Published online May 25, 2017. doi: 10.5495/wjcid.v7.i2.32
Peer-review started: April 19, 2016
First decision: May 17, 2016
Revised: January 31, 2017
Accepted: February 20, 2017
Article in press: February 21, 2017
Published online: May 25, 2017
Cryptosporidiosis, better known as an intestinal disease may disseminate to infect other sites including the respiratory tract. Little information however is available on respiratory cryptosporidiosis that may largely be due to lower frequency of respiratory cryptosporidiosis. Respiratory cryptosporidiosis has been majorly reported in immunocompromised individuals and children. Here we report a case of respiratory and intestinal cryptosporidiosis in a fifteen months old child with CD8+ deficiency. The patient in spite of treatment with Nitazoxanide and Azithromycin followed by Intravenous immunoglobulin and Bovine colostrum had a fatal outcome. The Cryptosporidium spp. isolate was subjected to molecular characterization. The Cryptosporidium spp. was identified both in stool specimen and Endotracheal aspirate (ETA). The blood sample was negative for Cryptosporidium spp. The Cryptosporidium spp. isolate from stool as well as ETA was identified as Cryptosporidium hominis (C. hominis) using Multiplex Allele Specific Polymerase Chain Reaction assay and was subtyped as IaA23G1R1 subtype using gp60 gene polymerase chain reaction assay followed by sequencing.
Core tip: Disseminated cryptosporidiosis has rarely been reported because of the lower frequency as compared to intestinal cryptosporidiosis. Here we describe a case of patient who developed intestinal cryptosporidiosis followed by respiratory cryptosporidiosis. The Cryptosporidium isolate was identified as Cryptosporidium hominis subtype IaA23R2.
- Citation: Khalil S, Mirdha BR, Paul J, Panda A, Singh Y. Disseminated cryptosporidiosis: Case report and literature review. World J Clin Infect Dis 2017; 7(2): 32-37
- URL: https://www.wjgnet.com/2220-3176/full/v7/i2/32.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v7.i2.32
Cryptosporidium species are globally important enteric protozoan parasites with infection most commonly observed in immunocompromised individuals and children[1]. It is mainly presented as diarrheal disease leading to significant morbidity and mortality in developing countries especially the rural areas[2,3]. Cryptosporidium is one of the leading causes of infectious diarrhea in Indian children with prevalence ranging from 1.1%-18.9%[4].
In immunocompetent individuals cryptosporidial diarrhea is transient self-limiting illness[5]. Infections amongst immunocompromised individuals may also become extra-intestinal, spreading to other sites including the gall bladder, biliary tract, pancreas and pulmonary system[5] and possible dissemination may occur through haematogenous route as post-mortem observation has shown the presence of Cryptosporidium spp. in the lumen of sub-mucosal colonic blood vessels[6]. Respiratory cryptosporidiosis can occur in immunocompetent children suffering from cryptosporidial diarrhea with unexplained cough[7]. In humans, it was first reported in 1984 in a patient with symptoms of chronic cough, fever, tachypnea, dyspnea with chest radiographs, findings consistent with interstitial pneumonia[8]. Several other cases of respiratory cryptosporidiosis have been reported albeit the relative rarity of the disease. It is postulated that involvement of the respiratory tract may result in transmission of Cryptosporidium oocysts by aerosols and fomites.
Present report describes the detection, identification and subtyping of a Cryptosporidium spp. detected in the respiratory secretions [Endotracheal aspirate (ETA)] in a fifteen months old child with CD8+ immunodeficiency. Genus specific 18S rRNA gene polymerase chain reaction (PCR) assay was used to detect Cryptosporidium spp., where as Multiplex Allele Specific (MAS) PCR assay was used to identify the species of Cryptosporidium. The gp60 gene was targeted for PCR assay followed by sequencing for subtyping.
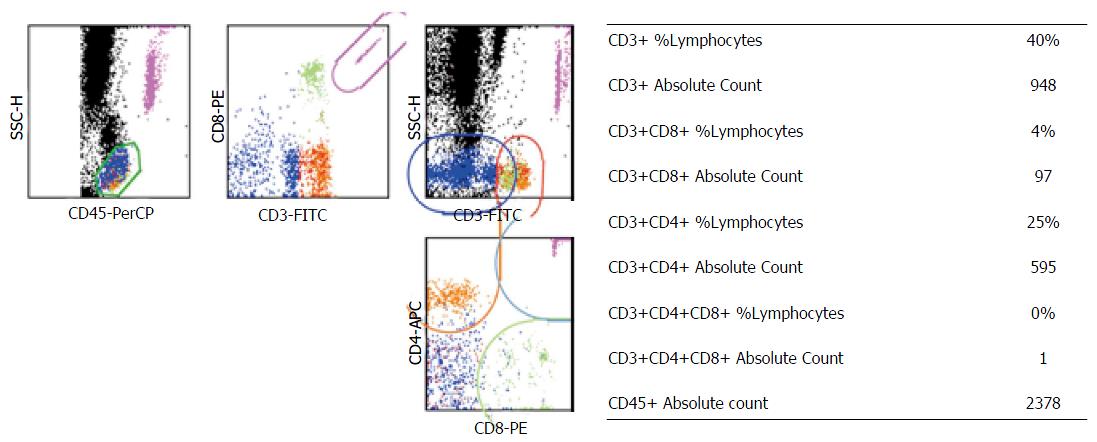
A fifteen months old male child with the complaints of fever and rapid breathing for at least two weeks along with cough and vomiting was admitted to the pediatric in-patient department of our tertiary care hospital. Patient had a history of recurrent fever since two and half months with each episode lasting for 10-15 d with an intermittent non-febrile stage of nearly a week. Child had decreased appetite and had lost approximately 500 g of body weight within three months. On admission the child was emaciated and severely malnourished. The patient was fourth child to a non consanguineous couple and was a follow up case of disseminated Cytomegalovirus (CMV) infection, periodic neutropenia, and Iron deficiency anaemia with CD8+ immunodeficiency. The CD4+ and CD8+ counts of child are given in Figure 1.
The patient’s main clinical and laboratory findings on admission were as follows: Tachycardia (166/min), Tachypnea (52/min), fever (99 °C), severe anaemia (6.8 g/dL), neutropenia [Total Leukocyte Count (3600/μL); Neutrophils (40%)] and normal Platelet count (5.25 × 105/μL). Serum biochemicals revealed normal kidney function [blood urea (15 mg/dL), Creatinine (0.2 mg/dL)]. Deranged Serum Glutamic Oxaloacetic Transaminase (99 IU) and elevated Alkaline phosphatase (565 IU) were observed. Serum immunoglobulin levels were normal (IgG-1137 mg/dL, IgA-108 mg/dL, IgM 102 mg/dL). Anthropometric measurements revealed Z-scores less than 3 [head circumference (41.5 cm); body weight (4.6 kg) and height (61 cm)] suggesting severe malnutrition. During present admission child was given prophylaxis of Fluconazole (25 mg once daily), Co-trimoxazole (20 mg/kg per day), lactose free diet as well as anti reflux measures. Urine and blood samples were sent for microbiological investigations and treatment for Severe Acute Malnutrition was started.
Urine culture was positive for Escherichia coli (> 105 CFU/mL) sensitive to Amikacin/Nitrofurantoin/Zosyn. Blood culture did not show growth of any pathogenic organism. Patient was started with combination of Injection (Inj) Piperacillin and Tazobactam 470 mg IV thrice a day along with Inj Amikacin 75 mg OD, Inj Vit K 2 mg, Syp cetrizine 2.5 mL (OD), Tab lanzol (Lansoprazole) 5 mg OD. In addition, Inj Magnesium sulphate 1 mL OD, Syp Zinc 2.5 mL OD, Folic acid tablets 5 mg OD then 1 mg OD, Syp Calcium carbonate and vitamin D3 2.5 mL OD, syp Atoz Multivitamin 2.5 mL OD along with the prophylaxis of Co-trimoxazole and Fluconazole.
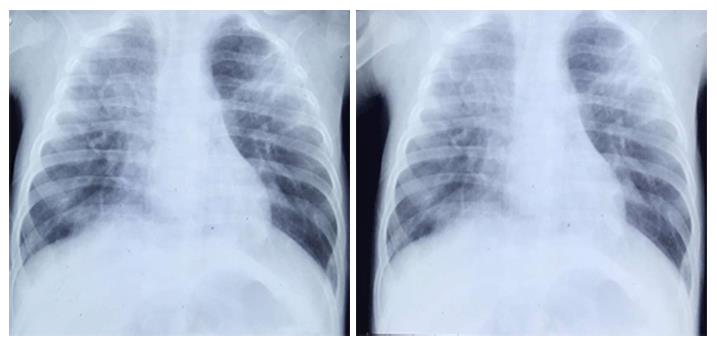
On third day of admission patient was afebrile, there was no vomiting and was accepting the oral feed well, however, he subsequently developed diarrhea with a frequency of up to 20 stools in a day. Domperidone and Cinnarizine combination syrup at a dosage of 1 mL thrice daily was started and urine and blood samples were again sent for microbiological investigations along with the stool sample. All the clinical samples after all the microbiological investigations were negative for any pathogens except the stool sample that showed high load of Cryptosporidium spp. Oocysts, i.e., upto 30 oocysts present per high power field. Syrup Nitazoxanide (NTZ) at a dose of 100 mg/5 mL twice daily and Azithromycin (AZ) at a dose of 45 mg/20 mL in normal Saline was given intravenously. However, diarrhea did not improve even after a week of continuous NTZ and AZ treatment. To circumvent this unresolving cryptosporidial diarrhea, Intravenous Immunoglobulin and Bovine Colostrum were started along with NTZ and AZ. After 24-48 h of this treatment there was no improvement in diarrheal symptoms and child began to develop respiratory distress with tachypnea and cool peripheries and further worsening. Chest X-ray showed bilateral infiltrates (Figure 2). Several causal possibilities of bilateral pneumonia were considered that included reactivation of CMV infection, Pneumocystis jirovecii Pneumonia, respiratory cryptosporidiosis as well as fungal sepsis. Amphotericin B was added for treatment of fungal sepsis and Co-trimoxazole dose was increased. On tenth day child had further worsening with increased heart rate (128/min), respiratory rate of 100/min along with increased frequency of voluminous diarrhea. Child was intubated and ventilated. Stool, endotracheal aspirate and blood samples were further sent for investigation with a special reference to detect presence of Cryptosporidium spp. oocysts. Child showed no signs of improvement and died. The primary reason leading to death was ascribed to disseminated cryptosporidiosis, with antecedent causes including immunodeficiency, periodic neutropenia and disseminated CMV infection.
The samples of stool, blood and ETA received in our laboratory were subjected to molecular analyses using primers given in Table 1. DNA was extracted from stool sample using QIAmp DNA stool minikit (Qiagen, United States) and blood and ETA using QIAmp Easy Blood and Tissue minikit (Qiagen, United States). The DNA from these three samples was subjected to diagnostic PCR assay using genus specific 18S rRNA gene primers. For identification of species Multiplex Allele Specific PCR assay targeting DHFR gene was used. For subtyping GP60 gene was targeted. Gel based extraction of the PCR products was performed as per the manufacturer’s instructions using MinElute gel extraction kit (Qiagen, United States). Sequencing for the study isolates was performed in both forward and reverse direction on ABI 3500xL Genetic Analyzer from Chromous Biotech. Consensus sequences were pairwise aligned using Clustal W and were manually refined using the BioEdit program version 7.0.4.
| Gene (Ref.) | Primers | Amplicon size |
| 18S rRNA[9] | CPB-DIAGF: 5’AGCTCGTAGTTGGATTTCTG-3’ | 435 bp |
| CPB-DIAGR: 5’-TAAGGTGCTGAAGGAGTAAGG-3’ | ||
| MAS PCR[10] | CINF: 5’GTGGGGATTTAACTTGATTT 3’ | 575 bp |
| CINR: 5’GGTATTTCTGGGAAATAAGT3’ | 357 bp | |
| 1R: 5’GCTGGAGGAAATAACGACAATTA3’ | 190 bp | |
| 2R: 5’TGTCCGTTAATTCCTATTCCTCTA3’ | ||
| GP60[11] | F1: 5’-ATAGTCTCCGCTGTATTC-3’ | 800-850 bp |
| R1: 5’-GGAAGGAACGATGTATCT-3’ | ||
| F2: 5’-TCCGCTGTATTCTCAGCC-3’ | ||
| R2: 5’ GCAGAGGAACCAGCATC-3’ |
A band size of 435 bp was obtained from DNA extracted both from stool sample as well as ETA showing the presence of Cryptosporidium spp. oocysts in both the samples. However, there was no amplification of cryptosporidial DNA from blood sample. MAS-PCR assay showed amplification of DNA bands suggestive of Cryptosporidium hominis (C. hominis). The desired band was obtained using gp60 gene based PCR assay and the amplified products were sequenced. The sequences of gp60 gene from both the sample identified them as Ia subtype family and IaA23G1R1 subtype. The sequence was submitted to genbank under Accession number KU169227.
Cryptosporidium spp. affects mainly the small intestines but infections of hepatic ducts, lungs and conjunctiva has also been reported[12,13]. However, a few case reports of respiratory cryptosporidiosis in human immunodeficiency virus (HIV)/AIDS cases are available[13]. Respiratory cryptosporidiosis is mostly presented as cough, dyspnea, low fever and abnormal chest X-ray with interstitial pneumopathy[14], with an unknown pathogenesis[15].
Respiratory route of Cryptosporidium transmission was suggested as results of epidemiological studies in children presumed to be immunocompetent. In a study from Switzerland, children with cryptosporidial diarrhea were more likely to have respiratory symptoms compared to those who had other infections, suggesting that respiratory infection may be common but transient in healthy individuals[16]. In a study from rural Brazil and Bangladesh, 50% and 33% of children with intestinal cryptosporidiosis had unexplained respiratory symptoms, respectively[17,18]. In a report from Gaza, 50% of children with cryptosporidial diarrhea and 10% of children without cryptosporidial diarrhea had respiratory symptoms and were also shedding Cryptosporidium in feces[19]. These findings led to the speculation that the respiratory system may serve as a viable alternative for Cryptosporidium propagation, transmission, and diagnosis, with or without apparent respiratory symptoms. Kumar et al[20], (2016) reported disseminated cryptosporidiosis in a 35 year old immunocompetent patient in India which was successfully treated with nitazoxanide.
In addition human respiratory cryptosporidiosis has been observed in patients with compromised cellular immunity as well as in individuals with induced immunosuppression; hence an association between cryptosporidiosis and depleted CD4+ T-cell count was established[6,15,21]. Disseminated cryptosporidiosis was reported in a child with nephrotic syndrome receiving immunosuppression[15].
In the present case, intestinal cryptosporidiosis was followed by respiratory cryptosporidiosis. Earlier studies have shown disseminated cryptosporidiosis originating from the intestinal tract infection. Subsequently cases of respiratory cryptosporidiosis lacking evidence of primary gastrointestinal involvement suggest the possibility of respiratory transmission of cryptosporidiosis[13,14]. The pathogenesis of Cryptosporidium spp. lung infection is still unclear. Infection can result from the inhalation of oocysts after vomiting or the hematogenous spread of the oocysts. Although intestinal Cryptosporidium spp. organisms are not usually invasive, oocysts have been found inside macrophages, which can have defective phagocyte killing ability[22]. In fact, Cryptosporidium spp. organisms can multiply in macrophages in vitro[23], suggesting that extraintestinal parasites might spread via circulating phagocytes. Regardless of the route of infection patients with disseminated cryptosporidiosis experience fulminant disease, fail to respond to existing therapies and have fatal outcome.
Human health risk is often compounded because there is only one Food and Drug Administration approved therapeutic agent, i.e., NTZ. It reduces the duration of diarrhea and oocyst shedding in both immunocompetent and immunocompromised[24,25]. The patient was initially treated with nitazoxanide, however no improvement was seen in diarrhea and was later started with the combination therapy. Higher doses and longer duration of therapy may be needed for HIV-positive malnourished children to derive benefit from the drug[25]. Spiramycin, Azithromycin and Immunoglubulins have not been efficacious in controlled trials in patients with AIDS[26].
Isolate of Cryptosporidium spp. in our study was identified as Cryptosporidium hominis (C. hominis). Mercado et al[14], (2007) had isolated C. hominis from the respiratory secretions of an HIV sero-positive patient. No reports are available on the subtypes of Cryptosporidium spp. causing disseminated infection and/or infection of the tissues other than intestinal[11].
Substantial information about which species and subtypes of Cryptosporidium infect humans and the pathogenic patterns of each of these is needed. C. hominis have the capacity to adapt to diverse environments and infect gastrointestinal as well as respiratory tract. This report supports the role of C. homnis as a human pathogen and the need to evaluate the importance of respiratory cryptosporidiosis as a disease in children as well as in immunocompromised host.
Fever, vomiting, cough and rapid breathing since 15 d and subsequent diarrhea.
Interstitial Pneumonia.
Cytomegalovirus reactivation, Pneumocystis pneumonia, Fungal sepsis.
Severe anaemia, neutropenia. Normal kidney fuction with deranged Serum Glutamate Oxaloacetic Transaminase and Alkaline phosphatase. Urine culture was positive for E. coli. Stool samples and Endotracheal aspirate were positive for Cryptosporidium species using PCR.
Bilateral infiltrates were seen on chest X-ray.
Syp Nitazoxanide and Azithromycin along with Intravenous Ig and Bovine Colostrum were given to treat cryptosporidiosis.
Mercado et al (2007) had isolated C. hominis from the respiratory secretions of an human immunodeficiency virus sero-positive patient. No reports are available on the subtypes of Cryptosporidium spp. causing disseminated infection and/or infection of the tissues other than intestinal.
Dissemination of cryptosporidiosis should be considered in patients with compromised cellular immunity as well as in individuals with induced immunosuppression.
It is a well written case report describing a 15 mo old child with CD8+ immunodeficiency, suffering from disseminated Cryptosporidiosis leading to death.
Manuscript source: Invited manuscript
Specialty type: Infectious diseases
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gonzalez-Granado LI, Moschovi MA, Nagata T, Pourshafie MR S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Fayer R, Morgan U, Upton SJ. Epidemiology of Cryptosporidium: transmission, detection and identification. Int J Parasitol. 2000;30:1305-1322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 522] [Cited by in F6Publishing: 536] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 2. | Mak JW. Important zoonotic intestinal protozoan parasites in Asia. Trop Biomed. 2004;21:39-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Huang DB, White AC. An updated review on Cryptosporidium and Giardia. Gastroenterol Clin North Am. 2006;35:291-314, viii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 164] [Cited by in F6Publishing: 140] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 4. | Ajjampur SS, Sankaran P, Kang G. Cryptosporidium species in HIV-infected individuals in India: an overview. Natl Med J India. 2008;21:178-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 5. | Hunter PR, Nichols G. Epidemiology and clinical features of Cryptosporidium infection in immunocompromised patients. Clin Microbiol Rev. 2002;15:145-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 292] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 6. | Gentile G, Baldassarri L, Caprioli A, Donelli G, Venditti M, Avvisati G, Martino P. Colonic vascular invasion as a possible route of extraintestinal cryptosporidiosis. Am J Med. 1987;82:574-575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Miao YM, Awad-El-Kariem FM, Franzen C, Ellis DS, Müller A, Counihan HM, Hayes PJ, Gazzard BG. Eradication of cryptosporidia and microsporidia following successful antiretroviral therapy. J Acquir Immune Defic Syndr. 2000;25:124-129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 73] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Brady EM, Margolis ML, Korzeniowski OM. Pulmonary cryptosporidiosis in acquired immune deficiency syndrome. JAMA. 1984;252:89-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Johnson DW, Pieniazek NJ, Griffin DW, Misener L, Rose JB. Development of a PCR protocol for sensitive detection of Cryptosporidium oocysts in water samples. Appl Environ Microbiol. 1995;61:3849-3855. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Gile M, Warhurst DC, Webster KA, West DM, Marshall JA. A multiplex allele specific polymerase chain reaction (MAS-PCR) on the dihydrofolate reductase gene for the detection of Cryptosporidium parvum genotypes 1 and 2. Parasitology. 2002;125:35-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Alves M, Xiao L, Sulaiman I, Lal AA, Matos O, Antunes F. Subgenotype analysis of Cryptosporidium isolates from humans, cattle, and zoo ruminants in Portugal. J Clin Microbiol. 2003;41:2744-2747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 393] [Cited by in F6Publishing: 405] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 12. | Uppal B, Kashyap B, Bhalla P. Enteric Pathogens in HIV/AIDS from a Tertiary Care Hospital. Indian J Community Med. 2009;34:237-242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Palmieri F, Cicalini S, Froio N, Rizzi EB, Goletti D, Festa A, Macrí G, Petrosillo N. Pulmonary cryptosporidiosis in an AIDS patient: successful treatment with paromomycin plus azithromycin. Int J STD AIDS. 2005;16:515-517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Mercado R, Buck GA, Manque PA, Ozaki LS. Cryptosporidium hominis infection of the human respiratory tract. Emerg Infect Dis. 2007;13:462-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Shrikhande SN, Chande CA, Shegokar VR, Powar RM. Pulmonary cryptosporidiosis in HIV negative, immunocompromised host. Indian J Pathol Microbiol. 2009;52:267-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Egger M, Mäusezahl D, Odermatt P, Marti HP, Tanner M. Symptoms and transmission of intestinal cryptosporidiosis. Arch Dis Child. 1990;65:445-447. [PubMed] [Cited in This Article: ] |
| 17. | Weikel CS, Johnston LI, De Sousa MA, Guerrant RL. Cryptosporidiosis in northeastern Brazil: association with sporadic diarrhea. J Infect Dis. 1985;151:963-965. [PubMed] [Cited in This Article: ] |
| 18. | Shahid NS, Rahman AS, Anderson BC, Mata LJ, Sanyal SC. Cryptosporidiosis in Bangladesh. Br Med J (Clin Res Ed). 1985;290:114-115. [PubMed] [Cited in This Article: ] |
| 19. | Sallon S, Deckelbaum RJ, Schmid II, Harlap S, Baras M, Spira DT. Cryptosporidium, malnutrition, and chronic diarrhea in children. Am J Dis Child. 1988;142:312-315. [PubMed] [Cited in This Article: ] |
| 20. | Kumar H, Singh VB, Meena BL, Agrawal J, Beniwal S, Swami T. Pulmonary cryptosporidiosis in an immunocompetent host treated successfully with nitazoxanide. Lung India. 2016;33:69-71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Pozio E, Rezza G, Boschini A, Pezzotti P, Tamburrini A, Rossi P, Di Fine M, Smacchia C, Schiesari A, Gattei E. Clinical cryptosporidiosis and human immunodeficiency virus (HIV)-induced immunosuppression: findings from a longitudinal study of HIV-positive and HIV-negative former injection drug users. J Infect Dis. 1997;176:969-975. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 67] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Ma P, Villanueva TG, Kaufman D, Gillooley JF. Respiratory cryptosporidiosis in the acquired immune deficiency syndrome. Use of modified cold Kinyoun and Hemacolor stains for rapid diagnoses. JAMA. 1984;252:1298-1301. [PubMed] [Cited in This Article: ] |
| 23. | Villacorta-Martinez de Maturana I, Ares-Mazás ME, Duran-Oreiro D, Lorenzo-Lorenzo MJ. Efficacy of activated sludge in removing Cryptosporidium parvum oocysts from sewage. Appl Environ Microbiol. 1992;58:3514-3516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 24. | Rossignol JF, Hidalgo H, Feregrino M, Higuera F, Gomez WH, Romero JL, Padierna J, Geyne A, Ayers MS. A double-’blind’ placebo-controlled study of nitazoxanide in the treatment of cryptosporidial diarrhoea in AIDS patients in Mexico. Trans R Soc Trop Med Hyg. 1998;92:663-666. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 134] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | Amadi B, Mwiya M, Musuku J, Watuka A, Sianongo S, Ayoub A, Kelly P. Effect of nitazoxanide on morbidity and mortality in Zambian children with cryptosporidiosis: a randomised controlled trial. Lancet. 2002;360:1375-1380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 303] [Cited by in F6Publishing: 250] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 26. | Cabada MM, White AC. Treatment of cryptosporidiosis: do we know what we think we know? Curr Opin Infect Dis. 2010;23:494-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |