Published online Feb 18, 2019. doi: 10.5312/wjo.v10.i2.71
Peer-review started: October 24, 2018
First decision: November 1, 2018
Revised: December 11, 2018
Accepted: January 5, 2019
Article in press: January 6, 2019
Published online: February 18, 2019
Cuboid fractures due to the particular bone anatomy and its protected location in the midfoot are rare, and they are usually associated with complex injuries of the foot. Clinical examination to diagnose these fractures should be detailed and the differential diagnosis, especially in the case of vague symptoms, should include the exclusion of all lateral foot pain causes. Conventional radiographs do not always reveal occult fractures, which can be under diagnosed especially in children. In this case, further investigation including magnetic resonance imaging or scintigraphy may be required. The treatment of these injuries depends on the particular fracture characteristics. Non-displaced isolated fractures of the cuboid bone can be effectively treated conservatively by immobilization and by avoiding weight bearing on the injured leg. In the case of shortening of the lateral column > 3 mm or articular displacement > 1 mm, surgical management of the fracture is mandatory in order to avoid negative biomechanical and functional consequences for the foot and adverse effects such as arthritis and stiffness as well as painful gait. In this review, an update on diagnosis and management of cuboid fractures is presented.
Core tip: The cuboid bone is an essential anatomic element of the midfoot contributing greatly to foot biomechanics. Cuboid fractures are rare and usually associated with complex foot fractures and dislocations. Such fractures require a high level of attention in order to ensure a timely diagnosis. Besides a detailed physical examination, further radiological assessment will identify the presence and type of fracture. Although simple cuboid fractures are effectively treated conservatively, displaced fractures require surgical treatment in order to avoid future devastating consequences. Because of the lack of adequate scientific evidence, the ideal surgical approach is still not universally accepted.
- Citation: Angoules AG, Angoules NA, Georgoudis M, Kapetanakis S. Update on diagnosis and management of cuboid fractures. World J Orthop 2019; 10(2): 71-80
- URL: https://www.wjgnet.com/2218-5836/full/v10/i2/71.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i2.71
Cuboid single fractures are rare due to the particular bone anatomy and the protected location of the midfoot. Their annual frequency reaches 1.8 per 100000 in the United Kingdom[1] and typically occur in combination with other midfoot fractures such as navicular or cuneiforms fractures or are associated with Lisfranc and Chopart fractures and dislocations[2,3].
Cuboid fractures can be the result of bone injury due to compression after a car accident or direct crush of the lateral aspect of the dorsum of the foot as it may happen after a heavy object falls on the foot. They may also be the result of avulsion injury involving any ligamentous attachments of the cuboid e.g., calcaneocuboid ligament. Such an injury is attributed to ankle sprain as a result of a twisting injury of the foot with the hindfoot inverted and the forefoot adducted. A particular type of isolated cuboid fracture was presented in the literature by Hermel and Gershon-Cohen[6] in 1953 who coined the term “nutcracker fracture” in order to describe a cuboid fracture that is caused by compression between the calcaneus proximally and the bases of the fourth and fifth metatarsals distally. This fracture is the result of forced plantar flexion of the hindfoot and midfoot against the fixed and forced abduction forefoot[2,4-6]. This injury is also described as a result of equestrian-related injuries in children and adolescents where compression cuboid fractures are combined with other midfoot injuries such as avulsion and compression navicular or cuneiform fractures[7].
Cuboid stress fractures are less common than fractures in other tarsal bones such as calcaneus and navicular because the cuboid is not a weight-bearing bone[8]. These fractures may occur in both toddlers[9-13] and adults[8,14-17] and may be a result of overuse affecting athletes[8,15] or military recruits[18]. They may also follow osteoporosis and reduced bone strength[17]. Although they are successfully treated non-operatively without having adverse effects due to vague symptoms, they may initially not come to attention[5].
Cuboid fractures are not always recognized promptly due to the special anatomy of the foot and the difficulty in interpreting the radiologic findings. However, delayed identification and effective treatment of these injuries may have adverse effects on the biomechanics of the foot, such as loss of length of the lateral column resulting in forefoot abduction and also lesser metatarsals lateral subluxation, resulting in planus deformity associated with compensatory hindfoot eversion and posterior tibial tendon insufficiency[4,19]. Anatomical disorder of the bone articulations with tarsal bones of may lead to foot stiffness and painful arthritis as well as foot deformity[20].
This review analyzes the modern diagnostic and therapeutic approach of these rare though challenging fractures whose inappropriate and delayed management, according to their specific characteristics can have significant negative consequences on the mechanics and functionality of the foot, causing pain and stiffness to the injured limb with a final negative impact on a patient’s quality of life.
The cuboid is one of the seven bones of the midfoot and hindfoot located most laterally in the distal tarsal row in the center of the foot lateral column. It has a pyramidal shape with five articular surfaces that are articulated with the bases of the fourth and fifth metatarsal bones in front with the calcaneus on the back as well as with the lateral cuneiform and navicular medially (Figure 1). Hence it is the only bone of the tarsus involved both in the tarsometatarsal joint (Lisfranc complex) and in the midtarsal joint (Chopart’s joint). It also links the lateral column to the transverse plantar arch[4,19,21-24]. Its articulation with the fourth and fifth metatarsals provides mobility three times greater than the mobility of the first through third tarsometatarsal joints and has the largest contribution to the dorsiflexion and plantar flexion of the midfoot[19,23]. It also has a primary contribution to pronation and supination assisted in this function by the calcaneocuboid joint[19].
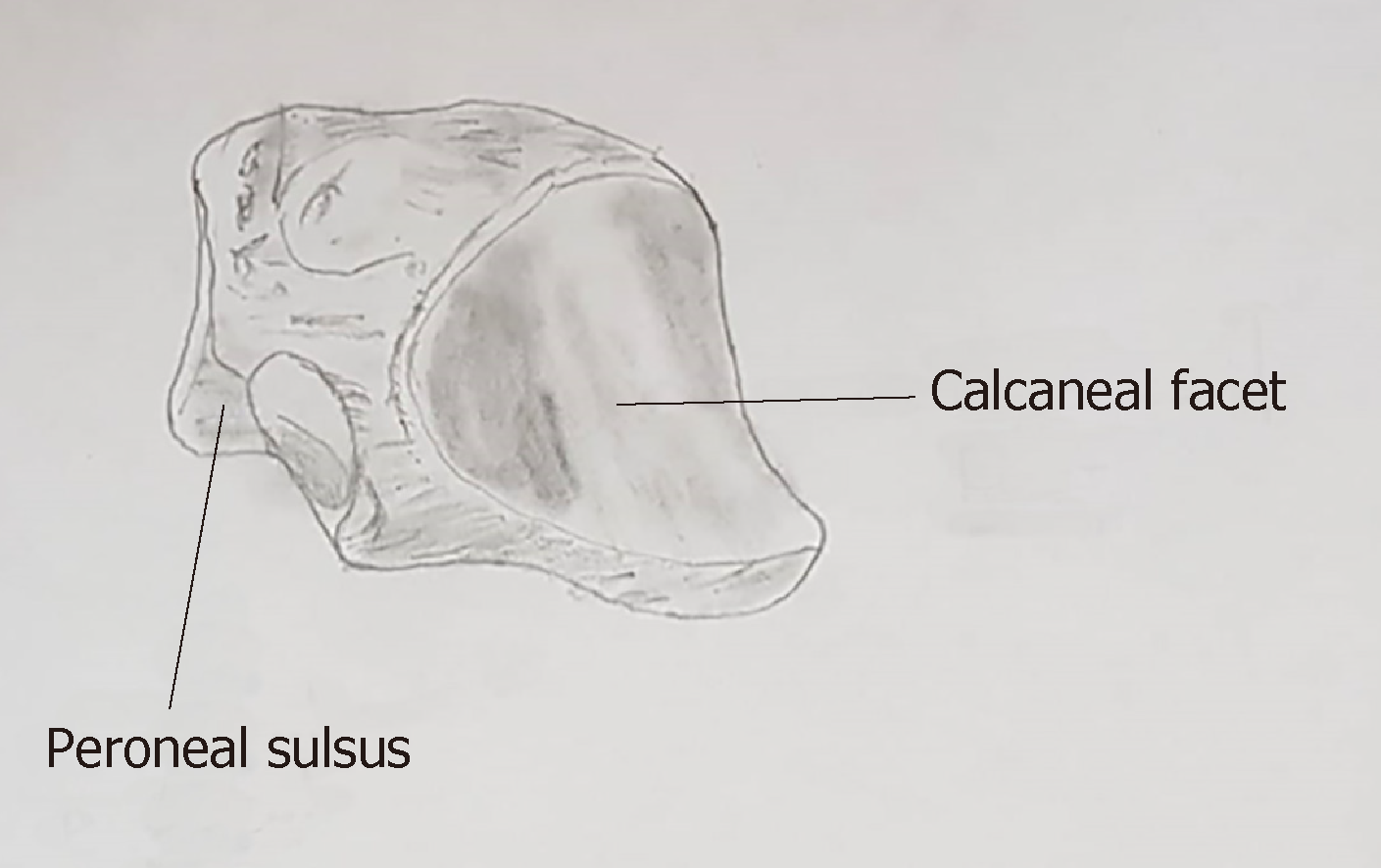
Due to its special anatomy and its position, the cuboid is the main supporting element of the rigid and static lateral column and ensures that its length is maintained. Its role is supported by a number of ligamentous, capsuloligamentous, and tendinous restraints. Although it does not participate directly in weight bearing, it receives significant forces during standing and ambulation, and its contribution is important in the mobility of the foot lateral column and the adaptation of the foot when walking on an uneven terrain[14,23]. The dorsal surface of the bone is bare, but on its plantar surface there is a groove that runs obliquely distal and medially and from which the tendon of peroneus longus passes acting as a fulcrum for the peroneus longus muscle contraction[4] (Figure 2). Gathering forces in this area during activities such as running can cause stress fractures[8].
Cuboid vascularization is ensured by the lateral plantar artery where anastomosis exists between the medial plantar artery. The satisfactory blood supply of the bone also explains the satisfactory bone consolidation following a fracture and the rare occurrence of events such as nonunion or osteonecrosis[4].
Although there is not a universally accepted classification system, cuboid fractures are classified according to their characteristics regarding the displacement of the fragments, the involvement of the articular surfaces, and the avulsion or comminuted type of fracture[23].
The Orthopaedic Trauma Association subdivides these fractures into three main categories[25]. Group A includes the simple extraarticular fractures, Group B includes calcaneocuboid or metatarsocuboid joint fractures, and Group C includes fractures involving both joints. This classification further subdivides the cuboid fractures from the simplest ones up to the most complex in each category according to the level and the particular anatomical position of each fracture. The fractures of each group are denoted with numbers with the most complex fractures being characterized by higher numbers.
Fenton et al[19] proposed the classification of cuboid fractures into five groups. A type 1 fracture is the most common type of avulsion fracture involving the capsule of the calcaneocuboid joint. Type 2 includes stable isolated extra-articular injuries of the fracture that do not require surgical treatment because the length of the foot lateral column is maintained, and there is no intra-articular involvement. Type 3 injuries are isolated intra-articular fractures within the body of the cuboid involving the calcaneocuboid, the tarsometatarsal joint, or both of them. The fractures of this category are treated conservatively. Type 4 fractures are associated with disruption of the midfoot as well as with tarsometatarsal injuries. These intra-articular fractures require anatomic reduction and stabilization. Finally, type 5 fractures are high-energy crushing injuries of the cuboid that may be accompanied by disruption of the mid-tarsal joint and loss of length of the lateral column alone or in combination with the medial column. These fractures are mostly treated surgically except in cases where the length of the foot lateral column is maintained.
The diagnosis of cuboid fractures, particularly of those that are not accompanied by other foot injuries, may be difficult. The early detection of these fractures requires a high degree of suspicion[26]. Regarding children, local swelling and antalgic limp with refusal to bear weight on the lateral side of the foot may accompany a fracture of the cuboid[11,27]. Cuboid fractures may be associated with lateral foot pain especially with push off when walking[28]. Typically there is tenderness to direct palpation of the cuboid over the lateral aspect of the midfoot (Figure 3) while the fracture can be accompanied by deformity, ecchymosis, or fracture blisters[5,22,23]. In the event that the calcaneocuboid joint is unstable, diagnostic maneuvers that control the integrity of this joint can cause pain[28].
Stress fractures of the cuboid may have no obvious clinical signs. Painful gait and mild tenderness on the lateral side of the foot may be present without swelling or evident hematoma[16]. Pain may be mild with a progressive nature and accompany a recent increase in athletic or other daily activity level of an individual. If there is significant periosteal reaction or sclerosis in the fracture area, then a palpable mass may be present in the area of maximum tenderness. The placement of a vibrating tuning fork just above the area of maximum tenderness can cause an increase in pain intensity and has been proposed as a diagnostic method for stress fractures[29].
Plain X-ray radiography usually diagnoses simple fractures of the cuboid and includes the anterior, posterior, lateral, and standard oblique view of the foot[4]. Imaging examination should include contralateral foot for the comparison and determination of the length of the foot lateral column as well as for the appropriate preoperative planning. The integrity of the foot lateral column can be evaluated by the anteroposterior view, which also allows the detection of any transverse plane deformity. The lateral radiograph assesses the congruity of the calcaneocuboid joint and can also reveal avulsion fractures[28]. The standard medial oblique view is particularly useful for assessing cuboid fractures because it allows the view of the cuboid and its articulation with the metatarsals and the calcaneus, free of superimposition of the bones with the open and equal cuboid joint. It also contributes to the evaluation of the length of the lateral column[4,23].
Although conventional radiography can provide a lot of information about the nature of the cuboid bone injury, the considerable overlap of bony structures in the foot leads to a failure regarding the depiction of occult cuboid fractures[30]. Miller et al[2] found that in 17 patients with pain over the lateral aspect of the midfoot, the X-ray radiography revealed cuboid fractures in only seven of them.
Computed tomography (CT) may provide additional information regarding the size, exact location, and pattern of fractures of the cuboid, as well as associated injuries such as other fractures and dislocations of other bones of the foot[7,8]. It clearly depicts tarsometatarsal joints and Lisfranc joint and also provides information on the fracture healing progression[8,31].
In the case of non-diagnostic radiography findings using plain film radiographs the contribution of magnetic resonance imaging (MRI) is a valuable, sensitive examination for the diagnosis of cuboid fractures in both children and adults[24,32,33] (Figure 4). Μiller et al[2] found that in 17 adults with isolated occult cuboid fractures, the presence of a fracture was confirmed by MRI in eight of them. In their recent study, O’Dell et al[24] used MRI to confirm cuboid fractures in 19 children aged 18 mo to 17 years, nine of whom the initial radiography was negative for fracture. This radiology examination revealed fractures that were the result of acute trauma or were stress fractures linear in configuration and most commonly adjacent to the tarsometatarsal joint.
In the case of cuboid fractures in the T1 weighted sequence, continuous hypointense signals are revealed in the cuboid bone extending from the cuneiform joint surface toward the lateral side as well as fat suppression[16], while in the T2 sequence a hyperintense signal in the bone as well as the loss of the bone marrow signal is detected[5].
Sonography, although not the method of choice for the detection of cuboid fractures, is a reliable and quick method when painful swelling adjacent to the bone is present in the case of subtle cuboid fractures with non-diagnostic plain radiography[5,30]. Bilateral ultrasonography that includes longitudinal and transverse scan planes reveals a cortical discontinuity and cortical step in the area of the fracture as well as soft tissue edema[5]. Wang et al[30] reported a study of 268 patients with post-traumatic pain in the area of the foot and ankle with negative findings in the initial radiology examination, where ultrasound examination revealed a fracture in 24 of them. Two of the patients examined suffered cuboid fractures.
Scintigraphy may reveal focal uptake in the cuboid and contribute to the early diagnosis of cuboid fractures, particularly in stress fractures in children in the case of a negative initial physical examination and non-diagnostic radiographs[9,12,13,15]. However, it should be taken into account that due to the complex anatomy of the midfoot, it is difficult to ascertain the exact intake area of the radiopharmaceutical, which reduces the diagnostic accuracy of the method[5].
Differential diagnosis includes bony causes of lateral foot pain such as ankle sprain, stress fractures of the foot, fracture of the fifth metatarsal distal to tuberosity, avulsion of the anterior process of the calcaneus, Lisfranc injuries, tarsal coalition, cuboid syndrome, and os perineum injury. Furthermore, soft tissue pathogens such as peroneus, longus tendon tenosynovitis or partial tearing, subluxing peroneal tendons, extensordigitorum, tendonitis, sinus tarsi syndrome, and lateral plantar nervous entrapment may have a similar clinical picture to cuboid fractures and should be excluded during the initial diagnosis in the case of negative radiology evaluation with a clinical picture similar to a cuboid fracture[2,28,34,35] (Table 1).
| Differential diagnosis of lateral foot pain |
| Ankle sprain |
| Peroneal tendonitis |
| Peroneus longus tendon tear |
| Subluxing peroneal tendons |
| Stress fracture |
| Fracture of the shaft of the fifth metatarsal |
| Avulsion of the base of the fifth metatarsal |
| Apophysitis of the fifth metatarsal |
| Jones fracture |
| Avulsion of the anterior process of the calcaneus |
| Lisfranc injuries |
| Tarsal coalition |
| Cuboid syndrome |
| Os peroneum fracture |
| Sinus tarsi syndrome |
| Lateral plantar nerve entrapment |
Cuboid syndrome is caused by the structural congruity of the calcaneocuboid joint and subluxation of the cuboid and usually concerns athletes or dancers. It is characterized by pain in the area of the plantar surface of the cuboid or in the foot. Two clinical maneuvers have been proposed for the clinical diagnosis of the syndrome, namely the midtarsal adduction and the midtarsal supination test[28,36].
Os perineum is an accessory bone located within the peroneus longus tendon adjacent to the lateral plantar aspect of the cuboid, which can cause foot pain. It is found in 4% to 30% of normal feet[28,37]. In most cases, it is asymptomatic but may be the cause of acute and chronic foot pain as in cases of stress fracture or diastasis. For the diagnosis of the syndrome, plain radiography films may be diagnostic or further examination by CT, MRI and/or sonography may be required[28].
The therapeutic approach of cuboid fractures is adjusted according to the severity of the fracture. Non-displaced low energy fractures such as avulsion fractures and stress fractures are effectively treated with conservative methods of treatment while complex high-energy injuries involving complex fractures with significant displacement and intra-articular involvement require anatomic reduction and external or internal osteosynthesis depending on the particular fracture characteristics.
In cuboid fractures with minimal pain and swelling, treating with an elastic bandage or with a fracture boot and walking with partial weight bearing until the satisfactory regression of the symptoms, may be enough. In the case of severe initial pain, a short walking cast for 4-6 wk is recommended[30]. Stress fractures require limiting the activity and use of the limb while it is recommended to have plantar arch support[16]. Avulsion fractures are treated with protected weight bearing as tolerated and a fracture boot for 4 to 6 wk[23]. These fractures require regular radiographic evaluation every month as they may be complicated with fibrous non-union. In this case as well as in the presence of recalcitrant pain, excisional surgery may be necessary[28].
According to Borrelli et al[4], open cuboid fractures are the only absolute indication for urgent surgical management. Surgery is also recommended when there is an articular displacement greater than 1 mm or a shortening of the foot lateral column length[22]. According to Holbein et al[38], this shortening requires surgical treatment of the fracture if it is greater than 3 mm. Surgical management of cuboid fractures includes external fixators, open reduction, and internal fixation with or without bone grafting and midtarsal arthrodesis[22]. The purpose of this surgical intervention is to restore the length of the lateral column as well as the normal anatomy and mobility of the surrounding joints, and in particular of the calcaneocuboid joint as well as of the fourth and fifth tarsometatarsal joints[20].
In the case of a severe comminution and displacement of fracture fragments and poor skin quality that does not allow open fixation, the application of spanning external fixation ensures that the length of the lateral column is restored[4,23].
The internal osteosynthesis of cuboid fractures can be conducted with lumbar or epidural anesthesia. The patient is placed in the supine position with a thigh tourniquet and a bump under the ipsilateral hip to avoid excessive external rotation of the foot and to ensure better access to the cuboid bone. A 6 cm lateral longitudinal incision over the cuboid from the tip of the fibula to the tip of the fifth metatarsal reveals the calcaneocuboid and tarsometatarsal joints and allows the anatomic reduction of the fracture or fractures[23] (Figure 5). The extension of this section, 5 mm centrally of the calcaneocuboid joint and beyond the level of the lateral base of the fifth metatarsal, allows a better view of the joints and the anatomic reduction of the fractures[4]. The incision is maintained at the lateral border of the extensor digitorum brevis muscle and proximal to the sural nerve, which must be identified and protected[4,22]. Further dissection is performed to visualize the extensor digitorum brevis and then the muscle belly is partially elevated off the periosteum to allow inspection of the cuboid as well as of the calcaneocuboid and tarsometatarsal joints[4,23].
After restoring the length of the cuboid, the dorsolateral wall is reconstructed. The articular surfaces should be reconstructed starting from the media fragments using the intact side of the joint as a model[20]. To maintain the reduction provisional fixation with small Kirschner wires may be required. The internal osteosynthesis is completed using locking or unlocking screws or mini fragment plates under fluoroscopy[4,23]. Any void is filled with autografts, allogenic, or cancellous bone chips, and an anatomic plate is placed over the cuboid to maintain the length. Postoperatively, the patient ambulates without weight bearing for 4-6 wk and for another 6 wk with partial weight bearing and with a walking cast. Full weight bearing walking is allowed after 12 wk[4,7,22].
Midtarsal primary arthrodesis is a surgical treatment method recommended for severe crush injuries with extensive comminution of the cuboid bone and articular involvement. However, this method presents the disadvantage of significant loss in lateral column motion and is mainly applied to less active patients[23,27]. In the case of failed internal fixation and persistent pain, secondary fusion may be an alternative treatment method[22].
The cuboid bone is located at the center of the lateral midfoot and its anatomic position provides a relative protection[17]. However, it is subject to a series of compressive and shearing forces[24]. Cuboid fractures, although rare, may be the result of direct or indirect pressure in the foot and usually associated with other fractures and dislocations in the area. Thus, these fractures can be the result of compression or crush of the lateral aspect foot[2].
Cuboid stress fractures are less frequent than other foot fractures as this bone is not weight bearing[8]. Although they are slightly more common in children, they have been are also described in adults[14]. They may be the result of increased athletic activity or involve bones with reduced strength such as after a prolonged corticosteroid uptake period[17]. A possible mechanism of this fracture assumes that these fractures are the result of the repetitive pull of the peroneus longus tendon as it passes through the peroneal groove of the cuboid[8].
Due to their vague symptoms and the complex anatomy of the area, cuboid fractures may not be detected initially. The diagnosis of these fractures should be immediate because their delayed detection and treatment can cause a shortening of the foot lateral column with particularly negative consequences for the biomechanics of the foot such as a painful flatfoot deformity associated with posterior tibial tendon insufficiency[20].
Conventional radiography includes the anterior, posterior, lateral, and standard oblique view of the foot[5]. The latest view provides useful information about the condition of the joints between the cuboid and the base of the fourth and fifth metatarsals as well as the length of the lateral column. CT is a diagnostic method that offers the best visualization for assessing fracture patterns and articular displacements[4]. In the presence of occult radiographs, further imaging modalities such as ultrasound examination, MRI, or scintigraphy can contribute to the early detection of the fracture and help avoid future adverse effects regarding foot function. Particularly in children these fractures often go undiagnosed due to non-diagnostic plain X-ray radiography and the difficulties faced in the clinical examination that constitutes the contribution of these modern imaging methods very useful[24,27].
Treatment depends on the type of the fracture. Factors that determine the method of treatment include the involvement of the articular surfaces of the bone, the disorder of joints architecture in which the bone is involved, the reduction of the length of the foot lateral column, and the presence of fractures and dislocations of the other bones in the area[4]. Non-displaced stable fractures can be treated conservatively by splinting or casting with or without restriction of weight bearing[20]. Open fractures, complex comminuted fractures, and fractures accompanied by a shortening of the length of the foot lateral column greater than 3 mm or articular displacement greater than 1 mm require surgical treatment[22,38]. The purpose of this therapeutic approach is to restore the lateral column length and plantar support of the midfoot, to restore the integrity of the articular surfaces of the calcaneocuboid and tarsometatarsal joints, and the mobility of the cuboid joints to the fourth and fifth metatarsal bases[20,22].
As there is no sufficient scientific evidence to allow safe conclusions about the optimal management of cuboid fractures, the current therapeutic approach is based presumably on personal experience and beliefs[25]. For example, some authors support that Kirschner wires are more reliable in maintaining reduction than external fixation[39] whilst another postulates that fixation of the fractured cuboid bone with plates is preferable than screws, which are not associated with satisfactory results[25]. More sophisticated surgical approaches such as preoperative planning locking plates based on 3D CT may contribute to the anatomical reduction of the fracture and therefore may provide more favorable outcomes[40]. Still, further research is needed, including studies of high quality with a focus to resolve uncertainties of management and determine which patients could be treated non-operatively or are candidates to develop arthrosis and warrant primary fusion[19,39].
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Tawonsawatruk T, Vulcano E, Yukata K S- Editor: Ji FF L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Court-Brown C, Zinna S, Ekrol I. Classification and epidemiology of midfoot fractures. Foot. 2006;16:138-141. [DOI] [Cited in This Article: ] |
| 2. | Miller TT, Pavlov H, Gupta M, Schultz E, Greben C. Isolated injury of the cuboid bone. Emerg Radiol. 2002;9:272-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Ohmori T, Katsuo S, Sunayama C, Mizuno K, Ojima T, Yamakado K, Ando T, Watanabe S, Hayashi S, Tsuchiya H. A Case Report of Isolated Cuboid Nutcracker Fracture. Case Rep Orthop. 2016;2016:3264172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Borrelli J, De S, VanPelt M. Fracture of the cuboid. J Am Acad Orthop Surg. 2012;20:472-477. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 5. | Enns P, Pavlidis T, Stahl JP, Horas U, Schnettler R. Sonographic detection of an isolated cuboid bone fracture not visualized on plain radiographs. J Clin Ultrasound. 2004;32:154-157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Hermel MB, GERSHON-COHEN J. The nutcracker fracture of the cuboid by indirect violence. Radiology. 1953;60:850-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 84] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ceroni D, De Rosa V, De Coulon G, Kaelin A. Cuboid nutcracker fracture due to horseback riding in children: Case series and review of the literature. J Pediatr Orthop. 2007;27:557-561. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Chen JB. Cuboid stress fracture. A case report. J Am Podiatr Med Assoc. 1993;83:153-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Blumberg K, Patterson RJ. The toddler's cuboid fracture. Radiology. 1991;179:93-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 54] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Blumberg K, Patterson RJ. Fractures of the cuboid bone in toddlers. Pediatr Radiol. 1999;29:563. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Senaran H, Mason D, De Pellegrin M. Cuboid fractures in preschool children. J Pediatr Orthop. 2006;26:741-744. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 12. | Joo SY, Jeong C. Stress fracture of tarsal cuboid bone in early childhood. Eur J Orthop Surg Traumatol. 2015;25:595-599. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Simonian PT, Vahey JW, Rosenbaum DM, Mosca VS, Staheli LT. Fracture of the cuboid in children. A source of leg symptoms. J Bone Joint Surg Br. 1995;77:104-106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Yu SM, Dardani M, Yu JS. MRI of isolated cuboid stress fractures in adults. AJR Am J Roentgenol. 2013;201:1325-1330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Beaman DN, Roeser WM, Holmes JR, Saltzman CL. Cuboid stress fractures: a report of two cases. Foot Ankle. 1993;14:525-528. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Hagino T, Ochiai S, Watanabe Y, Senga S, Takayama Y, Haro H. A case of a cuboid bone stress fracture in a senior high school rugby athlete. AP-SMART. 2014;1:132-135. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Franco M, Albano L, Kacso I, Gaïd H, Jaeger P. An uncommon cause of foot pain: The cuboid insufficiency stress fracture. Joint Bone Spine. 2005;72:76-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Greaney RB, Gerber FH, Laughlin RL, Kmet JP, Metz CD, Kilcheski TS, Rao BR, Silverman ED. Distribution and natural history of stress fractures in U.S. Marine recruits. Radiology. 1983;146:339-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 229] [Cited by in F6Publishing: 231] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Fenton P, Al-Nammari S, Blundell C, Davies M. The patterns of injury and management of cuboid fractures: a retrospective case series. Bone Joint J. 2016;98-B:1003-1008. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Mihalich RM, Early JS. Management of cuboid crush injuries. Foot Ankle Clin. 2006;11:121-126, ix. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Kolker D, Marti CB, Gautier E. Pericuboid fracture-dislocation with cuboid subluxation. Foot Ankle Int. 2002;23:163-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 22. | Yu G, Yu T, Yang Y, Li B, Yuan F, Zhou J. Nutcracker fracture of the cuboid: management and results. Acta Orthop Belg. 2012;78:216-219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Clements JR, Dijour F, Leong W. Surgical Management Navicular and Cuboid Fractures. Clin Podiatr Med Surg. 2018;35:145-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | O'Dell MC, Chauvin NA, Jaramillo D, Biko DM. MR imaging features of cuboid fractures in children. Pediatr Radiol. 2018;48:680-685. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Pountos I, Panteli M, Giannoudis PV. Cuboid Injuries. Indian J Orthop. 2018;52:297-303. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Lucerna A, Espinosa J, Butler N, Wenke A, Caltabiano N. Nutcracker Cuboid Fracture: A Case Report and Review. Case Rep Emerg Med. 2018;2018:3804642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Holbein O, Bauer G, Kinzl L. Fracture of the cuboid in children: case report and review of the literature. J Pediatr Orthop. 1998;18:466-468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | Traister E, Simons S. Diagnostic considerations of lateral column foot pain in athletes. Curr Sports Med Rep. 2014;13:370-376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Dodson NB, Dodson EE, Shromoff PJ. Imaging strategies for diagnosing calcaneal and cuboid stress fractures. Clin Podiatr Med Surg. 2008;25:183-201, vi. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Wang CL, Shieh JY, Wang TG, Hsieh FJ. Sonographic detection of occult fractures in the foot and ankle. J Clin Ultrasound. 1999;27:421-425. [PubMed] [DOI] [Cited in This Article: ] |
| 31. | Preidler KW, Peicha G, Lajtai G, Seibert FJ, Fock C, Szolar DM, Raith H. Conventional radiography, CT, and MR imaging in patients with hyperflexion injuries of the foot: diagnostic accuracy in the detection of bony and ligamentous changes. AJR Am J Roentgenol. 1999;173:1673-1677. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Sadineni RT, Pasumarthy A, Bellapa NC, Velicheti S. Imaging Patterns in MRI in Recent Bone Injuries Following Negative or Inconclusive Plain Radiographs. J Clin Diagn Res. 2015;9:TC10-TC13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Feldman F, Staron R, Zwass A, Rubin S, Haramati N. MR imaging: its role in detecting occult fractures. Skeletal Radiol. 1994;23:439-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Unnithan S, Thomas J. Not all ankle injuries are ankle sprains - Case of an isolated cuboid stress fracture. Clin Pract. 2018;8:1093. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Patterson SM. Cuboid syndrome: a review of the literature. J Sports Sci Med. 2006;5:597-606. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Durall CJ. Examination and treatment of cuboid syndrome: A literature review. Sports Health. 2011;3:514-519. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 37. | Schick F, Karanjia H, Daniel J, Dheer S, Langman C, Taweel N, Sullivan P, Lebaron T. Spontaneous Fracture of the Os Peroneum With Rupture of the Peroneus Longus Tendon. J Foot Ankle Surg. 2018;57:790-793. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 38. | Holbein O, Bauer G, Kinzl K. Displaced fractures of the cuboid: four case reports and review of the literature. Foot and Ankle Surgery. 1997;3:85-93. [DOI] [Cited in This Article: ] |
| 39. | Ahmed A, Westrick E. Management of Midfoot Fractures and Dislocations. Curr Rev Musculoskelet Med. 2018;11:529-536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Rony L, de Sainte Hermine P, Steiger V, Ferchaud F, Cronier P. Clinical and radiological outcomes of a cohort of 9 patients with anatomical fractures of the cuboid treated by locking plate fixation. Orthop Traumatol Surg Res. 2018;104:245-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |