Published online Nov 18, 2017. doi: 10.5312/wjo.v8.i11.836
Peer-review started: January 6, 2017
First decision: February 17, 2017
Revised: March 20, 2017
Accepted: April 6, 2017
Article in press: April 10, 2017
Published online: November 18, 2017
To correlate the Pang and Lee class with the clinical course in a consecutive series of patients presenting with painful torticollis.
Forty-seven dynamic rotational computed tomography (CT) scans in 35 patients were classified into one of the five types defined by Pang and Li, including types I (atlantoaxial rotatopry fixation), II (“pathologic stickiness” without crossover of C1 on C2), III (“pathologic stickiness” with crossover of C1 on C2), IV (normal or muscular torticollis), and V (diagnostic grey zone). The Pang and Li class was then compared with the radiologist’s report, which was graded abnormal, diagnosis of rotatory subluxation or fixation, or non-diagnostic. Medical records were reviewed and the clinical course was compared among the five sub-types.
We reviewed 47 CT scans in 35 patients, and the majority were performed without sedation. The average age was 7.7 years (4-14 years old) and associated conditions included minor trauma (20%), surgical procedures around the head and neck (29%), and Grisels syndrome (20%). Twenty-six percent of our studies fell within the pathologic spectrum (5% type 1 or rotatory fixation, 21% types 2 and 3 or rotatory subluxation), while 45% were classified as muscular torticollis (45%) and 28% fell within the diagnostic grey zone. Seven radiologists interpreted these studies, and their interpretation was discordant in 45% of cases. Clinical resolution occurred in 27 of 29 cases for which follow-up was available. One of two patients with fixed rotatory subluxation required a C1-C2 arthrodesis.
The Pang and Li classification characterizes a spectrum of abnormalities in rotation to facilitate communication, although the indications for dynamic CT scan should be further defined.
Core tip: Atlantoaxial rotatory displacement represents a spectrum of pathology. We classified 47 computed tomography (CT) scans in 35 patients presenting with painful torticollis according to Pang and Li, and found that the radiologist’s interpretation was discordant in 45%, suggesting the need to develop a common language with our imaging colleagues to accurately describe this pathology in the individual patient. Most patients resolved with non-operative treatment, although one of two with fixed rotatory subluxation required a fusion. As 74% were classified as muscular torticollis (45%) or fell within the diagnostic grey zone (28%), the indications for a dynamic CT scan should be revisited.
- Citation: Spiegel D, Shrestha S, Sitoula P, Rendon N, Dormans J. Atlantoaxial rotatory displacement in children. World J Orthop 2017; 8(11): 836-845
- URL: https://www.wjgnet.com/2218-5836/full/v8/i11/836.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i11.836
A variety of terms have been used to describe a spectrum of rotational abnormalities of the atlantoaxial joint observed in the absence of major trauma, most commonly atlantoaxial rotatory displacement, atlanto-axial rotatory subluxation (AARS) and atlanto-axial rotatory fixation (AARF)[1-12]. This lack of uniformity in terminology reflects the challenges of capturing dynamic rotational abnormalities occurring within the physiologic range of motion. As a loss of contact between the facets at C1 and C2 of up to 85% occurs during the extremes of physiologic rotation, subluxation is a normal finding and “pathologic” cannot be defined by the relationships between C1 and C2 at any particular point within the arc of rotation[13,14]. The dynamic computed tomography (CT) scan has been utilized to evaluate children presenting with a painful torticollis, although diagnostic imaging criteria have not been established. Pang and Li have developed a diagnostic approach in which measurements extracted from the dynamic rotational CT scan are plotted on a graph and compared with normative data[5-7]. The goal of this retrospective radiographic and clinical review is to correlate the Pang and Li class with the clinical course in a consecutive series of patients presenting with painful torticollis.
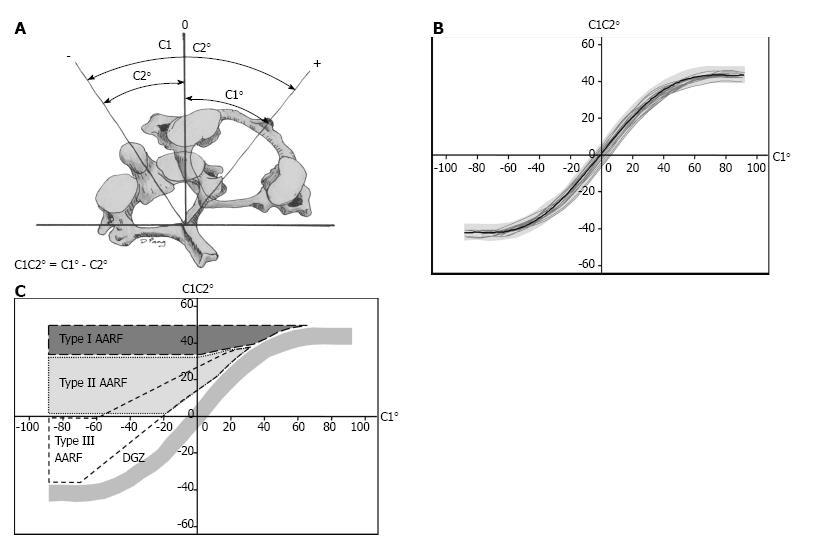
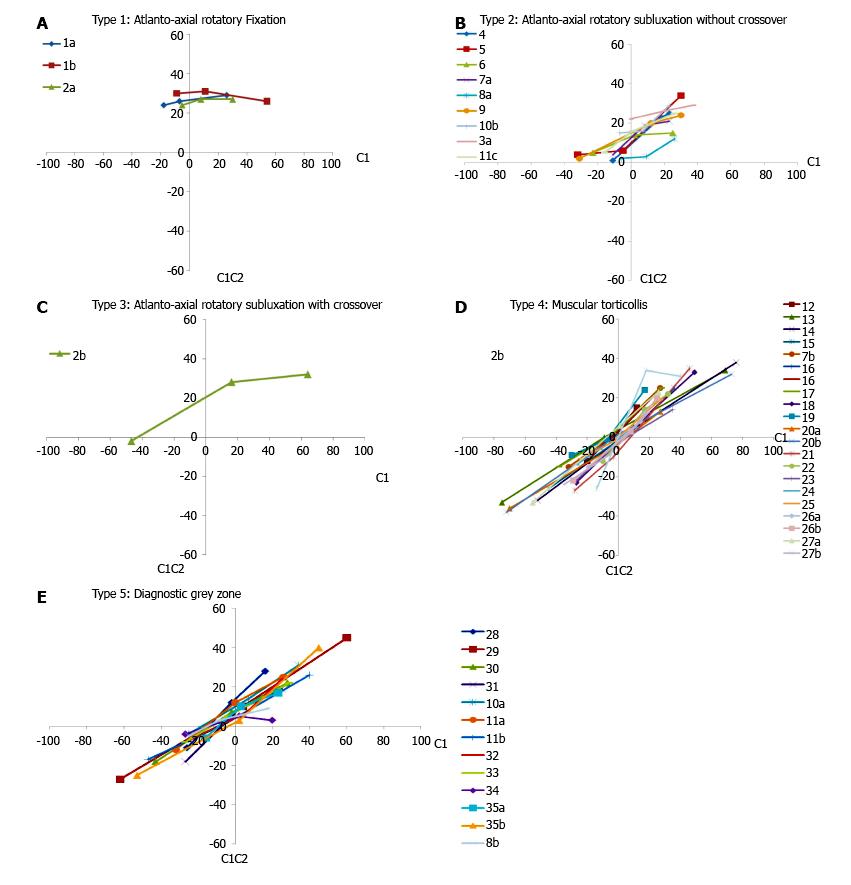
Pang and Li first defined normal composite rotational motion curves from dynamic rotational CT scans in 21 pediatric patients who had no signs or symptoms of atlanto-axial rotatory dysfunction (3 to 11.5 years of age)[5]. For each position of cervical rotation, they first measure the angle between the vertical axis and the sagittal axis of the occiput, C1, and C2. They then plot the C1 angle (head position) on the X axis and the C1-C2 angle (angle of separation or divergence) on the Y axis (Figures 1A and B). They identified three distinct phases within the normal motion curve (Figure 1B). C1 rotates in isolation during the first or “single motion” phase (0°-23°), and from 24°-63° both C1 and C2 rotate at different rates increasing the angle of separation or divergence to a maximum of approximately 45°. Rotation beyond 63° occurs through the subaxial spine with no further divergence between C1 and C2. C1 normally crosses over C2 at the zero or null point. This normative data provides a template of how C1 and C2 relate throughout the range of head positions, and was compared with data from patients presenting with painful torticollis to develop a classification system (Figure 1C)[6,7]. In patients with type I dynamics, C1 and C2 are locked (< 20% correction in separation angle through range of motion). This type might be referred to as AARF. In type II and type III there is a “pathologic stickiness” between C1 and C2; while mobility between C1 and C2 is preserved (> 20% correction in separation angle), C1 either does not (type II) or does (type III) cross over C2. Normal dynamics are observed in type 4 (muscular torticollis). In the type 5 or diagnostic grey zone, C1 crosses over C2 at a point between 8 and 20 degrees beyond the midline; the authors feel that this may represent a transitional type of dynamics which may either revert to normal or progress to one of the more severe forms of the condition. For clinical applications, the authors obtain the CT scan with the patients head in a comfortable position (P or presenting position, side to which the chin is rotated), with the nose pointing straight upwards (P0 or neutral position, partially corrected), and with the head rotated maximally to the opposite side (P-, maximally corrected position). By convention all values towards the presenting side are positive, and towards the opposite or corrected side are negative (Figure 1A).
We searched the database from our radiology department to identify all patients who underwent a dynamic rotational CT scan over seven consecutive years since a digital imaging system became available. Approval from the Institutional Review Board was obtained. The imaging protocol involved 1.5 millimeter cuts between the occiput and C3 with the patient’s shoulders flat and the head positioned at neutral, and with maximal voluntary rotation to the right and to the left. Digital calipers were used to measure the angle between the vertical axis and the sagittal axis of each bone (occiput, C1, and C2) at all three positions of cervical rotation (right, left, neutral). The angle of divergence between C1 and C2 (C1-C2 angle) was also calculated for each position of rotation. Three observers evaluated each CT scan independently (PS, SS, DS), and the reviewed each study together and constructed the graphs which were compared with the normative template provided by Pang and Li (types I-III = abnormal or within spectrum of AARS), type 4 = normal, type 5 = Diagnostic Grey Zone) (Figures 1B and 2). We reviewed the radiologist’s interpretation, which we graded as (1) positive (diagnosed as AARS or AARF); (2) negative; or (3) non-diagnostic.
We then reviewed each patient’s medical records with regard to age, gender, potential associations (minor trauma, inflammatory conditions, recent surgery around the head or neck), delay from symptom onset to presentation, treatment prior to referral, treatment course including immobilization, and outcomes (resolved, persisted, recurrent). We correlated the patient’s overall treatment course and outcomes for each of the 5 types. Patients who were imaged more than once were grouped according to their most severe type.
We reviewed 47 CT scans in 35 patients, and only 26% (12/47) of our studies fell within the pathologic spectrum from rotatory subluxation (21% types 2 and 3) to rotatory fixation (5% type I) (Table 1). Forty-five percent fell within the physiologic range (muscular torticollis), and 28% were in the diagnostic grey zone. Ten of our patients were imaged more than once. Normal dynamics was observed in two separate studies in 3 patients. One follow-up study demonstrated restoration of normal dynamics, and improvement was observed in 3 cases (type 1-3, type 2-4, type 2-5). There was either no change or progression to a higher class in 3 cases. A single patient had 3 studies performed, and while the first two were classified in the diagnostic grey zone, the third demonstrated type II dynamics. Two of these studies were performed with sedation, and a third in the operating room under general anesthesia.
| Pt. # | Rotation | Presenting position (P)(maximum rotation towards presenting side) | Neutral (Po)(partially corrected position) | Corrected position (P-)(best corrected position) | % Correction | Pang class | Rad int | Radiologist | |||||||||
| Oc | C1 | C2 | C1C2 | Oc | C1 | C2 | C1C2 | Oc | C1 | C2 | C1C2 | ||||||
| 1a | R | 30 | 26 | -3 | 29 | -1 | -7 | -31 | 26 | -22 | -18 | -42 | 24 | 17% | 1 | Yes | 4 |
| 1b | L | 45 | 54 | 31 | 26 | 13 | 11 | -20 | 31 | -23 | -9 | -39 | 30 | 15% | 1 | Yes | 1 |
| 2a | L | 17 | 30 | -3 | 27 | -3 | 8 | -21 | 27 | -15 | -5 | -29 | 24 | 11% | 1 | ND | 1 |
| 3a | L | 38 | 37 | 8 | 29 | 20 | 19 | -7 | 26 | -2 | -1 | -23 | 22 | 24% | 2 | Yes | 3 |
| 4 | L | 24 | 23 | -2 | 25 | 16 | 18 | -5 | 23 | -10 | -11 | -12 | 1 | 96% | 2 | Yes | 2 |
| 5 | L | 29 | 30 | -4 | 34 | 4 | -5 | -11 | 6 | -30 | -32 | -36 | 4 | 88% | 2 | ND | 7 |
| 6 | L | 23 | 25 | 10 | 15 | 2 | 2 | -12 | 14 | -20 | -23 | -28 | 5 | 66% | 2 | No | 1 |
| 7a | R | 18 | 23 | 2 | 21 | -2 | 8 | -11 | 19 | -19 | -11 | -15 | 4 | 81% | 2 | Yes | 2 |
| 8a | R | 25 | 26 | 14 | 12 | 7 | 9 | 6 | 3 | -3 | -6 | -8 | 2 | 83% | 2 | ND | 7 |
| 9 | L | 24 | 30 | 6 | 24 | 4 | 12 | -8 | 20 | -34 | -31 | -33 | 2 | 92% | 2 | No | 3 |
| 10b | R | 16 | 23 | -6 | 29 | -4 | 7 | -9 | 16 | -22 | -7 | -22 | 15 | 91% | 2 | Yes | 2 |
| 11c | L | 21 | 26 | 1 | 25 | -7 | 1 | -15 | 16 | -25 | -16 | -21 | 5 | NA | 2 | Yes | 5 |
| 2b | L | 53 | 64 | 32 | 32 | -2 | 16 | -12 | 28 | -61 | -47 | -45 | -2 | NA | 3 | Yes | 1 |
| 12 | L | 10 | 12 | -3 | 15 | -2 | -4 | -4 | 0 | -13 | -20 | -8 | -12 | NA | 4 | No | 1 |
| 13 | L | 67 | 69 | 35 | 34 | -6 | -9 | -9 | 0 | -80 | -75 | -42 | -33 | NA | 4 | No | 2 |
| 14 | R | 73 | 76 | 38 | 38 | 2 | 11 | 6 | 5 | -58 | -52 | -20 | -32 | NA | 4 | No | 1 |
| 15 | R | 34 | 36 | 11 | 25 | 8 | 10 | 6 | 4 | -48 | -45 | -19 | -26 | NA | 4 | No | 7 |
| 7b | R | 27 | 27 | 2 | 25 | -10 | -10 | -7 | -3 | -30 | -32 | -17 | -15 | NA | 4 | Yes | 1 |
| 16 | R | 22 | 23 | 2 | 21 | -1 | -1 | -3 | 2 | -20 | -18 | -9 | -9 | NA | 4 | ND | 7 |
| 17 | R | 33 | 28 | 3 | 25 | -1 | -3 | -5 | 2 | -38 | -38 | -23 | -15 | NA | 4 | ND | 4 |
| 18 | R | 44 | 49 | 16 | 33 | 5 | 10 | 5 | 5 | -33 | -27 | -4 | -23 | NA | 4 | No | 5 |
| 19 | R | 18 | 17 | -7 | 24 | -7 | -7 | -6 | -1 | -28 | -30 | -21 | -9 | NA | 4 | No | 1 |
| 20a | L | 24 | 27 | 14 | 13 | -6 | -1 | 3 | -4 | -71 | -70 | -34 | -36 | NA | 4 | ND | 3 |
| 20b | L | 76 | 73 | 41 | 32 | -5 | 1 | 3 | 2 | -71 | -72 | -34 | -38 | NA | 4 | No | 1 |
| 21 | R | 47 | 46 | 11 | 35 | -2 | -3 | 7 | -10 | -29 | -28 | -1 | -27 | NA | 4 | No | 2 |
| 22 | L | 20 | 32 | 10 | 22 | 8 | 17 | 6 | 14 | -20 | -10 | 2 | -12 | NA | 4 | ND | 3 |
| 23 | L | 32 | 35 | 21 | 14 | -1 | -1 | 2 | -3 | -28 | -27 | -5 | -22 | NA | 4 | No | 2 |
| 24 | L | 9 | 11 | 6 | 5 | 9 | -12 | -6 | -6 | -22 | -27 | -13 | -14 | NA | 4 | No | 7 |
| 25 | L | 27 | 27 | 24 | 19 | 5 | -3 | -1 | -2 | -20 | -24 | -13 | -11 | NA | 4 | No | 1 |
| 26a | L | 15 | 17 | 5 | 12 | 15 | 14 | 6 | 8 | -21 | -19 | -4 | -15 | NA | 4 | ND | 7 |
| 26b | L | 23 | 25 | 5 | 20 | 7 | 8 | 5 | 3 | -29 | -29 | -7 | -22 | NA | 4 | ND | 3 |
| 27a | L | 27 | 26 | 3 | 23 | 1 | 1 | -5 | 6 | -64 | -55 | -22 | -33 | NA | 4 | ND | 1 |
| 27b | L | 24 | 20 | 7 | 13 | -3 | -6 | 3 | -9 | -30 | -35 | -11 | -24 | NA | 4 | No | 3 |
| 3b | R | 37 | 40 | 9 | 31 | 16 | 18 | -16 | 34 | -12 | -14 | 12 | -26 | NA | 4 | Yes | 3 |
| 8b | L | 18 | 18 | 12 | 9 | -6 | -9 | -12 | 3 | -21 | -25 | -20 | -5 | NA | 5 | ND | 5 |
| 28 | R | 18 | 16 | -12 | 28 | 1 | -2 | -14 | 12 | -23 | -26 | -15 | -11 | NA | 5 | No | 1 |
| 29 | L | 66 | 60 | 16 | 45 | 1 | 4 | -6 | 10 | -69 | -62 | -35 | -27 | NA | 5 | No | 2 |
| 30 | R | 31 | 28 | 6 | 22 | -3 | -2 | -9 | 7 | -42 | -43 | -25 | -18 | NA | 5 | No | 1 |
| 31 | L | 23 | 25 | 6 | 19 | 3 | 1 | -7 | 8 | -20 | -27 | -9 | -18 | NA | 5 | Yes | 2 |
| 10a | R | 30 | 34 | 3 | 31 | -2 | 7 | -7 | 14 | -29 | -25 | -21 | -4 | NA | 5 | Yes | 2 |
| 11a | L | 21 | 26 | 1 | 25 | 7 | 0 | -12 | 12 | -34 | -32 | -20 | -12 | NA | 5 | Yes | 1 |
| 11b | L | 33 | 40 | 14 | 26 | -6 | -6 | -7 | 1 | -62 | -47 | -30 | -17 | NA | 5 | Yes | 6 |
| 32 | R | 25 | 25 | 1 | 24 | 2 | 6 | -13 | 7 | -25 | -27 | -19 | -8 | NA | 5 | No | 3 |
| 33 | R | 29 | 29 | 7 | 22 | -2 | -4 | -9 | 5 | -27 | -27 | -19 | -8 | NA | 5 | No | 7 |
| 34 | L | 22 | 20 | 23 | 3 | 3 | 2 | -3 | 5 | -29 | -27 | -23 | -4 | NA | 5 | No | 7 |
| 35a | L | 21 | 23 | 6 | 17 | 4 | 3 | -7 | 10 | -18 | -16 | -12 | -6 | NA | 5 | Yes | 2 |
| 35b | L | 41 | 45 | 5 | 40 | -1 | 2 | -1 | 3 | -50 | -53 | -18 | -25 | NA | 5 | Yes | 1 |
Seven radiologists interpreted these studies. For studies classified as types 1 through 3, the radiologist’s interpretation was concordant in 8/13 (62%) (Table 1). Two of the other 5 studies were read as normal and three were non-diagnostic. In the 21 studies graded as type 4 (normal or muscular torticollis), 12 (57%) were read as normal and of the remaining 9 (43%) were read as AARF (2) or non-diagnostic (7). For those studies in the diagnostic grey zone (type 5), the radiologists interpreted 46% (6/13) as normal, 46% (6/13) as AARF, and 8% (1/13) as non-diagnostic.
Our study population included 19 females and 16 males, and the average age was 7.7 years (range 4-14 years). All patients had neck pain, torticollis, and a normal neurologic examination. Associated conditions are listed in Table 2, and included minor trauma (20%), craniofacial or ENT procedures (29%), and Grisel syndrome (20%). Sufficient clinical information could be retrieved for 29 of 35 patients (Table 3). The time from the onset of symptoms to presentation ranged from three days to five months, and seven of the patients were treated by a variety of methods prior to referral to our orthopaedic service. Three patients were evaluated in our emergency room and were never seen by orthopaedics, while two others were seen once as outpatients for a second opinion. Patients having more than one study are grouped according to their highest grade of involvement.
| Associations | Pang class and associations | |
| Minor trauma (7) | I | Minor trauma (2) |
| ENT or craniofacial procedures (10) | II | Craniofacial procedures (3) |
| ENT procedures (3) | ||
| Grisels (1) | ||
| Unknown (2) | ||
| Grisels (7) | III | Minor trauma (1) |
| Unknown (8) | IV | Unknown (6) |
| ENT procedures (3) | ||
| Grisels (3) | ||
| Minor trauma (3) | ||
| Occipital condyle fracture (1) | ||
| Occipital condyle fracture (1) | V | Grisels (3) |
| ENT procedures (2) | ||
| Down syndrome (1) | Minor trauma (2) | |
| Unknown (1) | ||
| Congenital muscular torticollis (1) | Down syndrome (1) | |
| Pt # | Pang | Age | Gen | History | Delay to initial presentation | Prior treatment | 1° Rx. | Dur (d) | Results | 2° Rx. | Dur (d) | Results | 3° Rx. | Dur (wk) | Outcome | Immobilization | FU (wk) | Final results |
| 1 | 1, 1 | 8 | F | Fell backwards while walking | 3 wk initial, referred after 6 mo | 3, 5 | 5 | 14 | 3 | 6 | 1 | PH × 6 wk, SC × 1 wk | 108 | 1 | ||||
| 2 | 1, 3 | 8 | F | Shaking water from ear | 4 wk | 3, PT | 4 | 7 | 3 | 4 | 10 | 3 | 5 | 3 | 1 | PH × 3 mo | 150 | 1 |
| 3 | 2, 4 | 7 | M | Goldenhar syndrome, ear reconstruction | 7 d | None | 4 | 8 | 1 | - | - | - | - | - | - | PH × 4 wk | NR | 1 |
| 4 | 2 | 6 | F | Crouzon syndrome, midfacial advancement | None | None | 4 | 10 | 1 | - | - | - | - | - | - | PH × 4 wk | 2 | 1 |
| 5 | 2 | 10 | F | Pharyngitis | 7 d | None | 4 | 14 | 1 | - | - | - | - | - | - | PH × 2 mo | 6 | 1 |
| 6 | 2 | 7 | M | Awakened with stiff neck | 10 d | None | 4 | 3 | 2 | 4 | 4 | 2 | - | - | - | None | 2 | 1 |
| 7 | 2, 4 | 13 | F | ADN | 7 d | None | 4 | 7 | 1 | - | - | - | - | - | - | HC × 6 wk | 2 | 1 |
| 8 | 2, 5 | 7 | M | Tonsillectomy/ADN, Klippel-Feil | 5 d | None | 4 | 7 | 1 | - | - | - | - | - | - | SC | 2 | 1 |
| 9 | 2 | 8 | F | Tonsillectomy/ADN | 4 d | None | 1 | 10 | 2 | NR | 2 | NR | NR | NR | SC | 1.5 | 1 | |
| 10 | 5, 2 | 5 | M | Golderhar Syndrome, Hemifacial microsomia. 2 episodes S/P mandibular reconstruction and zygoma and mandible reconstruction | 4 d | None | 4, 4 | 4, 5 | 1 | - | - | - | - | - | - | PH × 4 wk, HC × 3 wk | 1 | |
| 11 | 5, 5, 2 | 9 | M | Neck pain | Unknown | None | 4 | 5 | 3 | - | - | - | - | - | - | PH × 3 wk | 18 | 3 |
| 12 | 4 | 6 | M | Unknown | Unknown | None | 1 | - | - | - | - | - | - | - | - | - | - | No Ortho |
| 13 | 4 | 5 | M | Unknown | 4-5 mo | None | Outpatient consult | - | - | - | - | - | - | - | - | None | NA | 1 |
| 14 | 4 | 6 | F | Scarlet fever | 6 wk | 6 wk of oral antibiotics | Outpatient consult | - | - | - | - | - | - | - | - | - | NA | 1 |
| 15 | 4 | 6 | M | Unknown | ER | None | 1 | - | - | - | - | - | - | - | - | - | - | No Ortho |
| 16 | 4 | 8 | M | Unknown | ER | None | 3 | - | - | - | - | - | - | - | - | PH × 8 wk | - | No Ortho |
| 17 | 4 | 9 | M | All terrain vehicle injury, occipital condyle fracture | None | None | 1 | - | - | - | - | - | - | - | - | 20 | 1 | |
| 18 | 4 | 6 | F | Cervical lymphadenitis | None | 2 | 4 | - | - | - | - | - | - | - | - | HC × 1 wk | 1 | 1 |
| 19 | 4 | 5 | F | Congenital muscular torticolis | 1 mo | Torticolis sx at 1.5 yr of age | Bipolar Release | - | 1 | - | - | - | - | - | - | - | - | - |
| 20 | 4, 4 | 12 | F | Retropharyngeal abscess | 3-4 d | None | 4 | 10 | 1 | - | - | - | - | - | - | SC × 2 wk | 3 | 1 |
| 21 | 4 | 6 | M | Throwing ball | 2 wk | 4 | 4 | 14 | 2 | - | 7 | 2 | 2 | Persistent | 1 | 1 | ||
| 22 | 4 | 9 | F | Unknown | None | None | PT | -03/ 17/ 003 | - | - | - | PT | Recurrence | 18 | - | |||
| 23 | 4 | 7 | F | Choanal Atresia repair, ADN | 2 d | 2 | 1 | 2 | 2 | 4 | - | - | - | - | - | CTO × 6 wk | 9 | 1 |
| 24 | 4 | 8 | Wrestling | None | None | 3 | - | - | - | - | - | - | - | HC | - | No FU | ||
| 25 | 4 | 10 | M | ADN | None | None | 3 | . | - | - | - | - | - | - | - | - | - | |
| 26 | 4, 4 | 8 | F | Minor trauma doing handstand | None | None | 4 | 5 | 1 | - | - | - | - | - | - | - | 18 | 1 |
| 27 | 4, 4 | 4 | F | None | NA | None | 3 PT | 2 | 1 | - | - | - | - | - | - | SC × 2 wk | 2 | 1 |
| 28 | 5 | 12 | F | Turning head during sleep | 1 d | None | 3 | - | - | - | - | - | - | - | - | - | - | No FU |
| 29 | 5 | 14 | F | Down syndrome | None | None | 4 | 10 | 2 | - | - | - | - | - | - | PH × 6 wk/SC, PT | 8 | 1 |
| 30 | 5 | 6 | F | ADN | 3-4 d | None | 4 | 2 | 1 | - | - | - | - | - | - | SC × 3 wk, PT | 8 | 1 |
| 31 | 5 | 5 | F | Pharyngitis | 3-4 d | None | 3 | - | 1 | - | - | - | - | - | - | SC × 2 wk | 8 | 1 |
| 32 | 5 | 7 | M | Lymphadenitis | 4 wk | PT | 4 | 7 | 1 | - | - | - | - | - | - | HC × 6 wk | 20 | 1 |
| 33 | 5 | 6 | ADN | None | None | 4 | 3 | 1 | - | - | - | - | - | - | HC × 6 wk, PT | 6 | 1 | |
| 34 | 5 | 6 | F | Serving tennis | 4 wk | None | 3 | 10 | 1 | - | - | - | - | - | - | - | 1.5 | No FU |
| 35 | 5 | 9 | M | URI | 2 d | None | 4 | 7 | 3 | 4 | 3 | 1 | - | - | - | PH × 8 wk | 10 | 1 |
Two patients were classified as having type 1 dynamics, or a true fixed rotatory subluxation. The first presented after 6 mo of previous treatment with skin traction, skeletal traction and bracing. Reduction was achieved with skeletal traction, but could not be maintained, and a C1-C2 arthrodesis was required. The second patient presented one month after the onset of symptoms and failed two courses of skin traction and bracing, during which her dynamics had improved from type I to type III. She was then treated by skeletal traction, and ultimately reduced and was managed in a pinless halo for 3 mo. She remains asymptomatic at more than 3 years follow-up.
Nine patients had type II (8) or type III (1) dynamics, five of whom were scanned more than once. Six were admitted for soft cervical traction (4-14 d) and then immobilized in a soft collar, hard collar, or pinless halo for an additional 2-8 wk. Two were managed with a soft collar and oral medications. While follow-up was limited, resolution was observed in eight patients. A single patient had persistent and intermittent symptoms, and initially had two studies that were in the diagnostic grey zone, and the third had demonstrated progression to a type II rotatory subluxation.
Sixteen patients exhibited normal dynamics (type 4, muscular torticollis). Four were never evaluated by orthopaedics, and two were seen once for an outpatient consultation. All but one of the remaining patients had clinically resolved at one to twenty weeks follow-up. Four patients were admitted for soft cervical traction, and seven were managed by nonsteroidal anti-inflammatory medications with or without a soft or hard cervical collar, or by physical therapy. A single patient with a history of congenital muscular torticollis and an acute episode of pain was treated by a bipolar sternocleidomastoid release once symptoms had abated.
Eight patients fell within the diagnostic grey zone (type 5). Five patients were effectively treated by soft cervical traction (2-10 d), with no relapse at two to twenty weeks follow-up. Of three patients treated by a soft collar and analgesics, one had resolved at 8 wk follow-up and records could not be obtained for the other two. Due to behavioral issues, a single patient with Down syndrome could not be imaged at presentation, and could not be maintained in halter traction despite oral sedation and analgesics. The decision was made to perform a dynamic rotational CT scan under anesthesia using the O-arm, and the diagnosis was muscular torticollis. The torticollis resolved with immobilization and physical therapy, and has not recurred at more than 2 years follow-up.
The terms atlanto-axial rotatory displacement (AARD), subluxation (AARS), and fixation (AARF) have all been used to describe a spectrum of rotational abnormalities of the atlanto-axial joint observed in the absence of major trauma[1-12]. Associated conditions include minor trauma[1,15], inflammatory disorders (Grisel syndrome)[3,16,17], or surgical procedures on the head or neck[6,7,17-20]. Predisposing factors may include anatomic features (horizontal facet orientation, facets shaped like biconvex discs, joint hypermobility), mechanical loading (intraoperative positioning, loss of normal muscle tone during general anesthesia), and physiologic factors (hyperemia from infection or inflammation) associated with increased mobility. Anatomic barriers to achieving reduction include inflamed synovial and/or capsular tissues[1,2,10] or abnormalities of a meniscus like synovial fold at the periphery of the joint (inflammation, rupture, in-folding)[21]. Pathologic findings identified in chronic cases include contracture of periarticular soft tissues, interposition of fibrous tissue, osseous cross union, and adaptive changes in facet morphology[1,7,15,22-24]. A timely diagnosis is critical, and the results following treatment are less predictable when the condition presents at a subacute (> 1 mo) or chronic stage[1,7], recurs, or presents with a fixed subluxation between C1 and C2[7].
Normal cervical rotation is approximately 70°-80° to each side in both children and adults[13,14], and the maximum divergence between C1 and C2 during normal rotation to either side ranges from 29° to 45°[5,13,25,26]. As a loss of contact between the C1 and C2 facets of up to 85% occurs at the extremes of physiologic rotation, subluxation is a normal finding during rotation[13,14]. This has led to the use of a dynamic CT scan as a diagnostic modality[5-7,9,26-28], although diagnostic criteria have yet to be established. Important concerns include how C1 and C2 move relative to one another throughout the arc of rotation (C1-C2 angle or angle of separation) and whether C1 crosses over C2. Mönckeberg et al[14] suggested that an angle of separation of less than 36° coupled with facet uncoverage of less than 60% were sufficient for a diagnosis. McGuire et al[27] recognized that both the separation angle and crossover of C1 were important, and attempted to classify patients as follows: I (normal), II (< 15° of separation between C1 and C2, C1 crosses over C2), and III (C1-C2 angle is fixed or C1 does not cross over C2). In contrast, several studies have questioned the value of dynamic CT scans. Hicazi et al[28] found no significant difference between the presenting and corrected sides in atlantoaxial rotation, the atlanto-dens interval, or the center of rotation. Alanay et al[29] found that both the intra-observer and inter-observer reliability were poor.
Pang and Li have developed a classification scheme relative to normative data, encompassing a spectrum from AARF (type I), through “pathologic stickiness” (types 2 and 3), and finally to muscular torticollis (type 4)[5-7]. They also defined a diagnostic grey zone in which dynamics may presumably return to normal or progress to one of the more severe forms of the condition. Recognizing the limitations of this retrospective review, our impression is that the classification adequately describes the spectrum of pathology, although it is clear that there was discordance with the radiologist’s interpretation in many cases.
Several technical points are worth mentioning. Care should be taken to ensure that the patient’s shoulders remain flat in the scanner to avoid a false positive result (rotation occurs through trunk rather than cervical spine). It is also prudent to remove the metal arc from the head frame, as this may restrict the active or passive range of cervical rotation. As rotation may also be limited by pain or muscle spasm, some have suggested that the study be performed under sedation, or even general anaesthesia[11,14]. While the 3 data points required to construct a line for the graph can be obtained even with a relatively limited arc of motion, it is possible for example that with greater rotation towards the corrected side, that a patient with type II dynamics could achieve cross over and be classified as type III.
Only 26% of studies in our series fell within the pathologic spectrum (types I-III), including just two cases of fixed rotatory subluxation, calling into question the indications for obtaining a dynamic CT scan. A number of these were obtained in the emergency room prior to orthopaedic consultation. Recognizing that an early diagnosis improves outcomes, consideration could be given to empiric treatment for patients presenting within several days of symptom onset with characteristic signs and symptoms of atlanto-axial rotatory pathology, reserving the dynamic CT scan for those failing initial management and/or those presenting in a delayed fashion. Although detailed follow-up information was mainly available for those patients with a greater severity of involvement, the majority of patients resolved with non-operative treatment measures. The two patients with a fixed rotatory subluxation had a protracted course, one of whom presented after 6 mo of previous treatment and ultimately required an arthrodesis. The second responded after three courses of traction and 3 mo of additional immobilization in a pinless halo. For patients with type II or type III dynamics, all but one resolved with treatment. One patient has relapsed on two occasions but has responded to symptomatic treatment, however the long-term prognosis remains uncertain. We found that all but two patients with normal dynamics or who were classified as being in the diagnostic grey zone resolved clinically, and records were unavailable for the other two. These clinical observations are consistent with a majority of studies[8,16,18,20,27-31].
There are several limitations of this study to be discussed, including the fact that the intra and inter-observer reliability of this scheme has not been reported. We attempted to minimize variations by having each study graded by three examiners, who then reviewed each study together prior to assigning a final class. From a technical standpoint, our scans were obtained in neutral and maximal voluntary rotation to the right and left, in contrast to Pang and Li who obtain their studies at the position of comfort (rotated to right or left), neutral, and toward the opposite or corrected side. Our angle of rotation towards the presenting side might be slightly greater than their “presenting” position, altering one data point on the graph. While our angle of divergence might be slightly greater for the “presenting” side, this should have minimal if any impact on classification. Our follow-up period was limited for all but the most severe cases, and we cannot provide a detailed quantitative assessment of cervical range of motion or of clinical outcomes. Our impression supports previous studies in suggesting that the vast majority of cases resolve without chronic residua. We have not routinely obtained dynamic CT scans after clinical resolution, and cannot prove that normal dynamics were restored in patients who resolved clinically. Persistent abnormalities in rotatory dynamics may be compensated for by an increase in motion at the occiput-C1 articulation or through the subaxial spine.
Atlantoaxial rotatory displacement represents a spectrum of rotational malalignment between C1 and C2, and Pang and Li have described a classification scheme which explains this spectrum, based on dynamic computed tomography (CT) imaging. The authors classified a group of patients presenting with painful torticollis according to Pang and Li and compared findings with the interpretation by the authors’ radiologists and with each patient’s clinical course.
There is limited information in the literature on atlantoaxial rotatory displacement, and a variety of terms have been utilized to describe the condition, suggesting that there is a need for a common language to describe the pathology.
There are few studies concerning the Pang and Li classification, and while this classification is able to capture a spectrum of pathology, it has not achieved wide clinical use to our knowledge. The authors sought to determine whether the Pang and Li class correlated with our radiologist’s interpretation of dynamic rotational CT scans.
The Pang and Li classification has practical applications and may be used by the clinician to characterize the findings on a dynamic CT scan. The findings allow the clinician to be more specific in articulating the nature of the pathology.
Atlantoaxial rotatory displacement: Abnormal relationship between C1 and C2 in the axial plane in which there may or may not be mobility between the two segments; Atlantoaxial rotatory subluxation: abnormal relationship between C1 and C2 in the axial plane in which there is mobility between the two vertebrae; Atlantoaxial rotatory fixation: fixed abnormal relationship between C1 and C2 in the axial plane.
The current study focused on an original issue. It is well-organized.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cartmell S, Erkan S, Peng BG, Rothschild BM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am. 1977;59:37-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 493] [Cited by in F6Publishing: 379] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 2. | Coutts MB. Atlanto-epistropheal subluxations. Arch Surg. 1934;29:297-311. [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 75] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Grisel P. Enucleation de l’atlas et torticolis nasopharyngien. Presse Med. 1930;38:50-53. [Cited in This Article: ] |
| 4. | Jones RW. Spontaneous Hyperæmic Dislocation of the Atlas. Proc R Soc Med. 1932;25:586-590. [PubMed] [Cited in This Article: ] |
| 5. | Pang D, Li V. Atlantoaxial rotatory fixation: Part 1--Biomechanics of normal rotation at the atlantoaxial joint in children. Neurosurgery. 2004;55:614-625; discussion 625-626. [PubMed] [Cited in This Article: ] |
| 6. | Pang D, Li V. Atlantoaxial rotatory fixation: part 2--new diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging. Neurosurgery. 2005;57:941-953. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Pang D, Li V. Atlantoaxial rotatory fixation: part 3-a prospective study of the clinical manifestation, diagnosis, management, and outcome of children with alantoaxial rotatory fixation. Neurosurgery. 2005;57:954-972. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 8. | Phillips WA, Hensinger RN. The management of rotatory atlanto-axial subluxation in children. J Bone Joint Surg Am. 1989;71:664-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 160] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Rinaldi I, Mullins WJ, Delaney WF, Fitzer PM, Tornberg DN. Computerized tomographic demonstration of rotational atlanto-axial fixation. Case report. J Neurosurg. 1979;50:115-119. [PubMed] [Cited in This Article: ] |
| 10. | Wortzman G, Dewar FP. Rotary fixation of the atlantoaxial joint: Rotational atlantoaxial subluxation. Radiology. 1968;90:479-487. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 109] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Been HD, Kerkhoffs GM, Maas M. Suspected atlantoaxial rotatory fixation-subluxation: the value of multidetector computed tomography scanning under general anesthesia. Spine (Phila Pa 1976). 2007;32:E163-E167. [PubMed] [Cited in This Article: ] |
| 12. | Crockard HA, Rogers MA. Open reduction of traumatic atlanto-axial rotatory dislocation with use of the extreme lateral approach. A report of two cases. J Bone Joint Surg Am. 1996;78:431-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 61] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Villas C, Arriagada C, Zubieta JL. Preliminary CT study of C1-C2 rotational mobility in normal subjects. Eur Spine J. 1999;8:223-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Mönckeberg JE, Tomé CV, Matías A, Alonso A, Vásquez J, Zubieta JL. CT scan study of atlantoaxial rotatory mobility in asymptomatic adult subjects: a basis for better understanding C1-C2 rotatory fixation and subluxation. Spine (Phila Pa 1976). 2009;34:1292-1295. [PubMed] [Cited in This Article: ] |
| 15. | Govender S, Kumar KP. Staged reduction and stabilisation in chronic atlantoaxial rotatory fixation. J Bone Joint Surg Br. 2002;84:727-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 112] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 16. | Fernández Cornejo VJ, Martínez-Lage JF, Piqueras C, Gelabert A, Poza M. Inflammatory atlanto-axial subluxation (Grisel’s syndrome) in children: clinical diagnosis and management. Childs Nerv Syst. 2003;19:342-347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 47] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Yu KK, White DR, Weissler MC, Pillsbury HC. Nontraumatic atlantoaxial subluxation (Grisel syndrome): a rare complication of otolaryngological procedures. Laryngoscope. 2003;113:1047-1049. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Karkos PD, Benton J, Leong SC, Mushi E, Sivaji N, Assimakopoulos DA. Grisel’s syndrome in otolaryngology: a systematic review. Int J Pediatr Otorhinolaryngol. 2007;71:1823-1827. [PubMed] [Cited in This Article: ] |
| 19. | Leong SC, Karkos PD, Papouliakos SM, Apostolidou MT. Unusual complications of tonsillectomy: a systematic review. Am J Otolaryngol. 2007;28:419-422. [PubMed] [Cited in This Article: ] |
| 20. | Subach BR, McLaughlin MR, Albright AL, Pollack IF. Current management of pediatric atlantoaxial rotatory subluxation. Spine (Phila Pa 1976). 1998;23:2174-2179. [PubMed] [Cited in This Article: ] |
| 21. | Kawabe N, Hirotani H, Tanaka O. Pathomechanism of atlantoaxial rotatory fixation in children. J Pediatr Orthop. 1989;9:569-574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 74] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Ishii K, Chiba K, Maruiwa H, Nakamura M, Matsumoto M, Toyama Y. Pathognomonic radiological signs for predicting prognosis in patients with chronic atlantoaxial rotatory fixation. J Neurosurg Spine. 2006;5:385-391. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Crossman JE, Thompson D, Hayward RD, Ransford AO, Crockard HA. Recurrent atlantoaxial rotatory fixation in children: a rare complication of a rare condition. Report of four cases. J Neurosurg. 2004;100:307-311. [PubMed] [Cited in This Article: ] |
| 24. | Crossman JE, David K, Hayward R, Crockard HA. Open reduction of pediatric atlantoaxial rotatory fixation: long-term outcome study with functional measurements. J Neurosurg. 2004;100:235-240. [PubMed] [Cited in This Article: ] |
| 25. | Dvorak J, Panjabi M, Gerber M, Wichmann W. CT-functional diagnostics of the rotatory instability of upper cervical spine. 1. An experimental study on cadavers. Spine (Phila Pa 1976). 1987;12:197-205. [PubMed] [Cited in This Article: ] |
| 26. | Kowalski HM, Cohen WA, Cooper P, Wisoff JH. Pitfalls in the CT diagnosis of atlantoaxial rotary subluxation. AJR Am J Roentgenol. 1987;149:595-600. [PubMed] [Cited in This Article: ] |
| 27. | McGuire KJ, Silber J, Flynn JM, Levine M, Dormans JP. Torticollis in children: can dynamic computed tomography help determine severity and treatment. J Pediatr Orthop. 2002;22:766-770. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Hicazi A, Acaroglu E, Alanay A, Yazici M, Surat A. Atlantoaxial rotatory fixation-subluxation revisited: a computed tomographic analysis of acute torticollis in pediatric patients. Spine (Phila Pa 1976). 2002;27:2771-2775. [PubMed] [Cited in This Article: ] |
| 29. | Alanay A, Hicazi A, Acaroglu E, Yazici M, Aksoy C, Cila A, Akalan N, Surat A. Reliability and necessity of dynamic computerized tomography in diagnosis of atlantoaxial rotatory subluxation. J Pediatr Orthop. 2002;22:763-765. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Mihara H, Onari K, Hachiya M, Toguchi A, Yamada K. Follow-up study of conservative treatment for atlantoaxial rotatory displacement. J Spinal Disord. 2001;14:494-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Burkus JK, Deponte RJ. Chronic atlantoaxial rotatory fixation correction by cervical traction, manipulation, and bracing. J Pediatr Orthop. 1986;6:631-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 0.9] [Reference Citation Analysis (0)] |