Published online Nov 23, 2015. doi: 10.5494/wjh.v5.i4.115
Peer-review started: June 20, 2015
First decision: July 27, 2015
Revised: August 3, 2015
Accepted: September 10, 2015
Article in press: September 16, 2015
Published online: November 23, 2015
Processing time: 153 Days and 14.6 Hours
In patients with primary hypertension, therapeutic strategies should be based on global cardiovascular risk profile rather than on the severity of blood pressure alone. Accurate assessment of concomitant risk factors and especially of the presence and extent of subclinical organ damage is of paramount importance in defining individual risk. Given the high prevalence of hypertension in the population at large, however, extensive diagnostic evaluation is often impractical or unfeasible in clinical practice. Low cost, easy to use markers of risk are needed to improve the clinical management of patients with hypertension. Early renal abnormalities such as a slight reduction in glomerular filtration rate and/or the presence of microalbuminuria are well known and powerful predictors of cardio-renal morbidity and mortality and provide a useful, low cost tools to optimize cardiovascular risk assessment. A greater use of these tests should therefore be implemented in clinical practice in order to optimize the management of hypertensive patients.
Core tip: Accurate assessment of global cardiovascular risk, including the search for subclinical organ damage is key for devising effective therapeutic strategies in patients with primary hypertension but is often unfeasible for economic and logistic reasons given the very high prevalence of this condition. Early renal abnormalities such as slight reduction in glomerular filtration rate and/or the presence of microalbuminuria are well known and powerful predictors of cardio-renal morbidity and mortality and provide the useful, low cost tools to optimize cardiovascular risk assessment. A greater use of these tests should therefore be implemented in clinical practice in order to optimize the management of hypertensive patients.
- Citation: Viazzi F, Cappadona F, Bonino B, Pontremoli R. Kidney and cardiovascular risk in primary hypertension. World J Hypertens 2015; 5(4): 115-118
- URL: https://www.wjgnet.com/2220-3168/full/v5/i4/115.htm
- DOI: https://dx.doi.org/10.5494/wjh.v5.i4.115
The worldwide prevalence of arterial hypertension, currently the most important modifiable risk factor for cardiac and cerebrovascular diseases, is going to increase dramatically over the next decades[1]. Recent surveys indicate that 30%-45% of adult population has high blood pressure (BP) in Western countries, with greater figures in at risk subgroups such as the elderlies, diabetics and patients with chronic kidney disease (CKD)[2]. Prevention and treatment of high BP therefore represent a big public health issue worldwide and a priority for many National Health Systems in developed countries.
Most International Guidelines recommend that therapeutic targets and strategies should be based not only on the severity of BP increase but rather on global cardiovascular (CV) risk profile in any given patient[2]. Accurate assessment of concomitant risk factors and especially of the presence and extent of subclinical target organ damage (OD) is of paramount importance in defining individual risk profile and therefore often becomes a key factor to improve cost effectiveness in the therapeutic algorithm[3].
Given the high prevalence of hypertension in the population however, extensive evaluation of risk factors including in-depth search for asymptomatic OD is often impractical or unfeasible both from a logistic and an economic point of view[4]. Low cost, easy to use, integrated markers of risk are therefore needed to improve the clinical management of patients with hypertension[5].
Even modest abnormalities of renal function, such as the presence of microalbuminuria or a slight reduction in glomerular filtration rate (GFR), have been shown to predict future cardiovascular events and death[6]. While these two features of CKD do not always coexist in the same patient, they are thought to reflect, at least in part, different pathogenic mechanisms and to carry independent predictive power in patients with high BP[7].
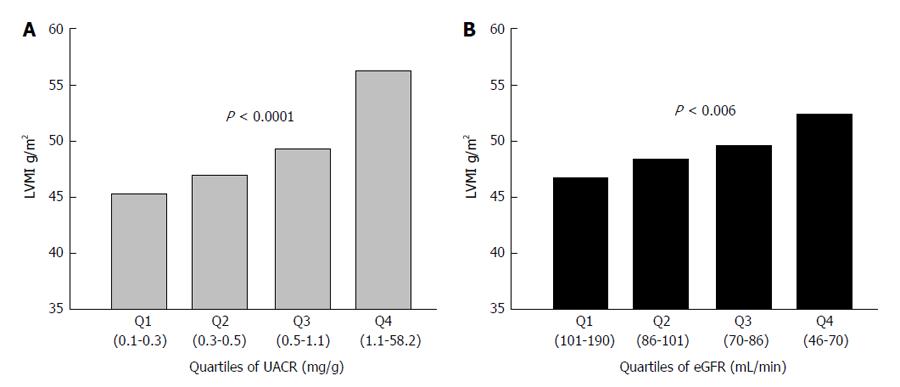
Microalbuminuria is currently regarded as an early sign of widespread vascular damage[8]. It has been shown to cluster with a variety of unfavourable risk factors such as metabolic syndrome, lipid abnormalities, hyperuricemia as well as with a greater haemodynamic load and blood pressure profile[9]. Furthermore, it has been shown to be an integrated marker of OD, as its presence often entails the concomitant occurrence of left ventricular hypertrophy (LVH) and systemic atherosclerosis (Figure 1)[10,11]. Increased urine albumin excretion (UAE) is a strong independent predictor of CV events, renal complications and death[12]. The relationship between UAE and risk is linear and holds also for albuminuria values well within the normal range[6]. These data, together with the relatively low cost and wide availability of this test, make searching for albuminuria an ideal screening and diagnostic tool to be used in clinical practice[5].
Even a mild reduction in GFR entails a cluster of unfavourable haemodynamic and metabolic modifications that negatively impact global and cardiovascular prognosis in hypertensive patients[13]. In fact, CKD, albeit often asymptomatic and therefore largely undetected in clinical practice, is known to bring about a number of atherogenic mechanisms such as insulin resistance, secondary hyperparathyroidism, vitamin D deficit, anaemia, subclinical inflammation, increased oxidative stress, lipids abnormalities, mild hyperuricemia and endothelial dysfunction[14].
Needless to say that the coexistence of GFR reduction and increase in UAE, a condition thought to occur in 20%-30% of CKD patients, entails an even higher risk as the two components of CKD retain independent prognostic power. Hence, GFR and UAE should be measured together to improve the assessment of risk[13].
The presence of subclinical OD at the cardiac, vascular and renal level has traditionally been regarded as an intermediate step between long-term exposure to risk factors and the incidence of major events[15]. As the development of OD signals a condition of greater risk, so prevention or regression of OD as a result of an effective treatment has been demonstrated to entail a parallel reduction of risk. Thus, regression of LVH has been shown to be associated with a better prognosis and has been proposed as an independent therapeutic target[16].
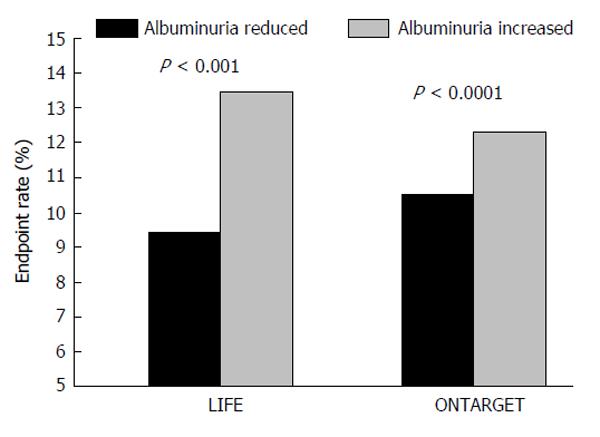
More recently, it has been suggested that albuminuria changes under treatment may provide additional information on the effectiveness of treatment[2,17]. Several clinical trials however, have yielded contrasting data on this issue. Thus, results of the Losartan Intervention For Endpoint reduction in hypertension (LIFE) study indicated that on-treatment modifications of UAE go in parallel to the incidence of fatal events[17,18]. On the contrary, in the ACCOMPLISH trial, antihypertensive treatment with angiotensin converting enzyme-inhibitors (ACE-I)/Calcium Channel Blockers combination was associated with better CV outcome as compared to ACE-I/diuretic combination, although the latter entailed a significantly greater reduction in urine albumin excretion[19]. In this context, results of the ONTARGET trial may give rise to conflicting interpretations. In fact, while a larger reduction in UAE was recorded in the arm treated with ACE-I/angiotensin II receptors blockers (ARB) combination, this treatment provided no clear benefit in the incidence of major endpoints as compared to ACE-I or ARB monotherapy[20]. However, when changes in UAE were analysed independently of randomization to specific treatment, those patients experiencing a greater reduction of albuminuria under treatment also showed better CV outcome as compared to patients with an increase or no change in albuminuria[21] (Figure 2). This issue has recently been the object of a large meta-regression analysis, involving thirty-two randomized studies and a total of 80812 hypertensive and/or diabetic patients[22]. In fact, Savarese et al[22] reported that reduction in UAE was associated with reduced risk of myocardial infarction and stroke, suggesting that UAE changes may represent a valuable intermediate end-point for CV risk evaluation in clinical practice. However, the conclusions of the above mentioned study were weakened by a number of biases, such as the heterogeneity of therapeutic interventions and length of follow-up that may limit the value of reported findings.
Accurate risk stratification is of paramount importance to devise cost-effective diagnostic and therapeutic strategies in patients with primary hypertension. An extensive search for subclinical OD is essential to assess global risk profile in most patients, but is often unfeasible for economic and logistic reasons due to the very high prevalence of hypertension. Early renal abnormalities such as slight reduction in GFR and/or the presence of microalbuminuria are well known and powerful predictors of cardio-renal morbidity and mortality and provide useful, low cost tools to optimize CV risk assessment. Furthermore, monitoring treatment-induced changes of UAE may be helpful in the management of high-risk patients.
P- Reviewer: Murata A, Tan XR S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ; Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2283] [Cited by in RCA: 2091] [Article Influence: 90.9] [Reference Citation Analysis (0)] |
| 2. | Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press. 2014;23:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 491] [Article Influence: 40.9] [Reference Citation Analysis (0)] |
| 3. | Viazzi F, Leoncini G, Parodi D, Ratto E, Vettoretti S, Vaccaro V, Parodi A, Falqui V, Tomolillo C, Deferrari G. Impact of target organ damage assessment in the evaluation of global risk in patients with essential hypertension. J Am Soc Nephrol. 2005;16 Suppl 1:S89-S91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Leoncini G, Ratto E, Viazzi F, Conti N, Falqui V, Parodi A, Tomolillo C, Deferrari G, Pontremoli R. Global risk stratification in primary hypertension: the role of the kidney. J Hypertens. 2008;26:427-432. [PubMed] |
| 5. | Leoncini G, Viazzi F, Pontremoli R. Overall health assessment: a renal perspective. Lancet. 2010;375:2053-2054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073-2081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3261] [Cited by in RCA: 3065] [Article Influence: 204.3] [Reference Citation Analysis (0)] |
| 7. | Viazzi F, Leoncini G, Conti N, Tomolillo C, Giachero G, Vercelli M, Deferrari G, Pontremoli R. Combined effect of albuminuria and estimated glomerular filtration rate on cardiovascular events and all-cause mortality in uncomplicated hypertensive patients. J Hypertens. 2010;28:848-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Leoncini G, Sacchi G, Viazzi F, Ravera M, Parodi D, Ratto E, Vettoretti S, Tomolillo C, Deferrari G, Pontremoli R. Microalbuminuria identifies overall cardiovascular risk in essential hypertension: an artificial neural network-based approach. J Hypertens. 2002;20:1315-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Pontremoli R. Microalbuminuria in essential hypertension--its relation to cardiovascular risk factors. Nephrol Dial Transplant. 1996;11:2113-2115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Pedrinelli R, Dell’Omo G, Di Bello V, Pontremoli R, Mariani M. Microalbuminuria, an integrated marker of cardiovascular risk in essential hypertension. J Hum Hypertens. 2002;16:79-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Leoncini G, Viazzi F, Conti N, Baratto E, Tomolillo C, Bezante GP, Deferrari G, Pontremoli R. Renal and cardiac abnormalities in primary hypertension. J Hypertens. 2009;27:1064-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Wachtell K, Ibsen H, Olsen MH, Borch-Johnsen K, Lindholm LH, Mogensen CE, Dahlöf B, Devereux RB, Beevers G, de Faire U. Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med. 2003;139:901-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 374] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 13. | Viazzi F, Leoncini G, Pontremoli R. Global cardiovascular risk assessment in the management of primary hypertension: the role of the kidney. Int J Hypertens. 2013;2013:542646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G; National Kidney Foundation. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3156] [Cited by in RCA: 3205] [Article Influence: 145.7] [Reference Citation Analysis (0)] |
| 15. | Devereux RB, Alderman MH. Role of preclinical cardiovascular disease in the evolution from risk factor exposure to development of morbid events. Circulation. 1993;88:1444-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 188] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Schmieder RE, Schlaich MP, Klingbeil AU, Martus P. Update on reversal of left ventricular hypertrophy in essential hypertension (a meta-analysis of all randomized double-blind studies until December 1996). Nephrol Dial Transplant. 1998;13:564-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 121] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE, Dahlöf B, Devereux RB, de Faire U, Fyhrquist F. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45:198-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 398] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 18. | Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE, Dahlöf B, Snapinn SM, Wan Y, Lyle PA. Does albuminuria predict cardiovascular outcomes on treatment with losartan versus atenolol in patients with diabetes, hypertension, and left ventricular hypertrophy? The LIFE study. Diabetes Care. 2006;29:595-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 82] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, Velazquez EJ, Staikos-Byrne L, Kelly RY, Shi V. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375:1173-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 331] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 20. | Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, Dagenais G, Sleight P, Anderson C; ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2526] [Cited by in RCA: 2388] [Article Influence: 140.5] [Reference Citation Analysis (0)] |
| 21. | Schmieder RE, Mann JF, Schumacher H, Gao P, Mancia G, Weber MA, McQueen M, Koon T, Yusuf S; ONTARGET Investigators. Changes in albuminuria predict mortality and morbidity in patients with vascular disease. J Am Soc Nephrol. 2011;22:1353-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 198] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 22. | Savarese G, Dei Cas A, Rosano G, D’Amore C, Musella F, Mosca S, Reiner MF, Marchioli R, Trimarco B, Perrone-Filardi P. Reduction of albumin urinary excretion is associated with reduced cardiovascular events in hypertensive and/or diabetic patients. A meta-regression analysis of 32 randomized trials. Int J Cardiol. 2014;172:403-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |