Published online Apr 28, 2013. doi: 10.4329/wjr.v5.i4.187
Revised: December 18, 2012
Accepted: January 14, 2013
Published online: April 28, 2013
Angiolipoma of the spine is a benign neoplasm consisting of both mature fatty tissue and abnormal vascular elements, and usually presents with a slow progressive clinical course. Our patient presented with bilateral lower extremity weakness and chest-back numbness. Physical examination revealed adipose elements superficial hypesthesia below the T5 level and analgesia below the T6 level. Magnetic resonance imaging (MRI) scan showed an avidly and heterogeneously enhancing mass which was located in the posterior epidural space. Compression of the thoracic cord by the fusiform mass was seen between T3-T4. During the operation, a flesh pink vascular mass (4.7 cm × 1.0 cm × 1.0 cm) with obscure margin and strong but pliable texture was found in the posterior epidural space extending from T3 to T4. There was no infiltration of the dura or the adjacent bony spine. Histopathological study of the surgical specimen showed a typical angiolipoma. We review the previously documented cases of spinal extradural angiolipomas performed with MRI.
- Citation: Meng J, Du Y, Yang HF, Hu FB, Huang YY, Li B, Zee CS. Thoracic epidural angiolipoma: A case report and review of the literature. World J Radiol 2013; 5(4): 187-192
- URL: https://www.wjgnet.com/1949-8470/full/v5/i4/187.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i4.187
Angiolipoma of the spine is a benign neoplasm consisting of mature fatty tissue and abnormal vascular elements, predominantly in middle-aged, female patients and situated mainly in the mid-thoracic region. There are only 142 cases with spinal extradural angiolipoma reported to date[1]. They account for about 0.14%-1.2% of all spinal axis tumors and 2%-3% of spinal epidural tumors[2]. We report another case of spinal angiolipoma in an elderly patient which showed a typical appearance on magnetic resonance imaging (MRI). The pathology, clinical features, diagnostic evaluation, and treatment of spinal angiolipoma were reviewed.
A 63-year-old man presented with a 1.0-year history of bilateral lower extremities numbness and a 6-mo history of difficulty in urination. Concurrently, he noticed bilateral lower extremity weakness and chest-back numbness one month prior to admission. Physical examination revealed a superficial hypesthesia below the T5 level and analgesia below the T6 level, varicose vein of the left lower limb, decreased muscle strength and increased muscle tension, as well as hyperreflexia of the low extremities.
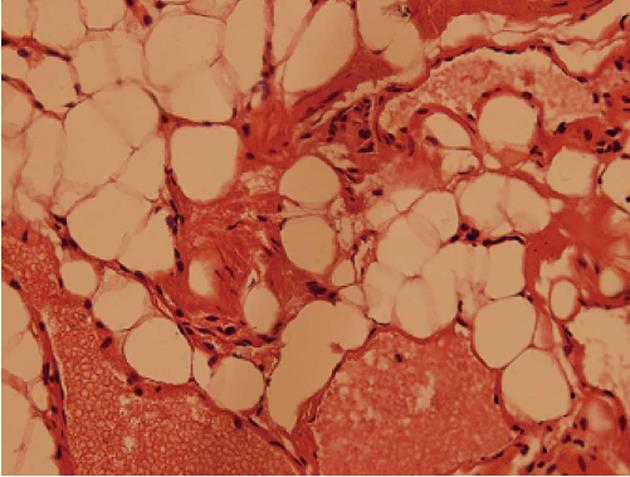
A MRI scan showed a fusiform posterior epidural mass compressing the thoracic cord over two vertebral body segments between T3-T4. The mass was inhomogeneous, isointense on T1-weighted images (Figure 1A), slightly hyperintense on T2-weighted image (Figure 1B), hyperintense on fat-saturated T2-weighted images (Figure 1C) and inhomogeneously enhanced on fat-saturated T1-weighted image (Figure 1D). The lesion’s long axis paralleled the long axis of the spinal cord, tapering at both ends. On the axial T1 weighted images, a crack like low signal between spinal cord and the lesion (Figure 1E) which is the typical appearance of the case can be seen. A laminectomy with gross total resection of the lesion was performed. During the operation, a flesh pink vascular mass with obscure margin and strong but pliable texture was found in the posterior epidural space from T3 to T4. There was no infiltration of the dura or the vertebrae. Histopathological study of the surgical specimen showed a typical angiolipoma (Figure 2) composed of mature fat cells and abnormal vascular elements.
Berenbruch et al[3] reported the first case of spinal angiolipoma (AGL) in 1890 in about a 16-year-old with numerous cutaneous lipomas, while the first pathological report was made by Howard et al[4] in 1960. It is composed of varying proportions of mature fat cells and abnormal capillary, sinusoidal, venous or arterial vascular elements. Subsequently, AGL has been further subdivided by Lin et al[5] into two categories: noninfiltrating and infiltrating. The former is encapsulated and well demarcated, not infiltrating the dura or the vertebrae, often in the dorsal aspect of the spinal canal. Whereas, the latter is very rare, entirely or partially unencapsulated, situated in the anterior or anterolateral aspect of the spinal canal with ill-defined margins and infiltrates the surrounding tissues. Our case is type 1, unencapsulated, but not infiltrating the dura or the vertebrae.
The origin and pathogenesis of AGLs is unknown. Histologically, the lesion is mainly composed of mature fat cells and blood vessels. The fat composition is similar to the general adipose tissue and the vascular components consist of capillaries, sinusoids, thin-walled blood vessels or thick-walled blood vessels with smooth muscle and occasionally well-developed small arteries can be seen. A diagnostic feature is the presence of fibrin thrombi in the lumen of capillaries. Degenerative changes (i.e., myxoid change, hyalinization and fibrosis) may be present in some longstanding cases[6]. Traditionally, AGL is considered a subtype of spinal lipomas, but more recent clinicalpathological studies[7] considered them as a specific entity different from pure lipomas because they were not associated with spinal dysraphism. AGLs usually contain a much greater number of mature, thick-walled vessels than liposarcomas[5]. Angiomyolipomas are a variant of angiolipoma characterized by vascular smooth muscle proliferation extending into the surrounding fat[8].
The clinical presentation of spinal AGLs is not different from any other benign epidural tumor. We found that the AGLs have been reported to occur predominantly in women (female:male = 22:17; Table 1) and are more common in the fifth decade[9]. In our review, age of presentation ranged from 4 to 81 years old, with mean age at presentation of 46 years. The mode of onset may be acute, subacute or chronic, may show radicular, paraplegic, progressive or remitting-relapsing clinical types. The most common initial symptoms are back pain, lower extremity numbness or paresthesias and leg weakness (Table 1), and progressive neurological symptoms secondary to spinal cord compression may develop later on. The symptoms usually evolve over a period of months to years, but the progression can be accelerated by vascular steal phenomena, vascular engorgement, venous stasis with thrombosis, bleeding into the tumor and rarely intratumoral abscess[10]. Bleeding is extremely rare in angiolipomas. Akhaddar et al[10] reported a case presenting with spontaneous bleeding causing acute paraplegia. Like other vascular lesions, onset or deterioration may occur during pregnancy[11] or with weight gain. This was not the case in our patient.
| Ref. | Age (yr) | Sex | Clinical presentation (signs/duration) | MRI finding (T1/T2, post-contrast) | Pathological finding |
| Turgut et al[1] | 26 | F | Acute onset of paraplegia, in week 31 of pregnancy | T1 and T2: Hyperintense | Angiolipoma |
| Diyora et al[6] | 20 | M | Upper abdominal pain/6 mo, and lower limb weakness/1 wk | Isointense/hyperintense; enhancement | Angiolipoma |
| Turgut et al[9] | 54 | F | Weakness, urinary incontinence, and constipation/5 mo | Very hyperintense/nearly isointense | Angiolipoma |
| Akhaddar et al[10] | 47 | M | Sudden back pain, paresthesia and complete neurological palsy/a few-minutes period | Isointense/slightly hyperintense; no gadolinium enhancement | Angiolipoma |
| Park et al[11] | 74 | F | Lower back pain/5 mo | Low signal intensity/iso-or high signal intensity; High signal intensity after gadolinium injection | Angiolipoma |
| Provenzale et al[12] | 38 | F | Lower back pain/3 yr | Moderately hypointense/nearly isointense; Slightly inhomogeneous enhancement | Angiolipoma |
| 61 | F | Paraparesis/2 yr | T1: Slightly hypointense; Inhomogeneous enhancement | Angiolipoma | |
| 42 | F | Midthoracic back pain/2 yr | Iso-hypo-intense/nearly isointense | Angiolipoma | |
| Leu et al[15] | 81 | M | Unstable gait, and lower limbs weakness/2 wk | Inhomogeneous hypointensity/high signal intensity; Strongly enhanced | Angiolipoma |
| Yen et al[16] | 71 | M | Acute paraparesis | T1: Homogeneously hyphointense | Angiolipoma |
| Fourney et al[17] | 46 | F | Feet and legs numbness/4 yr | Homogeneously hyperintense/hyperintense; enhanced | Angiolipoma |
| Shibata et al[18] | 38 | F | Paraparesis/6 mo | T1 and T2: High-intensity signal | Angiolipoma |
| Bouramas et al[19] | 27 | F | Diminution sensation/2 mo | Heterogeneous signal intensity/high signal intensity | Angiolipoma |
| Boockvar et al[20] | 34 | F | Interscapular back pain/5 mo | Hyperintense/hyperintense; Enhanced homogeneously | Angiolipoma |
| Amlashi et al[21] | 36 | M | Back pain, and both legs weakness | T1 and T2: Homogenous, hyperintense | Angiolipoma |
| Garg et al[22] | 12 | F | Paraparesis/the previous year | Hyperintensity/hyperintensity; Heterogeneous contrast enhancement | Angiolipoma |
| 26 | M | Paraparesis/3 mo | T1 and T2: Homogeneous high signal intensity; contrast enhancement | Angiolipoma | |
| 28 | M | Bowel and bladder impairment, paraparesis/the previous year | T1 and T2: Homogeneously hyperintense | Angiolipoma | |
| do Souto et al[23] | 46 | F | Low back pain/10 yr | Isointense/hyperintense; Homogeneous and intense enhancement | Angiolipoma |
| Rabin et al[24] | 47 | M | Legs paresthesias/6 mo | T1 and T2: High signal | Angiolipoma |
| Samdani et al[25] | 49 | F | Back pain, lower extremity weakness/3 yr | Intermediate-signal intensity/hyperintensity; homogenous contrast enhancement | Angiolipoma |
| Dogan et al[26] | 50 | F | Lumbosciatalgia/2 yr | Isointense/hyperintense; Homogeneous enhancement | Angiolipoma |
| 36 | M | Low back pain/8 mo | Isointense/hyperintense; Homogeneous enhancement | Angiolipoma | |
| Guzey et al[27] | 41 | F | Low back and leg pain/18 mo | Iso-hyperintense/hyperintense; homogeneously enhanced | Angiolipoma |
| Hungs et al[28] | 52 | Thoracolumbar pain/1.5 yr | T1: Hyperintense; Diffusely intense enhancement | Angiolipoma | |
| Sankaran et al[29] | 77 | M | Paraparesis/48 h | Isointense/inhomogeneous hyperintensity; Inhomogeneous enhancement | Angiolipoma |
| Weill et al[33] | 46 | F | Paraparesis/1 yr | Iso-hypointensities/mixed signal | Angiolipoma |
| 27 | F | Right leg weak/several week | Very-hyperintense/mixed-signal; Inhomogeneous enhancement | Angiolipoma | |
| Gelabert-González et al[34] | 16 | M | Low back pain/6 mo | Slightly inhomogeneous/heterogeneously hypointense | Angiolipoma |
| 45 | Both feet numbness, and leg weakness/6 mo | T1 and T2: Moderately hyperintense relative to spinal cord | Angiolipoma | ||
| Sakaida et al[36] | 72 | M | Legs abnormal sensation/4 mo | Inhomogeneous enhancement | Angiolipoma |
| Oge et al[37] | 72 | M | Paraparesis/4 d | T1: Hyperintense | Angiolipoma |
| al-Anazi et al[38] | 38 | F | Both feet numbness, 8-mo pregnant housewife | T1: Hyperintense | Angiolipoma |
| Gelabert-González et al[39] | 4 | M | Back pain, and both legs weakness/2 d | T1: Mixed-intensity | Angiolipoma |
| Rocchi et al[40] | 60 | M | Lumbosciatalgia/2 yr | T1: Signal intensity similar to that of the subcutaneous adipose tissue | Angiolipoma |
| 54 | F | Lumbosciatalgia/12 mo | Homogeneous contrast enhancement | Angiolipoma | |
| Chotai et al[41] | 69 | M | Back pain, paresthesias, and hypesthesia/5 yr | T1: Slightly high intensity with areas of hypointensity; Inhomogeneous enhancement | Angiolipoma |
| Konya et al[42] | 60 | F | Low back pain/6 mo | T1: Hyperintense; marked enhancement | Angiolipoma |
| Current study | 63 | M | Lower extremities numbness/1 yr | Isointense/slightly hyperintense; Obviously inhomogeneous enhancement | Angiolipoma |
The appearance of angiolipomas correlated well with their histological composition, so the AGL is often misdiagnosed. In the majority of cases, plain vertebral radiography demonstrates normalities. If causing adjacent bone destruction, AGL must be differentiated from epidural metastases. The metastasis is the most common malignancy of epidural space, which is typically an irregular soft tissue mass with adjacent bone destruction. Trabeculation of the affected vertebral body and erosion of the pedicle may be identified in tumors infiltrating bone[12,13]. Computed tomography (CT) usually demonstrates a hypodense lesion with fat density, provides information on the degree of bony involvement[7] and also can demonstrate variable degree of enhancement after contrast injection. However, CT may not be specific for spinal epidural angiolipomas and could be misleading in some cases[14].
MRI is the imaging modality of choice for detecting angiolipomas. MRI was performed in approximately 70 cases (since 1988), but there were only 39 cases with adequate data (Table 1). The angiolipomas appear as an isointense or hyperintense extradural mass on T1-weighted images, but occasionally a hypointense mass[11,12,15,16] may be seen. The degree of central hypointensity on T1-weighted images is predictive of the degree. On T2-weighted images, the tumors have variable signal intensity, with a predominance of hyperintensity[10,15,17-29]. Significant heterogeneity in the imaging studies is attributed to the variable vascular and adipose elements of the tumor[12]. In our case, the tumor is isointense with fewer areas of hypointensity on T1-weighted images and hyperintense on fat-saturated T2-weighted images. There is slightly heterogeneity which is consistent with few vascular elements, less adipose elements of the tumor. Gadolinium enhancement reflects the vascularity of these tumors. In our case, the lesion was strongly enhanced after contrast injection.
Spinal hemangiomas also present as mixed signal intensity lesions on MRI, although the hyperintensity on T2-weighted images is more striking. Suppression of high signal intensity on fat-saturated T1-weighted images may be very useful for distinguishing between angiolipomas and melanomas or sub-acute hemorrhage. Most spinal angiolipomas show enhancement with contrast medium which better defines the borders of the tumor[30]. In our case the tumor has an obscure margin, while after contrast injection its border becomes very clear. Contrast enhancement allows for differential diagnosis between spinal angiolipoma and extradural lipomatosis as the latter does not show contrast enhancement[31]. Unlike some other vascular tumors (e.g., glomus jugulare tumors), angiolipomas do not typically contain vascular flow voids on magnetic resonance images[32,33], there is only one case containing vascular flow voids in the literature. This is probably because of the preponderance of capillaries and venous channels in angiolipomas, which distinguish them from malformations with arteriovenous shunting and from those lesions with predominantly arteriolar circulation both of which produce fast flow, seen on MRI as flow-void phenomena. In our case, there is no flow-void phenomena which is identical with those reported in literature.
There is no clear consensus as to what combination of therapy is optimal for spinal AGL. The biological behavior of the infiltrating and noninfiltrating AGL implicates a different treatment approach[18]. To date, the main treatment is total surgical resection. Most extradural non-infiltrative tumors are amenable to complete excision via laminectomy. Total removal of infiltrating angiolipomas that often involve the vertebral body has been recommended using the anterolateral approach and stabilization of the affected vertebrae is desirable[9]. Extent of tumor resection in infiltrative angiolipoma has been debated, but most authors agree that risking neurological function is not necessary with aggressive attempts to attain gross total removal[9,17,34]. In spite of vascularization of the tumor, profuse hemorrhage has rarely been reported[10]. Although complete removal of the lesion is not always easily achievable, recurrence is exceptional[35]. In case of recurring or infiltrative SALs, wider resection followed by radiotherapy should be considered[17]. Most patients have a good prognosis because the tumors are usually slow growing and do not undergo malignant transformation. In our case, the patient’s clinical symptoms improved postoperatively. There are no signs of tumor recurrence and no neurological deficit during the two year follow-up period.
In conclusion, AGL is a rare but benign clinicopathological entity which is composed of fatty tissue and vascular elements. It grows in a spindle shape along the spinal canal, without associated malformations. The postoperative outcome after surgical management of this lesion is favorable. Accurate pre-operative diagnosis is very important. MRI typically shows an iso- to hyperintense mass on T1 weighted images and hyperintense mass without flow voids on T2 weighted images in the posterior epidural space. Following intravenous injection of contrast material, avid inhomogeneous enhancement is seen.
P- Reviewers Lokhande PV, Kasai Y S- Editor Song XX L- Editor Roemmele A E- Editor Xiong L
| 1. | Turgut M. Thoracic epidural angiolipoma with extraspinal extension. Neurol India. 2011;59:654; author reply 654-655. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Alter M. Statistical aspect of spinal cord tumor. Vinken PJ, Bruyn GW, editors. Handbook of Clinical Neurology. New York, NY: North Holland Publishing Co 1975; 1–22. [Cited in This Article: ] |
| 3. | Berenbruch K. Ein fall von multiplen angiolipomen konnbintert mit eniem angiom des rukenmarks. Tubingen. 1890;. [Cited in This Article: ] |
| 4. | Howard WR, Helwig FH. Angiolipoma. Arch Dermatol. 1980;82:924-931. [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 279] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 5. | Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974;34:720-727. [PubMed] [Cited in This Article: ] |
| 6. | Diyora B, Nayak N, Kukreja S, Kamble H, Sharma A. Thoracic epidural angiolipoma with bilateral multilevel extraspinal extensions: a rare entity. Neurol India. 2011;59:134-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Matsushima K, Shinohara Y, Yamamoto M, Tanigaki T, Ikeda A, Satoh O. Spinal extradural angiolipoma: MR and CT diagnosis. J Comput Assist Tomogr. 1987;11:1104-1106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Kujas M, Lopes M, Lalam TF, Fohanno D, Poirier J. Infiltrating extradural spinal angiolipoma. Clin Neuropathol. 1999;18:93-98. [PubMed] [Cited in This Article: ] |
| 9. | Turgut M. Spinal angiolipomas: report of a case and review of the cases published since the discovery of the tumour in 1890. Br J Neurosurg. 1999;13:30-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Akhaddar A, Albouzidi A, Elmostarchid B, Gazzaz M, Boucetta M. Sudden onset of paraplegia caused by hemorrhagic spinal epidural angiolipoma. A case report. Eur Spine J. 2008;17 Suppl 2:S296-S298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Park JH, Jeon SR, Rhim SC, Roh SW. Lumbar spinal extradural angiolipoma: case report and review of the literature. J Korean Neurosurg Soc. 2008;44:265-267. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Provenzale JM, McLendon RE. Spinal angiolipomas: MR features. AJNR Am J Neuroradiol. 1996;17:713-719. [PubMed] [Cited in This Article: ] |
| 13. | Rivkind A, Margulies JY, Lebensart P, Sherman Y, Robin GC. Anterior approach for removal of spinal angiolipoma. A case report. Spine (Phila Pa 1976). 1986;11:623-625. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Pagni CA, Canavero S. Spinal epidural angiolipoma: rare or unreported? Neurosurgery. 1992;31:758-64; discussion 764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Leu NH, Chen CY, Shy CG, Lu CY, Wu CS, Chen DC, Guo TH. MR imaging of an infiltrating spinal epidural angiolipoma. AJNR Am J Neuroradiol. 2003;24:1008-1011. [PubMed] [Cited in This Article: ] |
| 16. | Yen HL, Tsai SC, Liu SM. Infiltrating spinal angiolipoma. J Clin Neurosci. 2008;15:1170-1173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Fourney DR, Tong KA, Macaulay RJ, Griebel RW. Spinal angiolipoma. Can J Neurol Sci. 2001;28:82-88. [PubMed] [Cited in This Article: ] |
| 18. | Shibata Y, Sugimoto K, Matsuki T, Nose T. Thoracic epidural angiolipoma--case report. Neurol Med Chir (Tokyo). 1993;33:316-319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Bouramas D, Korres DS, Roussos L, Mantzilas T, Anagnostopoulos D. Spinal extradural angiolipoma. J Spinal Disord. 1995;8:324-327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Boockvar JA, Black K, Malik S, Stanek A, Tracey KJ. Subacute paraparesis induced by venous thrombosis of a spinal angiolipoma: a case report. Spine (Phila Pa 1976). 1997;22:2304-2308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Amlashi SF, Morandi X, Chabert E, Riffaud L, Haegelen C, Rolland Y. Spinal epidural angiolipoma. J Neuroradiol. 2001;28:253-256. [PubMed] [Cited in This Article: ] |
| 22. | Garg A, Gupta V, Gaikwad S, Deol P, Mishra NK, Sharma MC, Vaish S. Spinal angiolipoma: report of three cases and review of MRI features. Australas Radiol. 2002;46:84-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 23. | do Souto AA, Domingues FS, Chimelli L, Lemos AM. Lumbosacral angiolipoma: case report. Arq Neuropsiquiatr. 2003;61:269-273. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 24. | Rabin D, Hon BA, Pelz DM, Ang LC, Lee DH, Duggal N. Infiltrating spinal angiolipoma: a case report and review of the literature. J Spinal Disord Tech. 2004;17:456-461. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Samdani AF, Garonzik IM, Jallo G, Eberhart CG, Zahos P. Spinal angiolipoma: case report and review of the literature. Acta Neurochir (Wien). 2004;146:299-302; discussion 302. [PubMed] [Cited in This Article: ] |
| 26. | Dogan S, Arslan E, Sahin S, Aksoy K, Aker S. Lumbar spinal extradural angiolipomas. Two case reports. Neurol Med Chir (Tokyo). 2006;46:157-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Guzey FK, Bas NS, Ozkan N, Karabulut C, Bas SC, Turgut H. Lumbar extradural infiltrating angiolipoma: a case report and review of 17 previously reported cases with infiltrating spinal angiolipomas. Spine J. 2007;7:739-744. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Hungs M, Paré LS. Spinal angiolipoma: case report and literature review. J Spinal Cord Med. 2008;31:315-318. [PubMed] [Cited in This Article: ] |
| 29. | Sankaran V, Carey M, Shad A. Traumatic bleeding of spinal angiolipoma presenting with subacute paraparesis--a case report and histopathological aspects. Br J Neurosurg. 2010;24:714-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Klisch J, Spreer J, Bloss HG, Baborie A, Hubbe U. Radiological and histological findings in spinal intramedullary angiolipoma. Neuroradiology. 1999;41:584-587. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | O’Donovan NA, Naik K, Maloney WJ, Llewellyn CG. Spinal angiolipoma mimicking extradural lipomatosis. Can Assoc Radiol J. 1996;47:51-53. [PubMed] [Cited in This Article: ] |
| 32. | Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas. Report of three cases. J Neurosurg. 1993;78:280-286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 95] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 33. | Weill A, del Carpio-O’Donovan R, Tampieri D, Melanson D, Ethier R. Spinal angiolipomas: CT and MR aspects. J Comput Assist Tomogr. 1991;15:83-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Gelabert-González M, García-Allut A. Spinal extradural angiolipoma: report of two cases and review of the literature. Eur Spine J. 2009;18:324-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 35. | Ring D, Snyder B. Spinal canal compromise in Proteus syndrome: case report and review of the literature. Am J Orthop (Belle Mead NJ). 1997;26:275-278. [PubMed] [Cited in This Article: ] |
| 36. | Sakaida H, Waga S, Kojima T, Kubo Y, Matsubara T, Yamamoto J. Thoracic spinal angiomyolipoma with extracanal extension to the thoracic cavity. A case report. Spine (Phila Pa 1976). 1998;23:391-394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Oge HK, Söylemezoglu F, Rousan N, Ozcan OE. Spinal angiolipoma: case report and review of literature. J Spinal Disord. 1999;12:353-356. [PubMed] [Cited in This Article: ] |
| 38. | al-Anazi A, Ammar A, Shannon P, al-Mulhim F. Spinal extradural angiolipoma. Br J Neurosurg. 2000;14:471-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Gelabert-González M, Agulleiro-Díaz J, Reyes-Santías RM. Spinal extradural angiolipoma, with a literature review. Childs Nerv Syst. 2002;18:725-728. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Rocchi G, Caroli E, Frati A, Cimatti M, Savlati M. Lumbar spinal angiolipomas: report of two cases and review of the literature. Spinal Cord. 2004;42:313-316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Chotai S, Hur JS, Moon HJ, Kwon TH, Park YK, Kim JH. Spinal angiolipoma--case report. Neurol Med Chir (Tokyo). 2011;51:539-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Konya D, Ozgen S, Kurtkaya O, Pamir NM. Lumbar spinal angiolipoma: case report and review of the literature. Eur Spine J. 2006;15:1025-1028. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |