Published online Sep 28, 2017. doi: 10.4329/wjr.v9.i9.365
Peer-review started: February 9, 2017
First decision: June 12, 2017
Revised: July 24, 2017
Accepted: August 2, 2017
Article in press: August 2, 2017
Published online: September 28, 2017
Familial gastrointestinal stromal tumor (GIST) is a rare autosomal dominant disorder associated with mutations in the KIT gene in the majority of cases. Although, exon 11 appears to be the hot spot region for approximately 95% of germline mutations, pathogenic variations have also been identified in exon 8, 13 and 17. Exon 13 germline mutations are extremely rare amongst familial GISTs and seven families with a germline mutation have been reported to date. Moreover, the role of imatinib mesylate in this rare familiar settings is not completely known so far. We describe here clinical, imaging, pathological and genetic findings of a family with four affected members; grandmother, his son and two grand-sons having a germline gain-of-function mutation of KIT in exon 13 and discuss the imatinib mesylate treatment surveillance outcomes towards disease management.
Core tip: Familial gastrointestinal stromal tumor (GIST) with exon 13 germline mutations are extremely rare. Moreover, there are only a few reports describing the response to imatinib in familial GISTs. The data on the role of imatinib in familial GISTs is still limited. Understanding the role of imatinib is important for the appropriate management of mutation positive familial GISTs. It is also crucial to be able to determine the role of specific germline KIT mutations in. We hereby report our findings in consideration of up-to-date information.
- Citation: Engin G, Eraslan S, Kayserili H, Kapran Y, Akman H, Akyuz A, Aykan NF. Imatinib response of gastrointestinal stromal tumor patients with germline mutation on KIT exon 13: A family report. World J Radiol 2017; 9(9): 365-370
- URL: https://www.wjgnet.com/1949-8470/full/v9/i9/365.htm
- DOI: https://dx.doi.org/10.4329/wjr.v9.i9.365
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors originating in the gastrointestinal tract. GISTs constitute 1%-3% of all malignant gastrointestinal tumors and the majority of cases are sporadic[1]. Familial GIST is an extremely rare autosomal dominant condition which is predominantly due to germline gain-of-function mutations of KIT and to a lesser extent of PDGFRA[2]. Diffuse proliferation of interstitial cells of Cajal (ICCs) in the myenteric plexus layer of the intestine has been described in patients with familial GISTs[3].
Familial GISTs, associated with germline gain-of-function mutations of KIT have been described in 35 families[2,4,5]. Somatic KIT mutations are reported in approximately 60% of all sporadic GISTs, and almost 95% of all mutations are located in exon 11[6]. In patients with familial GISTs, most germline mutations are also located in exon 11[4]. Familial GISTs with exon 13 mutations are extremely rare, the range of frequency of exon 13 mutations is between 0.8% to 4.1%. Seven families with a germline gain-of-function mutation of KIT in exon 13 have been reported to-date[7-12].
Surgery is the primary treatment for localized GISTs. Imatinib mesylate, which is a tyrosine kinase inhibitor, is administered as adjuvant therapy for high-risk groups after the operation or as neoadjuvant therapy for the management of advanced GISTs which are not candidates for surgery at initial diagnosis[13,14]. There are only a few reports describing the response to imatinib in familial GISTs confirming it as a promising therapeutic option[4,5,10].
We here describe clinical, imaging, pathological and genetic findings of a family with four affected members, grandmother, his son and two grand-sons having a germline gain-of-function mutation of KIT in exon 13 and discuss the imatinib treatment surveillance outcomes towards disease management.
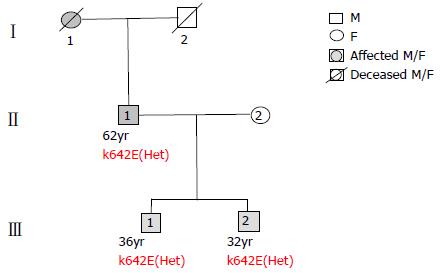
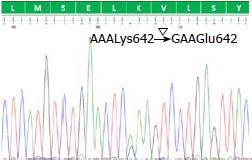
We describe a family, father and two sons, with multiple GISTs. Grandmother was reported as being operated at the age of 62 and staged as advanced GIST. Genetic analysis was carried out on DNA obtained from peripheral blood samples from three affected individuals, and there was no DNA available from the grandmother (Figure 1). Sequence analysis of KIT gene (RefSeq ID: NM_000222.2; NP_000213.1) revealed a heterozygous exon 13 c.1924A>G (p.Lys642Glu; p.K642E) gain-of-function mutation in all three cases (Figure 2). This result was in concordance with the familial GIST diagnosis.
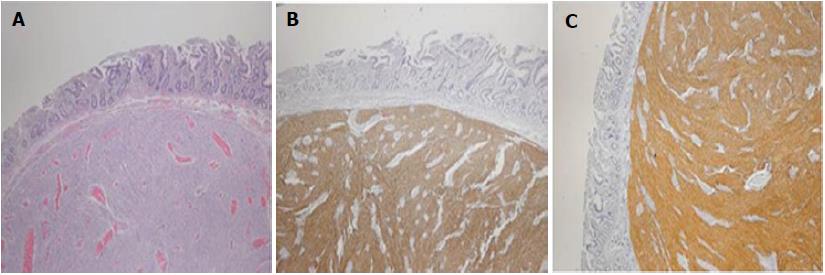
All three had been operated and found to have low risk, grade 1 multiple GISTs (T2N0M0). Immunohistochemical studies of the tumors showed strong positivity for CD117 (c-kit) (Figure 3). The father and older sibling were treated with imatinib for rest tumors after resection and showed a partial response to treatment.
Patient 1 (III-1; 36 years)
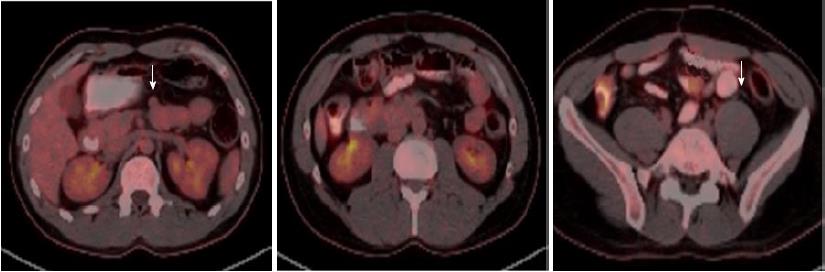
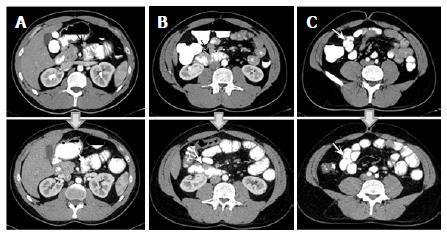
The patient has been hospitalized due to massive GIS bleeding at the age of 20 and was operated at the age of 27 after an intensive rectal bleeding. Mesenteric angiography showed bleeding from proximal jejunal branches and tumoral staining. The bleeding branches embolized. Abdominal computed tomography (CT) revealed proximal jejunal wall thickening and nodular solid lesions with 2.5 cm in diameter. Laparoscopic jejunal resection was made and histopathological examination showed low risk grade 1 GIST with strong positivity for CD117(c-kit) (pT2N0M0). Postoperative follow-up PET-CT demonstrated normal findings. He was, thereafter, treated with imatinib (400 mg/d) for five years due to residual multiple, milimetric GISTs and annual follow-up PET-CT showed no recurrence during that period. Imatinib treatment was terminated upon patient’s request, end of five years treatment, in 2012. A recent follow-up PET-CT scan identified two nodular lesions in jejunum, 2 cm (SUVmax: 4.69) and 1.5 cm (SUVmax: 1.68) in diameters, which were consistent with GIST recurrence (Figure 4). Abdominal CT revealed multiple duodenal, jejunal and ileal contrast enhanced solid, nodular lesions with maximum 3 cm in diameter. The patient rejected the operation and preferred the re-treatment of imatinib (400 mg/d). A partial response was obtained again in the following 3 mo (Figure 5). The proband had multiple nevi on palms and soles which showed regression after the initiation of the treatment and had hypopigmentation of skin in general.
Patient 2 (III-2; 32 years)
He was referred due to abdominal distension and dysphagia at the age of 32. Gastroduodenal endoscopic examination and endoscopic ultrasonography (EUS) showed a gastric submucosal 1.4 cm tumor in diameter on the small curvature of prepyloric antrum. Colonoscopy showed normal findings. 18F-FDG PET-CT revealed two lesions, one at the prepyloric antrum 1.5 cm in diameter with a SUVmax: 5.0 and another at jejunum 2.2 cm in diameter with a SUVmax: 5.39. Abdominal CT showed multiple solid, contrast enhanced mass lesions maximum 3.5 cm in diameter located at the jejunum in addition to the prepyloric antral mass. Partial jejunal resection, multiple wedge resection of stomach and jejunum was performed. Histopathological examination showed low risk grade 1, multifocal masses, two, in stomach at 2.5 cm in diameter and multiple in jejunum, more than 20 with a maximum diameter of 4 cm). Tumors showed strong positivity for CD117 (c-kit) (pT2N0M0). The patient opted for no adjuvant therapy and decided to be followed up by routine annual PET-CT.
Patient 3 (III-3; 62 years)
The father had been treated for gastrointestinal bleeding at the age of 18 and preoperatively diagnosed as GIST at the age of 25. He had Billroth operation at the age of 28 and had bleeding episodes thereafter and is on imatinib for the past eight years. At the age of 53, abdominal CT revealed multiple solid lesions with heterogenous contrast enhancement at the distal duodenum, max 5.2 cm in diameter, proximal and middle jejunum, max 5.0 cm in diameter. Three similar solid lesions were further identified at the esophageal wall of the esophago-gastric junction level (2.0 cm in diameter), at the colonic wall of the splenic flexura level (1.2 cm in diameter) and of the rectosigmoid junction level (1.0 cm in diameter), respectively. There was no additional pathologic finding in the liver, peritoneal or retroperitoneal areas. Partial jejunal resection and multiple wedge resections from the esophagus, colon and rectum were performed. Histopathological examination showed low risk grade 1 multifocal GIST with strong positive CD117 (c-kit) (pT2N0M0). After the operation, the patient has been treated with imatinib (400 mg/d) for 8 years due to residual multiple, milimetric GISTs without recurrence on annual follow-up PET-CT.
We present an extremely rare condition of autosomal dominant familial GIST with heterozygous c.1924A>G (p.Lys642Glu; p.K642E) germline KIT mutation in exon 13 (K642E). All three patients had been operated and two of them were treated with imatinib due to residual multiple, milimetric GISTs to which they all showed partial response.
Surgery is the initial treatment for primary and localized GISTs, targeting complete resection with macroscopic and microscopic negative margins and functional preservation by wedge resection, whenever applicable. The management of a positive microscopic margin after macroscopic complete resection is not well defined, and options may include re-excision, watchful waiting, and adjuvant imatinib therapy. Imatinib mesylate is a first-line standard therapy for inoperable, metastatic, or recurrent GISTs. It is also indicated as adjuvant treatment for intermediate or high risk group of GISTs[14].
Only about half of the patients with sporadic GIST respond to imatinib treatment; 12%-14% show primary resistance to imatinib, and 40%-50% experience secondary resistance and disease progression within 2-3 years from the beginning of therapy[5]. With regard to familial GISTs, there are only 12 reports on the use of imatinib in 24 patients with KIT germline mutations[8,10,15-24].
The effect of imatinib on the inhibition of KIT activation is dependent on the site of the mutation within the KIT gene[5,25]. Previous studies described that the best responses were obtained in GISTs with exon 11 mutations with a daily dose of 400 mg while a daily double dose of 800 mg is required in cases with exon 9 mutation[5,26,27]. Clinical data on the effect of imatinib against sporadic GISTs with exon 13 mutations are limited. However, it has been proven that imatinib is effective in controlling the progression of sporadic GISTs in patients with K642E mutation. In vitro assays also showed that activation of K642E is inhibited by imatinib[26,27].
Several research and follow-up studies has shown that twelve exon 11 positive patients on 400 mg/d imatinib had stable outcome, lasting from 12 to 58 mo[10,19-21,23]. Three out of four exon 17 mutated patients[22,24], two out of three exon 13 mutated patients[8,10] and one exon 8 mutated patient[15] also reported to be stable after imatinib treatment initiation.
In our family, the father and the older son were treated with imatinib (400 mg/d) without recurrence. There were no signs of recurrence in the father. However, the older son showed recurrence four years after the cessation of imatinib treatment upon patient’s request. Imatinib was re-administered with a daily dose of 400 mg and CT scan showed a significant decrease in the tumor size, after three months of the treatment.
We conclude that, KIT mutation analysis is advisable prior to initiation of imatinib treatment, as it can help predicting the tumor response. However, data on the role of imatinib in familial GISTs is still limited. We believe that case studies will contribute to our understanding the significance of mutation analysis in regard to the drug dosage, duration of treatment, drug response and follow-up studies of imatinib therapy in familial GISTs. The prognostic comparison of the outcome of imatinib treatment in sporadic GISTs and familial GISTs may play a role in defining the underlying mechanisms and pathways.
A family, a father (62-year-old) and two sons (32 and 36 years old) having multiple gastrointestinal stromal tumor (GIST) are described.
Massive GIS hemorrhage in the father and his older son, abdominal distension and dysphagia in the younger son.
Gastric varices, Mallory-Weiss tear, neoplasm and hemorrhagic gastritis in upper GIS; bleeding, diverticulosis, angiodysplasia, colitis (infectious or ischemic), inflammatory bowel disease, colon cancer in lower GIS bleeding. Dysphagia can be seen in mechanical obstruction or neuromuscular motility disorders.
All labs were within normal limits.
Imaging computed tomography showed multiple, submucosal, solid masses in 2-5 cm sizes in the upper and lower gastrointestinal tract. 18F-FDG PET-CT revealed high FDG activity (SUVmax 5.0-5.4) in the solid lesions.
Immunohistochemistry for DOG1 and c-kit showed immun activity in the tumor cell. Sequence analysis of KIT gene revealed a heterozygous exon 13 c.1924A>G gain-of-function mutation in all three cases in concordance with the familial GIST diagnosis.
Exon 13 germline mutations are extremely rare amongst familial GISTs and seven families with a germline mutation have been reported to date. Moreover, there are only a few reports describing the response to imatinib in familial GISTs confirming it as a promising therapeutic option.
Familial gastrointestinal stromal tumor (GIST) is a rare autosomal dominant disorder associated with mutations in the KIT gene in the majority of cases presents multiple GIST. Although surgery is the primary treatment for localized GISTs, imatinib mesylate is used as adjuvant or neoadjuvant therapy in high risk or advanced GIST groups.
We conclude that KIT mutation analysis is advisable prior to initiation of imatinib treatment in familial GIST, as it can help predicting the tumor response. We believe that case studies will contribute to our understanding the significance of mutation analysis in regard to the drug dosage, duration of treatment, drug response and follow-up studies of imatinib therapy in familial GISTs.
The authors describe three members of a family treated with surgery and imatinib due to a familiar GIST with a rare mutation. The role of imatinib in this rare familiar settings is not completely known so far. The paper is interesting, addresses a novel topic and adds further knowledge to literature.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Vallicelli C S- Editor: Kong JX L- Editor: A E- Editor: Zhao LM
| 1. | Cassier PA, Ducimetière F, Lurkin A, Ranchère-Vince D, Scoazec JY, Bringuier PP, Decouvelaere AV, Méeus P, Cellier D, Blay JY. A prospective epidemiological study of new incident GISTs during two consecutive years in Rhône Alpes region: incidence and molecular distribution of GIST in a European region. Br J Cancer. 2010;103:165-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Hirota S, Nishida T, Isozaki K, Taniguchi M, Nishikawa K, Ohashi A, Takabayashi A, Obayashi T, Okuno T, Kinoshita K. Familial gastrointestinal stromal tumors associated with dysphagia and novel type germline mutation of KIT gene. Gastroenterology. 2002;122:1493-1499. [PubMed] [Cited in This Article: ] |
| 3. | Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577-580. [PubMed] [Cited in This Article: ] |
| 4. | Bamba S, Hirota S, Inatomi O, Ban H, Nishimura T, Shioya M, Imaeda H, Nishida A, Sasaki M, Murata S. Familial and multiple gastrointestinal stromal tumors with fair response to a half-dose of imatinib. Intern Med. 2015;54:759-764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Gupta D, Chandrashekar L, Larizza L, Colombo EA, Fontana L, Gervasini C, Thappa DM, Rajappa M, Rajendiran KS, Sreenath GS. Familial gastrointestinal stromal tumors, lentigines, and café-au-lait macules associated with germline c-kit mutation treated with imatinib. Int J Dermatol. 2017;56:195-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Hirota S, Ohashi A, Nishida T, Isozaki K, Kinoshita K, Shinomura Y, Kitamura Y. Gain-of-function mutations of platelet-derived growth factor receptor alpha gene in gastrointestinal stromal tumors. Gastroenterology. 2003;125:660-667. [PubMed] [Cited in This Article: ] |
| 7. | Yamanoi K, Higuchi K, Kishimoto H, Nishida Y, Nakamura M, Sudoh M, Hirota S. Multiple gastrointestinal stromal tumors with novel germline c-kit gene mutation, K642T, at exon 13. Hum Pathol. 2014;45:884-888. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Bachet JB, Landi B, Laurent-Puig P, Italiano A, Le Cesne A, Lévy P, Safar V, Duffaud F, Blay JY, Emile JF. Diagnosis, prognosis and treatment of patients with gastrointestinal stromal tumour (GIST) and germline mutation of KIT exon 13. Eur J Cancer. 2013;49:2531-2541. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Isozaki K, Terris B, Belghiti J, Schiffmann S, Hirota S, Vanderwinden JM. Germline-activating mutation in the kinase domain of KIT gene in familial gastrointestinal stromal tumors. Am J Pathol. 2000;157:1581-1585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 181] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Graham J, Debiec-Rychter M, Corless CL, Reid R, Davidson R, White JD. Imatinib in the management of multiple gastrointestinal stromal tumors associated with a germline KIT K642E mutation. Arch Pathol Lab Med. 2007;131:1393-1396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 11. | Vilain RE, Dudding T, Braye SG, Groombridge C, Meldrum C, Spigelman AD, Ackland S, Ashman L, Scott RJ. Can a familial gastrointestinal tumour syndrome be allelic with Waardenburg syndrome? Clin Genet. 2011;79:554-560. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Peña-Irún A, Villa-Puente M, García-Espinosa R, Cavadas-López A. [Familial gastrointestinal stroma tumor due to mutation in exon 13 (K642E) of the KIT gene]. Med Clin (Barc). 2012;139:512-513. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Wadt K, Andersen MK, Hansen TV, Gerdes AM. [A new genetic diagnosis of familiar gastrointestinal stromal tumour]. Ugeskr Laeger. 2012;174:1462-1464. [PubMed] [Cited in This Article: ] |
| 14. | Nishida T, Blay JY, Hirota S, Kitagawa Y, Kang YK. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer. 2016;19:3-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 284] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 15. | Speight RA, Nicolle A, Needham SJ, Verrill MW, Bryon J, Panter S. Rare, germline mutation of KIT with imatinib-resistant multiple GI stromal tumors and mastocytosis. J Clin Oncol. 2013;31:e245-e247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Adela Avila S, Peñaloza J, González F, Abdo I, Rainville I, Root E, Carrero Valenzuela RD, Garber J. Dysphagia, melanosis, gastrointestinal stromal tumors and a germinal mutation of the KIT gene in an Argentine family. Acta Gastroenterol Latinoam. 2014;44:9-15. [PubMed] [Cited in This Article: ] |
| 17. | Jones DH, Caracciolo JT, Hodul PJ, Strosberg JR, Coppola D, Bui MM. Familial gastrointestinal stromal tumor syndrome: report of 2 cases with KIT exon 11 mutation. Cancer Control. 2015;22:102-108. [PubMed] [Cited in This Article: ] |
| 18. | Wozniak A, Floris G, Debiec-Rychter M, Sciot R, Schöffski P. Implications of mutational analysis for the management of patients with gastrointestinal stromal tumors and the application of targeted therapies. Cancer Invest. 2010;28:839-848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Lasota J, Miettinen M. A new familial GIST identified. Am J Surg Pathol. 2006;30:1342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Kleinbaum EP, Lazar AJ, Tamborini E, Mcauliffe JC, Sylvestre PB, Sunnenberg TD, Strong L, Chen LL, Choi H, Benjamin RS. Clinical, histopathologic, molecular and therapeutic findings in a large kindred with gastrointestinal stromal tumor. Int J Cancer. 2008;122:711-718. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Woźniak A, Rutkowski P, Sciot R, Ruka W, Michej W, Debiec-Rychter M. Rectal gastrointestinal stromal tumors associated with a novel germline KIT mutation. Int J Cancer. 2008;122:2160-2164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Thalheimer A, Schlemmer M, Bueter M, Merkelbach-Bruse S, Schildhaus HU, Buettner R, Hartung E, Thiede A, Meyer D, Fein M. Familial gastrointestinal stromal tumors caused by the novel KIT exon 17 germline mutation N822Y. Am J Surg Pathol. 2008;32:1560-1565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Campbell T, Felsten L, Moore J. Disappearance of lentigines in a patient receiving imatinib treatment for familial gastrointestinal stromal tumor syndrome. Arch Dermatol. 2009;145:1313-1316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Veiga I, Silva M, Vieira J, Pinto C, Pinheiro M, Torres L, Soares M, Santos L, Duarte H, Bastos AL. Hereditary gastrointestinal stromal tumors sharing the KIT Exon 17 germline mutation p.Asp820Tyr develop through different cytogenetic progression pathways. Genes Chromosomes Cancer. 2010;49:91-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Ashman LK, Griffith R. Therapeutic targeting of c-KIT in cancer. Expert Opin Investig Drugs. 2013;22:103-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 26. | Heinrich MC, Corless CL, Demetri GD, Blanke CD, von Mehren M, Joensuu H, McGreevey LS, Chen CJ, Van den Abbeele AD, Druker BJ. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21:4342-4349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1782] [Cited by in F6Publishing: 1599] [Article Influence: 76.1] [Reference Citation Analysis (0)] |
| 27. | Debiec-Rychter M, Sciot R, Le Cesne A, Schlemmer M, Hohenberger P, van Oosterom AT, Blay JY, Leyvraz S, Stul M, Casali PG. KIT mutations and dose selection for imatinib in patients with advanced gastrointestinal stromal tumours. Eur J Cancer. 2006;42:1093-1103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 640] [Cited by in F6Publishing: 613] [Article Influence: 34.1] [Reference Citation Analysis (0)] |