Published online Jun 12, 2019. doi: 10.5492/wjccm.v8.i3.28
Peer-review started: February 15, 2019
First decision: March 14, 2019
Revised: March 31, 2019
Accepted: May 21, 2019
Article in press: May 22, 2019
Published online: June 12, 2019
Protocols for nurse-led extubation are as safe as a physician-guided weaning in general intensive care unit (ICU). Early extubation is a cornerstone of fast-track cardiac surgery, and it has been mainly implemented in post-anaesthesia care units. Introducing a nurse-led extubation protocol may lead to reduced extubation time.
To investigate results of the implementation of a nurse-led protocol for early extubation after elective cardiac surgery, aiming at higher extubation rates by the third postoperative hour.
A single centre prospective study in an 18-bed, consultant-led Cardiothoracic ICU, with a 1:1 nurse-to-patient ratio. During a 3-wk period, the protocol was implemented with: (1) Structured teaching sessions at nurse handover and at bed-space (all staff received teaching, over 90% were exposed at least twice; (2) Email; and (3) Laminated sheets at bed-space. We compared “standard practice” and “intervention” periods before and after the protocol implementation, measuring extubation rates at several time-points from the third until the 24th postoperative hour.
Of 122 cardiac surgery patients admitted to ICU, 13 were excluded as early weaning was considered unsafe. Therefore, 109 patients were included, 54 in the standard and 55 in the intervention period. Types of surgical interventions and baseline left ventricular function were similar between groups. From the third to the 12th post-operative hour, the intervention group displayed a higher proportion of patients extubated compared to the standard group. However, results were significant only at the sixth hour (58% vs 37%, P = 0.04), and not different at the third hour (13% vs 6%, P = 0.33). From the 12th post-operative hour time-point onward, extubation rates became almost identical between groups (83% in standard vs 83% in intervention period).
The implementation of a nurse-led protocol for early extubation after cardiac surgery in ICU may gradually lead to higher rates of early extubation.
Core tip: Fast-track is emerging in cardiac surgery, and early extubation is a cornerstone for fast-track. Nurse-led extubation protocols may be introduced in clinical practice with different teaching techniques, aiming for early extubation.
- Citation: Serena G, Corredor C, Fletcher N, Sanfilippo F. Implementation of a nurse-led protocol for early extubation after cardiac surgery: A pilot study. World J Crit Care Med 2019; 8(3): 28-35
- URL: https://www.wjgnet.com/2220-3141/full/v8/i3/28.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v8.i3.28
Close monitoring of patients is required during the early postoperative period after cardiac surgery, particularly the first few hours, in order to identify and treat potentially life-threatening complications such as bleeding and cardiovascular instability. Traditionally, patients are managed in the intensive care unit (ICU) during the initial perioperative period. Nonetheless, the evolution of surgical perfusion techniques and anaesthetic management have allowed the successful implementation of fast-track care protocols after cardiac surgery. Patients with lower levels of complexity can be safely managed in post-anaesthesia care units (PACUs) with a decreased time to extubation, shorter ICU and hospital length of stay (LOS), and possible cost reduction[1-3]. These results have been confirmed by a Cochrane meta-analysis, which found no difference in complication rates, and outcomes between conventional care vs fast-track approach in low and moderate risk cardiac surgery patients. Moreover, the fast-track approach shortened time to extubation and LOS in ICU compared to conventional care[4]. Early extubation is a cornerstone for fast-track cardiac care and is associated with shorter duration of mechanical ventilation (MV), decreased ICU and hospital LOS, and fewer postoperative respiratory complications[5]. Conversely, prolonged MV in ICU is associated with higher incidence of pulmonary complications, increased ICU and hospital LOS and associated cost in both general ICU[6] and in the post-cardiac surgery populations[2,7,8].
In the general ICU setting, Kollef et al[9] showed that a nurse-led extubation protocol was as safe as physician-guided extubation, showing similar complications and mortality rates, significantly reducing MV time and possibly being effective in cost reduction. In the cardiac surgery setting, the largest amount of studies evaluating the safety and advantages of early extubation are based in the PACU, where staff are usually more experienced in rapid extubation than ICU personnel, and often have a higher physician-to-patient ratio.
Early extubation following cardiac surgery can be also used as a performance indicator in cardiac surgical centres[10]. Achieving safe early extubation depends on many contributing factors comprising the pre, intra and postoperative periods. Early extubation also relies on the successful coordination of efforts from multiple disciplines, i.e., nursing, surgery, anaesthesia and critical care.
In our study, we aimed to evaluate the results of the implementation of a nurse-led protocol for early extubation after cardiac surgery in ICU as part of a quality im-provement initiative. Research Ethics committee authorization and informed consent were not required to perform this study.
This was a single centre prospective study in an 18-bed Cardiothoracic ICU across an 11-week period (11.08.2014 – 21.12.2014). Our Cardiothoracic ICU is a closed critical care consultant-led ICU admitting patients after cardiac, thoracic and vascular procedures. During the period of study, the Cardiothoracic ICU was staffed with a team of two consultants from 8:00 to 18:00 and one consultant during the night hours with junior doctor support. Patients mechanically ventilated after cardiac surgery received nursing care in a one-to-one ratio.
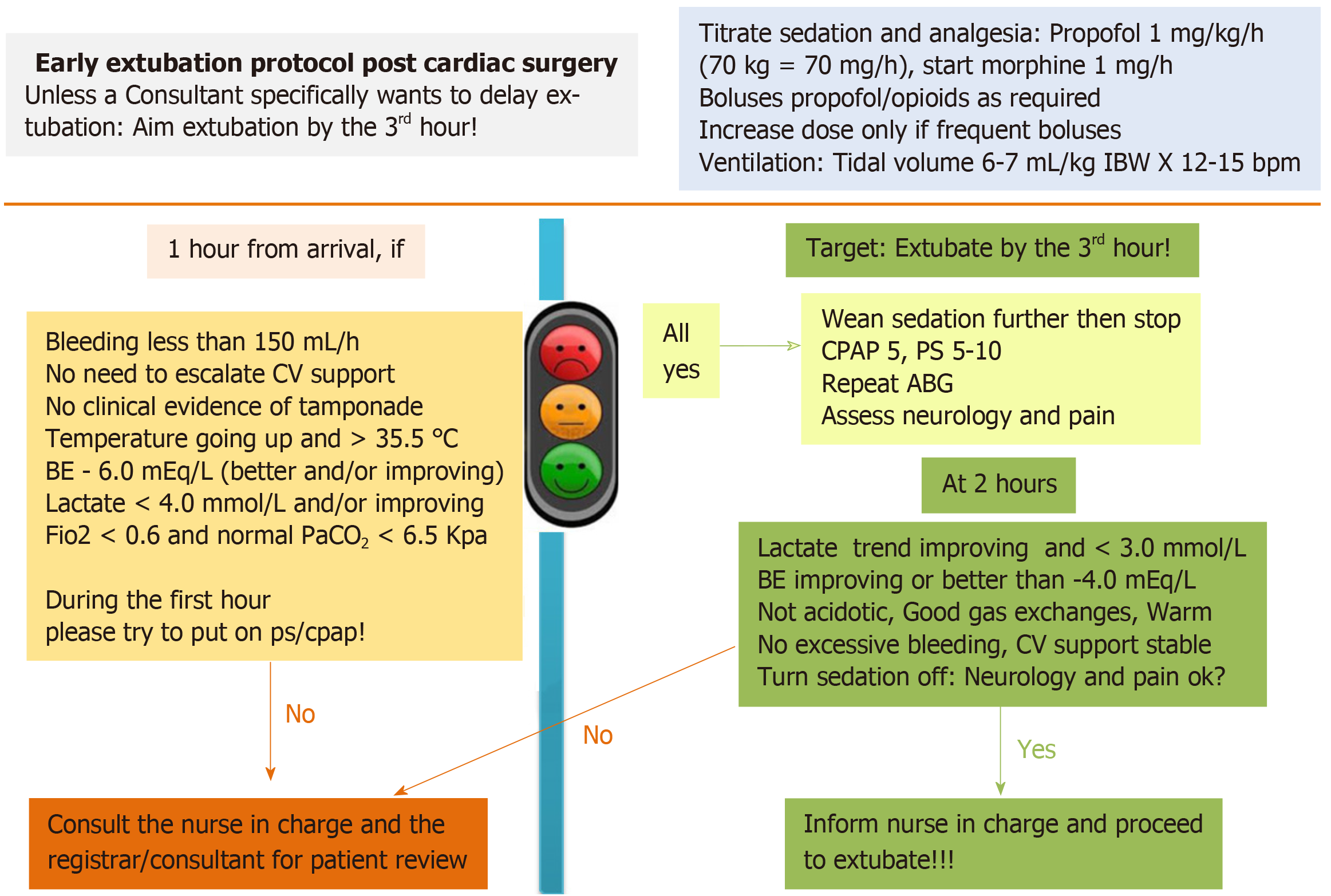
In the two years preceding this study, almost 1000 cardiac surgical cases per year were performed at our institution with an average of 80% being admitted to the Cardiothoracic ICU. The remaining 20% was managed in the fast-track PACU. In this study, we aimed to evaluate the results of the introduction of a nurse-led protocol for early extubation after cardiac surgery. Before the implementation of the nurse-led protocol, patients after cardiac surgery were extubated according to the decision of the treating physician. A simplified nurse-led protocol for extubation after cardiac surgery was introduced as part of a quality improvement initiative. A small steering group wrote a draft of the nurse-led protocol, which was reviewed, modified and approved by all of the Cardiothoracic ICU consultants and senior nurses. The final version of the protocol is shown in Figure 1. The protocol did not involve any changes in the anaesthetic or surgical intraoperative management.
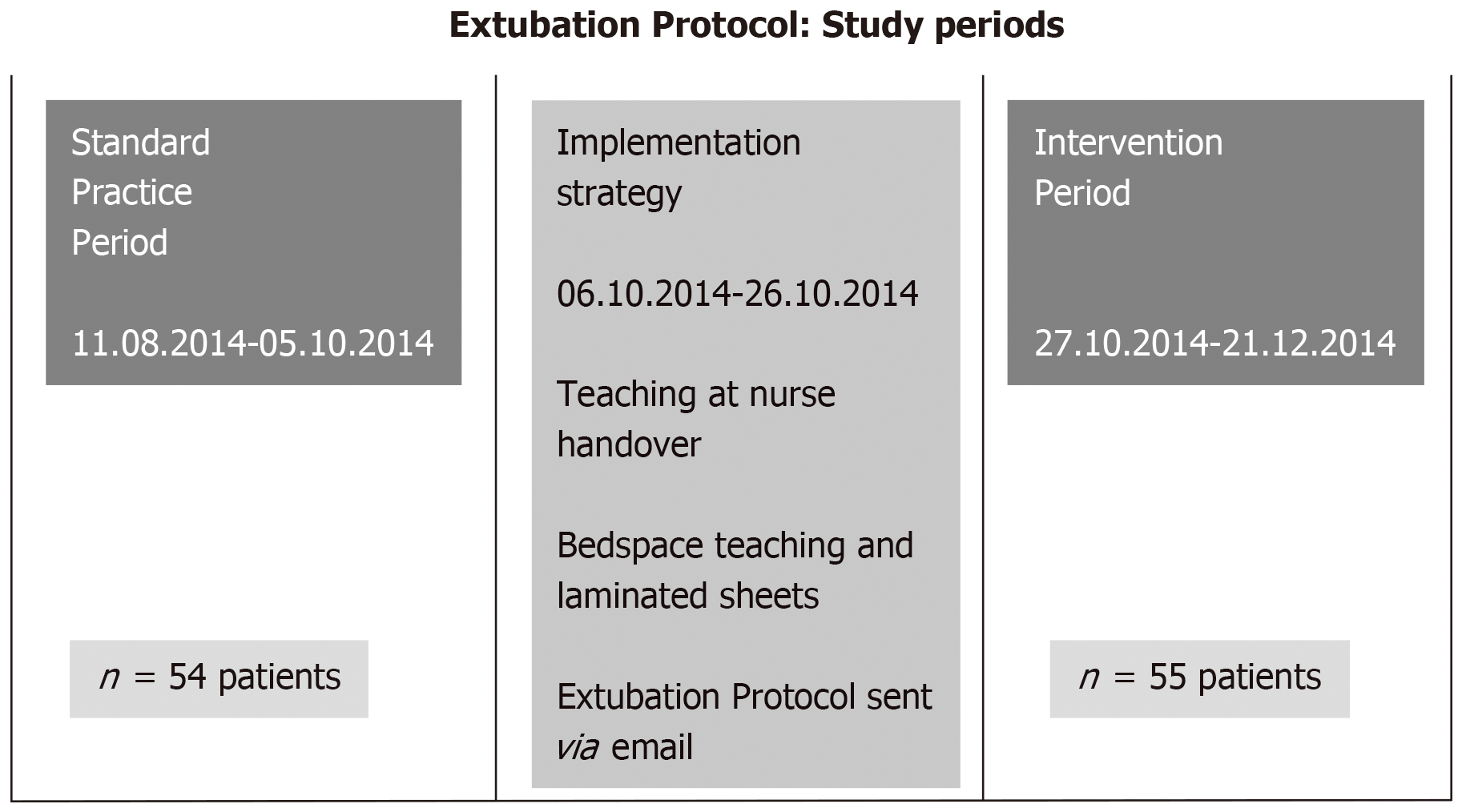
The study was divided into two periods of eight weeks each. The “standard practice” period, 11/08/2014 to 05/10/2014 and the “intervention” period, 27/10/2014 to 21/12/2014 (Figure 2). We anticipated approximately 100 patients per period. The overall data collection included the following time-points: admission, 1st - 2nd - 3rd - 4th - 5th - 6th - 9th - 12th – 15th - 18th - 24th postoperative hour. Data were collected in a pre-defined sheet by the bed-space nurse and entered into spread-sheet software (Microsoft Office Excel 2011). Patients admitted to the ICU were included in the nurse led protocol, unless a consultant anaesthetist/intensivist or cardiac surgeon stated it would have not been safe to extubate the patient early, based on both premorbid status and/or intraoperative course. Therefore, for this pilot study, we followed a pragmatic approach for the inclusion of patients in the nurse-led extubation pathway.
The two study periods were separated by a three-week period (06/10/2014 – 26/10/2014) dedicated to teaching the new protocol to all nursing and medical staff using short small group sessions held by the members of the steering group. Additionally, we delivered one to one bed-side teaching to the nursing staff. An attendance form was kept to ensure that all staff received frontal teaching. This resulted in over 90% of the staff exposed to this teaching at least twice. The protocol was disseminated via email to the entire staff, and laminated sheets containing the protocol were printed and distributed at each bed-space with additional copies available in the staff room.
As shown in Figure 1, the new protocol set a target of extubation from operating theatre arrival by the third postoperative hour, if conditions specified by the protocol were met. The bedside nurse was in charge of implementing the protocol from arrival with setting of pre-specified parameters for titration of sedation and analgesia. Mechanical ventilation settings following a “lung protective strategy” were also outlined in the protocol. Within one hour from arrival, the bedside nurse confirmed the absence of several exclusion criteria (excessive bleeding and/or tamponade, metabolic and hemodynamic derangements, hypoxia and or hypercarbia, hypothermia) against a checklist, before decreasing sedation levels and attempting to start pressure support ventilation mode. From the second postoperative hour, or whenever criteria for extubation were met, nurses were asked to wean sedation and mechanical ventilation in order to extubate by the third postoperative hour, after confirming the clinical decision with the senior nurse in charge or with the doctor on duty. Bedside nurses informed the senior nurse in charge and/or the doctor on duty in case of clinical issues or uncertainty.
The primary outcome of our study was that a proportion of patients extubated at different pre-defined time-points (from the third until the 12th postoperative hour). Secondary outcomes were re-intubation rates within 12 hours from extubation and adherence to a lung protective ventilation strategy. Lung protective was defined as a tidal volume of 6-8 mL/kg ideal body weight.
Formal sample size calculation was not performed in this study, but assumption on the length of each period was made based on average number of cardiac surgery intervention admitted to the Cardiothoracic ICU.
The Kolmogorov-Smirnoff test, histograms and normal quartile plots were examined to test for the normality assumption of continuous variables. Continuous variables are presented as mean (SD) with 95% confidence interval (95%CI) or median [(interquartile range) (IQR)] and categorical variables as number and percentage (%). A Wilcoxon signed rank test was then used to detected differences among pairs of samples. Categorical variables were compared through the Chi-square test with Yates correction. All tests were two-sided, and a result of P < 0.05 was considered statis-tically significant. Statistical analyses were performed using IBM® SPSS® Statistics 17 for Windows.
During the two study periods, a total of 122 postoperative cardiac surgical patients were admitted to the cardiothoracic ICU, 60 in the standard practice and 62 during the intervention period. Thirteen patients (six in the standard practice period and seven in the intervention period) were excluded from the early extubation protocol at the discretion of the attending consultant due to complex surgery, comorbidities or intraoperative issues. Therefore, data from a total of 109 patients were collected, 54 in the standard practice and 55 in the intervention period.
Patients in the “standard period”, as compared to the “intervention period”, had similar height (168.3 ± 9.7 cm vs 170.8 ± 8.8 cm respectively, P = 0.11) and age (66.5 ± 11.7 vs 65.7 ± 10.9, respectively, P = 0.74) and body weight (76.8 ± 13.4 kg vs 82.3 ± 14.8 kg, respectively, P = 0.07). In both periods, male patients represented 76% of the population (P = 0.96).
The types of interventions were similar between groups. The two most common surgical intervention were isolated elective coronary artery surgery (n = 31/54, 57% of all surgeries during the “standard period” vs n = 27/55, 49% in the “intervention period”, P = 0.50) and coronary surgery associated to aortic valve replacement (n = 7/54, 13% “standard period” vs n = 5/55, 9% “intervention period”, P = 0.73). The groups were also comparable with regards to their baseline LV function (Table 1).
| Before the implementation of extubation protocol (n of patients) | After the implementation of extubation protocol (n of patients) | |
| Normal LV function | 41 | 40 |
| Mild-to-moderate LV impairment | 11 | 14 |
| Severe LV impairment | 2 | 1 |
| Total | 54 | 55 |
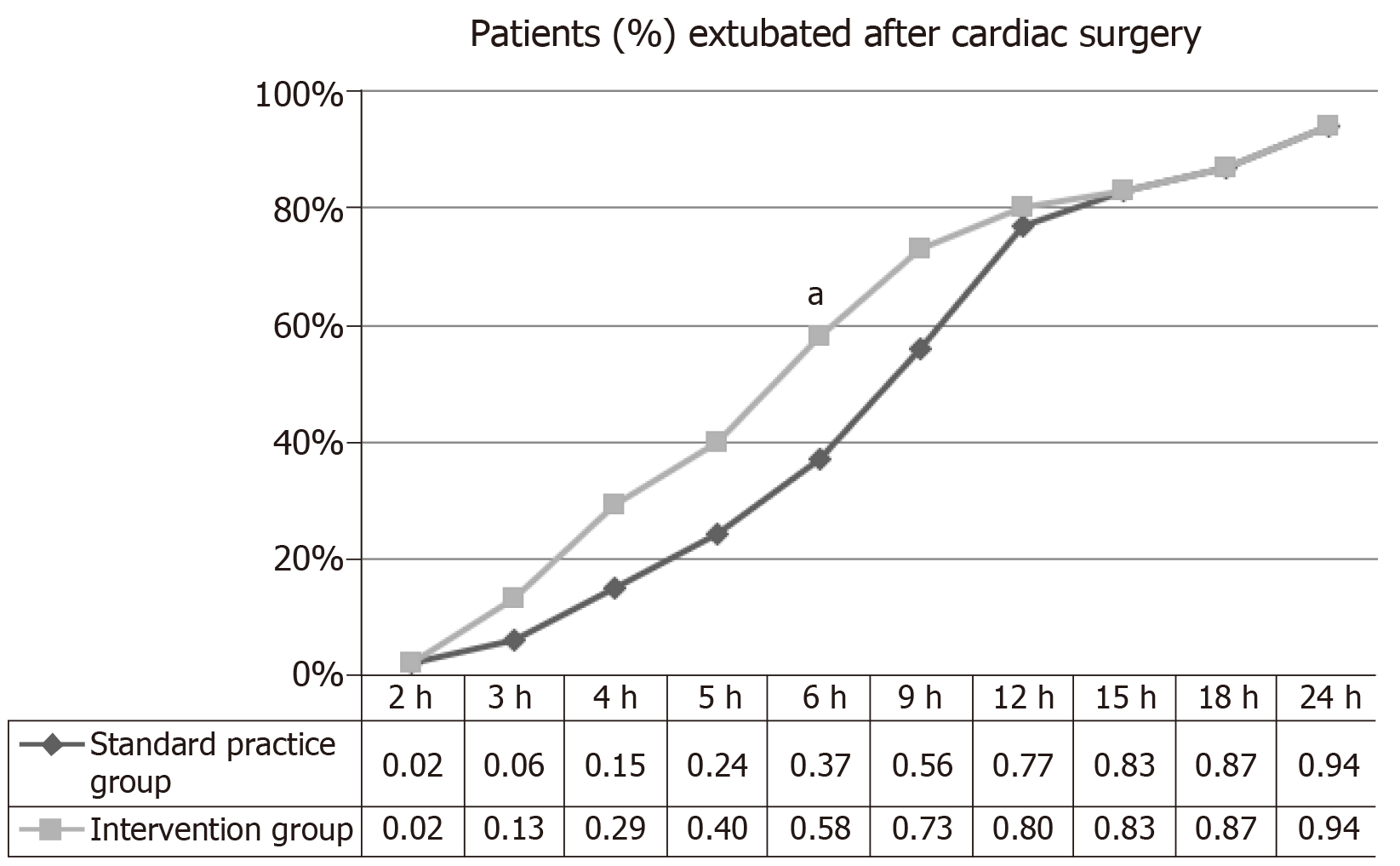
Extubation rates did not differ between the two study groups at the third post-operative hour. However, from the third to the 12th post-operative hour, the inter-vention group displayed a higher proportion of patients extubated compared to the standard group. The difference was only statistically significant at the sixth postoperative hour (37% in the standard vs 58% in the intervention period, P = 0.04). A non-significant trend towards higher extubation rates in the intervention period was found from the fourth until the ninth postoperative hour (fourth hour: P = 0.12; 5th h: P = 0.13; ninth hour: P = 0.10). From the 12th post-operative hour time-point onward, extubation rates became almost identical between the groups (Figure 3). Only one patient in the standard group and two patients in the intervention group were re-intubated within 12 h after extubation. All cases were due to respiratory failure, and the difference between periods was not statistically significant (P = 0.99).
Patients were ventilated with similar positive end-expiratory pressure (PEEP) levels throughout the postoperative period between groups. More than 99% of PEEP values recorded were 5 cmH2O or above in both groups. There was an acceptable degree of adherence to the indication regarding the TV, with less than 7% of patients in both groups ventilated with 8 mL/kg or higher, and in most cases, such TV were achieved in pressure support ventilation mode.
Early extubation is a cornerstone in fast-track care protocols after cardiac surgery, and it has been repeatedly investigated in dedicated PACU settings. Our study found that early extubation following the introduction of a nurse-led protocol can be implemented in a cardiovascular ICU setting, possibly resulting in a greater number of early extubations.
The early extubation project constitutes the initial stages of a quality cycle aimed to streamline and standardize patient flow in our cardiovascular ICU to improve patient outcomes. We observed statistically significantly higher rates of extubation in the intervention group at the sixth postoperative hour (P = 0.04). Although non-significant, we saw also a trend towards higher extubation rates from the fourth until the ninth postoperative hour. We believe that our study was underpowered to detect significant differences in extubation rates between the study groups. Indeed, there was a lower-than-expected number of patients included in the study due to unplanned reduction in our case-load. Therefore, it remains speculative that collecting a higher number of cases would have resulted in an earlier and larger separation of the extubation rate curves. From the 12th postoperative hour, the curves of patients extubated did not differ between the two investigated periods, likely because patients mechanically ventilated beyond this stage were not suitable for early extubation and that the reduced number of cases had no impact after the 12th postoperative hour. We found similar compliance with TV and PEEP levels compatible with a lung protective strategy in both groups, which probably reflects the widespread practice of lung protective ventilation in modern ICUs.
We acknowledge that our protocol failed to boost the target set by our protocol of increasing extubation rates as early as two hours after cardiac surgery. This is not unexpected, since adopting a new and faster protocol may take time. Resistance to sudden changes in clinical practice is not uncommon. Nevertheless, studies in other scenarios have shown that improvements in clinical practice can be obtained when new interventions are introduced using a continuous education program leading to improving outcomes in critically ill patients[11]. The need for a learning curve based on experience is likely, and this should be taken into account as well. Moreover, the lower-than-expected number of cases included in our study probably reduced staff exposure to the new strategy on early extubation, which in turn may have slowed the learning curve process. We believe our strategy for implementing the new protocol was well-designed and had the advantage of making the personnel more comfortable with the new approach.
Extubation remains a challenging perioperative stage with a higher number of perioperative respiratory complications occurring at the extubation rather than during the intubation process (12.6% vs 4.6%)[12]. Furthermore, extubation may expose fragile cardiac patients to significant shifts in intrathoracic pressures, which can lead to a number of cardiac complications such as pulmonary oedema due to left ventricular dysfunction. Therefore, safe extubation demands a systematic approach, especially in the setting of complex surgery in patients with significant comorbidities. Early extubation of patients after cardiac surgery involves multiple tasks, such as appropriate sedation and analgesia titration, frequent neurological assessment, continuous evaluation of haemodynamic stability, progressive respiratory weaning, careful temperature control and assessment of bleeding. Our protocol covered all of the aspects mentioned above. We believe that these tasks can be satisfactorily accomplished by trained and motivated nurses, with the back-up support of experienced medical staff. In the general ICU, a large study showed that a nurse-led extubation protocol had similar complications and mortality rates than physician-guided extubation and significantly reduced MV time, possibly having positive effects on cost saving[9].
Our study has the value of investigating the implementation of a structured nurse-led protocol for early extubation after cardiac surgery in a Cardiothoracic ICU with a 1:1 nurse-to-patient ratio for ventilated patients. However, in the cardiac surgery setting, the largest amount of studies evaluating safety and advantages of early extubation are based in the PACU, where staff have more experience in extubation than the ICU personnel. Moreover, PACU usually has a higher consultant-to-patient ratio compared to ICU. For instance, Probst et al[13] recently compared post-cardiac surgery management in PACU vs cardiac ICU and found a significant shorter extubation time and a higher rate of extubation within the first six postoperative hours in hemodynamically stable, normo-thermic, non-bleeding patients admitted to PACU as compared to a similar group of patients admitted to ICU. Moreover, PACU patients had shorter LOS before step-down and less arrhythmic complication, with no difference in other complication rates. When looking at such results, it is worthwhile noting some of the structural differences between PACU and ICU in this study: (1) 3-bed PACU vs 21-bed ICU; (2) Dedicated post-cardiac surgery PACU vs mixed ICU; and (3) 1:3 consultant-to-patient ratio in PACU and 1:12 in ICU. Considering these structural differences together with the usually higher airway skills of PACU staff, the observed differences are not surprising.
The most important limitation of our study is the lower than expected number of cases collected in the study period. We were able to analyse data from only 105 patients rather than the estimated target of 200. A second limitation is the lack of standardisation of anaesthetic management that likely influenced the neurological appropriateness for extubation. A third limitation of this study is that safety could not be fully evaluated with such small numbers; although only three patients were re-intubated after extubation, this is not an infrequent event after cardiac surgery, and larger numbers are required to fully evaluate the safety of early extubation in Cardiothoracic ICU after cardiac surgery. Finally, protocols implementing nurse-led extubation should take into account the staff skills and knowledge. Our results should be interpreted, considering that in the United Kingdom, there is a very high level of training and continuous re-training for nurses. Other countries and Healthcare Systems with lower resources may struggle in providing such level of training and therefore the practice of nurse-led extubation after cardiac surgery may not be practical.
The study covered the data acquisition, pattern analysis, interpretation and change in action stages necessary to initiate a quality cycle[14]. Our intention is to complete the quality cycle by acquiring further data for a larger cohort of patients and periodical evaluation of outcomes.
In conclusion, we implemented a nurse-led protocol for early extubation in the Cardiothoracic ICU with structured teaching and training. Although the extubation rates were similar by the third postoperative hour, a higher rate of patients in the intervention group was extubated by the sixth postoperative hour. We did not have enough data to establish the safety of our early extubation protocol.
Nurse led-extubation is safe in the general intensive care unit (ICU) setting, but data in field of cardiac surgery are scarce and limited to post-anaesthesia care units.
Nurse-led extubation protocols may help in shortening postoperative mechanical ventilation, thus expediting patient recovery after cardiac surgery.
To evaluate the results of the implementation of a nurse-led extubation protocol.
In a single centre prospective study during a 3-wk period, we implemented a nurse-led extubation protocol in patients admitted after cardiac surgery. The protocol was implemented with structured teaching sessions at nurse handover, teaching at bed-space, information provided via email and apposition of laminated sheets with the protocol at each bed-space. We performed a comparison of before and after protocol implementation (“standard practice” and “intervention” periods, respectively), measuring extubation rates at several time-points from the third until the 24th postoperative hour.
We included 109 patients, 54 in the standard and 55 in the intervention period. Although the intervention group displayed a higher proportion of patients extubated from the third to the 12th post-operative hour compared to the standard group, results were significant only at the sixth hour (58% vs 37%, P = 0.04) and not different at the third hour (13% vs 6%, P = 0.33). After the 12th post-operative hour time-point onward, extubation rates become almost identical between groups.
The implementation of a nurse-led protocol for early extubation after cardiac surgery in the cardiac ICU may gradually lead to higher rates of early extubation.
The present study adds information regarding a growing body of literature of fast-track extubation and identifies a nurse-led protocol as a possible intervention that shortens the length of mechanical ventilation in patients recovering after cardiac surgery. The study findings should be interpreted in the context of the level of training and the nurse-to-patient ratio.
Manuscript source: Unsolicited manuscript
Specialty type: Critical care medicine
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Drabek T S-Editor: Wang JL L-Editor: Filipodia E-Editor: Wu YXJ
| 1. | Cheng DC. Fast track cardiac surgery pathways: early extubation, process of care, and cost containment. Anesthesiology. 1998;88:1429-1433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 123] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Cheng DC, Karski J, Peniston C, Asokumar B, Raveendran G, Carroll J, Nierenberg H, Roger S, Mickle D, Tong J, Zelovitsky J, David T, Sandler A. Morbidity outcome in early vs conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. 1996;112:755-764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 268] [Cited by in F6Publishing: 273] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Cheng DC, Wall C, Djaiani G, Peragallo RA, Carroll J, Li C, Naylor D. Randomized assessment of resource use in fast-track cardiac surgery 1-year after hospital discharge. Anesthesiology. 2003;98:651-657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Zhu F, Lee A, Chee YE. Fast-track cardiac care for adult cardiac surgical patients. Cochrane Database Syst Rev. 2012;10:CD003587. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Meade MO, Guyatt G, Butler R, Elms B, Hand L, Ingram A, Griffith L. Trials comparing early vs late extubation following cardiovascular surgery. Chest. 2001;120:445S-453S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005;33:2184-2193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 729] [Cited by in F6Publishing: 707] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 7. | Cheng DC. Pro: early extubation after cardiac surgery decreases intensive care unit stay and cost. J Cardiothorac Vasc Anesth. 1995;9:460-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 75] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Cheng DC, Karski J, Peniston C, Raveendran G, Asokumar B, Carroll J, David T, Sandler A. Early tracheal extubation after coronary artery bypass graft surgery reduces costs and improves resource use. A prospective, randomized, controlled trial. Anesthesiology. 1996;85:1300-1310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 278] [Cited by in F6Publishing: 281] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Kollef MH, Shapiro SD, Silver P, St John RE, Prentice D, Sauer S, Ahrens TS, Shannon W, Baker-Clinkscale D. A randomized, controlled trial of protocol-directed vs physician-directed weaning from mechanical ventilation. Crit Care Med. 1997;25:567-574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 504] [Cited by in F6Publishing: 525] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 10. | Lobdell K, Camp S, Stamou S, Swanson R, Reames M, Madjarov J, Stiegel R, Skipper E, Geller R, Velardo B, Mishra A, Robicsek F. Quality improvement in cardiac critical care. HSR Proc Intensive Care Cardiovasc Anesth. 2009;1:16-20. [PubMed] [Cited in This Article: ] |
| 11. | Pellis T, Sanfilippo F, Roncarati A, Dibenedetto F, Franceschino E, Lovisa D, Magagnin L, Mercante WP, Mione V. A 4-year implementation strategy of aggressive post-resuscitation care and temperature management after cardiac arrest. Resuscitation. 2014;85:1251-1256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Asai T, Koga K, Vaughan RS. Respiratory complications associated with tracheal intubation and extubation. Br J Anaesth. 1998;80:767-775. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 161] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Probst S, Cech C, Haentschel D, Scholz M, Ender J. A specialized post anaesthetic care unit improves fast-track management in cardiac surgery: a prospective randomized trial. Crit Care. 2014;18:468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | Donabedian A. Evaluating the quality of medical care. 1966. Milbank Q. 2005;83:691-729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1526] [Cited by in F6Publishing: 1267] [Article Influence: 66.7] [Reference Citation Analysis (0)] |