Published online Nov 4, 2017. doi: 10.5492/wjccm.v6.i4.185
Peer-review started: April 21, 2017
First decision: July 18, 2017
Revised: July 26, 2017
Accepted: September 3, 2017
Article in press: September 4, 2017
Published online: November 4, 2017
To prospectively evaluate the reproducibility of diaphragm thickness measurement by ultrasonography at the bedside by critical care physicians in patients on invasive mechanical ventilation.
In a prospective observational study of 64 invasively ventilated patients, diaphragmatic thickness measurement was taken by 2 different observers at the same site. Three measurements were taken by each observer and averaged. The intraobserver and interobserver variability was assessed by estimation of intraclass correlation coefficient. The limits of agreement were plotted as the difference between two observations against the average of the two observations in Bland and Altman analysis.
The mean diaphragm thickness at the functional residual capacity was 2.29 ± 0.4 mm and the lower limit of the normal, i.e., the 5th percentile was 1.7 mm (95%CI: 1.6-1.8). The intraclass correlation coefficient for intraobserver variability was 0.986 (95%CI: 0.979-0.991) with a P value of < 0.001. The intraclass correlation coefficient for interobserver variability was 0.987 (95%CI: 0.949-0.997) with a P value of < 0.001. In Bland and Altman analysis, both intraobserver and interobserver measurements showed high limits of agreement.
Our study demonstrates that the measurement of diaphragm thickness by ultrasound can be accurately performed by critical care physicians with high degree of reproducibility in patients on mechanical ventilation.
Core tip: Ultrasonography (USG) is a cheap, cost effective and non-invasive bedside tool for evaluation of diaphragm thickness during mechanical ventilation. Measurement of diaphragm thickness by USG can be accurately performed by critical care physicians with high degree of reproducibility. USG should be used more often by the physicians in the intensive care unit for the assessment of the diaphragm.
- Citation: Dhungana A, Khilnani G, Hadda V, Guleria R. Reproducibility of diaphragm thickness measurements by ultrasonography in patients on mechanical ventilation. World J Crit Care Med 2017; 6(4): 185-189
- URL: https://www.wjgnet.com/2220-3141/full/v6/i4/185.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v6.i4.185
Invasive mechanical ventilation causes progressive decline in diaphragm bulk and strength in a phenomenon called ventilator induced diaphragm dysfunction[1]. Diaphragm movement and function can be assessed by various methods which include chest X-ray, supine vital capacity, maximum inspiratory pressure, electromyography and magnetic phrenic nerve stimulation. Ultrasonography (USG) is a cheap, cost effective and non-invasive bedside tool for evaluation of diaphragm thickness. It has been used successfully to measure diaphragm thickness and movement in ambulatoryin dividuals[2,3]. Diaphragm thickness is a surrogate of its strength and helps to predict the outcome of extubation in patients on mechanical ventilation[4,5]. However, localization and measurement may be more difficult in critically ill ventilated patients in the intensive care unit (ICU) due to significant subcutaneous edema and supine position. The variability may also be due to variation in image acquisition and interpretation.
This was a prospective observational study done in mechanically ventilated patients admitted to the Pulmoanry Medicine ICU, All India Institute of Medical Sciences, New Delhi. Ethical clearance was obtained from the Institute Ethics Committee and written informed consent was obtained in all patients. Diaphragm measurements were taken within the 1st 24 h of ICU admission.
The inclusion criteria including: (1) patients aged > 18 years and requiring endotracheal intubation and mechanical ventilation; and (2) admitted to the ICU within 72 h of initiation of mechanical ventilation.
The exclusion criteria including: (1) mechanical ventilation for more than 72 h before admission; (2) any form of mechanical ventilation in the preceding 3 mo or those who are on home non-invasive or invasive ventilation; (3) surgical dressings over the right lower rib cage; and (4) surrogates of the patient not willing for consent.
Both observers who conducted the ultrasonography were provided training in ultrasonographic measurement of diaphragm thickness by a radiologist in 3 sessions, each session lasting 30 min.
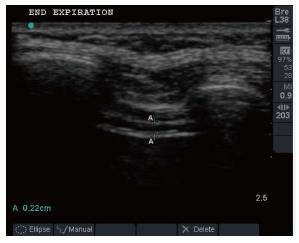
All ultrasound examinations were done with Sonosite Micromaxx Portable Ultrasound Machine (Sonosite, Inc. United States) using the B-mode and a 5-10 MHz linear transducer. Patients were put in a supine position at 0 °C of incline. The same incline was used for all subsequent measurements for a given patient. Diaphragm thickness was measured in right hemi diaphragm in the zone of apposition. USG probe was positioned at the 8th or 9th right intercostal space with vertical orientation in the mid-axillary line and adjusted until the diaphragm was properly visualised. The distal end of the transducer was marked with permanent ink. The diaphragm was identified as the last set of parallel lines, the pleural and peritoneal membranes overlying the less echogenic muscle. Figure 1 shows an USG sample image of a patient taken at end expiration. Three measurements of the diaphragm thickness were taken and averaged to report the mean. In 10 randomly selected patients, diaphragm thickness was re-measured on the same day by 2nd observer who was blinded to the results of the 1st observer. The results of diaphragm measurements were not revealed to the treating physician nor it was taken into consideration in any clinical decision-making or management of the patients.
The primary outcome was intraobserver and interobserver variability of the measurements. The intraobserver variability was assessed by estimation of intraclass correlation coefficient using the three observations in the same patient by the 1st observer. Interobserver variability was tested between observations made by the 1st and the 2nd observers in the same subjects. The limits of agreement were plotted as the difference between two observations against the average of the two observations in Bland and Altman analysis. Data was analysed using International Business Machine (IBM) SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.
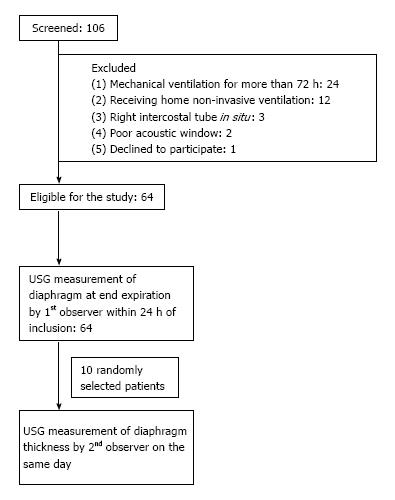
A total of 106 patients admitted to the ICU were assessed for eligibility and inclusion into the study. Forty two of the 106 were excluded as they did not meet the eligibility criteria. Right hemidiaphragm localisation for measurement of thickness was successful in 64 out of 66 (97%) subjects. The flow of the patients enrolled into the study is shown in Figure 2.
The mean age of the study population was 54.5 ± 15.3 years. The mean diaphragm thickness at the functional residual capacity was 2.29 ± 0.4 mm and the lower limit of the normal, i.e., the 5th percentile was 1.7 mm (95%CI: 1.6-1.8).The baseline characteristic of the study population is depicted in Table 1.
| Classification | Quantity, n (%) |
| Mean age, yr | 54.5 ± 15.3 |
| Male sex | 45 (70) |
| Diagnoses | |
| COPD | 20 (31) |
| Post tuberculosis sequelae | 11 (17) |
| Interstitial lung disease | 8 (13) |
| Asthma | 5 (8) |
| Lung cancer | 5 (8) |
| Others1 | 15 (23) |
| Mean apache II score at admission | 15.5 ± 5.3 |
| Mean diaphragm thickness at FRC (mm) | 2.29 ± 0.4 |
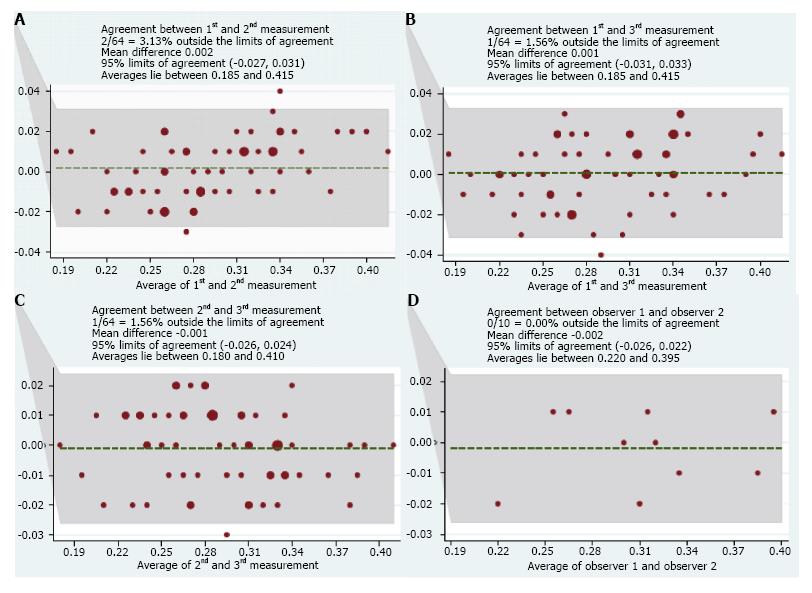
The intraclass correlation coefficient was 0.986 (95%CI: 0.979-0.991) with a P value of < 0.001. In Bland and Altman plots, 2 out of 64 observations were outside the limits of agreement when first and second measurements were compared. Similarly 1 out of 64 observations was outside the 95% limit of agreement when the second and third or first and third measurements were compared.
The intraclass correlation coefficient of interobserver variability was 0.987 (95%CI: 0.949-0.997) with a P value of < 0.001. In Bland and Altman analysis, no measurements were outside the limit of agreement. Bland and Altman plots of intraobserver and interobserver agreement are shown in Figure 3.
Diaphragm is the principal muscle of respiration and its proper functioning is the critical determinant of the ability of a patient to be successfully weaned from mechanical ventilation. Assessment of diaphragm thickness and function is relevant to clinical practice because diaphragm dysfunction is an important cause of complications in mechanically ventilated patients[1,4]. We were able to successfully measure diaphragm thickness in 64 of the 66 (97%) patients who were eligible to participate in the study. This finding is important as measurement of diaphragm thickness by USG is an easy to learn, non-invasive bedside tool and is hazard free. It also avoids the hassle of shifting the patients out of the ICU and the associated complications.
Previous studies have shown that USG measurements of diaphragm thickness and movement have high degree of reproducibility in both spontaneously breathing and mechanically ventilated patients[6-8]. In the study by DiNino et al[5] diaphragm thickness was measured by an intensivist after an initial training of three to five sessions lasting ten to 15 min each. The intra-observer variability after such training was less than 10%. Similarly, in the study by Schepens et al[9] the coefficient of reproducibility was high (0.945 for intra-observer and 0.971 for inter-observer variability). Francis et al[10] also demonstrated both to be greater than 0.95. The intraclass correlation coefficients of both intra and inter observer variability in our study was high. Our study demonstrates that the measurement of diaphragm thickness by ultrasound can be accurately performed by critical care physicians after a short training with high degree of reproducibility.
The mean diaphragm thickness in our cohort was 2.29 ± 0.4 mm and the lower limit of normal was 1.7 mm (95%CI: 1.6-1.8). Prior studies have reported a diaphragm thickness in the range of 1.5 to 3.2 mm in normal healthy population[6,11,12]. The diaphragm thickness and contractility are minimally affected by age, body habitus and smoking history and may differ in different population. Majority of the patients in our study had underlying chronic respiratory disorder, as the most common diagnoses were chronic obstructive pulmonary disease (COPD), post tuberculosis sequelae, interstitial lung disease, asthma and lung cancer. The mean diaphragm thickness in COPD patients, as reported by Baria et al[12] was 2.8 mm and the lower limit of normal was 1.4 mm. The diaphragm thickness in COPD population was lesser than the normal controls. There was also a wider deviations of diaphragm thickness from the mean in those with COPD as compared to the controls (SD = 1.6 vs 1.3 mm for COPD and controls respectively).
Our study also has some limitations. Though we analysed the intraobserver variability of diaphragm thickness measurements in all included patients, interobserver variability was only evaluated in 10 randomly selected patients in the study cohort. This was due to technical difficulties in performing ultrasonography twice in all patients. Hence, the results of interobserver agreements may need to be replicated in a larger cohort. All the measurements were taken by physicians trained in critical care ultrasonography and the radiologist was only involved in the initial training of the observers. Another limitation of the study is that we only used B mode for the measurement of diaphragm thickness. M mode USG has also been suggested by some authors as an alternative modality to assess diaphragmatic excursions[2,8]. Reproducibility compared to a radiologist derived measurement would have added more value to the results.
In conclusion, the results of our study indicate that the measurement of diaphragm thickness by ultrasound can be accurately performed by critical care physicians with high degree of reproducibility. Hence, USG should be used more often by the physicians in the ICU for the assessment of the diaphragm.
Ultrasonography (USG) is a cheap, cost effective and non-invasive bedside tool for evaluation of diaphragm thickness and function during mechanical ventilation. However, there may be variability in the measurement of diaphragm thickness by USG due to variation in image acquisition and interpretation.
The reproducibility of diaphragm thickness measurement by critical care physicians at bedside needs to be further explored. The results from this study suggest that the intraobserver and interobserver agreements of the measurements by critical care physicians after adequate training is high.
This study adds to the current literature of evidence that USG can be used at the bedside to measure diaphragm thickness during mechanical ventilation even by critical care physicians, and can be used as a guide to assess weaning outcomes.
USG should be used more often by the physicians in the intensive care unit for the assessment of the diaphragm.
USG: A technique using echoes of ultrasound pulses to delineate objects or areas of different density in the body. Diaphragm: The principal muscle of inspiration muscle that separates the chest (thoracic) cavity from the abdomen. Mechanical ventilation: The technique through which gas is moved toward and from the lungs through an external device connected directly to the patient.
The authors describe a study to evaluate the interobserver agreement of sonographic measurement of the diaphragm thickness in 64 ventilated patients.
Manuscript source: Unsolicited manuscript
Specialty type: Critical care medicine
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: He HW, Muensterer OH, Zhang ZH S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
| 1. | Vassilakopoulos T, Petrof BJ. A Stimulating Approach to Ventilator-induced Diaphragmatic Dysfunction. Am J Respir Crit Care Med. 2017;195:281-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 299] [Cited by in F6Publishing: 288] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 2. | Gerscovich EO, Cronan M, McGahan JP, Jain K, Jones CD, McDonald C. Ultrasonographic evaluation of diaphragmatic motion. J Ultrasound Med. 2001;20:597-604. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 222] [Cited by in F6Publishing: 211] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | Wait JL, Nahormek PA, Yost WT, Rochester DP. Diaphragmatic thickness-lung volume relationship in vivo. J Appl Physiol. 1989;67:1560-1568. [PubMed] [Cited in This Article: ] |
| 4. | Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39:2627-2630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 280] [Cited by in F6Publishing: 287] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 5. | DiNino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successfulextubation from mechanical ventilation. Thora. 2014;69:423-427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 246] [Cited by in F6Publishing: 249] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 6. | Cohn D, Benditt JO, Eveloff S, McCool FD. Diaphragm thickening during inspiration. J Appl Physiol. 1997;83:291-296. [PubMed] [Cited in This Article: ] |
| 7. | Vivier E, Mekontso Dessap A, Dimassi S, Vargas F, Lyazidi A, Thille AW, Brochard L. Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensive Care Med. 2012;38:796-803. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 203] [Cited by in F6Publishing: 201] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 8. | Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135:391-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 391] [Cited by in F6Publishing: 410] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 9. | Schepens T, Verbrugghe W, Dams K, Corthouts B, Parizel PM, Jorens PG. The course of diaphragm atrophy in ventilated patients assessed with ultrasound: a longitudinal cohort study. Crit Care. 2015;19:422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 10. | Francis CA, Hoffer JA, Reynolds S. Ultrasonographic Evaluation of Diaphragm Thickness During Mechanical Ventilation in Intensive Care Patients. Am J Crit Care. 2016;25:e1-e8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen JA, Watson JC, Sorenson EJ. Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve. 2013;47:884-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 170] [Cited by in F6Publishing: 184] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 12. | Baria MR, Shahgholi L, Sorenson EJ, Harper CJ, Lim KG, Strommen JA, Mottram CD, Boon AJ. B-mode ultrasound assessment of diaphragm structure and function in patients with COPD. Chest. 2014;146:680-685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |