Published online Jul 18, 2016. doi: 10.5312/wjo.v7.i7.442
Peer-review started: March 4, 2016
First decision: April 15, 2016
Revised: April 22, 2016
Accepted: May 10, 2016
Article in press: May 11, 2016
Published online: July 18, 2016
AIM: To evaluate the results of hip reconstruction with extensive excision for tumor confined to the femoral head and neck.
METHODS: We designed a resection preserving the greater trochanter and lower portion of calcar femorale, and utilized conventional total hip prosthesis. We retrospectively reviewed 7 patients, who underwent a wide resection and reconstruction using conventional hip prosthesis. There were 3 men and 4 women and their mean age was 42.5 years (22 to 65 years). The histologic diagnosis of each patient was low-grade osteosarcoma, diffuse large B-cell lymphoma, liposclerosing myxofibroma, intraosseous lipoma, chondroblastoma, giant cell tumor and focal intramedullary fibrosis.
RESULTS: One patient with lymphoma died due to disease dissemination at 10 mo postoperatively and the remaining 6 patients were followed for a mean of 4.7 years (3 to 6 years). All patients were able to return to their daily activities and no patient had local recurrence. No radiographic signs of loosening, wear, and osteolysis were found at the last follow-up.
CONCLUSION: Trochanter/calcar-preserving resection of the proximal femur and reconstruction using conventional total hip prosthesis, is a satisfactory treatment for tumors confined to the femoral head and neck.
Core tip: This is a retrospective study to evaluate the results of trochanter and calcar preserving reconstruction in tumors involving the femoral head and neck. While usual osteotomy for primary total hip arthroplasty is made straightly at 0.5 inch above the lesser trochanter, we made a curved osteotomy in coronal plane from the tip of greater trochanter to lower level or below the lesser trochanter to remove the tumor lesion confined to femoral head and neck. This technique can preserve the greater trochanter and lower portion of the calcar femorale. This surgical technique is a satisfactory treatment for tumors confined to the femoral head and neck.
- Citation: Cho HS, Lee YK, Ha YC, Koo KH. Trochanter/calcar preserving reconstruction in tumors involving the femoral head and neck. World J Orthop 2016; 7(7): 442-447
- URL: https://www.wjgnet.com/2218-5836/full/v7/i7/442.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i7.442
The proximal femur is a common site of primary malignant bone tumors, including chondrosarcoma, Ewing’s sarcoma and osteosarcoma[1]. An array of benign bone tumors; giant cell tumor, chondroblastoma, and clear cell chondrosarcoma may develop at the proximal femoral epiphysis and extend to the metaphysis[2-4]. Intra-articular involvement is rare in these tumors, although they might occur following a pathologic fracture.
Patients with tumors confined to the femoral head have been candidates for curettage-bone graft[5] or an extensive resection of the proximal femur and reconstruction, usually hemiarthroplasty, using tumor prosthesis depending on the biologic aggressiveness of the tumor[6-8].
In the process of resection and reconstruction, the greater trochanter is osteomized or excised and after then, the greater trochanter or the insertion of the abductor muscle is attached to the tumor prosthesis with wires or cable grip, which can induce complications including wire or cable breakage, trochanteric fragment migration, nonunion, bursitis, and metallosis[9-12].
Tumor prosthesis is highly costive. One more drawback of the tumor prosthesis is the difficulty on determining the actual length and width of the resected bone even with a use of modular endoprosthesis[13]. Intermediate to long term survivorship of bipolar tumor prosthesis is not satisfactory compared to conventional total hip arthroplasty[7,8,14].
Since 2007, we have treated tumors involving femoral head and neck using a trochanter/calcar-preserving resection and conventional total hip prosthesis. In this study, we present the operative technique and evaluate the results after trochanter-preserving resection with use of conventional prosthesis.
The surgical treatment algorithm of tumors of the femoral head and neck at our department is as follows. The primary treatment for histologically-proven benign bone tumors confined to the femoral head and neck is curettage and bone graft[5]. However: (1) when there is a suspicion of malignancy or solitary bone metastasis; (2) when there is a risk of superior retinacular or lateral epiphyseal arterial damage during the curettage and consequent develop of osteonecrosis; (3) when the lesion is large and located at the subchondral portion of the femoral head apex and consequent collapse is expected after the curettage; and (4) when there is a local recurrence after the curettage, we perform a trochanter/calcar-preserving resection of the proximal femur and reconstruction using conventional hip prostheses.
Tumors with a pathologic fracture, an involvement of the greater trochanter, involvement of the lesser trochanter, cortical penetration, or intra-articular involvement are treated with more extensive resection and reconstruction using revision prosthesis or tumor-prosthesis.
Between June 2007 and December 2011, 20 patients were operated due to tumors of the femoral head and neck at the authors’ hospital. Among them, 13 patients were treated with curettage with bone graft (11 patients) or cement filling (2 patients). The remaining seven patients, who were operated with a trochanter-preserving resection of the proximal femur and total hip arthroplasty using conventional prosthesis, were subjects of this study.
There were 3 men (3 hips) and 4 women (4 hips), and the mean age at the time of operation was 42.5 years (range, 22 to 65 years). All patients presented with a pain of affected hip. The mean time interval between the onset of hip pain and the index operation was 13.6 mo (range, 1.3 to 48.1 mo).
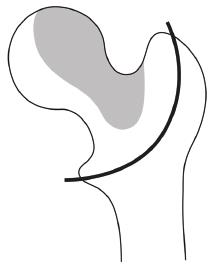
We made preoperative diagnoses and evaluated the tumor extent on plain radiographs, computed tomography and/or magnetic resonance image. We planned a wide resection (≥ 1 cm from the tumor margin) bearing in mind the possibility of the malignant tumor (Figure 1).
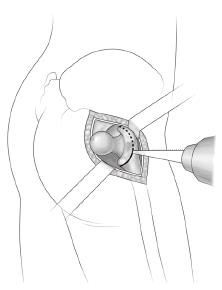
All THAs were carried out by one surgeon. The patient was placed in a lateral position on the operating room table. A longitudinal posterolateral incision was made. Trochanteric bursa and underlying fat tissues were removed to expose short external rotators and sciatic nerve. External rotators were cut at their tendinous attachments to the trochanteric crest and the posterior capsule of the hip joint was incised. The femoral head was dislocated posteriorly.
To remove the diseased femoral head and neck, preserving the greater trochanter and lower portion of the calcar femorale, we made a curved osteotomy in coronal plane from the tip of greater trochanter to lower level or below the lesser trochanter according to the tumor margin while usual osteotomy for primary total hip arthroplasty is made straightly at 0.5 inch above lesser trochanter. The posterior cortex and endo-osteal cancellous bone was cut using a 7 mm width osteotome and the anterior cortex was cut with use of a reciprocating saw (Figure 2). This osteotomy is similar to curved varus osteotomy, which has been use for the surgical treatment of femoral head osteonecrosis[15].
After the planned intertrochanteric osteotomy, attachments of vastus muscles and the anterior capsule were detached from the intertrchanteric line of proximal segment to remove the proximal segment. And attachment of psoas was partially detached from the lesser trochanter.
On the inspection of the resected segment, no tumor showed a penetration into the joint or cortical invasion. Resected specimens were submitted for pathological evaluation.
The rest of the procedure was performed in the ordinary manner of cementless THA.
Three designs of implants were used; PINNACLE cup with Corail stem (DePuy, Saint-Priest, France) in 4 hips, PLASMACUP® SC acetabular component with BiCONTACT® stem (Aesculap, Tuttlingen, Germany) in 2 hips, and Bencox cup with Bencox stem (Corentec, Seoul, South Korea) in 1 hip. Third-generation ceramic articulation (BIOLOX Forte alumina head and liner; CeramTec, Plochingen, Germany) was used in 2 hips, and fourth-generation (BIOLOX Delta alumina head and liner; CeramTec) in 5 hips. The diameter of the femoral head was 28 mm in 1 hip, 32 mm in 5 hips, and 36 mm in 1 hip.
The final diagnoses by histological examination were low-grade osteosarcoma, diffuse large B-cell lymphoma, liposclerosing myxofibroma, intraosseous lipoma, chondroblastoma, giant cell tumor, and focal intramedullary fibrosis (Table 1). Surgical margins were negative for the tumor in all patients.
| Patient | Sex/age | Initial diagnosis on MRI | Final histologic diagnosis | Follow-up (yr) | ISOLS score |
| 1 | F/36 | Giant cell tumor | Liposclerosing myxofibroma | 6 | 30 |
| 2 | F/38 | Low-grade osteosarcoma | Low-grade osteosarcoma | 6 | 29 |
| 3 | F/64 | Clear cell chondrosarcoma | Intraosseous lipoma | 5 | 28 |
| 4 | M/22 | Chondroblastoma | Chondroblastoma | 5 | 30 |
| 5 | M/33 | Giant cell tumor | Giant cell tumor | 3 | 30 |
| 6 | F/60 | Breast cancer metastasis | Focal intramedullary fibrosis | 3 | 28 |
| 7 | M/41 | Aneurysmal bone cyst | Lymphoma | Died at 10 mo |
Two patients with malignant tumors underwent a computed tomographic scan of the chest and whole body bone scan, which revealed no evidences of distant metastasis. The patient with lymphoma was treated with adjuvant chemotherapy. Patients were instructed to walk with partial weight bearing with the aid of two crutches for four weeks after surgery.
Routine follow-up visits were scheduled for six weeks, three, six, nine, twelve months, and six months thereafter. Patients who had not returned for regularly scheduled visits were contacted by telephone.
Clinical evaluation was performed with use of the Harris hip score (HHS)[16], and the functional classification system of the International Society of Limb Salvage (ISOLS), which includes six functional parameters; pain, function, emotional acceptance, use of walking supports, walking ability, and gait. Each parameter is scored from 0 to 5 (a maximum score of 30)[17].
The radiographic evaluation was done to confirm if there was the evidence of recurrence; a newly discovered osteolytic or osteosclerotic lesion on follow-up radiographs or MRI.
Fixations of the acetabular and femoral components[18,19], ceramic wear[20] and osteolysis[21-23] were assessed on serial radiographs.
The design and protocol of this retrospective study were approved by the institutional review board in our hospital, which waived the informed consents.
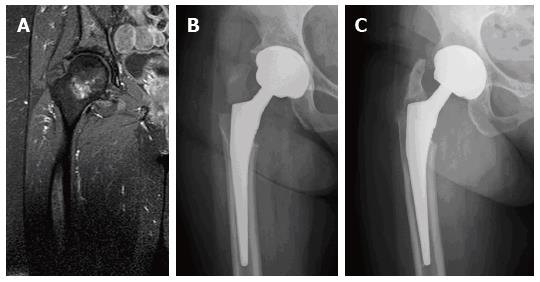
Fracture of the greater trochanter occurred in one patient who was operated due to intraosseous lipoma. The fracture was detected on postoperative 6 wk radiographs. In this patient, the inner portion of the greater trochanter had been removed during the operation to achieve a wide resection and only a thin cortical portion had been left. This patient had no history of trauma, and had little pain postoperatively. Thus, the fracture seemed to be an avulsion fracture. It healed completely with protected weight-bearing for 3 mo and an osseointegration of the prosthesis was achieved (Figure 3).
One patient with lymphoma recovered well and returned to his normal activity after the operation. The postoperative radiographs at 6 mo were uneventful. However, this patient died because of disseminated disease at the 10 mo postoperative.
The remaining 6 patients were followed-up for an average of 4.7 years (3 to 6 years). All patients returned to their daily activities and were walking with full weight bearing. At the last follow-up, the mean HHS was 98.0 points (range 96-100 points), and the mean ISOLS functional score was 29.2 points (range 28-30 points) (Table 1). During the follow-up there was no evidence of local recurrence. At the latest follow-up, there were no radiographic signs of aseptic loosening, wear, or osteolysis (Figure 4).
The proximal femur is a common site for primary bone tumors and the most common site of metastatic tumors. Since the introduction of tumor prosthesis in 1980s, tumors in the femoral head and neck have been treated with extensive resection and reconstruction of the proximal femur. The femur is resected below the lesser trochanter and the greater trochanter is resected or osteomized. The reconstruction is consisted of a hemiarthroplasty with use of an endoprosthesis. Although modular system improved the endoprostheic reconstruction[14], there are several drawbacks in this procedure. The greater trochanter is osteotomized or the abductors are transected through their tendinous attachments. If the greater trochanter is resected en-bloc, the remaining abductors are attached to the prosthesis. If a fragment of the greater trochanter is remains, it is fixed to the prosthesis with a cable grip system.
However, problems have appeared after the use of cable grip. Silverton et al[24] reviewed 68 trochanteric osteotomies, which were repaired with Dall-Miles cable grip system (Howmedica, Rutherford, NJ). Trochanteric nonunion occurred in 25%, with fraying and fragmentation of the cable. Among the 51 patients with trochanteric union, 35% also had signs of fraying and fragmentation. Osteolysis around the cable was seen in 10%. Metallosis at the inferior border of the acetabulum were seen in 12%[24].
As the life expectancy of patients with bone tumors improves, endoprosthetic replacement of the proximal femur is not durable in young patients with low-grade tumor (IA/IB or benign)[7]. Bernthal et al[7] reviewed 86 proximal femoral replacements used for tumor reconstruction. Their study included 43 high-grade tumors (IIA/IIB), 20 low-grade tumors (IA/IB or benign), and 23 with metastatic disease. The 5-, 10-, and 20-year survival for IIA/IIB patients was 54%, 50%, and 44%, respectively; all patients with low-grade disease survived; the 5-year survival rate for patients with metastatic disease was 16%. The 5-, 10- and 20-year implant survivorships were 93%, 84%, and 56%, respectively. Although bipolar proximal femoral reconstruction proved a durable technique in patients with metastatic disease and high-grade disease, patients with low-grade disease outlived their implants[7]. In this study, there was a suspicious solitary bone metastasis (patient 6), which was confirmed intramedullary fibrosis. Solitary bone metastasis is defined as a single skeletal metastasis with no tumor in any other part of the body including the primary cancer site or with a primary lesion in resectable status. Although there has been some debate on whether curative resection for a solitary bone metastasis leads to survival gain, most authors believed that patients with a solitary bone metastasis from several cancers live longer than those with multiple metastasis regardless of treatment modalities. Jung et al[25] reported that patients who had wide resection for a solitary bone metastasis had a disease-specific survival rate of 100% at mean follow-up of 69 mo. Therefore, they suggested that patients with solitary bone lesion are candidates for aggressive surgical treatment with curative intent. In addition, durable reconstruction is needed to avoid revision surgery which may complicate future management for cancer.
Our study showed that trochanter/calcar preserving resection allows adequate surgical margins for tumors in femoral head and neck and reconstruction using conventional total hip prosthesis affords a satisfactory functional outcome without local recurrence or prosthetic loosening.
There were several limitations in our study. Our study was a retrospective review performed in a small number of cases. There was no control group of wide resection of the proximal femur and reconstruction using endo-prosthesis. However, the mean HHS (98 points) was satisfactory at last follow-up, which was comparable with that of primary THA[26]. Our procedure is applicable on the condition that the lesion was confined to the femoral head and neck. Therefore, a careful evaluation of tumor extent using MRI is mandatory preoperatively.
Our results of trochanter/calcar preserving resection and reconstruction using conventional total hip prosthesis were satisfactory. We would recommend this procedure as a primary surgical treatment along with curettage and bone graft for tumors confined to the femoral head and neck, especially in young patients.
Tumors confined to the femoral head have been treated by curettage-bone graft or tumor prosthesis following an extensive resection of the proximal femur according to the suspected pathology. When using tumor prosthesis with high cost, an extensive resection of the proximal femur leads to sacrifice of the greater trochanter or the insertion of the abductor muscle. In this study, the authors presented a trochanter/calcar-preserving resection and conventional total hip prosthesis in tumors involving femoral head and neck, and evaluated the outcomes.
This study contributes to presenting the surgical technique of total hip arthroplasty following trochanter/calcar-preserving resection in the selected patients.
In this study, trochanter/calcar-preserving resection was presented for patients with tumor confined to femoral head and neck. This technique does not require a sacrifice of greater trochanter which abductor muscles are inserted. This means that patients can preserve their abductor mechanism, even though surgery of proximal femur.
This study suggests that trochanter/calcar-preserving resection is useful for treatment in patients with tumor confined to femoral head and neck.
Calcar: The dense, vertically oriented bone present in the posteroemedial region of the femoral shaft inferior to the lesser trochanter of the femur.
The effort to reduce postoperative morbidity by preserving trochanter and calcar seemed to have yielded a good result.
Manuscript source: Invited manuscript
P- Reviewer: Bicanic G, Jun Y S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Unni K. Dahlin’s bone tumors. Philadelphia, PA: Lippincott-Raven 1996; 72, 144, 250. [Cited in This Article: ] |
| 2. | Ramappa AJ, Lee FY, Tang P, Carlson JR, Gebhardt MC, Mankin HJ. Chondroblastoma of bone. J Bone Joint Surg Am. 2000;82-A:1140-1145. [PubMed] [Cited in This Article: ] |
| 3. | Springfield DS, Capanna R, Gherlinzoni F, Picci P, Campanacci M. Chondroblastoma. A review of seventy cases. J Bone Joint Surg Am. 1985;67:748-755. [PubMed] [Cited in This Article: ] |
| 4. | Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg Am. 1987;69:106-114. [PubMed] [Cited in This Article: ] |
| 5. | Cho HS, Park IH, Han I, Kang SC, Kim HS. Giant cell tumor of the femoral head and neck: result of intralesional curettage. Arch Orthop Trauma Surg. 2010;130:1329-1333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Ogilvie CM, Wunder JS, Ferguson PC, Griffin AM, Bell RS. Functional outcome of endoprosthetic proximal femoral replacement. Clin Orthop Relat Res. 2004;44-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Bernthal NM, Schwartz AJ, Oakes DA, Kabo JM, Eckardt JJ. How long do endoprosthetic reconstructions for proximal femoral tumors last? Clin Orthop Relat Res. 2010;468:2867-2874. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Finstein JL, King JJ, Fox EJ, Ogilvie CM, Lackman RD. Bipolar proximal femoral replacement prostheses for musculoskeletal neoplasms. Clin Orthop Relat Res. 2007;459:66-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Jarit GJ, Sathappan SS, Panchal A, Strauss E, Di Cesare PE. Fixation systems of greater trochanteric osteotomies: biomechanical and clinical outcomes. J Am Acad Orthop Surg. 2007;15:614-624. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Simank HG, Chatzipanagiotis C, Kaps HP. Complication rate following trochanteric osteotomy in total hip endoprosthesis. A retrospective study with failure analysis. Z Orthop Ihre Grenzgeb. 1996;134:457-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Wieser K, Zingg P, Dora C. Trochanteric osteotomy in primary and revision total hip arthroplasty: risk factors for non-union. Arch Orthop Trauma Surg. 2012;132:711-717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Glassman AH. Complications of trochanteric osteotomy. Orthop Clin North Am. 1992;23:321-333. [PubMed] [Cited in This Article: ] |
| 13. | Jeys LM, Kulkarni A, Grimer RJ, Carter SR, Tillman RM, Abudu A. Endoprosthetic reconstruction for the treatment of musculoskeletal tumors of the appendicular skeleton and pelvis. J Bone Joint Surg Am. 2008;90:1265-1271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 186] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 14. | Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Buckley L. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009;91:108-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 15. | Zhao G, Yamamoto T, Ikemura S, Motomura G, Mawatari T, Nakashima Y, Iwamoto Y. Radiological outcome analysis of transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head at a mean follow-up of 12.4 years. J Bone Joint Surg Br. 2010;92:781-786. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [PubMed] [Cited in This Article: ] |
| 17. | Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;241-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 764] [Cited by in F6Publishing: 818] [Article Influence: 26.4] [Reference Citation Analysis (1)] |
| 18. | Engh CA, Glassman AH, Suthers KE. The case for porous-coated hip implants. The femoral side. Clin Orthop Relat Res. 1990;63-81. [PubMed] [Cited in This Article: ] |
| 19. | Latimer HA, Lachiewicz PF. Porous-coated acetabular components with screw fixation. Five to ten-year results. J Bone Joint Surg Am. 1996;78:975-981. [PubMed] [Cited in This Article: ] |
| 20. | Livermore J, Ilstrup D, Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518-528. [PubMed] [Cited in This Article: ] |
| 21. | Engh CA, Hooten JP, Zettl-Schaffer KF, Ghaffarpour M, McGovern TF, Macalino GE, Zicat BA. Porous-coated total hip replacement. Clin Orthop Relat Res. 1994;89-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;20-32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 196] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;17-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 246] [Cited by in F6Publishing: 234] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 24. | Silverton CD, Jacobs JJ, Rosenberg AG, Kull L, Conley A, Galante JO. Complications of a cable grip system. J Arthroplasty. 1996;11:400-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 25. | Jung ST, Ghert MA, Harrelson JM, Scully SP. Treatment of osseous metastases in patients with renal cell carcinoma. Clin Orthop Relat Res. 2003;223-231. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 119] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010;92:1715-1719. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |