis dysfunction, neurotrophic hypothesis and cytokine hypothesis[1]. Among them, neurotrophins, particularly brain-derived neurotrophic factor (BDNF), are extensively studied for their role in mood disorders. Additionally, dysfunctions in BDNF and its precursor pro-BDNF in the central nervous system (CNS) are well known to play a critical role in the pathogenesis of mood disorders. However, it is still unclear whether peripheral BDNF can reflect changes in the levels of BDNF in the CNS. Moreover, recent studies have shown that there are changes in BDNF and pro-BDNF signaling in the immune cells of patients with depression[6]. Nonetheless, the exact mechanisms of BDNF/pro-BDNF in neuroimmune crosstalk are yet to be elucidated. The changes in BDNF/pro-BDNF signaling in the CNS and immune system suggest that this neurotrophin is a linker in neuroimmune crosstalk; an emerging topic that has gained popularity in the field of mood disorders.
BDNF is the second identified member of the neurotrophin family and the most widely distributed neurotrophin in the CNS as well as the peripheral nervous system[7]. Previous studies have reported that BDNF is expressed in neurons, astrocytes, Schwann cells, fibroblasts and possibly, smooth muscle cells[8]. In addition, regulation of BDNF processing is governed by complex regulatory mechanisms at the transcriptional, translational and posttranslational levels of gene expression[9]. The human BDNF gene is located on chromosome 11, region p13-14 and spans 70 kb. The gene has a complex structure as it consists of 11 exons (I-IX, plus Vh and VIIIh) in the 5′ end and nine functional promoters. The coding sequence resides in exon 9 and has eight upstream exons that encode promoters regulating regional and cell-type-specific expression[10]. Moreover, the BDNF protein is initially synthesized into pro-BDNF in the endoplasmic reticulum. Pro-BDNF is then subsequently cleaved by proconvertases/furin to generate either a 28-kDa truncated form (truncated BDNF) or the 13.5-kDa mature BDNF. Following this, the mature BDNF is stored in the dense-core vesicle and is secreted upon neuronal activation. Additionally, BDNF signaling plays a critical role in promoting neuronal survival, phenotypic differentiation, axonal and dendritic growth and synapse formation[11,12].
BDNF function is mediated by two receptor systems, namely, TrkB and p75NTR (pan 75 neurotrophin receptor)[13]. Extensive research has shown that BDNF binds to its high-affinity receptor TrkB, causing the autophosphorylation of TrkB, subsequently activating the mitogen-activated protein kinase pathway, phospholipase C-γ pathway, phosphatidylinositol 3-kinase pathway and other signaling pathways. Additionally, BDNF-TrkB signaling affects the survival, development and function of neurons. They also promotes the formation of the dendritic spine, provides a structural basis for synapse formation and improves the transmission efficiency of synapses[14].
As the intermediate during the synthesis of BDNF, pro-BDNF can also be secreted outside the cells in different sites of the CNS, such as the cerebral cortex, cerebellum, substantia nigra, amygdala and hypothamalus[8]. In addition, pro-BDNF can be cleaved extracellularly into mature or truncated BDNF by matrix metalloproteinases/plasmin[12]. Pro-BDNF can also bind to its high affinity receptor, p75NTR with its co-receptor sortilin and exert an effect opposite to the biological function of mature BDNF, including neuronal apoptosis, pruning of axons and dendrites and long-term depression[13-15]. Therefore, it is important to discuss the roles of these two proteins involved in mood disorders. Moreover, activation of TrkB and p75NTR promotes and suppresses the growth of the dendritic spine, respectively. Therefore, cleavage of pro-BDNF may represent a new mechanism that controls the direction of BDNF regulation, i.e., synaptic potentiation or synaptic depression.
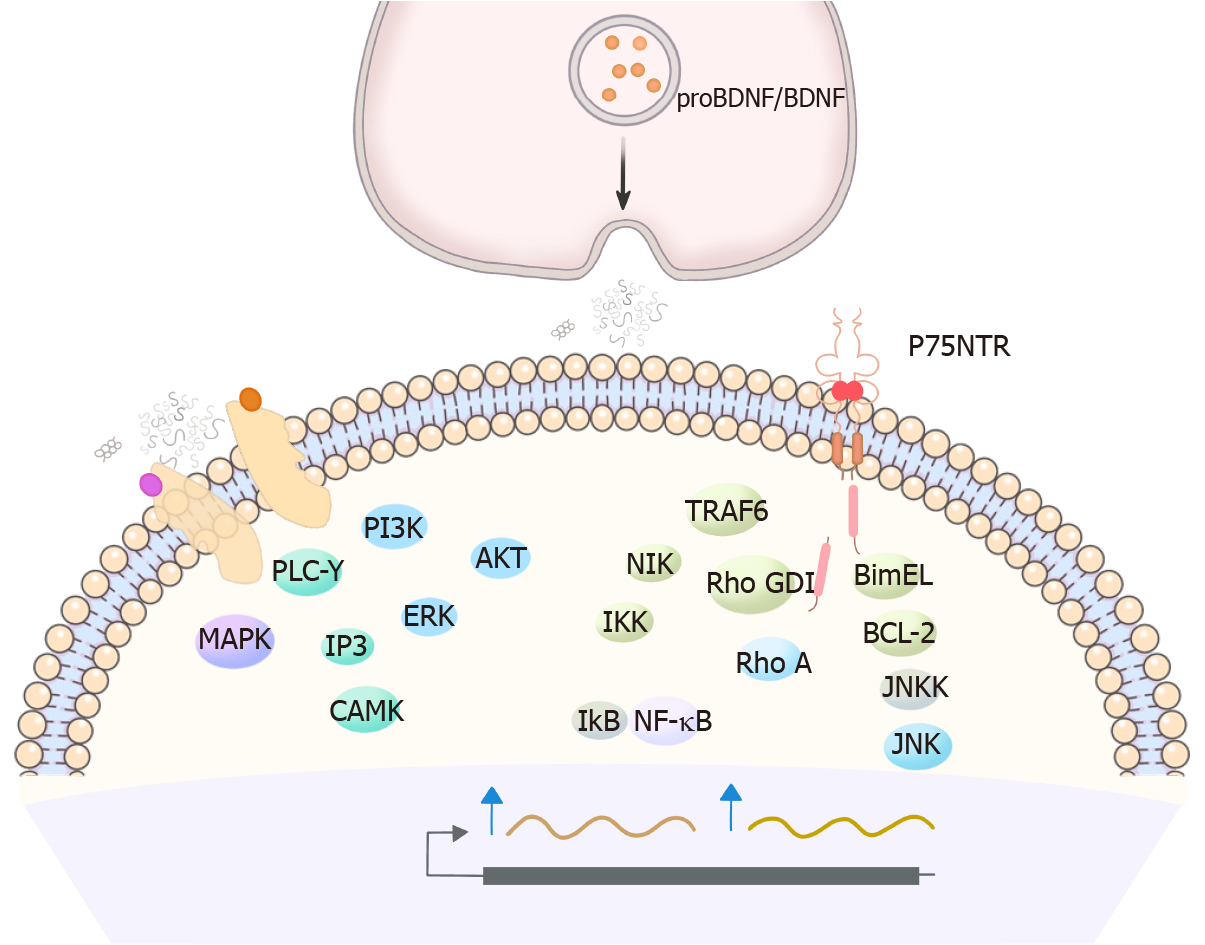
Several signaling pathways are activated following the binding of pro-neurotrophin to p75NTR. These signaling pathways which summarized in Figure 1 are mediated by the interaction of p75NTR to its adaptor proteins, including tumor necrosis factor receptor-associated factor 6, the neurotrophin receptor-interacting factor, melanoma-associated antigen (MAGE), neurotrophin receptor p75 interacting MAGE homolog, Schwann cell factor 1, rho GDP dissociation inhibitor (RhoGDI) and other proteins[16]. Additionally, there are three major downstream pathways for p75NTR including nuclear factor (NF)- κB signaling, RhoGDI and the RhoA signaling, and Jun kinase signaling cascade. Notably, NF-κB is a transcription factor that can be activated by p75NTR but not via Trk receptors. Moreover, RIP2 was previously shown to link p75NTR to the NF-κB pathway[17]. Activation of NF-κB also contributes to the NGF-dependent survival of developing sensory neurons, oligodendrocytes and Schwann cells[18-21]. It mediates the NGF-dependent increase in the expression of the survival factor Bcl-xL and a survival pathway in PC12 cells[22]. RhoA causes the actin cytoskeleton to become rigid, which limits the mobility of the growth cone and inhibits neuronal elongation in the developing nervous system[23]. Recent evidence suggests that RhoA activity is regulated by the cytoplasmic domain of p75NTR[24]. Furthermore, the unbound state of p75NTR associates with RhoGDI, which subsequently interacts with RhoA and activates RhoA signaling[25]. It was also shown that neurotrophins inhibit the association between RhoGDI and p75NTR, thus suppressing the release of RhoA and promoting the elongation of the growth cone[26,27]. Additionally, pro-neurotrophin binds to p75NTR and activates the c-Jun N-terminal kinases (JNK) signaling pathway, causing apoptosis of developing neurons[28]. In contrast, TrkA can prevent p75NTR-mediated apoptosis induced by the JNK pathway[29].
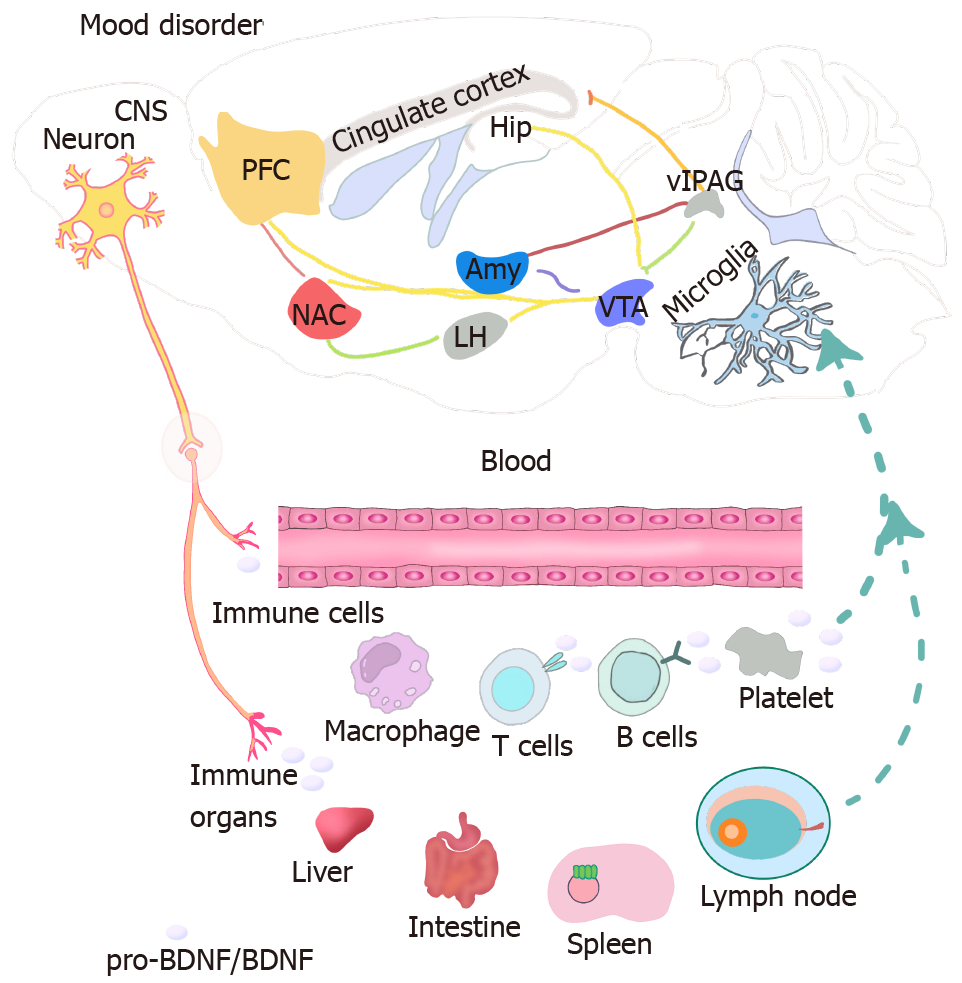
The neurocircuits involved in regulating mood disorders include the hypothalamus, hippocampus, brain stem nuclei, temporal lobe, caudate, the anterior cingulate cortex (ACC), frontal cortex, basal forebrain, the extended amygdala, including the central nucleus of the amygdala (CeA) and medial nucleus of the amygdala (MeA), bed nucleus of the stria terminalis (BNST) and the shell of the nucleus accumbens (NAc)[11,30]. Clinical and experimental studies showed that depression may be driven by a dysregulated circuit function across multiple brain regions[31]. In addition, BDNF was also shown to be highly expressed in the cortex, hippocampus, limbic structures, cerebellum and the olfactory bulb[32]. Using specific antibodies against pro-BDNF, previous studies showed that pro-BDNF is widely and abundantly expressed throughout the adult brain. Moreover, experimental studies have shown that pro-BDNF, in different brain regions, regulates depressive behaviors. A previous study also reported that pro-BDNF is upregulated in the hippocampus, neocortex, the medial prefrontal cortex (PFC) and brainstem of individuals with a depression-like phenotype[33]. In contrast, there was a decrease in the expression of pro-BDNF in the NAc of rats with learned helplessness. These studies therefore suggest that the association of BDNF and pro-BDNF with the mood status is dependent on the specific location and the neural circuitry.
Existing evidence shows that the BDNF in the hippocampus plays an important role in the pathogenesis of depression[34]. First, previous studies reported that the expression of hippocampal BDNF declined in different depression models. For instance, chronic-stress-induced models of depression showed decreasing levels of BDNF in the hippocampus and antidepressant treatment upregulated the expression of BDNF and TrkB in the hippocampus of rats[35]. It was also shown that chronic unpredictable mild stress (CUMS) decreased the levels of BDNF in the hippocampus and PFC, but increased the levels of BDNF in the basolateral nucleus of the amygdala (BLA). On the contrary, the blood oxygen level-dependent (BOLD) activity was elevated in the hippocampus and PFC but reduced in the BLA after exposure to CUMS, indicating that the levels of BDNF were negatively correlated with BOLD activity in the WT CUMS-exposed mice[30]. Second, it was reported that various antidepressants can restore the downregulation of BDNF in the hippocampus. Notably, antidepressant drugs increased the expression of BDNF mRNA in the hippocampi of rats[36]. In addition, treatment with monoamine oxidase inhibitors increased the expression of BDNF in specific hippocampal subfields. Consistent with these results, it is reported that administration of leptin exerted antidepressant effects and increased the expression of BDNF in the hippocampus[37]. Third, it has been shown that impairment of hippocampal BDNF signaling produces certain depression-related behaviors and reduces the effect of the antidepressants[38]. Previous studies have shown that upregulating the levels of hippocampal BDNF produces antidepressant effects. In addition, it is reported that direct incorporation of BDNF in the hippocampus of rodents mimics antidepressant treatment[12]. Moreover, it was previously shown that peripheral administration of BDNF produces anxiolytic and antidepressant effects. Therefore, the downregulation of BDNF in the hippocampus contributes to the pathogenesis of depression.
Several mechanisms have been proposed to underlie the role of hippocampal BDNF in depression. It is well known that BDNF/TrkB signaling activates the cAMP-response element binding protein (CREB) cascade and that antidepressant treatment upregulates the cAMP-CREB cascade in the hippocampus[39]. The activating cAMP-CREB signaling enhances the response to a tricyclic antidepressant. Therefore, downregulation of BDNF may inhibit downstream cAMP-CREB signaling and promote progression of mood disorders. In contrast, the inhibition of neurogenesis resulting from the reduced levels of BDNF may contribute to mood disorders, particularly depression. It is noteworthy that neurogenesis in adult animals is restricted to the subventricular zone of lateral ventricles and the dentate gyrus of the hippocampus. Furthermore, hippocampal neurogenesis is mediated by BDNF/ TrkB signaling and is sensitive to a variety of environmental stimuli, including exercise, enrichment and antidepressant treatment[40]. It has also been shown that chronic antidepressant treatment increases neurogenesis in the hippocampus of adult rodents. Moreover, the effects of antidepressants on neurogenesis are dependent on intact BDNF signaling through TrkB[36]. According to a previous study, mice lacking TrkB in hippocampal neural progenitor cells failed to exhibit antidepressant-induced proliferation and neurogenesis[41].
It has also been shown that the levels of pro-BDNF and its receptors are increased in the hippocampus of rats with depression[42]. In addition, pro-BDNF negatively regulates dendritic complexity and depresses synaptic transmission in the hippocampus. There was an increase in the levels of hippocampal pro-BDNF in carioca high-conditioned freezing (a model of anxiety disorder) rats[43]. Additionally, injection of anti-pro-BDNF antibodies through the intracerebroventricular and intraperitoneal routes reverses the stress-induced depressive behavior[44]. In the major depressive disorder (MDD), reductions in the levels of pro-BDNF are seen in the right but not the left hippocampus, with no changes in the dentate gyrus[45]. Furthermore, exposure to the water maze increases the levels of the pro-BDNF protein in the dorsal hippocampus although the levels decrease in the ventral hippocampus. A recent study by our research group also demonstrated that pro-BDNF was upregulated in the hippocampus of rats with a depression-like or anxiety-like phenotype[44]. Moreover, intra-hippocampal injection of pro-BDNF antibodies attenuated the depression-like and anxiety-like behaviors, suggesting that pro-BDNF, in the hippocampus, is a common mediator of anxiety and depression[44].
The hypothalamus is a vital neuroendocrine region that not only influences the neuroendocrine and immune systems but also is closely related to the pathogenesis of depression. Additionally, many preclinical and clinical studies have proven that certain depressive characteristics are associated with abnormities in the hypothalamus. For instance, neuroimaging and postmortem brain microscopy studies showed widespread anatomical changes, volume deficits and neuron pathological changes in the hypothalamus of individuals with depression[46]. It has also been shown that intracerebroven
The PFC is an important region of the brain that is involved in depression-like behavior. Previous studies reported that depressed suicide victims had low levels of BDNF in the hippocampus and PFC, especially in the ventromedial PFC[51]. Additionally, the antidepressant effects of ketamine were lost in mice lacking BDNF or TrkB or when the medial PFC was injected with anti-BDNF antibodies. Moreover, the chronic administration of different antidepressants such as escitalopram and fluoxetine is capable of increasing the levels of BDNF in the PFC of both rats and humans[52]. The mPFC-selective knockdown of BDNF showed diminished motivation but not impaired response-outcome learning[53].
The ACC is located in the medial subregion of the frontal lobe and is part of a neural system involved in motivating or energizing behavior and hierarchical reinforcement learning. It has been shown that there is a decrease in BDNF signaling in the subequal ACC of individuals with MDD[54]. Additionally, the Chaihu Shugan Powder significantly improves depressive behavior by increasing the mRNA expression levels of BDNF and TrkB in the hippocampus, amygdala and frontal lobe[55]. It is also reported that treatment with anti-pro-BDNF antibodies in the ACC restores the CUMS-induced decrease in the levels of BDNF mRNA in the cortex and hippocampus[56].
The midbrain, also known as the mesencephalon, is a region of the developing vertebrate brain that is composed of the tectum and tegmentum. The tectum makes up the rear portion of the midbrain and is composed of two paired rounded swellings, the superior and inferior colliculi. The tegmentum is located in front of the tectum. It consists of fiber tracts and three regions distinguished by their color, i.e., the red nucleus, the periaqueductal gray (PAG) and the substantia nigra[57]. It has been shown that the BDNF and TrkB receptors are enriched in the dorsal PAG of the rat midbrain, which is considered to be a key structure in the pathophysiology of panic disorder. In addition, BDNF/TrkB signaling in the dorsal PAG is implicated in the beneficial effects of antidepressants in panic disorder[58,59]. Moreover, chronic infusion of BDNF into the midbrain is reported to increase the neurotransmission of 5-hydroxytryptamine (HT) and exert antidepressant effects in the learned helplessness and forced swim test depression models[60]. Moreover, direct administration of BDNF into the midbrain is sufficient to induce antidepressant-like behavior and neurogenesis[36]. A recent study also showed that BDNF-TrkB-mTORC1 signaling in the ventral PAG is required for sustained antidepressant effects[61].
The monoamine hypothesis postulates that depression is primarily caused by imbalances in the neurotransmission of monoamines, namely dopamine (DA), serotonin (5-HT) or norepinephrine (NE)[62]. In addition, numerous studies have suggested that BDNF signaling is closely associated with changes in the 5-HT and DA systems during the development and neuroplasticity of mood dysfunction.
Distinct effects of BDNF on the 5-HT system have been identified in depression. Notably, 5-HT is produced in the raphe nuclei of the brain stem region then spreads to terminal regions throughout the brain including the hypothalamus, cortex, hippocampus and amygdala. It also regulates a wide repertoire of functions such as behavior, cognition and mood[12,34]. Previous studies conducted on preschoolers have revealed a correlation between BDNF and 5-HT polymorphisms during brain development. The studies have also shown high levels of cortisol that could be a cause of depression. Additionally, the local administration of BDNF into the main cluster of the cell bodies of serotonergic neurons in the dorsal raphe nuclei (DRN) is reported to increase the length of dendrites and alter the electrophysiological activity of 5-HT neurons[63].
Infusion with BDNF results in hyperinnervation of 5-HT axons at the site of infusion in either the cerebral cortex or hippocampus. Moreover, BDNF has a profound effect on the sprouting of either intact 5-HT or neurotoxin-lesioned neurons[62]. Reduced levels of BDNF in BDNF+/- mice also leads to decreased functional activity in the 5-HT1A receptor in the hippocampus and deficient 5-HT2A receptors in the PFC and DRN of the midbrain. In addition, BDNF/TrkB is an upstream regulator of the 5-HT2A pathway[64]. It is also reported that hippocampal BDNF improves some specific behavioral impairments including anxiety and anhedonia in 5-HT4R KO mice[65].
Depression is likely controlled by two interacting brain systems: the brain stress system HPA pathway and the brain reward system [ventral tegmental area-NAc (VTA-NAc) and VTA-PFC]. The VTA-NAc is the origin of dopaminergic neurons[12] and the dopaminergic VTA-NAc pathway is critical for reward and motivation. Notably, intrahippocampal infusion of BDNF produces antidepressant effects although it appears to play a prodepressive role in the VTA-NAc reward system. Additionally, many studies have shown that the levels of BDNF are increased in the VTA and NAc of depressed rats and mice although the levels are reduced in the hippocampus. Moreover, recent research has shown that intra-VTA injections of BDNF lead to an increase in depression-like behavior in rats as revealed by the forced swim test. It has also been shown that chronic neonatal stress not only leads to long-term changes in the expression of BDNF in the VTA, but also causes depression-like behavior in adults. In addition, the increased levels of BDNF seem to disinhibit the VTA DA neurons since knocking down BDNF in VTA prevents social-defeat-induced cross-sensitization to amphetamine. Furthermore, BDNF activity is closely associated with the excitability of VTA-DA neurons[66]. Chronic optogenetic phasic stimulation of VTA DA neurons increases the levels of NAc-BDNF and exacerbates social avoidance. Additionally, blocking BDNF-TrkB signaling in the NAc and VTA prevents aggravation of social avoidance. Therefore, BDNF signaling in the VTA-NAc pathway is required for the development of the susceptible phenotype induced by chronic social stress.
NAc is located in the basal forebrain, rostral to the preoptic areas. In addition, neurons in NAc integrate reward-related dopaminergic signals as well as glutamatergic input from the PFC, hippocampus, amygdala and hypothalamus[38,67]. In NAc, BDNF is expressed in dopaminergic and excitatory neurons projecting to NAc. TrkB is expressed in neurons expressing both the dopamine D1 and D2 receptors. Similar to VTA, it is reported that enhancing BDNF function in NAc can induce the behavioral changes associated with mood disorders, including anhedonia, anxiety and social interaction in rodents[38]. Moreover, inhibiting BDNF–TrkB signaling using dominant-negative TrkB-T1 in NAc, results in a dramatic antidepressant effect.
Moreover, previous research has enhanced basal dopaminergic and BDNF signaling to investigate their effects on behavioral changes. The results have shown significant comorbidity of substance dependence and depressive disorders[68]. However, the implication of pro-BDNF signaling in NAc on mood disorders is yet to be explored. Since the antidepressant effects on behavior despair are mediated by BDNF–TrkB signaling in the hippocampus, it is possible that pro-BDNF-p75NTR mechanisms are involved in the VTA-NAc-mediated anhedonic phenotype. Therefore, selective deletion of genes encoding receptor p75NTR in NAc may be helpful in explaining the specific role of pro-BDNF and mBDNF in depressive behaviors.
Pharmacological, genetic and postmortem evidence strongly suggests the involvement of synaptic dysfunction in affective disorders. Importantly, disorders are associated with a broad range of altered glutamatergic and glutamatergic and γ-aminobutyric acid (GABAergic) neurometabolism[69].
It is noteworthy that decreased levels of GABA in the plasma, cerebrospinal fluid, prefrontal and occipital cortices and dorsal anterolateral PFC neurons have been reported in patients with MDD[70]. Additionally, the effect of BDNF on the plasticity of GABAergic neurons in the hippocampus has been widely investigated in neuropsychiatric disorders. Previous studies using transgenic mouse models have shown that the genes with a high level of BDNF dependency were Cort, Vgf, Sst, Tac1 and Npy. Those with intermediate BDNF dependency were Snap25 and Gad2 (Gad65) and those with little or no BDNF dependency were Gad1 (GAD67), Pvalb, Rgs4, Slc6a1, Calb2 and Gabra1[71]. BDNF regulates transmission at glutamatergic and GABAergic synapses through both pre- and postsynaptic mechanisms. In addition, BDNF promotes the release of GABA and increases the expression of cell membrane GABAA-R through the presynaptic tyrosine receptor kinase B[72]. It is also reported that postsynaptic BDNF promotes the expression and synaptic insertion of glutamate receptors. A previous study on promoter IV mutant BDNF (BDNF-KIV) mice uncovered the suppression of GABAergic transmission and an aberrant plasticity in the mPFC. This suggests that decreased activity-dependent transcription of BDNF results in altering synaptic function[73].
Additionally, previous studies have found a higher hippocampal mRNA expression of the GABAA-R subunit in the right hemisphere of rats. Intra-PFC infusion with allopregnanolone is also able to increase the gene expression of the γ2 GABAA-R subunit and BDNF in the right hemisphere of the same infused area, while bilateral injection increases the expression of BDNF in the hippocampus and PFC[53]. Moreover, deletion of the serotonin transporter induces neuroplastic impairments mediated by BDNF signaling in the spine and reduces the levels of GABAergic markers in both adulthood and during development[74]. Furthermore, the application of BDNF in the neocortical layer 2/3 rapidly suppresses GABAergic transmission through the release of endocannabinoids from the postsynaptic pyramidal cells, which act in a retrograde manner to suppress the release of presynaptic transmitters[75].
Several studies have shown that BDNF can also modulate the release and function of glutamatergic neurons. For example, a previous study showed that there was a decrease in the levels of the N-methyl-D-aspartate (NMDA) receptor and GABAergic transmission in BDNFMet/Met mice in which the processing of BDNF was impaired[41]. It is also reported that BDNF-dependent synaptic plasticity is involved in the antidepressant effect of low-dose ketamine, a noncompetitive antagonist of the NMDA receptor. According to a previous study, ketamine enhances BDNF signaling and augments plasticity at excitatory synapses[76]. In addition, activation of TrkB modulates presynaptic glutamate release in hippocampus[77]. Overall, these studies strongly suggest the critical role of BDNF-dependent synaptic activity in the regulation of affective behaviors.
More recent studies have been conducted to explore the neuroimmune crosstalk in mood disorders[78]. The crosstalk includes the communication between the nervous and immune systems, the effects of neuroendocrine hormones on the immune system, the innervation of lymphoid organs and the regulatory effects of cytokines on the HPA axis[79]. In addition, it is reported that microglia (resident immune cells in the CNS) as well as astrocytes can secrete some soluble agents such as chemokines, cytokines and neurotrophic factors to regulate immune responses in the CNS, and are implicated in the pathogenesis of mood disorders. Moreover, the levels of pro-BDNF/BDNF in the blood or mononuclear cells are associated with mood disorders, suggesting that peripheral pro-BDNF/BDNF can be diagnostic markers of mood disorders.
Neurotrophins, inflammatory mediators and oxidative stress are three well studied circulating diagnostic markers of mood disorders[80,81]. BDNF can also be used to indicate the efficacy of psychotropics. However, it is still debatable whether the levels of blood BDNF reflect the brain BDNF levels. In clinical studies, ELISA or western-blotting-based measurements of BDNF protein levels in body fluids or tissue samples are considered as potential proxies of brain function and associated diseases. Most clinical studies measure the levels of peripheral BDNF in saliva, serum, plasma, platelets and whole blood. The results show that peripheral blood BDNF appears to be a good indicator of brain BDNF levels. Additional studies have also corroborated that the levels of BDNF in whole blood and plasma are associated with the BDNF levels in the hippocampus[82].
A meta-analysis has shown that the levels of peripheral BDNF are equally reduced in patients with manic and depressive episodes[83]. In addition, previous studies have shown that there is a decrease in the levels of circulating BDNF in older and adolescent bipolar disorder patients in a euthymic state[84-86]. Moreover, a preliminary study showed that patients with bipolar mania had lower levels of the BDNF protein and mRNA, compared to healthy controls[87]. However, these findings were not consistent across all the studies. For instance, a previous study reported that the levels of mature BDNF and the ratio BDNF/proBDNF were significantly higher in patients with BD[88]. It was shown that pediatric bipolar patients had significantly higher levels of BDNF mRNA after eight weeks of treatment[89]. Moreover, a recent study reported that BD patients responsive to lithium had normal levels of serum BDNF[90]. Further research also revealed that lithium and valproic acid selectively activate the promoter IV of BDNF and trigger the respective downstream targets in neurons[91].
Pro-BDNF and its receptors, p75NTR and sortilin are upregulated in the serum of female patients with depression and positively correlated with depression scores[92]. Furthermore, the increased levels of pro-BDNF in the serum of patients with depression is reversed by long-term antidepressant treatment. It has been reported that the serum levels of BDNF in mood-stabilized bipolar disorder patients are significantly higher than those in healthy controls[93]. The serum levels of pro-BDNF in bipolar disorder patients are significantly lower than those in controls. These studies suggest that pro-BDNF/BDNF is closely related to the pathophysiology of bipolar disorder. However, further studies are required to explore how peripheral pro-BDNF/BDNF affects the pathogenesis of bipolar disorder.
Despite the close correlation between the levels of blood BDNF and various mood disorders, it is still unclear whether BDNF is able to cross the blood-brain barrier. While some studies argue that BDNF cannot directly traverse the blood-brain barrier, others indicate that BDNF is able to be transported[94,95]. Moreover, a number of studies have reported on additional problems related to the poor half-life and rapid degradation of BDNF[94,95]. More importantly, BDNF and pro-BDNF are enriched in human platelets but are undetectable in mice because the BDNF gene is not expressed in mouse megakaryocytes[96]. Therefore, it may be unrealistic to compare the peripheral BDNF levels in the mouse models of mood disorders with those of patients. Beyond the serum or plasma, peripheral BDNF/TrkB or pro-BDNF/p75NTR can be derived from immune cells.
The hypotheses that inflammatory processes contribute to brain-related pathologies such as depressive disorders, has gained popularity particularly because of the activation of immune responses. Might it be possible that some immune cells such as nonspecific leukocytes and lymphocytes produce neurotransmitters and neuropeptides? Notably, immune mediators often interact with neurotransmitter receptors and also modulate neural pathways[97]. In turn, neuropeptides trigger the release of proinflammatory mediators that may amplify or facilitate inflammation by enhancing vasodilation, blood flow, vascular leakiness and leukocyte trafficking to sites of inflammation.
Similarly, BDNF and TrkB are expressed and released from microglia/monocytes, T and B cells. The released BDNF is in turn believed to exert neurotrophic effects[98]. In the CNS, BDNF and TrkB are expressed in the microglia which are the resident macrophages within the brain parenchyma[2]. When the microglia are activated, they can induce Ca2+-response elements then bind to CREB and the calcium-responsive factor to mediate BDNF transcription[99,100]. Additionally, the released BDNF from the microglia can bind to TrkB and this has been implicated in neuropathic pain. However, it is still unclear what role the BDNF in the microglia plays in mood disorders and this requires to be studied further.
In addition, more recent studies have shown that pro-BDNF and p75NTR are also expressed in monocytes, T and B cells and are upregulated in the different immune-mediated inflammatory cells (Figure 2)[101-103]. Previous research on septic mice also showed that pro-BDNF signaling contributes to the development of cognitive dysfunctions by interfering with the functions of immune cells[104]. Moreover, additional studies have shown that pro-BDNF and p75NTR are upregulated in patients with multiple sclerosis as well as in mouse models and this contributes to the dysfunction of immune cells, mediated by pro-BDNF-p75NTR-NF-κB signaling[105]. Our recent study showed that increased expression of proBDNF in M2-like monocytes may be highly associated with proinflammatory responses in the type-A aortic dissection disease[106]. Therefore, use of monoclonal antibodies against pro-BDNF may be a promising treatment to modulate the perturbed immune functions in the immune-mediated inflammatory diseases[105].
It is also reported that there is an increase in the levels of pro-BDNF, p75NTR and sortilin in the peripheral blood mononuclear cells of patients with depression and this is associated with the severity of disease[92]. In addition, both pro-BDNF and p75NTR are significantly upregulated in the lymphocytes of MDD subjects[92]. An early study reported that systemic administration of anti-pro-BDNF antibodies attenuated the depression-like behavior in rats. Given that it is hard for antibodies to reach the brain through the intact blood–brain barrier, it is likely that the therapeutic effect of systemic treatment with anti-pro-BDNF antibodies may be realized by neutralizing the peripheral pro-BDNF. Furthermore, a recent study by our research group showed that there was an increase in the levels of pro-BDNF and p75NTR in the CD11b+ monocytes and macrophages in the intestinal laminar propria of mice under CUMS-induced depression[107].
Upregulation of pro-BDNF/p75NTR in monocytes/macrophage is closely related to the activation of proinflammatory cytokines and gastrointestinal immobility. Our recent study showed that treatment with fluoxetine can inhibit upregulation of pro-BDNF/p75NTR, cytokine activation and attenuate gastrointestinal immobility[107]. These results therefore indicate that pro-BDNF/p75 signaling may be involved in the gut-brain axis during depression. We also used a lipopolysaccharide-induced model of cognitive dysfunction in mice to show that there was an increase in the levels of pro-BDNF/p75NTR in CD4+ T lymphocytes in the meninges. There was also an increase in the levels of the tumor necrosis factor-, interleukin (IL)-1, IL-6 and interferon-. Additionally, systemic administration but not the intracerebroventricular injection of anti-pro-BDNF antibodies attenuated cognitive dysfunction and inhibited the activation of proinflammatory cytokines[108]. A recent study also revealed that pro-BDNF and p75NTR in monocytes played a role in neuroinflammation after chronic infection[109]. Therefore, pro-BDNF/p75NTR signaling derived from immune cells may act as the inflammatory mediators to promote the interaction of neuroimmune during the development of depression or cognitive dysfunction.
BDNF/TrkB and pro-BDNF/p75NTR signaling pathways are widely expressed in different regions of brain. BDNF signaling exert different effects on mood disorders. In contrast, pro-BDNF/p75NTR signaling in CNS mainly promotes the development of mood disorders, such as depression and anxiety. Low levels of BDNF in circulation are negatively correlated with disease severity of depression. It should be noted, however, that BDNF is enriched in platelets and can be detected in human samples whereas BDNF is undetectable in the serum or platelets from mouse. This difference may limit the application of findings about BDNF/pro-BDNF signaling in mice to clinical practice. In contrast, pro-BDNF/p75NTR signaling in immune cells is upregulated in patients with depression or depressive mice. Further studies should investigate the roles of pro-BDNF/p75NTR in the neuroimmune crosstalk during the pathogenesis of mood disorders.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Siniscalco D S-Editor: Gao CC L-Editor: Kerr C P-Editor: Gao CC
| 1. | Racagni G, Popoli M. Cellular and molecular mechanisms in the long-term action of antidepressants. Dialogues Clin Neurosci. 2008;10:385-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Jin Y, Sun LH, Yang W, Cui RJ, Xu SB. The Role of BDNF in the Neuroimmune Axis Regulation of Mood Disorders. Front Neurol. 2019;10:515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 3. | Wittchen HU. The burden of mood disorders. Science. 2012;338:15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Borgonetti V, Les F, López V, Galeotti N. Attenuation of Anxiety-Like Behavior by Helichrysum stoechas (L.) Moench Methanolic Extract through Up-Regulation of ERK Signaling Pathways in Noradrenergic Neurons. Pharmaceuticals (Basel). 2020;13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Bremner JD, Campanella C, Khan Z, Shah M, Hammadah M, Wilmot K, Al Mheid I, Lima BB, Garcia EV, Nye J, Ward L, Kutner MH, Raggi P, Pearce BD, Shah AJ, Quyyumi AA, Vaccarino V. Brain Correlates of Mental Stress-Induced Myocardial Ischemia. Psychosom Med. 2018;80:515-525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Pandey GN, Dwivedi Y, Rizavi HS, Ren X, Zhang H, Pavuluri MN. Brain-derived neurotrophic factor gene and protein expression in pediatric and adult depressed subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:645-651. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Rybakowski JK. BDNF gene: functional Val66Met polymorphism in mood disorders and schizophrenia. Pharmacogenomics. 2008;9:1589-1593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Teixeira AL, Barbosa IG, Diniz BS, Kummer A. Circulating levels of brain-derived neurotrophic factor: correlation with mood, cognition and motor function. Biomark Med. 2010;4:871-887. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 9. | Altar CA. Neurotrophins and depression. Trends Pharmacol Sci. 1999;20:59-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 352] [Cited by in F6Publishing: 384] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 10. | Pruunsild P, Kazantseva A, Aid T, Palm K, Timmusk T. Dissecting the human BDNF locus: bidirectional transcription, complex splicing, and multiple promoters. Genomics. 2007;90:397-406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 466] [Cited by in F6Publishing: 506] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 11. | Moonat S, Pandey SC. Stress, epigenetics, and alcoholism. Alcohol Res. 2012;34:495-505. [PubMed] [Cited in This Article: ] |
| 12. | Roy M, Tapadia MG, Joshi S, Koch B. Molecular and genetic basis of depression. J Genet. 2014;93:879-892. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Gupta VK, You Y, Gupta VB, Klistorner A, Graham SL. TrkB receptor signalling: implications in neurodegenerative, psychiatric and proliferative disorders. Int J Mol Sci. 2013;14:10122-10142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 157] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 14. | Bathina S, Das UN. Brain-derived neurotrophic factor and its clinical implications. Arch Med Sci. 2015;11:1164-1178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 443] [Cited by in F6Publishing: 540] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 15. | Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10:1089-1093. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 797] [Cited by in F6Publishing: 858] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 16. | Yamashita T, Fujitani M, Hata K, Mimura F, Yamagishi S. Diverse functions of the p75 neurotrophin receptor. Anat Sci Int. 2005;80:37-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Reichardt LF. Neurotrophin-regulated signalling pathways. Philos Trans R Soc Lond B Biol Sci. 2006;361:1545-1564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1633] [Cited by in F6Publishing: 1565] [Article Influence: 86.9] [Reference Citation Analysis (0)] |
| 18. | Khursigara G, Bertin J, Yano H, Moffett H, DiStefano PS, Chao MV. A prosurvival function for the p75 receptor death domain mediated via the caspase recruitment domain receptor-interacting protein 2. J Neurosci. 2001;21:5854-5863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 115] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Hamanoue M, Middleton G, Wyatt S, Jaffray E, Hay RT, Davies AM. p75-mediated NF-kappaB activation enhances the survival response of developing sensory neurons to nerve growth factor. Mol Cell Neurosci. 1999;14:28-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 158] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Gentry JJ, Casaccia-Bonnefil P, Carter BD. Nerve growth factor activation of nuclear factor kappaB through its p75 receptor is an anti-apoptotic signal in RN22 schwannoma cells. J Biol Chem. 2000;275:7558-7565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 92] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Fogarty MP, Downer EJ, Campbell V. A role for c-Jun N-terminal kinase 1 (JNK1), but not JNK2, in the beta-amyloid-mediated stabilization of protein p53 and induction of the apoptotic cascade in cultured cortical neurons. Biochem J. 2003;371:789-798. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Bui NT, König HG, Culmsee C, Bauerbach E, Poppe M, Krieglstein J, Prehn JH. p75 neurotrophin receptor is required for constitutive and NGF-induced survival signalling in PC12 cells and rat hippocampal neurones. J Neurochem. 2002;81:594-605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Omelchenko A, Firestein BL. Axonal Development: RhoA Restrains but Does Not Specify. Curr Biol. 2019;29:R1179-R1181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Yamashita T, Tohyama M. The p75 receptor acts as a displacement factor that releases Rho from Rho-GDI. Nat Neurosci. 2003;6:461-467. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 358] [Cited by in F6Publishing: 351] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 25. | Yamashita T, Tucker KL, Barde YA. Neurotrophin binding to the p75 receptor modulates Rho activity and axonal outgrowth. Neuron. 1999;24:585-593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 369] [Cited by in F6Publishing: 399] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 26. | Hasegawa Y, Fujitani M, Hata K, Tohyama M, Yamagishi S, Yamashita T. Promotion of axon regeneration by myelin-associated glycoprotein and Nogo through divergent signals downstream of Gi/G. J Neurosci. 2004;24:6826-6832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Gehler S, Gallo G, Veien E, Letourneau PC. p75 neurotrophin receptor signaling regulates growth cone filopodial dynamics through modulating RhoA activity. J Neurosci. 2004;24:4363-4372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 28. | Akhter R, Sanphui P, Das H, Saha P, Biswas SC. The regulation of p53 up-regulated modulator of apoptosis by JNK/c-Jun pathway in β-amyloid-induced neuron death. J Neurochem. 2015;134:1091-1103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 29. | Kenchappa RS, Tep C, Korade Z, Urra S, Bronfman FC, Yoon SO, Carter BD. p75 neurotrophin receptor-mediated apoptosis in sympathetic neurons involves a biphasic activation of JNK and up-regulation of tumor necrosis factor-alpha-converting enzyme/ADAM17. J Biol Chem. 2010;285:20358-20368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 30. | Huang P, Gao T, Dong Z, Zhou C, Lai Y, Pan T, Liu Y, Zhao X, Sun X, Hua H, Wen G, Gao L, Lv Z. Neural circuitry among connecting the hippocampus, prefrontal cortex and basolateral amygdala in a mouse depression model: Associations correlations between BDNF levels and BOLD - fMRI signals. Brain Res Bull. 2018;142:107-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 31. | Ressler KJ, Mayberg HS. Targeting abnormal neural circuits in mood and anxiety disorders: from the laboratory to the clinic. Nat Neurosci. 2007;10:1116-1124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 664] [Cited by in F6Publishing: 683] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 32. | Ide S, Kakeda S, Watanabe K, Yoshimura R, Abe O, Hayashi K, Ueda I, Kishi T, Katsuki A, Umene-Nakano W, Iwata N, Nakamura J, Korogi Y. Relationship between a BDNF gene polymorphism and the brain volume in treatment-naive patients with major depressive disorder: A VBM analysis of brain MRI. Psychiatry Res. 2015;233:120-124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Lütcke H, Murayama M, Hahn T, Margolis DJ, Astori S, Zum Alten Borgloh SM, Göbel W, Yang Y, Tang W, Kügler S, Sprengel R, Nagai T, Miyawaki A, Larkum ME, Helmchen F, Hasan MT. Optical recording of neuronal activity with a genetically-encoded calcium indicator in anesthetized and freely moving mice. Front Neural Circuits. 2010;4:9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 34. | Foster JA, MacQueen G. Neurobiological factors linking personality traits and major depression. Can J Psychiatry. 2008;53:6-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Krystal AD, Weiner RD. EEG correlates of the response to ECT: a possible antidepressant role of brain-derived neurotrophic factor. J ECT. 1999;15:27-38. [PubMed] [Cited in This Article: ] |
| 36. | Kafetzopoulos V, Kokras N, Sotiropoulos I, Oliveira JF, Leite-Almeida H, Vasalou A, Sardinha VM, Papadopoulou-Daifoti Z, Almeida OFX, Antoniou K, Sousa N, Dalla C. The nucleus reuniens: a key node in the neurocircuitry of stress and depression. Mol Psychiatry. 2018;23:579-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 37. | Rao U. Biomarkers in pediatric depression. Depress Anxiety. 2013;30:787-791. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 38. | Krishnan V, Nestler EJ. Linking molecules to mood: new insight into the biology of depression. Am J Psychiatry. 2010;167:1305-1320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 469] [Cited by in F6Publishing: 446] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 39. | Blendy JA. The role of CREB in depression and antidepressant treatment. Biol Psychiatry. 2006;59:1144-1150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 260] [Cited by in F6Publishing: 269] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 40. | Li Y, Luikart BW, Birnbaum S, Chen J, Kwon CH, Kernie SG, Bassel-Duby R, Parada LF. TrkB regulates hippocampal neurogenesis and governs sensitivity to antidepressive treatment. Neuron. 2008;59:399-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 443] [Cited by in F6Publishing: 472] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 41. | Ma Z, Zang T, Birnbaum SG, Wang Z, Johnson JE, Zhang CL, Parada LF. TrkB dependent adult hippocampal progenitor differentiation mediates sustained ketamine antidepressant response. Nat Commun. 2017;8:1668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 42. | Bai YY, Ruan CS, Yang CR, Li JY, Kang ZL, Zhou L, Liu D, Zeng YQ, Wang TH, Tian CF, Liao H, Bobrovskaya L, Zhou XF. ProBDNF Signaling Regulates Depression-Like Behaviors in Rodents under Chronic Stress. Neuropsychopharmacology. 2016;41:2882-2892. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 43. | Yang J, Harte-Hargrove LC, Siao CJ, Marinic T, Clarke R, Ma Q, Jing D, Lafrancois JJ, Bath KG, Mark W, Ballon D, Lee FS, Scharfman HE, Hempstead BL. proBDNF negatively regulates neuronal remodeling, synaptic transmission, and synaptic plasticity in hippocampus. Cell Rep. 2014;7:796-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 221] [Cited by in F6Publishing: 202] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 44. | Zhong F, Liu L, Wei JL, Hu ZL, Li L, Wang S, Xu JM, Zhou XF, Li CQ, Yang ZY, Dai RP. Brain-Derived Neurotrophic Factor Precursor in the Hippocampus Regulates Both Depressive and Anxiety-Like Behaviors in Rats. Front Psychiatry. 2018;9:776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 45. | Dunham JS, Deakin JF, Miyajima F, Payton A, Toro CT. Expression of hippocampal brain-derived neurotrophic factor and its receptors in Stanley consortium brains. J Psychiatr Res. 2009;43:1175-1184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 129] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 46. | Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Struct Funct. 2008;213:93-118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1560] [Cited by in F6Publishing: 1477] [Article Influence: 92.3] [Reference Citation Analysis (0)] |
| 47. | Wu Y, Wei Z, Li Y, Wei C, Cheng P, Xu H, Li Z, Guo R, Qi X, Jia J, Jia Y, Wang W, Gao X. Perturbation of Ephrin Receptor Signaling and Glutamatergic Transmission in the Hypothalamus in Depression Using Proteomics Integrated With Metabolomics. Front Neurosci. 2019;13:1359. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 48. | Gelfo F, Tirassa P, De Bartolo P, Croce N, Bernardini S, Caltagirone C, Petrosini L, Angelucci F. NPY intraperitoneal injections produce antidepressant-like effects and downregulate BDNF in the rat hypothalamus. CNS Neurosci Ther. 2012;18:487-492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 49. | Angelucci F, Ricci E, Padua L, Sabino A, Tonali PA. Music exposure differentially alters the levels of brain-derived neurotrophic factor and nerve growth factor in the mouse hypothalamus. Neurosci Lett. 2007;429:152-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 50. | Segi-Nishida E, Sukeno M, Imoto Y, Kira T, Sakaida M, Tsuchiya S, Sugimoto Y, Okuno Y. Electroconvulsive seizures activate anorexigenic signals in the ventromedial nuclei of the hypothalamus. Neuropharmacology. 2013;71:164-173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 51. | Pang C, Cao L, Wu F, Wang L, Wang G, Yu Y, Zhang M, Chen L, Wang W, Lv W, Zhu J, Pan J, Zhang H, Xu Y, Ding L. The effect of trans-resveratrol on post-stroke depression via regulation of hypothalamus-pituitary-adrenal axis. Neuropharmacology. 2015;97:447-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 52. | Qi XR, Zhao J, Liu J, Fang H, Swaab DF, Zhou JN. Abnormal retinoid and TrkB signaling in the prefrontal cortex in mood disorders. Cereb Cortex. 2015;25:75-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 53. | Almeida FB, Gomez R, Barros HMT, Nin MS. Hemisphere-dependent Changes in mRNA Expression of GABAA Receptor Subunits and BDNF after Intra-prefrontal Cortex Allopregnanolone Infusion in Rats. Neuroscience. 2019;397:56-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 54. | Gourley SL, Swanson AM, Jacobs AM, Howell JL, Mo M, Dileone RJ, Koleske AJ, Taylor JR. Action control is mediated by prefrontal BDNF and glucocorticoid receptor binding. Proc Natl Acad Sci U S A. 2012;109:20714-20719. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 93] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 55. | Tripp A, Oh H, Guilloux JP, Martinowich K, Lewis DA, Sibille E. Brain-derived neurotrophic factor signaling and subgenual anterior cingulate cortex dysfunction in major depressive disorder. Am J Psychiatry. 2012;169:1194-1202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 188] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 56. | Deng Y, Zhang CH, Zhang HN. [Effects of chaihu shugan powder on the behavior and expressions of BDNF and TrkB in the hippocampus, amygdala, and the frontal lobe in rat model of depression]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2011;31:1373-1378. [PubMed] [Cited in This Article: ] |
| 57. | Yang CR, Bai YY, Ruan CS, Zhou FH, Li F, Li CQ, Zhou XF. Injection of Anti-proBDNF in Anterior Cingulate Cortex (ACC) Reverses Chronic Stress-Induced Adverse Mood Behaviors in Mice. Neurotox Res. 2017;31:298-308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 58. | Ruchalski K, Hathout GM. A medley of midbrain maladies: a brief review of midbrain anatomy and syndromology for radiologists. Radiol Res Pract. 2012;2012:258524. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 59. | Casarotto PC, de Bortoli VC, Corrêa FM, Resstel LB, Zangrossi H Jr. Panicolytic-like effect of BDNF in the rat dorsal periaqueductal grey matter: the role of 5-HT and GABA. Int J Neuropsychopharmacol. 2010;13:573-582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 60. | Kozicz T, Tilburg-Ouwens D, Faludi G, Palkovits M, Roubos E. Gender-related urocortin 1 and brain-derived neurotrophic factor expression in the adult human midbrain of suicide victims with major depression. Neuroscience. 2008;152:1015-1023. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 61. | Siuciak JA, Lewis DR, Wiegand SJ, Lindsay RM. Antidepressant-like effect of brain-derived neurotrophic factor (BDNF). Pharmacol Biochem Behav. 1997;56:131-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 623] [Cited by in F6Publishing: 622] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 62. | Yang PS, Peng HY, Lin TB, Hsieh MC, Lai CY, Lee AS, Wang HH, Ho YC. NMDA receptor partial agonist GLYX-13 alleviates chronic stress-induced depression-like behavior through enhancement of AMPA receptor function in the periaqueductal gray. Neuropharmacology. 2020;178:108269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 63. | Duman RS. Role of neurotrophic factors in the etiology and treatment of mood disorders. Neuromolecular Med. 2004;5:11-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 397] [Cited by in F6Publishing: 417] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 64. | Kraus C, Castrén E, Kasper S, Lanzenberger R. Serotonin and neuroplasticity - Links between molecular, functional and structural pathophysiology in depression. Neurosci Biobehav Rev. 2017;77:317-326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 206] [Cited by in F6Publishing: 243] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 65. | Chhibber A, Woody SK, Karim Rumi MA, Soares MJ, Zhao L. Estrogen receptor β deficiency impairs BDNF-5-HT2A signaling in the hippocampus of female brain: A possible mechanism for menopausal depression. Psychoneuroendocrinology. 2017;82:107-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 66. | Amigó J, Díaz A, Pilar-Cuéllar F, Vidal R, Martín A, Compan V, Pazos A, Castro E. The absence of 5-HT4 receptors modulates depression- and anxiety-like responses and influences the response of fluoxetine in olfactory bulbectomised mice: Adaptive changes in hippocampal neuroplasticity markers and 5-HT1A autoreceptor. Neuropharmacology. 2016;111:47-58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 67. | Douma EH, de Kloet ER. Stress-induced plasticity and functioning of ventral tegmental dopamine neurons. Neurosci Biobehav Rev. 2020;108:48-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 97] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 68. | Quintero GC. Role of nucleus accumbens glutamatergic plasticity in drug addiction. Neuropsychiatr Dis Treat. 2013;9:1499-1512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 69. | Autry AE, Monteggia LM. Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev. 2012;64:238-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 862] [Cited by in F6Publishing: 920] [Article Influence: 76.7] [Reference Citation Analysis (0)] |
| 70. | Reddy-Thootkur M, Kraguljac NV, Lahti AC. The role of glutamate and GABA in cognitive dysfunction in schizophrenia and mood disorders - A systematic review of magnetic resonance spectroscopy studies. Schizophr Res. 2020;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 41] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 71. | Fogaça MV, Duman RS. Cortical GABAergic Dysfunction in Stress and Depression: New Insights for Therapeutic Interventions. Front Cell Neurosci. 2019;13:87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 143] [Cited by in F6Publishing: 184] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 72. | Kerman IA. New insights into BDNF signaling: relevance to major depression and antidepressant action. Am J Psychiatry. 2012;169:1137-1140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 73. | Zhu G, Sun X, Yang Y, Du Y, Lin Y, Xiang J, Zhou N. Reduction of BDNF results in GABAergic neuroplasticity dysfunction and contributes to late-life anxiety disorder. Behav Neurosci. 2019;133:212-224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 74. | Sakata K, Woo NH, Martinowich K, Greene JS, Schloesser RJ, Shen L, Lu B. Critical role of promoter IV-driven BDNF transcription in GABAergic transmission and synaptic plasticity in the prefrontal cortex. Proc Natl Acad Sci U S A. 2009;106:5942-5947. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 151] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 75. | Calabrese F, Guidotti G, Middelman A, Racagni G, Homberg J, Riva MA. Lack of serotonin transporter alters BDNF expression in the rat brain during early postnatal development. Mol Neurobiol. 2013;48:244-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 76. | Zhao L, Levine ES. BDNF-endocannabinoid interactions at neocortical inhibitory synapses require phospholipase C signaling. J Neurophysiol. 2014;111:1008-1015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 77. | Ninan I. Synaptic regulation of affective behaviors; role of BDNF. Neuropharmacology. 2014;76 Pt C:684-695. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 78. | Björkholm C, Monteggia LM. BDNF - a key transducer of antidepressant effects. Neuropharmacology. 2016;102:72-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 493] [Cited by in F6Publishing: 610] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 79. | Pereira DB, Rebola N, Rodrigues RJ, Cunha RA, Carvalho AP, Duarte CB. Trkb receptors modulation of glutamate release is limited to a subset of nerve terminals in the adult rat hippocampus. J Neurosci Res. 2006;83:832-844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 80. | Niu Z, Yang L, Wu X, Zhu Y, Chen J, Fang Y. The Relationship Between Neuroimmunity and Bipolar Disorder: Mechanism and Translational Application. Neurosci Bull. 2019;35:595-607. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 81. | Dantzer R. Neuroimmune Interactions: From the Brain to the Immune System and Vice Versa. Physiol Rev. 2018;98:477-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 547] [Cited by in F6Publishing: 491] [Article Influence: 81.8] [Reference Citation Analysis (0)] |
| 82. | Rowland T, Perry BI, Upthegrove R, Barnes N, Chatterjee J, Gallacher D, Marwaha S. Neurotrophins, cytokines, oxidative stress mediators and mood state in bipolar disorder: systematic review and meta-analyses. Br J Psychiatry. 2018;213:514-525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 110] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 83. | Sagar R, Pattanayak RD. Potential biomarkers for bipolar disorder: Where do we stand? Indian J Med Res. 2017;145:7-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 84. | Lopes TDS, Silva WDS, Ribeiro SB, Figueiredo CA, Campbell FQ, Daltro GC, Valenzuela A, Montoya P, Lucena RCS, Baptista AF. Does Transcranial Direct Current Stimulation Combined with Peripheral Electrical Stimulation Have an Additive Effect in the Control of Hip Joint Osteonecrosis Pain Associated with Sickle Cell Disease? Front Hum Neurosci. 2017;11:633. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 85. | Fernandes BS, Molendijk ML, Köhler CA, Soares JC, Leite CM, Machado-Vieira R, Ribeiro TL, Silva JC, Sales PM, Quevedo J, Oertel-Knöchel V, Vieta E, González-Pinto A, Berk M, Carvalho AF. Peripheral brain-derived neurotrophic factor (BDNF) as a biomarker in bipolar disorder: a meta-analysis of 52 studies. BMC Med. 2015;13:289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 174] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 86. | Cevher Binici N, Inal Emiroğlu FN, Resmi H, Ellidokuz H. Serum Brain-derived Neurotrophic Factor Levels among Euthymic Adolescents with Bipolar Disorder Type I. Noro Psikiyatr Ars. 2016;53:267-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 87. | Lin CC, Huang TL. Brain-derived neurotrophic factor and mental disorders. Biomed J. 2020;43:134-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 88. | Diniz BS. Decreased Brain-Derived Neurotrophic Factor (BDNF) in Older Adults with Bipolar Disorder: Meaning and Utility? Am J Geriatr Psychiatry. 2016;24:602-603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 89. | Lin CC, Lee CT, Lo YT, Huang TL. Brain-derived neurotrophic factor protein and mRNA levels in patients with bipolar mania - A preliminary study. Biomed J. 2016;39:272-276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 90. | Södersten K, Pålsson E, Ishima T, Funa K, Landén M, Hashimoto K, Ågren H. Abnormality in serum levels of mature brain-derived neurotrophic factor (BDNF) and its precursor proBDNF in mood-stabilized patients with bipolar disorder: a study of two independent cohorts. J Affect Disord. 2014;160:1-9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 91. | Pandey GN, Rizavi HS, Dwivedi Y, Pavuluri MN. Brain-derived neurotrophic factor gene expression in pediatric bipolar disorder: effects of treatment and clinical response. J Am Acad Child Adolesc Psychiatry. 2008;47:1077-1085. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 92. | Rybakowski JK. Response to lithium in bipolar disorder: clinical and genetic findings. ACS Chem Neurosci. 2014;5:413-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 93. | Yasuda S, Liang MH, Marinova Z, Yahyavi A, Chuang DM. The mood stabilizers lithium and valproate selectively activate the promoter IV of brain-derived neurotrophic factor in neurons. Mol Psychiatry. 2009;14:51-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 246] [Cited by in F6Publishing: 246] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 94. | Zhou L, Xiong J, Lim Y, Ruan Y, Huang C, Zhu Y, Zhong JH, Xiao Z, Zhou XF. Upregulation of blood proBDNF and its receptors in major depression. J Affect Disord. 2013;150:776-784. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 111] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 95. | Hashimoto K. Ethnic differences in the serum levels of proBDNF, a precursor of brain-derived neurotrophic factor (BDNF), in mood disorders. Eur Arch Psychiatry Clin Neurosci. 2016;266:285-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 96. | Tosi G, Duskey JT, Kreuter J. Nanoparticles as carriers for drug delivery of macromolecules across the blood-brain barrier. Expert Opin Drug Deliv. 2020;17:23-32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 97. | Molinari C, Morsanuto V, Ruga S, Notte F, Farghali M, Galla R, Uberti F. The Role of BDNF on Aging-Modulation Markers. Brain Sci. 2020;10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 98. | Chacón-Fernández P, Säuberli K, Colzani M, Moreau T, Ghevaert C, Barde YA. Brain-derived Neurotrophic Factor in Megakaryocytes. J Biol Chem. 2016;291:9872-9881. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 128] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 99. | Cox MA, Duncan GS, Lin GHY, Steinberg BE, Yu LX, Brenner D, Buckler LN, Elia AJ, Wakeham AC, Nieman B, Dominguez-Brauer C, Elford AR, Gill KT, Kubli SP, Haight J, Berger T, Ohashi PS, Tracey KJ, Olofsson PS, Mak TW. Choline acetyltransferase-expressing T cells are required to control chronic viral infection. Science. 2019;363:639-644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 100. | Kerschensteiner M, Gallmeier E, Behrens L, Leal VV, Misgeld T, Klinkert WE, Kolbeck R, Hoppe E, Oropeza-Wekerle RL, Bartke I, Stadelmann C, Lassmann H, Wekerle H, Hohlfeld R. Activated human T cells, B cells, and monocytes produce brain-derived neurotrophic factor in vitro and in inflammatory brain lesions: a neuroprotective role of inflammation? J Exp Med. 1999;189:865-870. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 757] [Cited by in F6Publishing: 752] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 101. | Lu Q, Qu Y, Ding Y, Kang X. p75NTR/proBDNF Modulates Basal Cell Carcinoma (BCC) Immune Microenvironment via Necroptosis Signaling Pathway. J Immunol Res. 2021;2021:6652846. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 102. | Tao X, West AE, Chen WG, Corfas G, Greenberg ME. A calcium-responsive transcription factor, CaRF, that regulates neuronal activity-dependent expression of BDNF. Neuron. 2002;33:383-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 249] [Cited by in F6Publishing: 260] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 103. | Zheng F, Zhou X, Moon C, Wang H. Regulation of brain-derived neurotrophic factor expression in neurons. Int J Physiol Pathophysiol Pharmacol. 2012;4:188-200. [PubMed] [Cited in This Article: ] |
| 104. | Fauchais AL, Lalloué F, Lise MC, Boumediene A, Preud'homme JL, Vidal E, Jauberteau MO. Role of endogenous brain-derived neurotrophic factor and sortilin in B cell survival. J Immunol. 2008;181:3027-3038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 105. | Zhou XF, Song XY, Zhong JH, Barati S, Zhou FH, Johnson SM. Distribution and localization of pro-brain-derived neurotrophic factor-like immunoreactivity in the peripheral and central nervous system of the adult rat. J Neurochem. 2004;91:704-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 106. | Schuhmann B, Dietrich A, Sel S, Hahn C, Klingenspor M, Lommatzsch M, Gudermann T, Braun A, Renz H, Nockher WA. A role for brain-derived neurotrophic factor in B cell development. J Neuroimmunol. 2005;163:15-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 107. | Kozlov EM, Grechko AV, Chegodaev YS, Wu WK, Orekhov AN. Contribution of Neurotrophins to the Immune System Regulation and Possible Connection to Alcohol Addiction. Biology (Basel). 2020;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 108. | Hu ZL, Luo C, Hurtado PR, Li H, Wang S, Hu B, Xu JM, Liu Y, Feng SQ, Hurtado-Perez E, Chen K, Zhou XF, Li CQ, Dai RP. Brain-derived neurotrophic factor precursor in the immune system is a novel target for treating multiple sclerosis. Theranostics. 2021;11:715-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 109. | Shen WY, Luo C, Reinaldo Hurtado P, Hurtado-Perez E, Luo RY, Hu ZL, Li H, Xu JM, Zhou XF, Dai RP. The regulatory role of ProBDNF in monocyte function: Implications in Stanford type-A aortic dissection disease. FASEB J. 2020;34:2541-2553. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |