Published online Feb 4, 2018. doi: 10.5492/wjccm.v7.i1.24
Peer-review started: August 29, 2017
First decision: September 25, 2017
Revised: November 5, 2017
Accepted: December 3, 2017
Article in press: December 3, 2017
Published online: February 4, 2018
To evaluate the predictive capability of respiratory mechanics for the development of ventilator-associated pneumonia (VAP) and mortality in the intensive care unit (ICU) of a hospital in southern Brazil.
A cohort study was conducted between, involving a sample of 120 individuals. Static measurements of compliance and resistance of the respiratory system in pressure-controlled ventilation (PCV) and volume-controlled ventilation (VCV) modes in the 1st and 5th days of hospitalization were performed to monitor respiratory mechanics. The severity of the patients’ illness was quantified by the Acute Physiology and Chronic Health Evaluation II (APACHE II). The diagnosis of VAP was made based on clinical, radiological and laboratory parameters.
The significant associations found for the development of VAP were APACHE II scores above the average (P = 0.016), duration of MV (P = 0.001) and ICU length of stay above the average (P = 0.003), male gender (P = 0.004), and worsening of respiratory resistance in PCV mode (P = 0.010). Age above the average (P < 0.001), low level of oxygenation on day 1 (P = 0.003) and day 5 (P = 0.004) and low lung compliance during VCV on day 1 (P = 0.032) were associated with death as the outcome.
The worsening of airway resistance in PCV mode indicated the possibility of early diagnosis of VAP. Low lung compliance during VCV and low oxygenation index were death-related prognostic indicators.
Core tip: The results show that the respiratory function is a prognostic measure, and is strongly associated with mortality. Low oxygen and low lung compliance during volume-controlled ventilation demonstrate this fact. Worsening of respiratory system resistance during pressure-controlled ventilation, associated with the development of ventilator-associated pneumonia, indicates the possibility of early diagnosis. Based on this assumption, this procedure should be performed routinely in the intensive care unit environment, providing the intensive care physician and the physiotherapist with additional prognosis and diagnosis variables, in addition to the clinical, laboratory and radiological data.
- Citation: Kock KS, Maurici R. Respiratory mechanics, ventilator-associated pneumonia and outcomes in intensive care unit. World J Crit Care Med 2018; 7(1): 24-30
- URL: https://www.wjgnet.com/2220-3141/full/v7/i1/24.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v7.i1.24
Factors influencing the outcomes in intensive care unit (ICU) enable behaviors that can benefit the patient and reduce hospital costs[1,2]. Monitoring of respiratory mechanics in the admission of patients may provide an additional parameter for the monitoring of cases with possible epidemiological implications[3]. Invasive ventilatory support is a resource frequently used in extremely critical care, either to rescue breathing in patients unable to maintain the ventilatory demand, or as a strategy for energy saving in seriously ill patients[4]. Knowledge about respiratory mechanics may facilitate the detection of changes in the respiratory status of the patient and enable appropriate adjustment in ventilatory parameters, as well as support an appropriate therapeutic intervention to improve his or her clinical condition[5,6].
Few studies use these variables as prognostic measures in ICU[7]. The main applications of monitoring respiratory mechanics are performed on well-established cases, such as in patients with obstructive lung disease[8] and in patients with acute respiratory distress syndrome (ARDS)[9]. Some studies discuss the importance of these measures in patients with pulmonary fibrosis[10] or with the human immunodeficiency virus (HIV) infection and pneumonia[11].
The measurements of respiratory mechanics most frequently used are compliance and resistance of the respiratory system. Compliance is associated with distensibility of the respiratory system, which is resulting from the tidal volume variation divided by the peak inspiratory pressure. Resistance is related to the conduction of air, obtained mathematically from the variation between the peak and plateau pressures divided by the inspiratory airflow[12].
Ventilator-associated pneumonia (VAP) is the most common infection in ICU. This pulmonary condition may change the respiratory mechanics. Beyond the importance of the bundles of care for the prevention of VAP[13], information of compliance and resistance of respiratory system can provide additional data for an early diagnosis. The aim of this study was to assess the risk of changes in respiratory mechanics for determination of outcomes: development of VAP, and mortality in ICU.
A cohort study was performed on adults in the intensive care unit of the of the Hospital Nossa Senhora da Conceição, located in Tubarão, State of Santa Catarina, Brazil. Individuals hospitalized between February and September 2013 who required invasive ventilatory support and whose family signed the informed consent were selected. The study was approved by the Human Research Ethics Committee of the University of Southern Santa Catarina (number 12.460.4.08.III).
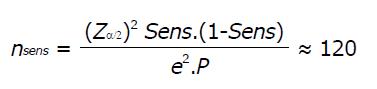
As this is a study of diagnostic and prognostic accuracy, the sample size was dimensioned for a prevalence of mortality[14] and VAP[15] of 20% (P = 0.2), with a 12% error (e = 0.12) in the 95% confidence interval (Zα/2 = 1.96). Sensitivity was defined 90% (Sens = 0.9). The equation[16] used is described below:
Math 1
The following subjects were excluded from the study: Patients who were hospitalized in the ICU for cardiac surgery, those who developed pneumonia, died, or were extubated within 48 h of the onset of mechanical ventilation, those who were reintubated and those whose cause of orotracheal intubation was respiratory infection. The patients who were transferred to another ICU were excluded as well.
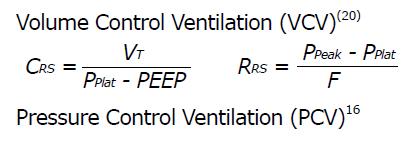
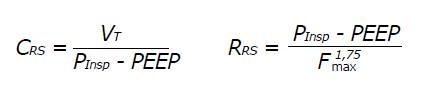
The following procedures were performed for the data collection: Day 1 (D1) - First 24 h of mechanical ventilation. APACHE II[17] scoring, assessment of oxygenation index obtained from the PaO2/FiO2 ratio[18], and assessment of the respiratory system compliance and resistance were performed. The patients should score 5-6 in the Ramsay sedation scale[19] for measuring airflow compliance and resistance. Respiratory mechanic was measured in volume-controlled ventilation (VCV) and pressure-controlled ventilation (PCV)[20]. The equations for calculating respiratory mechanics were these:
Math 2
Math 3
CRS: Respiratory system compliance (mL/cmH2O); RRS: Respiratory system resistance (cmH2O/L/s); PEEP: Positive end-expiratory pressure (cmH2O); PInsp: Inspiratory pressure (cmH2O); Ppeak: Peak inspiratory pressure (cmH2O); Pplat: Plateau pressure (cmH2O); VT: Tidal volume (mL); F: Forced inspiratory flow (L/s); Fmax: Peak inspiratory flow (L/s).
Day 5 (D5) - Assessment of the respiratory system compliance and resistance was performed as described above. If the patient were in the ventilatory weaning process, this measure would not be collected.
Patients were monitored until their discharge from the ICU or death. The duration of mechanical ventilation and length of ICU stay were taken into account, until the emergence of at least one of those outcomes.
VAP was diagnosed by the emergence of new or progressive pulmonary infiltrate on the chest X-Ray, associated with signs and laboratory alterations, such as fever (> 38 °C), leukocytosis (> 10000/mm3) or leukopenia (< 4000/mm3), and purulent tracheal secretions[21].
Early VAP was performed when it was diagnosed within the first 5 d. Late VAP was considered when the diagnosis occurred after the sixth day[15].
Data were stored in a database using a Microsoft Excell® software, which was exported to SPSS® Statistics 20.0. They were presented using absolute numbers and percentages, and measures of central tendency and dispersion. The cutoff point for normal respiratory compliance and resistance was defined as the means obtained from the results.
The analysis of numerical data was performed primarily by the Kolmogorov-Smirnov test for normality. The results with normal distribution were compared using Student’s t-test, and the non-normal distribution results by using the Mann-Whitney test[22]. The Chi-square test was used for categorical data analysis. Variable comparisons were made in relation to the VAP outcomes, mortality, ICU stay and duration of mechanical ventilation. The relative risk was estimated, by univariate analysis, for variables with statistical association. The confidence interval was set at 95% and a P < 0.05 was considered statistically significant.
Measurements of the oxygenation index and respiratory mechanics were performed by analyzing the worsening or improvement in these variables between D1 and D5.
A higher airflow resistance in D1 than in D5 was considered a better state. Reversely, a lower airflow resistance, a worse result.
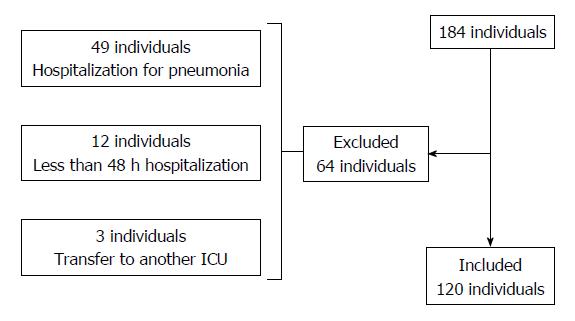
A total of 184 patients who were hospitalized in the ICU of the Hospital Nossa Senhora da Conceição (Tubarão, State of Santa Catarina, Brazil) between February and September 2013 were consecutively monitored (Figure 1).
According to the selection criteria, 120 patients were allocated to participate in the study. Table 1 describes the general characteristics of the sample.
| Sample characteristics (n = 120) | Results |
| Age (yr) | |
| Mean ± SD | 58.5 ± 19.4 |
| Minimum-maximum | 15-91 |
| Gender n (%) | |
| Male | 69 (57.5) |
| Female | 51 (42.5) |
| APACHE II (score) | |
| Mean ± SD | 27.4 ± 6.7 |
| Minimum–maximum | 8-47 |
| Risk of mortality (%)-APACHE II | |
| Mean ± SD | 61.8 ± 7.3 |
| Admission diagnoses n (%) | |
| Diseases of the circulatory system | 43 (35.8) |
| Diseases of the respiratory system | 15 (12.5) |
| Lesions, poisoning and other consequences of external causes | 14 (11.7) |
| Gastrointestinal diseases | 8 (6.7) |
| Unclassified signs and symptoms | 8 (6.7) |
| Diseases of the genitourinary system | 7 (5.8) |
| Neoplasia | 4 (3.3) |
| Nervous system disorders | 4 (3.3) |
| Infectious and parasitic diseases | 3 (2.5) |
| Endocrine, nutritional and metabolic diseases | 3 (2.5) |
| Other | 11 (9.2) |
| Mechanical ventilators n (%) | |
| 1Servo S | 89 (74.2) |
| 1Servo 900 | 203 (16.7) |
| 1Dixtal | 11 (9.2) |
Oxygenation index and respiratory mechanics on days 1 and 5 are shown in Table 2. On the 5th day, only 77 of the 120 patients were monitored, because they were either extubated, weaned from mechanical ventilation, or had died by then.
| Oxygenation index | Mean ± SD | Minimum-maximum |
| Respiratory mechanics | ||
| 1st day (n = 120) | ||
| PaO2/FiO2 (mmHg) | 236.0 ± 97.6 | 47.0-465.7 |
| Compliance-VCV (mL/cm H2O) | 40.9 ± 12.8 | 15.0-88.0 |
| Resistance-VCV (cm H2O/L/s) | 13.2 ± 4.9 | 4.1-28.6 |
| Compliance-PCV (mL/cm H2O) | 35.0 ± 10.0 | 15.0-62.0 |
| Resistance-PCV (cm H2O/L/s) | 27.3 ± 16.2 | 9.1-131.1 |
| 5th day (n = 77) | ||
| PaO2/FiO2 (mmHg) | 241.7 ± 88.7 | 58.0-445.0 |
| Compliance-VCV (mL/cm H2O) | 39.7 ± 13.2 | 18.0-83.0 |
| Resistance-VCV (cm H2O/L/s) | 13.8 ± 6.0 | 5.3-43.0 |
| Compliance-PCV (mL/cm H2O) | 32.9 ± 9.3 | 13.5-52.5 |
| Resistance-PCV (cm H2O/L/s) | 26.4 ± 11.8 | 6.2-73.5 |
The incidence of VAP was 31.8% (38 cases), with an infection density of 24/1000 d. The 38 cases of VAP, 19 (50%) were of early 19 (50%) were late. The overall mortality rate was 62 cases (51.7%). The mean length of stay in ICU was 15.2 ± 11.1 d and mean duration of mechanical ventilation was 13.1 ± 10.6 d.
Tables 3 and 4 shows the numeric variables compared with VAP rates and outcomes: Mortality.
| Variables | VAP | P value | |
| Yes | No | ||
| APACHE II1 | 29.2 ± 5.6 | 26.5 ± 7.1 | 0.026 |
| Age (yr) | 57.1 ± 19.1 | 59.2 ± 19.6 | 0.565 |
| 1st day (n = 120) | |||
| PaO2/FiO2 (mmHg)1 | 232.3 ± 79.9 | 237.8 ± 105.2 | 0.756 |
| Compliance-VCV (mL/cmH2O) | 43.1 ± 14.9 | 39.8 ± 11.6 | 0.365 |
| Resistance-VCV (cmH2O/L/s) | 13.7 ± 5.0 | 13.0 ± 4.8 | 0.594 |
| Compliance-PCV (mL/cmH2O)1 | 34.8 ± 10.4 | 35.1 ± 9.8 | 0.879 |
| Resistance-PCV (cmH2O/L/s) | 23.6 ± 10.3 | 29.0 ± 18.1 | 0.114 |
| 5th day (n = 77) | |||
| PaO2/FiO2 (mmHg)1 | 244.1 ± 94.1 | 240.2 ± 86.1 | 0.850 |
| Compliance-VCV (mL/cmH2O) | 43.3 ± 14.0 | 37.6 ± 12.3 | 0.092 |
| Resistance-VCV (cmH2O/L/s) | 13.9 ± 6.8 | 13.8 ± 5.5 | 0.996 |
| Compliance-PCV (mL/cmH2O)1 | 33.6 ± 8.9 | 32.5 ± 9.6 | 0.606 |
| Resistance-PCV (cmH2O/L/s) | 27.1 ± 11.7 | 25.9 ± 12.0 | 0.777 |
| (n = 120) | |||
| Duration of MV (d) | 18.4 ± 14.9 | 10.7 ± 6.8 | 0.001 |
| Length of stay in ICU (d) | 20.4 ± 15.3 | 12.8 ± 7.6 | 0.003 |
| Variables | Outcome | P value | |
| High | Death | ||
| APACHE II1 | 27.0 ± 7.6 | 27.7 ± 5.8 | 0.606 |
| Age (yr) | 51.1 ± 19.9 | 65.4 ± 16.1 | < 0.001 |
| 1st day (n = 120) | |||
| PaO2/FiO2 (mmHg)1 | 263.1 ± 100.9 | 210.7 ± 87.8 | 0.003 |
| Compliance-VCV (mL/cm H2O) | 43.5 ± 12.5 | 38.4 ± 12.6 | 0.015 |
| Resistance-VCV (cm H2O/L/s) | 13.3 ± 4.3 | 13.2 ± 5.4 | 0.935 |
| Compliance-PCV (mL/cm H2O)1 | 36.6 ± 9.8 | 33.6 ± 9.9 | 0.103 |
| Resistance-PCV (cm H2O/L/s) | 25.0 ± 10.5 | 29.4 ± 20.0 | 0.416 |
| 5th day (n = 77) | |||
| PaO2/FiO2 (mmHg)1 | 268.8 ± 81.9 | 214.7 ± 87.9 | 0.004 |
| Compliance-VCV (mL/cm H2O) | 40.7 ± 12.7 | 38.7 ± 13.7 | 0.356 |
| Resistance-VCV (cm H2O/L/s) | 14.2 ± 5.0 | 13.5 ± 6.9 | 0.22 |
| Compliance-PCV (mL/cm H2O)1 | 34.1 ± 9.4 | 31.8 ± 9.1 | 0.282 |
| Resistance-PCV (cm H2O/L/s) | 25.7 ± 10.8 | 27.1 ± 12.9 | 0.76 |
| (n = 120) | |||
| Duration of MV (d) | 14.5 ± 12.4 | 11.9 ± 8.6 | 0.212 |
| Length of stay in ICU (d) | 18.3 ± 12.5 | 12.4 ± 8.9 | < 0.001 |
Table 5 presents the relative risk estimate for the variables that demonstrated statistical association with VAP and the outcomes.
| Variables | RR | 95%CI | P value |
| VAP | |||
| APACHE II above the average | 1.62 | 1.03-2.55 | 0.016 |
| Male gender | 1.56 | 1.18-2.08 | 0.004 |
| Resistance worsening-PCV | 1.85 | 1.16-2.94 | 0.01 |
| Outcome: Death | |||
| Age above the average | 2.08 | 1.34-3.23 | 0.001 |
| Compliance-VCV below average on 1st day | 1.49 | 1.00-2.21 | 0.032 |
| ICU stay below the average | 2.05 | 1.28-3.28 | 0.001 |
The general characteristics of the sample were similar to those of other studies on ICU, i.e., most individuals were male and the mean age exceeded middle age[14,23,24].
Among the surveyed patients, the severity of disease classified by the APACHE II was considered relatively high. A research carried out by Wunsch et al[14] analyzed the clinical and epidemiological characteristics of over 170000 patients from 160 ICUs in England and 137 ICUs in the United States. In the United States, the mean APACHE II score was 15.3 ± 8, and for mechanically ventilated subjects, the score was 20.1 ± 8.9. In England, these scores were significantly higher, reaching 20.5 ± 8.5 in the APACHE II score and 22.3 ± 8.2 for individuals undergoing artificial respiration.
A study conducted by Matic et al[25] assessed the influence of the APACHE II score on the selection of the mechanical invasive or non-invasive ventilatory support. The median APACHE II score was 24 in the group that received non-invasive mechanical ventilation, and 26 in the group that required invasive support. These data corroborate the findings of the present study, despite the fact that higher APACHE II scores indicate a more severe clinical condition in patients requiring invasive mechanical ventilatory support. However, the disease severity is related to the characteristics of each ICU, and comorbidities may influence the score, and consequently, the outcomes[26].
With respect to the most common causes of hospitalization in the ICU, the results of this study are in line with the research carried out by Wunsch et al[14], in which the main reasons were of cardiac origin (44.6% in the United States and 27.1% in England), followed by respiratory (20.2% in the United States and 26.3% in England), neurological (19, 1% in the United States. and 24.1% in England) and gastrointestinal (9.5% in the United States and 10.1% in England) causes. These results may differ according to the characteristics of each ICU[27,28].
The length of stay in the ICU and duration of MV were relatively high. According to a review study by Elliott[29], the length of stay for all patient profiles can vary from 2 to 13 d, according to the ICU and the severity of cases. A study by Esteban et al[30] that analyzed the characteristics and outcomes of adult patients requiring mechanical ventilation indicated an average length of stay in the ICU and duration of MV of 13.7 and 7.2 d, respectively. A study by Matic et al[25], also in mechanically ventilated patients, found an average duration in MV of 7 d, and length of stay in ICU of 8.5 d. A Brazilian multicenter study sample consisting of 775 adult patients from 45 ICUs showed that the average length of stay in ICU among subjects requiring only non-invasive ventilation was 7 d. Those who required invasive ventilatory support stayed for 13 d on average[31].
The data regarding the incidence of VAP in the present study were similar to those found in the literature. A review conducted by Joseph et al[15] demonstrated that the incidence can vary from 6% to 52%. The density of VAP infection described in the systematic review by Arabi et al[32] may vary from 10 episodes per 1000 ventilator days, such as in Thailand and Columbia, to 41.7 episodes per 1000 ventilator days in a cancer ICU in Brazil.
By comparing the significant associations of the variables for the development of VAP, it was observed that the APACHE II was a predictor, indicating that severe disease in ICU admission favors the occurrence of VAP. Other studies show no association; however, they describe that higher APACHE II scores are related to higher mortality when applied at the time of VAP diagnosis[33,34].
A longer ICU stay and VM duration are also associated with VAP as demonstrated in this study, which is commonly presented in other works as well. Guimarães et al[35] evaluated 278 patients in a Brazilian university hospital, and reported a significant difference between the group with and without VAP, having stayed in the ICU for 14 and 5 d, respectively. Patients with spinal cord injury who require prolonged mechanical ventilation also had a higher incidence of VAP due to the increased length of ICU stay and MV dependence[36].
As evidenced in this study, the risk for the development of VAP is higher in men than women. According to Tejerina et al[37], 2897 patients from 361 ICUs were surveyed in 20 countries, in which it was shown that men have a relative risk of 1.3 for the occurrence of VAP compared with women.
Worsening resistance during PCV was related to VAP, possibly indicating increased airway inflammation and/or an increase in bronchopulmonary secretions, which is consistent with the pathophysiological mechanism of respiratory infection[21]. A worsening of lung compliance in subjects who developed VAP was also expected, but it did not occur. A study by Lorx et al[38] analyzed patients admitted to the ICU because of community-acquired pneumonia stratified into mild and severe conditions. Using low frequency forced oscillometry technique, it was observed that elastance, which is inversely proportional to compliance, was significantly higher in patients with severe pneumonia compared with those who had mild pneumonia. This evidence demonstrates the restrictive aspect of pneumonia, which was not found in the present study.
Monitoring of respiratory mechanics can assist the intensive care physician to detect early changes in lung function, associating them with the evolution of the ventilation status, and present scores associated with increased risk of mortality and VAP development. In addition, monitoring of mechanical breathing is performed at the bedside, does not involve patient transport, and has no financial cost to be implemented.
The results of the respiratory mechanics of the present study demonstrated a lower compliance and a higher resistance than the predicted values[3,6,12]. This may demonstrate a reduction in lung function of the participants. Advanced age was statistically associated with death as the outcome, which was also observed in other studies[23,30]. Low levels of oxygenation in the 1st and 5th days was also related to mortality, which corroborates the study by Eastwood et al[39] and de Jonge et al[40] that found an association between low levels of oxygenation in the first 24 h and mortality rates in their retrospective observational studies. Low pulmonary compliance during VCV on day 1 also indicated a prediction of mortality in individuals with low pulmonary distensibility. A study by Matić et al[7] monitored the static pulmonary compliance with intraesophageal balloon before intubation. It was shown that poor lung compliance was associated with high mortality rates.
It was expected that the incidence of VAP and higher APACHE II scores were associated with mortality, which was not observed. Generally, VAP is associated with higher mortality rates[15]; however, Tejerina et al[37] found no significant differences between the groups with and without VAP, with an incidence of 38.1% and 37.9%, respectively.
The limitation of this study was the monitoring of respiratory mechanics with sedated patients and not with neuromuscular block. This may have a small influence on the results.
In conclusion, monitoring of the mechanical aspects of lung function is already commonly used in well-established groups with chronic obstructive pulmonary disease and ARDS. It is a simple procedure performed at the bedside, without any physical damage and no additional cost. Based on this assumption, this procedure should be performed routinely in the ICU environment, providing the intensive care physician and the physiotherapist with additional prognosis and diagnosis variables, in addition to the clinical, laboratory and radiological data.
The results show that the respiratory function is a prognostic measure, and is strongly associated with mortality. Low oxygen and low lung compliance during VCV demonstrate this fact. Worsening of respiratory system resistance during PCV, associated with the development of VAP, indicates the possibility of early diagnosis.
The measurements of respiratory mechanics most frequently used are compliance and resistance of the respiratory system. Compliance is associated with distensibility of the respiratory system, which is resulting from the tidal volume variation divided by the peak inspiratory pressure. Resistance is related to the conduction of air, obtained mathematically from the variation between the peak and plateau pressures divided by the inspiratory airflow.
The aim is evaluate the predictive capability of respiratory mechanics for the development of VAP and mortality in the intensive care unit (ICU) of a hospital in southern Brazil.
Respiratory mechanics, ventilator-associated pneumonia.
A cohort study was conducted between, involving a sample of 120 individuals. Static measurements of compliance and resistance of the respiratory system in pressure-controlled ventilation (PCV) and volume-controlled ventilation (VCV) modes in the 1st and 5th days of hospitalization were performed to monitor respiratory mechanics. The severity of the patients’ illness was quantified by the Acute Physiology and Chronic Health Evaluation II (APACHE II). The diagnosis of VAP was made based on clinical, radiological and laboratory parameters.
The significant associations found for the development of VAP were APACHE II scores above the average (P = 0.016), duration of MV (P = 0.001) and ICU length of stay above the average (P = 0.003), male gender (P = 0.004), and worsening of respiratory resistance in PCV mode (P = 0.010). Age above the average (P < 0.001), low level of oxygenation on day 1 (P = 0.003) and day 5 (P = 0.004) and low lung compliance during VCV on day 1 (P = 0.032) were associated with death as the outcome.
The worsening of airway resistance in PCV mode indicated the possibility of early diagnosis of VAP. Low lung compliance during VCV and low oxygenation index were death-related prognostic indicators.
The results show that the respiratory function is a prognostic measure, and is strongly associated with mortality.
Manuscript source: Unsolicited manuscript
Specialty type: Critical Care Medicine
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Jeong KJ, Zhang ZH S- Editor: Cui LJ L- Editor: A E- Editor: Li RF
| 1. | Nguyen YL, Wunsch H, Angus DC. Critical care: the impact of organization and management on outcomes. Curr Opin Crit Care. 2010;16:487-492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Rubenfeld GD, Angus DC, Pinsky MR, Curtis JR, Connors AF Jr, Bernard GR. Outcomes research in critical care: results of the American Thoracic Society Critical Care Assembly Workshop on Outcomes Research. The Members of the Outcomes Research Workshop. Am J Respir Crit Care Med. 1999;160:358-367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 154] [Cited by in F6Publishing: 158] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Henderson WR, Sheel AW. Pulmonary mechanics during mechanical ventilation. Respir Physiol Neurobiol. 2012;180:162-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Hamed HMF, Ibrahim HG, Khater YH, Aziz ES. Ventilation and ventilators in the ICU: What very intensivist must know. Curr Anaesth Crit Care. 2006;17:77-83. [Cited in This Article: ] |
| 5. | Polak AG. Analysis of multiple linear regression algorithms used for respiratory mechanics monitoring during artificial ventilation. Comput Methods Programs Biomed. 2011;101:126-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Lucangelo U, Bernabé F, Blanch L. Respiratory mechanics derived from signals in the ventilator circuit. Respir Care. 2005;50:55-65; discussion 65-67. [PubMed] [Cited in This Article: ] |
| 7. | Matić I, Pavicić F, Sakić-Zdravcević K, Danić D, Jurjević M. Pulmonary compliance values provide prognosis in mechanically ventilated patients--a randomized prospective study. Coll Antropol. 2007;31:829-836. [PubMed] [Cited in This Article: ] |
| 8. | Dhand R. Ventilator graphics and respiratory mechanics in the patient with obstructive lung disease. Respir Care. 2005;50:246-261; discussion 259-261. [PubMed] [Cited in This Article: ] |
| 9. | Koutsoukou A, Perraki H, Orfanos SE, Koulouris NG, Tromaropoulos A, Sotiropoulou C, Roussos C. History of mechanical ventilation may affect respiratory mechanics evolution in acute respiratory distress syndrome. J Crit Care. 2009;24:626.e1-626.e6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Nava S, Rubini F. Lung and chest wall mechanics in ventilated patients with end stage idiopathic pulmonary fibrosis. Thorax. 1999;54:390-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 88] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | D’Angelo E, Calderini E, Robatto FM, Puccio P, Milic-Emili J. Lung and chest wall mechanics in patients with acquired immunodeficiency syndrome and severe Pneumocystis carinii pneumonia. Eur Respir J. 1997;10:2343-2350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Jubran A. Monitoring patient mechanics during mechanical ventilation. Crit Care Clin. 1998;14:629-653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Hellyer TP, Ewan V, Wilson P, Simpson AJ. The Intensive Care Society recommended bundle of interventions for the prevention of ventilator-associated pneumonia. J Intensive Care Soc. 2016;17:238-243. [Cited in This Article: ] |
| 14. | Wunsch H, Angus DC, Harrison DA, Linde-Zwirble WT, Rowan KM. Comparison of medical admissions to intensive care units in the United States and United Kingdom. Am J Respir Crit Care Med. 2011;183:1666-1673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 163] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 15. | Joseph NM, Sistla S, Dutta TK, Badhe AS, Parija SC. Ventilator-associated pneumonia: a review. Eur J Intern Med. 2010;21:360-368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193-204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 396] [Cited by in F6Publishing: 506] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 17. | Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818-829. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10902] [Cited by in F6Publishing: 10643] [Article Influence: 272.9] [Reference Citation Analysis (0)] |
| 18. | Sánchez Casado M, Quintana Díaz M, Palacios D, Hortigüela V, Marco Schulke C, García J, Canabal A, Pérez Pedrero MJ, Velasco Ramos A, Arrese MA. Relationship between the alveolar-arterial oxygen gradient and PaO2/FiO2-introducing PEEP into the model. Med Intensiva. 2012;36:329-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656-659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1848] [Cited by in F6Publishing: 1774] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 20. | Nassar BS, Collett ND, Schmidt GA. The flow-time waveform predicts respiratory system resistance and compliance. J Crit Care. 2012;27:418.e7-418.14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes brasileiras para tratamento das pneumonias adquiridas no hospital e das associadas à ventilação mecânica. J Bras Pneumol. 2007;33 Suppl 1:1-30. [Cited in This Article: ] |
| 22. | Zhang Z. Univariate description and bivariate statistical inference: the first step delving into data. Ann Transl Med. 2016;4:91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 23. | Acuña K, Costa E, Grover A, Camelo A, Santos Júnior R. Clinical-epidemiological characteristics of adults and aged interned in an intensive care unity of the Amazon (Rio Branco, Acre). Rev Bras Ter Intensiva. 2007;19:304-309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Rocha MS, Caetano JÁ, Soares E, Medeiros FL. Caracterização da população atendida em unidade de terapia intensiva: subsídio para a assistência. Rev enferm UERJ. 2007;15:411-416. [Cited in This Article: ] |
| 25. | Matic I, Titlic M, Dikanovic M, Jurjevic M, Jukic I, Tonkic A. Effects of APACHE II score on mechanical ventilation; prediction and outcome. Acta Anaesthesiol Belg. 2007;58:177-183. [PubMed] [Cited in This Article: ] |
| 26. | Norena M, Wong H, Thompson WD, Keenan SP, Dodek PM. Adjustment of intensive care unit outcomes for severity of illness and comorbidity scores. J Crit Care. 2006;21:142-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Doak MW, Nixon AC, Lupton DJ, Waring WS. Self-poisoning in older adults: patterns of drug ingestion and clinical outcomes. Age Ageing. 2009;38:407-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 28. | Sudarsanam TD, Jeyaseelan L, Thomas K, John G. Predictors of mortality in mechanically ventilated patients. Postgrad Med J. 2005;81:780-783. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Elliott D. Measuring the health outcomes of general ICU patients: a systematic review of methods and findings. Aust Crit Care. 1999;12:132-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguía C, Nightingale P. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287:345-355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1117] [Cited by in F6Publishing: 1021] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 31. | Azevedo LC, Park M, Salluh JI, Rea-Neto A, Souza-Dantas VC, Varaschin P, Oliveira MC, Tierno PF, dal-Pizzol F, Silva UV, Knibel M, Nassar AP Jr, Alves RA, Ferreira JC, Teixeira C, Rezende V, Martinez A, Luciano PM, Schettino G, Soares M; ERICC (Epidemiology of Respiratory Insufficiency in Critical Care) investigators. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care. 2013;17:R63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 105] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 32. | Arabi Y, Al-Shirawi N, Memish Z, Anzueto A. Ventilator-associated pneumonia in adults in developing countries: a systematic review. Int J Infect Dis. 2008;12:505-512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 33. | Huang KT, Tseng CC, Fang WF, Lin MC. An early predictor of the outcome of patients with ventilator-associated pneumonia. Chang Gung Med J. 2010;33:274-282. [PubMed] [Cited in This Article: ] |
| 34. | Mirsaeidi M, Peyrani P, Ramirez JA; Improving Medicine through Pathway Assessment of Critical Therapy of Hospital-Acquired Pneumonia (IMPACT-HAP) Investigators. Predicting mortality in patients with ventilator-associated pneumonia: The APACHE II score versus the new IBMP-10 score. Clin Infect Dis. 2009;49:72-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Guimarães MMQ, Rocco JR. Prevalência e prognóstico dos pacientes com pneumonia associada à ventilação mecânica em um hospital universitário. Bras Pneumol. 2006;32:339-346. [Cited in This Article: ] |
| 36. | García-Leoni ME, Moreno S, García-Garrote F, Cercenado E. Ventilator-associated pneumonia in long-term ventilator-assisted individuals. Spinal Cord. 2010;48:876-880. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Tejerina E, Frutos-Vivar F, Restrepo MI, Anzueto A, Abroug F, Palizas F, González M, D’Empaire G, Apezteguía C, Esteban A; Internacional Mechanical Ventilation Study Group. Incidence, risk factors, and outcome of ventilator-associated pneumonia. J Crit Care. 2006;21:56-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 98] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 38. | Lorx A, Suki B, Hercsuth M, Szabó B, Pénzes I, Boda K, Hantos Z. Airway and tissue mechanics in ventilated patients with pneumonia. Respir Physiol Neurobiol. 2010;171:101-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Eastwood G, Bellomo R, Bailey M, Taori G, Pilcher D, Young P, Beasley R. Arterial oxygen tension and mortality in mechanically ventilated patients. Intensive Care Med. 2012;38:91-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 40. | de Jonge E, Peelen L, Keijzers PJ, Joore H, de Lange D, van der Voort PH, Bosman RJ, de Waal RA, Wesselink R, de Keizer NF. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care. 2008;12:R156. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 239] [Cited by in F6Publishing: 251] [Article Influence: 15.7] [Reference Citation Analysis (0)] |