Published online Nov 18, 2016. doi: 10.5312/wjo.v7.i11.718
Peer-review started: May 19, 2016
First decision: July 5, 2016
Revised: August 26, 2016
Accepted: September 7, 2016
Article in press: September 8, 2016
Published online: November 18, 2016
Ankle fractures are accompanied by a syndesmotic injury in about 10% of operatively treated ankle fractures. Usually, the total rupture of the syndesmotic ligaments with an external rotation force is associated with a Weber type B or C fracture or a Maisonneuve fracture. The clinical assessment should consist of a comprehensive history including mechanism of injury followed by a specific physical examination. Radiographs, and if in doubt magnetic resonance imaging, are needed to ascertain the syndesmotic injury. In the case of operative treatment the method of fixation, the height and number of screws and the need for hardware removal are still under discussion. Furthermore, intraoperative assessment of the accuracy of reduction of the fibula in the incisura using fluoroscopy is difficult. A possible solution might be the assessment with intraoperative three-dimensional imaging. The aim of this article is to provide a current concepts review of the clinical presentation, diagnosis and treatment of syndesmotic injuries.
Core tip: The aim of this article is to provide a current concepts review of the clinical presentation, diagnosis and management of syndesmotic lesions. Even if syndesmotic injuries are common, the appropriate management is still under discussion. Current treatment options are discussed and future directions are provided.
- Citation: Schnetzke M, Vetter SY, Beisemann N, Swartman B, Grützner PA, Franke J. Management of syndesmotic injuries: What is the evidence? World J Orthop 2016; 7(11): 718-725
- URL: https://www.wjgnet.com/2218-5836/full/v7/i11/718.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i11.718
Ankle fractures are accompanied by a syndesmotic injury in about 10% of operatively treated ankle fractures[1-3]. Numerous mechanisms can lead to disruption of the syndesmosis complex, and the most accepted mechanism of injury is external rotation, hyperdorsiflexion and talar eversion[4-6]. This leads to sequentially tearing the anterior inferior tibiofibular ligament and the deltoid complex or causing a malleolar fracture, the interosseous ligament and finally the posterior inferior tibiofibular ligament[7-9]. In most cases, a total lesion of the syndesmotic ligaments is associated with a distal fibular fracture type Weber B or C or a proximal fibular fracture (Maisonneuve injury)[10,11].
Local swelling and tenderness are suspicious for a syndesmotic injury[12]. There are several tests available such as the external rotation test, heel thump test, dorsiflexion compression test or the squeeze test to evaluate the integrity of the syndesmosis[6]. However, in the presence of pain or swelling these tests are of limited use[13]. Clinical tests for syndesmotic lesions have a low predictive value to verify a syndesmotic injury. Several authors could show that the external rotation test might be the most sensitive test with the lowest false-positive rate[6,14].
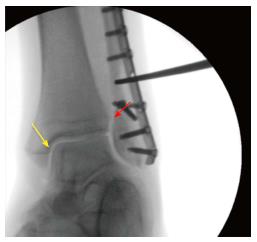
Intraoperatively, the integrity of the syndesmosis can be checked by the external rotation test or the bone hook test, which is supposed to be more reliable (Figure 1). However, these tests are also limited by a poor inter-observer reliability, which further highlights the importance of both clinical examination and imaging to diagnose an injury of the syndesmosis[13-15].
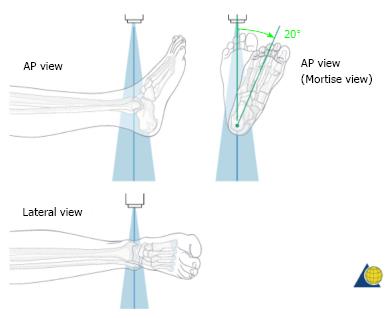
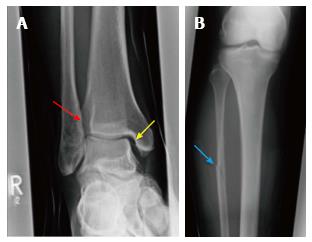
Standard radiographic examination of the ankle should consist of at least two views: Lateral view and mortise view (Figures 2 and 3). The anterior-posterior (AP) view of the ankle can be obtained as a third view, but it does not provide any additional information regarding the reduction of the mortise. In case of suspicion of a proximal fibular fracture or an injury of the syndesmosis in the clinical examination or on plain radiographs of the ankle, standard radiographs of the whole lower leg should be obtained to exclude proximal fractures/Maisonneuve injury (Figure 4)[6].
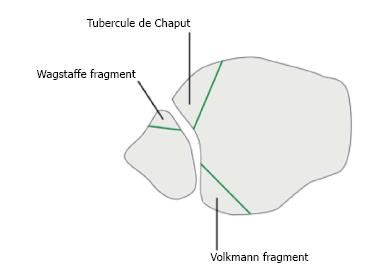
If an ankle fracture is present, the fracture pattern is most commonly described using the AO comprehensive classification system[16,17]. The plain radiographs should also be carefully checked for avulsion fractures of the anterior part of the syndesmosis, the so-called Tubercule de Chaput or Wagstaffe le Fort fragment and the posterior malleolus (Volkmann fragment) (Figure 5)[18,19].
If the mechanism of injury and the clinical examination are suspicious for a syndesmotic injury, the plain radiography should be examined for: (1) the tibiofibular clear space; (2) the tibiofibular overlap; and (3) the increased medial clear space (Figure 4). These measurements are helpful to detect the presence of syndesmotic injuries[19].
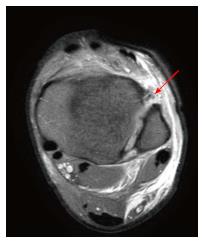
As a limitation, it should be mentioned that the measurements for the assessment of the syndesmosis on radiographs are based on cadaveric studies, and that the measurements are influenced by the quality of the radiographs. Recently, Hermans et al[20] investigated a study to compare magnetic resonance imaging (MRI) findings with plain radiographs in syndesmotic injuries. The authors found that the tibiofibular overlap and the tibiofibular clear space did not correlate with a syndesmotic injury seen on MRI. Therefore, further imaging with MRI scan is recommended, if there is any suspicion of a syndesmotic lesion. The sensitivity and specificity of MRI scans for the evaluation of the syndesmotic complex is up to 100%, and the integrity of the syndesmosis can be optimally visualized on MRI axial views (Figure 6)[21,22].
In addition to plain radiographs, manual or the gravity external rotation stress radiographs can be applied to the injured ankle to evaluate the integrity of the deltoid ligament[23]. The amount of medial clear space widening of > 5 mm is highly suspicious for a rupture of the deep deltoid ligament. As a limitation of the manual stress test it should be mentioned that the amount of applied force necessary when performing an external rotation stress radiograph is not well defined and mainly determined by the patient’s pain level[23].
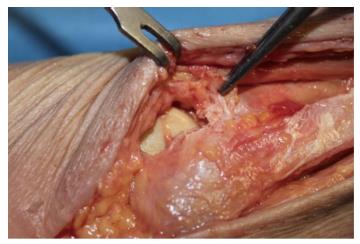
In the presence of fractures, clinical or radiological examination of the syndesmotic integrity is not necessary, as this can be done intraoperatively[6]. Lui et al[24] could show that arthroscopy can detect syndesmotic injuries more reliable than intraoperative stress radiographs. However, arthroscopy of the ankle joint is technically demanding and therefore, it is not used routinely. Normally, the integrity of the syndesmosis is checked by the hook test following fixation of ankle fractures (Figure 1). Alternatively, especially in unclear cases with fracture type Weber B, the integrity of the syndesmosis can be verified by intraoperative visualization and by intraoperative testing of the stability (Figure 7).
Syndesmotic injuries without an associated fracture occur much less frequently compared to fracture associated syndesmotic lesions[6,25]. However, if an isolated syndesmotic injury is missed, it is prone to deteriorated clinical outcome with pain and instability. The management of isolated syndesmotic injuries is still under discussion. In simple syndesmotic sprains without diastasis of the syndesmotic region most authors prefer non-operative management with a non-weight bearing cast and report good functional long-term results[26]. In contrast, a displaced and widened mortise needs operative fixation of the syndesmosis[26,27].
Non-surgical management includes plaster immobilization for 2-6 wk with a non weight-bearing cast[26]. There are only few literature data available reporting on clinical results after conservative treatment of isolated syndesmotic injuries. Recently, a comprehensive review with isolated syndesmotic injuries has been published[25]. The period of plaster immobilization varies between 2 and 6 wk indicating that there is no consensus. From our experience, plaster immobilization should be performed for at least 6 wk to prevent chronic instability and recurrent injuries.
The reported complication rates after non-surgical management of isolated syndesmotic injuries were high (up to 68%)[28-30]. The most common complications recorded in the studies were stiffness, pain with activity, heterotopic ossification and residual painful instability.
Reports about operatively treated isolated syndesmotic injuries are rare. Taylor et al[31] published the results of six patients with isolated syndesmotic injuries that were treated operatively with a 4.5-mm stainless steel cortical screw. The mean time from injury to treatment was 3 d and all the patients were treated within 7 d. Average time to return to sports was 40.7 d (32-48 d) in all patients. The assessment of the clinical outcome showed good to excellent results in all patients.
In the treatment of ankle fractures with an associated syndesmotic lesion the primary goal is to restore ankle stability and to maintain correct alignment of tibia and fibula to allow sufficient healing of the syndesmotic ligaments[32]. In the case of surgical stabilization, the method of fixation is still under discussion[6]. Beside the use of syndesmotic screws, which is the most widespread method, suturing of the syndesmosis, syndesmosis hooks, bioabsorbable screws, Endo Buttons (Smith and Nephew Endoscopy, Andover, Massachusetts), and the TightRope device (Arthrex, Naples, Florida), which in particular became popular in the last decade, are also used for syndesmotic fixation[6].
Stabilization of the ankle mortise is generally recommended, when the fracture pattern, intraoperative assessment with a hook or the direct visualization demonstrates a syndesmotic diastasis. A consensus for the appropriate size of the syndesmosis screw has not been reached yet. Most authors prefer either 3.5 or 4.5 mm cortical screws. In Europe most surgeons use one single 3.5-mm tricortical diastasis screw for stabilization of the syndesmosis in Weber B or C fractures. The preferred height is at 2.1 to 4 cm above the ankle joint line. Two syndesmotic screws are commonly used in Maisonneuve fractures[33]. In biomechanical studies, 3.5 and 4.5 mm cortical screws showed comparable biomechanical characteristics[34]. In cadaveric studies the influence of the numbers of syndesmotic screws has been investigated[35]. There is evidence that two screws provide a better construct biomechanically compared to one diastasis screw alone.
The placement height of the syndesmotic screw and the number of cortices engaged with the diastasis screws are also the topic of an ongoing discussion. Beumer et al[35] could show that there is no difference in clinical outcome comparing the engagement of three vs four cortices. Most authors agree that diastasis screws should be placed 2 to 3 cm proximal to the tibial plafond. Interestingly, the placement of diastasis screws at 2, 3 and 5 cm proximal to the ankle joint seems to have no influence on functional outcome[36].
Despite the invention of novel devices such as the Tightrope or bioabsorbable screws for restoration and maintenance of the congruent syndesmosis following syndesmotic injury, the metallic syndesmotic screw is still considered to be the gold standard[37]. A possible disadvantage of the syndesmotic screw is the need for implant removal. In general, the syndesmosis takes 8 to 12 wk to heal, and afterwards removal of the hardware is recommended by most authors[38]. However, the hardware removal is accompanied by high complication rates such as wound infection, re-occurrence of screw breakage and diastasis during removal[39]. Alternatively, the syndesmotic screw can be left in situ. Schepers published a review with 472 patients included with retained syndesmotic screws. Eighty patients had loose diastasis or broken screws[40]. Despite this, there were no significant differences in clinical outcome between retained or removed screws.
Another alternative fixation device are bioabsorbable screws. Bioabsorbable screws can be used instead of syndesmotic screws for stabilization of the syndesmosis but have the advantage that screw removal is unnecessary. A recently published review compared the results of bioabsorbable and metallic syndesmotic screws[38]. Bioabsorbable syndesmotic screws and metallic syndesmotic screws were comparable with respect to the incidence of complications and range of motion. However, the absolute number of complications was greater with bioabsorbable screws (23.4% vs 5.7%). Most frequent complications of bioabsorbable screws were wound-related complications in 19.7% of the patients.
Currently, debate exists over rigid screw fixation vs suture button techniques as the ideal fixation method. The theoretical advantages of a suture-button device over metallic syndesmotic screws are that it allows physiologic motion at the syndesmosis while maintaining the reduction, less risk of hardware pain and subsequent implant removal, and it may permit earlier return to motion as there is no risk of screw breakage and subsequent recurrent syndesmotic diastasis[41]. In a cadaveric study, Teramoto et al[42] sequentially assessed native syndesmosis ligament stability, suture button, and screw fixation for diastasis in six anatomic specimens. With anatomically directed fixation, there was no significant difference in diastasis for any fixation technique compared with the intact native ligaments. However, screw fixation provided the most rigid fixation and greatest stability against external rotation force.
In the last two decades, many authors have sought to compare suture button techniques vs rigid fixation with cortical screws[26]. To date, for isolated unstable syndesmosis injuries, no study has shown suture button techniques to be inferior to rigid fixation with regard to joint stability and patient satisfaction.
The use of the Tightrope as fixation method of the ankle diastases has been developed recently. Naqvi et al[43] reported on their experience with 49 patients who were stabilized with the Tightrope device, and found satisfactory clinical results after 2 years of follow-up. One major advantage of this method compared to screws is that there is no need to remove the knot routinely. A potential limitation of this technique might be the higher costs compared to the screws and, some authors have reported soft tissue irritation from the knot with the need for revision surgery[44]. According to current literature, the functional outcome is comparable using either Tightrope or syndesmotic screws as fixation device. Detailed analysis of both groups revealed that the Tightrope device was superior to syndesmotic screws regarding the time to return to work. In addition, fewer patients needed implant removal after Tightrope fixation of the syndesmotic diastasis. Recently, a prospective randomized controlled study was published to compare syndesmosis screw and TightRope fixation in terms of accuracy and maintenance of syndesmosis reduction using intraoperative 3D imaging and postoperative bilateral computed tomography (CT)[45]. No difference was found regarding reduction of the syndesmosis. At two-year follow-up the incidence of ankle joint osteoarthritis and functional outcome showed no difference between the fixation methods.
Several cadaveric studies have demonstrated that standard radiographic measurements used to evaluate the integrity of the syndesmosis are inaccurate and unreliable[46-48]. Multiple articles have described malreduction after operative treatment in up to 50% of the cases[46,49]. Even under direct visualization of the syndesmotic region malreduction has been reported in about 15% because of missing anatomical landmarks[50-52]. A CT scan allows better visualization of the transverse relationship between the fibula and incisura fibularis[53-55].
Accuracy of reduction has been shown to correlate with poorer outcome and the development of post-traumatic arthritis[56-58]. Therefore, some authors advocate the use of a CT scan routinely after operative stabilization of syndesmotic diastasis[59]. Gardner et al[46] reported on 25 patients who underwent open reduction of a syndesmotic diastasis, and postoperative CT scans showed that 52% of the patients had a malreduced fibula within the incisura.
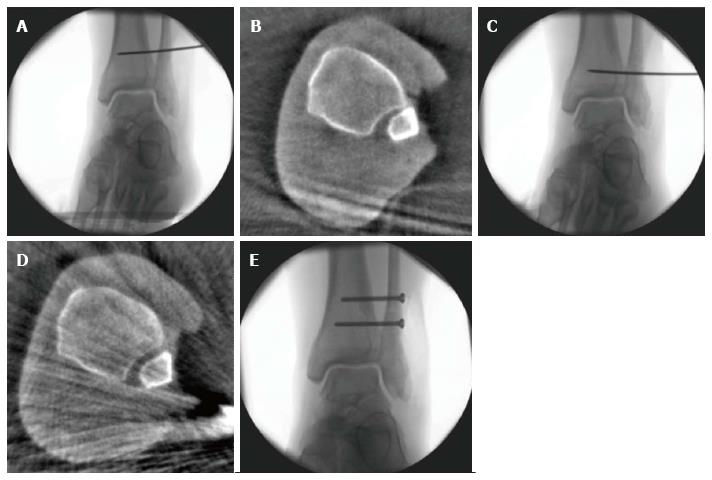
One possible solution to overcome these problems might be the routine use of intraoperative three-dimensional imaging, as this will allow anatomical fixation of the syndesmosis and immediate intraoperative revision in the case of malreduction. Franke et al[3] investigated a study with the routine use of the intraoperative three-dimensional scan for the assessment of accuracy of syndesmosis reduction in 251 patients. After closed reduction and fixation of the syndesmosis with a 3.5 mm syndesmosis screw, a conventional check of the ankle joint by fluoroscopy in the three standard views was performed. Only if the findings on fluoroscopy showed an adequate reduction by the surgeon’s impression an intraoperative three-dimensional scan was performed. In 82 patients (32.7%), malreduction of the syndesmosis was found on the three-dimensional scan despite the fact that the fracture appeared to be adequately reduced on fluoroscopy. After immediate intraoperative revision(s), a repeated intraoperative three-dimensional scan showed anatomical reduction of the syndesmosis.
Examples of intraoperative assessment of syndesmotic reduction with an intraoperative three-dimensional scan are shown in Figure 8.
Syndesmotic injuries are common lesions after ankle sprain and require careful examination and management. A displaced and widened mortise requires operative fixation of the syndesmosis. Variable fixation techniques have been reported with comparable results. Furthermore, accuracy of reduction of the syndesmosis is of great concern, as it has been shown to correlate with poorer outcome and the development of post-traumatic osteoarthritis. In view of the high percentage of patients with malreduction of the syndesmosis, intraoperative three-dimensional imaging may be a solution for overcoming this problem. Alternatively, a postoperative CT scan should be performed to assess appropriate reduction.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Fanter NJ, Ohishi T, Zhen P S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Egol KA, Pahk B, Walsh M, Tejwani NC, Davidovitch RI, Koval KJ. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. J Orthop Trauma. 2010;24:7-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 165] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 2. | Stark E, Tornetta P, Creevy WR. Syndesmotic instability in Weber B ankle fractures: a clinical evaluation. J Orthop Trauma. 2007;21:643-646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 76] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Franke J, von Recum J, Suda AJ, Grützner PA, Wendl K. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am. 2012;94:1386-1390. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 120] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 4. | Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294-298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 288] [Cited by in F6Publishing: 237] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10:325-330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 268] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Magan A, Golano P, Maffulli N, Khanduja V. Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull. 2014;111:101-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | McCollum GA, van den Bekerom MP, Kerkhoffs GM, Calder JD, van Dijk CN. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21:1328-1337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 109] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 8. | Beumer A, Valstar ER, Garling EH, Niesing R, Ginai AZ, Ranstam J, Swierstra BA. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77:531-540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 9. | Xenos JS, Hopkinson WJ, Mulligan ME, Olson EJ, Popovic NA. The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J Bone Joint Surg Am. 1995;77:847-856. [PubMed] [Cited in This Article: ] |
| 10. | Lauge-hansen N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950;60:957-985. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 11. | Wuest TK. Injuries to the Distal Lower Extremity Syndesmosis. J Am Acad Orthop Surg. 1997;5:172-181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 79] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Zalavras C, Thordarson D. Ankle syndesmotic injury. J Am Acad Orthop Surg. 2007;15:330-339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 148] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 13. | van den Bekerom MP, Lamme B, Hogervorst M, Bolhuis HW. Which ankle fractures require syndesmotic stabilization? J Foot Ankle Surg. 2007;46:456-463. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27:276-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 101] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Beumer A, Swierstra BA, Mulder PG. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73:667-669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Müller ME, Koch P, Nazarian S, Schatzker J. The comprehensive classification of fractures of long bones. Berlin: Springer-Verlag 1990; . [DOI] [Cited in This Article: ] |
| 17. | Harper MC. Ankle fracture classification systems: a case for integration of the Lauge-Hansen and AO-Danis-Weber schemes. Foot Ankle. 1992;13:404-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 39] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Park JW, Kim SK, Hong JS, Park JH. Anterior tibiofibular ligament avulsion fracture in weber type B lateral malleolar fracture. J Trauma. 2002;52:655-659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Dias LS, Giegerich CR. Fractures of the distal tibial epiphysis in adolescence. J Bone Joint Surg Am. 1983;65:438-444. [PubMed] [Cited in This Article: ] |
| 20. | Hermans JJ, Wentink N, Beumer A, Hop WC, Heijboer MP, Moonen AF, Ginai AZ. Correlation between radiological assessment of acute ankle fractures and syndesmotic injury on MRI. Skeletal Radiol. 2012;41:787-801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. 2004;182:131-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 152] [Cited by in F6Publishing: 156] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 22. | Hermans JJ, Beumer A, Hop WC, Moonen AF, Ginai AZ. Tibiofibular syndesmosis in acute ankle fractures: additional value of an oblique MR image plane. Skeletal Radiol. 2012;41:193-202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | van den Bekerom MP, Mutsaerts EL, van Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2009;129:227-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Lui TH, Ip K, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy. 2005;21:1370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 86] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | van Dijk CN, Longo UG, Loppini M, Florio P, Maltese L, Ciuffreda M, Denaro V. Conservative and surgical management of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24:1217-1227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Miller TL, Skalak T. Evaluation and treatment recommendations for acute injuries to the ankle syndesmosis without associated fracture. Sports Med. 2014;44:179-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14:232-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 28. | Fritschy D. An unusual ankle injury in top skiers. Am J Sports Med. 1989;17:282-285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 87] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29:31-35. [PubMed] [Cited in This Article: ] |
| 30. | Taylor DC, Englehardt DL, Bassett FH. Syndesmosis sprains of the ankle. The influence of heterotopic ossification. Am J Sports Med. 1992;20:146-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 149] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 31. | Taylor DC, Tenuta JJ, Uhorchak JM, Arciero RA. Aggressive surgical treatment and early return to sports in athletes with grade III syndesmosis sprains. Am J Sports Med. 2007;35:1833-1838. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Hunt KJ, Phisitkul P, Pirolo J, Amendola A. High Ankle Sprains and Syndesmotic Injuries in Athletes. J Am Acad Orthop Surg. 2015;23:661-673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 33. | Schepers T, van Zuuren WJ, van den Bekerom MP, Vogels LM, van Lieshout EM. The management of acute distal tibio-fibular syndesmotic injuries: results of a nationwide survey. Injury. 2012;43:1718-1723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 34. | Thompson MC, Gesink DS. Biomechanical comparison of syndesmosis fixation with 3.5- and 4.5-millimeter stainless steel screws. Foot Ankle Int. 2000;21:736-741. [PubMed] [Cited in This Article: ] |
| 35. | Beumer A, Campo MM, Niesing R, Day J, Kleinrensink GJ, Swierstra BA. Screw fixation of the syndesmosis: a cadaver model comparing stainless steel and titanium screws and three and four cortical fixation. Injury. 2005;36:60-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 100] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 36. | McBryde A, Chiasson B, Wilhelm A, Donovan F, Ray T, Bacilla P. Syndesmotic screw placement: a biomechanical analysis. Foot Ankle Int. 1997;18:262-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 150] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 37. | Kaftandziev I, Spasov M, Trpeski S, Zafirova-Ivanovska B, Bakota B. Fate of the syndesmotic screw--Search for a prudent solution. Injury. 2015;46 Suppl 6:S125-S129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 38. | van der Eng DM, Schep NW, Schepers T. Bioabsorbable Versus Metallic Screw Fixation for Tibiofibular Syndesmotic Ruptures: A Meta-Analysis. J Foot Ankle Surg. 2015;54:657-662. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 39. | Andersen MR, Frihagen F, Madsen JE, Figved W. High complication rate after syndesmotic screw removal. Injury. 2015;46:2283-2287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg. 2011;131:879-883. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 102] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 41. | Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012;36:1199-1206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 140] [Cited by in F6Publishing: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 42. | Teramoto A, Suzuki D, Kamiya T, Chikenji T, Watanabe K, Yamashita T. Comparison of different fixation methods of the suture-button implant for tibiofibular syndesmosis injuries. Am J Sports Med. 2011;39:2226-2232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 43. | Naqvi GA, Shafqat A, Awan N. Tightrope fixation of ankle syndesmosis injuries: clinical outcome, complications and technique modification. Injury. 2012;43:838-842. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 44. | Qamar F, Kadakia A, Venkateswaran B. An anatomical way of treating ankle syndesmotic injuries. J Foot Ankle Surg. 2011;50:762-765. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 45. | Kortekangas T, Savola O, Flinkkilä T, Lepojärvi S, Nortunen S, Ohtonen P, Katisko J, Pakarinen H. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury. 2015;46:1119-1126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 119] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 46. | Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788-792. [PubMed] [Cited in This Article: ] |
| 47. | Nielson JH, Gardner MJ, Peterson MG, Sallis JG, Potter HG, Helfet DL, Lorich DG. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;216-221. [PubMed] [Cited in This Article: ] |
| 48. | Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, Swierstra BA. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;227-234. [PubMed] [Cited in This Article: ] |
| 49. | Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011;32:616-622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 93] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 50. | Miller AN, Carroll EA, Parker RJ, Boraiah S, Helfet DL, Lorich DG. Direct visualization for syndesmotic stabilization of ankle fractures. Foot Ankle Int. 2009;30:419-426. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 51. | Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26:439-443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 305] [Cited by in F6Publishing: 304] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 52. | Lilyquist M, Shaw A, Latz K, Bogener J, Wentz B. Cadaveric Analysis of the Distal Tibiofibular Syndesmosis. Foot Ankle Int. 2016;37:882-890. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 53. | Laflamme M, Belzile EL, Bédard L, van den Bekerom MP, Glazebrook M, Pelet S. A prospective randomized multicenter trial comparing clinical outcomes of patients treated surgically with a static or dynamic implant for acute ankle syndesmosis rupture. J Orthop Trauma. 2015;29:216-223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 54. | Malhotra G, Cameron J, Toolan BC. Diagnosing chronic diastasis of the syndesmosis: a novel measurement using computed tomography. Foot Ankle Int. 2014;35:483-488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 55. | Mukhopadhyay S, Metcalfe A, Guha AR, Mohanty K, Hemmadi S, Lyons K, O’Doherty D. Malreduction of syndesmosis--are we considering the anatomical variation? Injury. 2011;42:1073-1076. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 56. | Yablon IG, Leach RE. Reconstruction of malunited fractures of the lateral malleolus. J Bone Joint Surg Am. 1989;71:521-527. [PubMed] [Cited in This Article: ] |
| 57. | Chissell HR, Jones J. The influence of a diastasis screw on the outcome of Weber type-C ankle fractures. J Bone Joint Surg Br. 1995;77:435-438. [PubMed] [Cited in This Article: ] |
| 58. | Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19:102-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 359] [Cited by in F6Publishing: 345] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 59. | Taser F, Shafiq Q, Ebraheim NA. Three-dimensional volume rendering of tibiofibular joint space and quantitative analysis of change in volume due to tibiofibular syndesmosis diastases. Skeletal Radiol. 2006;35:935-941. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |